The outlook for children born with congenital heart disease continues to improve as a result of advances in paediatric cardiac surgery, catheter interventions, medical and perioperative management and imaging techniques. Most patients are now expected to live to adulthood, leading to a significant increase in the population of adults with congenital heart disease.1,2,3 These young people need to be supported as they make the transition into adulthood; they must be encouraged to take responsibility for their own health and to make informed decisions regarding careers and lifestyle.
Transition is a generic process that applies to all children and adolescents with chronic disease, including those with cardiac, diabetes, renal, rheumatological and respiratory conditions. The transition of care from child to adult healthcare systems must be seen as a continuous process, not a single event. It may be defined as “a purposeful, planned process that addresses the medical, psychosocial and educational/vocational needs of adolescents and young adults with chronic physical and medical conditions as they move from child‐centred to adult‐orientated health care systems”.4 The transition period is not completed on entrance to adult care and is only successfully achieved when the patient is empowered to take responsibility for their own health and lifestyle, often when they are in their mid‐20s. In some patients, this period may never end and in each patient this process is age and development dependent.
Congenital heart disease affects patients' lives in a number of ways and addressing the issues of education, employment and sports as well as relationships, healthcare, reproduction and lifestyle at an early stage will optimise patients' quality of life. The benefits of a well‐planned transition include improvements in clinical, educational and social outcomes for young people.5,6
The aim of this review is to highlight best practice for transition from paediatric to full adult care at the most suitable age for the patient. These recommendations arise from published literature, reports from working parties and expert groups, and a wealth of experience with many patients and their families.3,7,8,9,10
General aspects
The aim of a transition service is to orchestrate the smooth transfer of a paediatric patient to adult services over a length of time, possibly several years, during a period of medical stability. This generic process is essential to promote the young adult's understanding of their condition and its implications for adult life and lifestyle, and to develop a sense of independence and responsibility in the patient while providing support for the family. Previously, the prime consultation will have been with the parents, and hence it is of paramount importance that the patient begins to take an active role in their own management during the teenage years. Adolescence is a particularly vulnerable time, and unless transition is managed sensitively, teenagers may disappear from medical care with a significant proportion returning to specialist care only by default or when problems develop.11,12,13
Many young adults with congenital heart disease will require further intervention, develop heart failure or arrhythmias or be at increased risk of premature death, and many may want to become pregnant. Therefore, nearly all, except for those with the simplest cardiac lesions, will require expert cardiology care and management at some point in their lives.
The transition to an adult specialist centre can be an overwhelming experience with large volumes of information given in a new environment, so it is important that this occurs at a rate compatible with the patient's psychosocial development. Inherent difficulties with adult clinics include the shorter consultation times with new, different doctors and nurses. Young patients may be surrounded in the waiting room by older patients with very different pathology. The initial stage of transition is only successfully completed once patient attendance at the adult‐orientated clinic is established.
Transitional care plan
Transition clinics should be held frequently, in an agreed and structured, but flexible, multi‐disciplinary fashion between paediatric and adult services and where appropriate, involve specialist dental and gynaecological services.
Transition clinics should begin by 12 years of age, with age‐appropriate information, discussion and objectives. The patient's parents or carers should continue to be involved, but the patient should have some confidential time with their cardiologists and clinical nurse specialist. As teenagers grow older, the approach should change to give them more autonomy and provide information appropriate to their developmental stage. The staged approach should allow the patient to feel secure with their new medical team before full transfer to adult services around 16–18 years of age.
