Abstract
Objectives
To evaluate the effectiveness and cost effectiveness of an intensive home visiting programme in improving outcomes for vulnerable families.
Design
Multicentre randomised controlled trial in which eligible women were allocated to receive home visiting (n = 67) or standard services (n = 64). Incremental cost analysis.
Setting
40 general practitioner practices across 2 counties in the UK.
Participants
131 vulnerable pregnant women.
Intervention
Selected health visitors were trained in the Family Partnership Model to provide a weekly home visiting service from 6 months antenatally to 12 months postnatally.
Main outcome measures
Mother–child interaction, maternal psychological health attitudes and behaviour, infant functioning and development, and risk of neglect or abuse.
Results
At 12 months, differences favouring the home‐visited group were observed on an independent assessment of maternal sensitivity (p<0.04) and infant cooperativeness (p<0.02). No differences were identified on any other measures. A non‐significant increase in the likelihood of intervention group infants being the subject of child protection proceedings, or being removed from the home, and one death in the control group were found. The mean incremental cost per infant of the home visiting intervention was £3246 (bootstrapped 95% CI for the difference £1645–4803).
Conclusion
This intervention may have the potential to improve parenting and increase the identification of infants at risk of abuse and neglect in vulnerable families. Further investigation is needed, along with long‐term follow‐up to assess possible sleeper effects.
Multiple studies undertaken over many years attest to the effect of parenting on the development of children and young people,1,2 and on their mental3,4,5 and physical health in adult life.6,7 Good quality, timely support for parents has now been identified in national and international policy documents as important for reducing social inequalities in health,8 preventing mental illness,9,10,11 and enhancing social and educational development.12
Questions remain, however, about how best to enable improvements in parenting in vulnerable families where parenting skills are poor, social and environmental risk factors are high, and a considerable risk of abuse or neglect exists. Children growing up in such families have a high incidence of emotional and behavioural problems, school failure, delinquency in childhood and adolescence, and psychological and social difficulties as adults.13
Home visiting programmes have been posited as one approach to supporting parenting in vulnerable families, and such programmes are now being used in countries such as the USA, Australia and New Zealand. Although the evidence base suggests that these programmes are not uniformly effective, recent reviews of reviews conclude that they can support parents, change parenting practices and improve infant outcomes.14 A small number of studies in the UK15,16,17,18 have compared the effectiveness of different types of home visiting programmes with standard health visiting, but none has dealt with the effectiveness of such programmes with parents who have been identified prenatally as being at high risk of poor parenting.
Methods
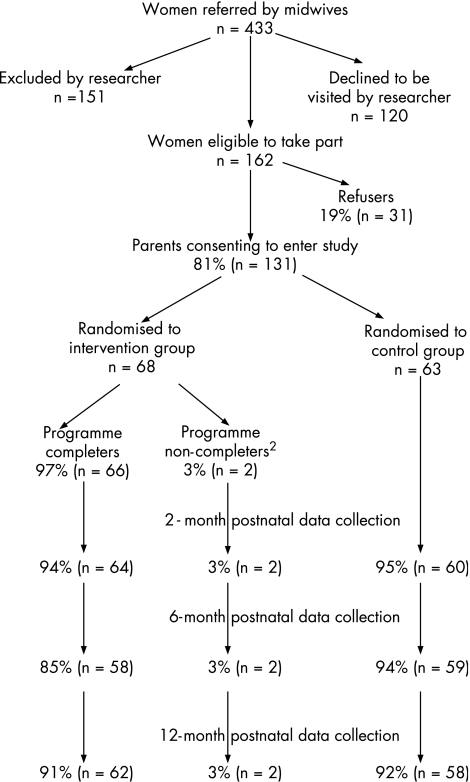
A multicentre randomised controlled trial (RCT) was conducted comparing home visiting with standard treatment. After consent and the collection of baseline data, randomisation was undertaken using sequentially numbered sealed opaque envelopes (fig 1). Ethical approval was given by the Oxford Psychiatric Research Ethics Committee.
Figure 1 Uptake and attrition rates.
Intervention
All parents randomised to the intervention group received 18 months of weekly visits from a health visitor trained in understanding the processes of helping, skills of relating to parents effectively and methods of promoting parent–infant interaction using the Family Partnership Model.19 Parents in both the control and intervention groups continued to receive the standard help currently available to such families.