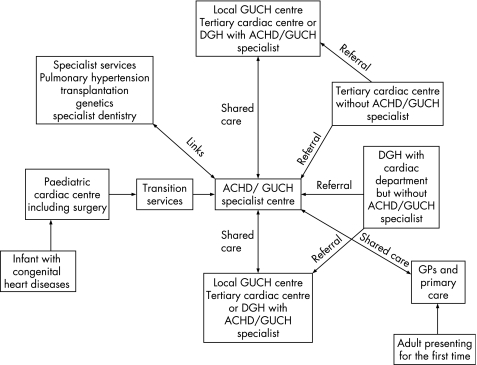
Care of these patients must involve local hospitals closely linked with specialist centres in order to provide patient facilities ranging from simple blood tests (eg, anticoagulation monitoring) in the local hospital to tertiary referral specialist services with specialist adult congenital cardiothoracic surgeons.10,14 A service model of transitional care, adjusted from the recent Department of Health document, is shown in fig 1. This highlights the need for close communication between local district general hospitals without an adult congenital heart disease specialist, tertiary specialist centres and primary care.10
Figure 1 A service model for adults with congenital heart disease.10
The transition clinic
There is no gold standard for the organisation of a transition clinic and local clinical needs will determine the available resources. Location of the clinic in parallel with the paediatric clinic makes the initial transition from paediatric care easier although at the expense of a slightly more difficult subsequent jump to the adult service. Clinic staffing is also determined by local resources. As a minimum, specialists and trainees in both paediatric and adult congenital heart disease should be present. In addition, a specialist nurse with particular experience of the needs of young adults with congenital heart disease should be provided with their own consulting area.
Our clinic involves not only an adult and paediatric cardiologist accompanied by trainees in their respective disciplines but also a specialist nurse with training in advanced counselling. These are assisted by a dedicated echocardiographer and ECG technician. On arrival in clinic all patients are initially seen by the specialist nurse with private discussion time before being seen by the physicians. Information regarding the transition process is given to each patient (a copy of the leaflet containing this information is available online at http://adc.bmj.com/supplemental). Each physician consulting room has a separate examination room, providing private discussion areas for patients.
Running a transition service
Each patient should have a comprehensive “passport” of information including diagnosis, full details of previous surgery and interventions, current and previous medical therapy and outpatient appointments, as well as contact details and information on the coordinating nurse specialist. The free flow of clinical information between treatment centres and the development of national networks and registries are essential to maintain accurate records as young adults move around the country and transfer to different specialist areas, as well as to facilitate research into this growing speciality.
The most important role within this transition model is that of the coordinating nurse specialist who should be available as the main contact point and coordinator throughout the transition process and should be experienced in the counselling of adolescents. Care pathways can be established to ensure essential information is obtained from and provided to all patients, who should be encouraged to discuss problems with the specialist nurse at the earliest possible opportunity.
Ideally the adult specialist centre should be accessible 24 h a day to provide both medical and non‐medical information and advice to both patients and other healthcare professionals. However, in the real world this is unlikely to be possible in most centres, and indeed transfer to the patient of responsibility to access appropriate health services is in itself a key aim of the transition process.
Inpatient care must be sensitive to young people's needs. Ideally, a dedicated ward should be provided for young people, not necessarily only those with cardiac disease, with facilities fulfilling their requirements, such as computers with internet facilities, a study area, games, television and private bathrooms as well as kitchen facilities. Financial demands may limit the availability of such specialised facilities; nonetheless, areas with specialty‐specific expert nursing care and equipment to cater for young adults with chronic disease should be provided within the hospital.
Patient profiles
Not all patients require the same level of specialist adult care: a quarter of cases are complex and require long‐term expert follow‐up, moderate cases must have access to a specialist, and some simple and/or corrected cases may not require any specialist follow‐up. Nonetheless, all adolescents require assistance through the transition period. The needs of those who will not require specialist follow‐up in adulthood should be addressed with care since they will not have access to specialist advice once they have been discharged from paediatric services.
Management
Medical follow‐up
The transition period may be the first opportunity for these patients to take personal responsibility for their health and is an appropriate time to address a wide range of issues with opportunities for private discussions with nurse specialists, counsellors and physicians.