Inclusion or exclusion criteria
Community midwives attached to 40 participating general practitioner practices across 2 counties screened women using a range of demographic and socioeconomic criteria (eg, mental health problems or housing problems). Women not wishing to be randomised or without a working understanding of English were excluded.
Statistical power
The study was powered to detect a change of 0.5 standard deviations (SDs) on one measure of mother–child interaction (the CARE Index) and one measure of maternal mental health (the General Health Questionnaire), allowing for a 25% loss to follow‐up and using 80% power.
Blinding
Data were collected, coded and analysed by researchers who had not been involved in recruitment and were therefore blind to the intervention group.
Economic evaluation
Resource‐use data were obtained as an integral part of the trial data collection forms. Women were asked to maintain a diary of service use to aid recall. Unit costs (2003–4) were then attached to the items of resource use to identify a mean difference in costs between the two arms of the trial.20 Recommended discount rates of 3.5% were used for both costs and benefits where applicable.21 The perspective of the study was societal (ie, health service, social services, legal and housing costs were included).
Data analysis
An intent‐to‐treat analysis was conducted using univariate analysis of covariance for continuous variables and multivariate analysis of covariance for continuous variables in which the predictor variable comprised multiple scales. Significance was assessed at the 0.05 level. All analyses were adjusted for baseline scores and for baseline level of risk as indicated by the number of risk factors present at screening. Relative risk (RR) was calculated for dichotomous variables along with 95% confidence intervals (CIs).
Outcome measures
Home visiting is a holistic intervention from which a wide range of positive outcomes have been reported14; therefore, several measures of outcome were included.
Parent–child interaction
Mother–infant interaction was assessed at 12 months on the basis of a 3‐min video recording and coded for maternal sensitivity and infant cooperativeness using the CARE Index.22 One researcher, blinded to the intervention group, coded all videotapes and a random sample of 10% of videos was independently coded. A ⩽2‐point difference was observed for 92% of codings for maternal sensitivity and for 75% of codings for infant cooperativeness.
Maternal psychopathology was assessed at 6 and 12 months using the General Health Questionnaire,23 and postnatal depression was assessed at 8 weeks using the Edinburgh Postnatal Depression Scale.24
Parenting attitudes and competence were assessed at 6 and 12 months using the Adult Adolescent Parenting Inventory.25 Parenting competence/confidence and experiences were measured at 12 months using the Parenting Sense of Competence scale26 and What Being the Parent of a Baby is Like (WBPB).27
Social support, marital/partner discord, self‐esteem, perceived self‐efficacy and parenting stress were assessed at 6 and 12 months using the Social Support Questionnaire,28 the Rust Inventory of Marital State,29 Rosenberg Self‐Esteem Inventory,30 Generalised Self‐Efficacy Scale31 and the Parenting Stress Inventory.32
The quality of the infant's home environment was assessed at 12 months using the HOME Inventory,33 and infant–toddler social and emotional adjustment was assessed using the Brief Infant–Toddler Social and Emotional Assessment,34 comprising two subscales: competence and problems. Infant development was assessed independently at 12 months using the Bayley Scales of Infant Development.35 Maternal assessment of the infant's temperament was measured using the Infant Temperament Scale (ITS).36 Parents were also asked to report infant well‐being at 6 months (eg, feeding, immunisation, disability). Participating health visitors provided data relating to case conferences, children on the protection register, children removed from the home and child deaths. Demographic details were collected from all respondents at baseline.
Results
Sample
In all, 162 women were eligible and 20% (n = 31) of these refused. No significant differences were found between the refusers and those who agreed to participate.
Dropout rate from the intervention was 3% and attrition <10%. Table 1 shows the distribution of demographic and other risk factors for the sample.
Table 1 Description of demographic and risk factors in sample.