Cardiac
Most patients reach adolescence without fully understanding their condition.15 Private consultation without parents is an essential first step in young people taking responsibility for their health. Clinical assessment, investigations and treatment modalities will be patient specific, but the development of unit protocols may aid in the rotation of junior staff and consistency of management.
Non‐cardiac surgery
Patients with congenital heart disease need to be aware of the implications of their condition for the provision of non‐cardiac surgery and medical care and non‐medical procedures such as piercing or intrauterine contraceptive coil fittings. This is particularly important as they move away from their home region to start work or college. They should know the importance of informing other medical providers about their condition and where these providers can obtain expert advice. Patients with cyanotic heart disease and pulmonary vascular disease represent the highest perioperative or periprocedure risk.16
Fertility, contraception and pregnancy
All adolescents should be counselled about sexual health, and girls should be counselled about contraception and pregnancy before they become sexually active. Discussions must be sensitive to the patient's developmental stage,17 and may be introduced gradually through the transition period. It must be remembered that the presence of parents may preclude any fruitful discussion and opportunities should be sought to allow the patient to ask questions in their absence. Patients should be reassured that discussions with the cardiology team are entirely confidential and will not be revealed to their parents without their consent. Up‐to‐date information should be provided of the risks of pregnancy to both the mother and the fetus, discussing not only the potential effects of a pregnancy on the mother's heart condition and her life expectancy but also the effects of her heart disease on the pregnancy. This allows the patient to make informed decisions about both her lifestyle and childbearing potential. Patients who have NYHA class III or IV, or pulmonary hypertension and systemic ventricular dysfunction, which have significant (>10%) maternal mortality rates, should be advised against pregnancy.18,19
In patients who are actively planning pregnancy, preconception prescription of folic acid may reduce the incidence of congenital heart disease. Finally, patients should be encouraged to inform the team as soon as they become pregnant, irrespective of their intentions for the pregnancy, to allow optimal care to be provided.
Genetic transmission and aetiology
As young patients become independent and take responsibility for their own health, they may wish to understand more about the causes of their condition and any implications this may have for their children or relatives. Understanding of the genetics of congenital and inherited cardiac diseases is increasing rapidly, but there is still a variable recurrence rate of congenital heart disease in offspring, ranging from 3% to 50%.20 Genetic counselling should be offered prospectively where more than one family member is affected or where a syndrome or specific genetic defect is suspected. Fetal echocardiography before 18 weeks' gestation should be available to all patients with congenital heart disease.
Dental care and endocarditis
Most congenital heart disease patients have a lifelong risk of bacterial endocarditis and hence must be educated regarding dental health, good oral hygiene and the need for regular dental check‐ups. Emphasis must be placed on the risks of endocarditis with body‐piercing, tattoos, acne, intrauterine contraceptive device (IUCD) insertion and interventional procedures with need for good skin hygiene. Following a publication from the British Society for Antimicrobial Chemotherapy,21 NICE guidelines for the use of antibiotics for endocarditis prophylaxis are awaited. Specialist dental teams should be involved in the transition period of all cardiac patients.
Psychosocial issues and counselling
Provision for psychosocial support and counselling of these patients is essential. Teenagers have to overcome a number of hurdles and those with cardiac disease need additional support for their anxieties regarding their condition and its management, social interaction, sexuality and childbearing, lack of self‐confidence as well as specific issues such as employment or insurance. Counselling regarding medication including its potential interaction with alcohol, drug use and tobacco should be provided. Support must also be given for parents and families, preparing for difficulties and fears of letting go of their child as they approach adulthood. Promotion of self‐esteem and encouragement to aim to fulfil realistic lifetime goals and aspirations must be provided sensitively.
Information/advice on occupation
Early counselling and discussion with teenagers and their families about achievable and realistic career choices should allow them to plan their education and aim for appropriate occupations. For many patients, physically demanding jobs are best avoided because of current or inevitable future cardiovascular restrictions to their exercise capacity. Close liaison with specialist career advisors, although not widely available, may be invaluable in allowing patients to develop realistic and appropriate life goals.
Sporting activities and interests
Many patients with congenital heart disease have impaired exercise capacity, and education regarding exercise and physical limitations is essential. However, involvement in sporting activities improves confidence and social interaction. Recommendations concerning participation in sports must be based on an understanding of the effects of the exercise on the individual's haemodynamics and must be tailored and adapted to the individual.22
Insurance
Current insurance policies are based on mortality risks of patients in long‐term follow‐up studies compared to population controls and may have a heavily loaded premium. However, within patient subgroups, morbidity and mortality rates vary and are changing with advancing medical care. Patients who may be offered high premiums or refused coverage should be advised to contact support groups (the Grown Up Congenital Heart Patients Association (http://www.guch.org.uk/) provides an excellent source of insurance advice and information) before applying, to gain the best deals and to avoid being turned down.23 Some patients may receive insurance cover through employers' group policies which do not require individual assessment. All patients should be given general lifestyle advice to minimise their coronary disease risk such as not to smoke.
Travel and driving
Patients should be empowered to seek the advice of the team as part of their travel planning. Although concerns may exist regarding air travel, patients with cyanotic heart disease usually tolerate commercial aircraft cabin pressures without the need for inhaled oxygen. Where appropriate, patients should not be discouraged from travel, but advice should be given with respect to realistic travel destinations. The same is true of driving: within the UK, there are regularly updated guidelines concerning the influence of a medical condition on a patient's safety to drive both a domestic or class II vehicle.24 It is the physician's responsibility to inform the patient regarding these and also of the implications certain treatment options may have on their driving, for example the insertion of an implantable cardioverter defibrillator (ICD).
Other support networks
There are a number of local, national and international support and advice groups. Patient support groups, including the GUCH Patients Association, and local support groups should encourage support with information leaflets and the sharing of real‐life experiences amongst both patients and their carers within each specialist centre.
Future training of specialists
With the ever increasing number of paediatric patients graduating to adult services, there is a pressing need to improve and expand training for cardiology and nursing trainees, particularly in the area of transition. Currently, this service need is not being met universally because of a shortage of trained and experienced medical, nursing, counselling and administrative staff. Recent recommendations for specialist training in adult congenital heart disease, with particular attention to the transition period, will hopefully improve service provision.3,8
Conclusion
The transition of care from paediatric to adult services represents a critical opportunity in the care of young people with cardiovascular disease. When successful it should empower them to take control of their own health and provides a platform for optimal disease management throughout their adult life. A poor transition risks alienating young adults from healthcare providers with subsequent poor compliance, loss to follow‐up and substandard medical care. Features of a successful transition programme include a coordinated, multidisciplinary and individualised patient‐centred approach which anticipates the social, emotional and psychological problems faced by all young adults.
A copy of the leaflet containing information on the transition process is available online at http://adc.bmj.com/supplemental.
Supplementary Material
Footnotes
Competing interests: None.
A copy of the leaflet containing information on the transition process is available online at http://adc.bmj.com/supplemental.
References
- 1.Macmahon B, McKeown T, Record R G. The incidence and life expectation of children with congenital heart disease. Br Heart J 195315121–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wren C, O'Sullivan J J. Survival with congenital heart disease and need for follow up in adult life. Heart 200185438–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.British Cardiac Society Working Party Grown‐up congenital heart (GUCH) disease: current needs and provision of service for adolescents and adults with congenital heart disease in the UK. Heart 200288(Suppl 1)i1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blum R W, Garell D, Hodgman C H.et al Transition from child‐centered to adult health‐care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J Adolesc Health 199314570–576. [DOI] [PubMed] [Google Scholar]
- 5.Steinkamp G, Ullrich G, Muller C.et al Transition of adult patients with cystic fibrosis from paediatric to adult care—the patients' perspective before and after start‐up of an adult clinic. Eur J Med Res 2001685–92. [PubMed] [Google Scholar]
- 6.Robertson L P, McDonagh J E, Southwood T R.et al Growing up and moving on. A multicentre UK audit of the transfer of adolescents with juvenile idiopathic arthritis from paediatric to adult centred care. Ann Rheum Dis 20066574–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Warnes C A, Liberthson R, Danielson G K.et al Task force 1: the changing profile of congenital heart disease in adult life. J Am Coll Cardiol 2001371170–1175. [DOI] [PubMed] [Google Scholar]
- 8.Deanfield J, Thaulow E, Warnes C.et al Management of grown up congenital heart disease. Eur Heart J 2003241035–1084. [DOI] [PubMed] [Google Scholar]
- 9.Therrien J, Dore A, Gersony W.et al CCS Consensus Conference 2001 update: recommendations for the management of adults with congenital heart disease. Part I. Can J Cardiol 200117940–959. [PubMed] [Google Scholar]
- 10.DH Vascular Programme Team Adult congenital heart disease: a commissioning guide for services for young people and grown ups with congenital heart disease (GUCH). London: Department of Health, 2006
- 11.Viner R. Transition from paediatric to adult care. Bridging the gaps or passing the buck? Arch Dis Child 199981271–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kipps S, Bahu T, Ong K.et al Current methods of transfer of young people with type 1 diabetes to adult services. Diabet Med 200219649–654. [DOI] [PubMed] [Google Scholar]
- 13.de Bono J, Freeman L J. Aortic coarctation repair—lost and found: the role of local long term specialised care. Int J Cardiol 2005104176–183. [DOI] [PubMed] [Google Scholar]
- 14.Tucker L B, Cabral D A. Transition of the adolescent patient with rheumatic disease: issues to consider. Pediatr Clin North Am. 2005;52: 641–52, viii, [DOI] [PubMed]
- 15.Dore A, de Guise P, Mercier L A. Transition of care to adult congenital heart centres: what do patients know about their heart condition? Can J Cardiol 200218141–146. [PubMed] [Google Scholar]
- 16.Warner M A, Lunn R J, O'Leary P W.et al Outcomes of noncardiac surgical procedures in children and adults with congenital heart disease. Mayo Perioperative Outcomes Group. Mayo Clin Proc 199873728–734. [DOI] [PubMed] [Google Scholar]
- 17.Thorne S A. Pregnancy in heart disease. Heart 200490450–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yentis S M, Steer P J, Plaat F. Eisenmenger's syndrome in pregnancy: maternal and fetal mortality in the 1990s. Br J Obstet Gynaecol 1998105921–922. [DOI] [PubMed] [Google Scholar]
- 19.Avila W S, Grinberg M, Snitcowsky R.et al Maternal and fetal outcome in pregnant women with Eisenmenger's syndrome. Eur Heart J 199516460–464. [DOI] [PubMed] [Google Scholar]
- 20.Burn J, Brennan P, Little J.et al Recurrence risks in offspring of adults with major heart defects: results from first cohort of British collaborative study. Lancet 1998351311–316. [DOI] [PubMed] [Google Scholar]
- 21.Gould F K, Elliott T S, Foweraker J.et al Guidelines for the prevention of endocarditis: report of the Working Party of the British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother 2006571035–1042. [DOI] [PubMed] [Google Scholar]
- 22.Mitten M J, Maron B J. Legal considerations that affect medical eligibility for competitive athletes with cardiovascular abnormalities and acceptance of Bethesda Conference recommendations. Med Sci Sports Exerc 199426S238–S241. [PubMed] [Google Scholar]
- 23.Vonder Muhll I, Cumming G, Gatzoulis M A. Risky business: insuring adults with congenital heart disease. Eur Heart J 2003241595–1600. [DOI] [PubMed] [Google Scholar]
- 24.Driver and Vehicle Licensing Authority Medical rules for drivers. http://www.dvla.gov.uk/medical.aspx (accessed 10 June 2007)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.