| Home visiting (n = 68), % (n) | Control group (n = 63) % (n) | |
|---|---|---|
| Single parent | 35.9 (23) | 34.3 (23) |
| Eligible for free school meals | 20 (13) | 11.7 (7) |
| Ethnicity | ||
| White | 92.5 (62) | 95.3 (61) |
| Black | 1.5 (1) | 1.6 (1) |
| Asian | 3 (2) | |
| Other | 3 (2) | 3.1 (2) |
| Work status | ||
| Working full/part time | 28.2 (17) | 29 (18) |
| Caring for home | 41.8 (28) | 39.1 (25) |
| Unemployed | 13.4 (9) | 9.4 (6) |
| Disabled | 6 (4) | 9.4 (6) |
| Other | 13.4 (9) | 14 (9) |
| Accommodation | ||
| Owned | 16.4 (11) | 23.8 (15) |
| Rented | 83.5 (56) | 76.2 (48) |
| ⩾2 moves in the past 12 months | 31.3 (21) | 45.3 (29) |
| No educational/vocational qualifications | 34.8 (23) | 26.6 (17) |
| Age <17 years | 17.9 (12) | 22.2 (14) |
| Poverty (<£200 per week) | 59.7 (40) | 62.5 (40) |
| No educational/vocational qualifications | 34.3 (23) | 25.4 (16) |
| No support network | 6 (4) | 7.9 (5) |
| Unhappy childhood | 26.9 (18) | 19 (12) |
| Children with behaviour problems | 35.8 (24) | 28.6 (18) |
| Social worker* | 23.9 (16) | 19.0 (12) |
| ⩾2 moves in the past 12 months | 9 (6) | 15.9 (10) |
| Physical illness/disability | 11.9 (8) | 7.8 (5) |
| Mental health problem* | 64.2 (43) | 58.7 (37) |
| Partner with mental health problem | 17.9 (12) | 12.7 (8) |
| Housing concerns | 55.2 (37) | 50.8 (32) |
| Unwanted pregnancy | 35.8 (24) | 34.9 (22) |
| Recent event that caused concern | 49.3 (33) | 49.2 (21) |
| Alcohol problem† | 14.9 (10) | 9.5 (6) |
| Drug misuser | 10.4 (7) | 3.2 (2) |
| Domestic violence (current)‡ | 34.3 (23) | 34.3 (22) |
| Previous attendance of self/partner at court for criminal reasons | 29.9 (20) | 23.8 (15) |
*Previous or current.
†People who are concerned about their drinking, now or in the past.
‡Includes oral harassment and women who reported other forms of violence sometimes or regularly. May be an underestimate: excludes women who “prefer not to say” or who answered “rarely”.
The mean number of risk factors per woman was five in both the intervention and control groups, but a slightly larger number of women in the intervention group were classified as high risk (22.4% of home‐visited women had ⩾8 risk factors compared with 14.1% of the control group). We found no differences between the groups in any of the measures collected at birth, including gestational age, birth weight or method of delivery. Women in the control group had a mean of 9.2 visits by health visitors compared with 41.2 visits in the intervention arm. The intervention group received on average two thirds of the total possible number of visits (n = 72).
Two‐month assessment
We found no statistically significant differences between the two groups in scores on the Edinburgh Postnatal Depression Scale.
Six‐month assessment
A larger but non‐significant proportion of infants in the home visiting arm were breast fed up to 6 months (55% v 45%), and minor disabilities were detected (9.7% v 1.7%). A smaller but again non‐significant proportion of home‐visited infants were admitted to hospital during the first 6 months after birth (8.5% v 14.5%). No differences were seen between the groups with respect to the introduction of solids before 12 weeks, the mean number of days stayed in hospital or uptake of immunisations.
No significant differences were observed between the two groups at 6 months in any of the standardised parent‐report outcomes (mental health self‐esteem, self‐efficacy, social support, relationship with partner) (table 2).
Table 2 Effect of intervention on infant outcomes at 6‐month follow‐up*.
| Variable | Home visiting | Control group | RR (95% CI) |
|---|---|---|---|
| (n = 68) | (n = 63) | ||
| Proportion that continued breast feeding for at least 6 months, % (n) | 55.2 (48) | 44.5 (39) | 1.22 (0.85 to 1.75) |
| Proportion with disabilities, % (n)† | 9.7 (6) | 1.7 (1) | 3.53 (0.57 to 21.85) |
| Proportion introduced to solids before 12 weeks, % (n) | 13.5 (9) | 17.5 (11) | 0.85 (0.51 to 1.43) |
| Proportion of admissions of baby to hospital since birth, % (n) | 8.1 (5) | 14.3 (8) | 1.38 (0.68 to 2.8) |
| Median days stayed in hospital, mean (SD) | 3 (8.7) | 4.0 (1.1) | NA |
| Proportion of immunisations during the past 6 months, % (n) | 98.3 (58) | 100 (59) | NA |
NA, not applicable.
*Based on the maternal report 6 months after birth.
†Includes the following: squint, shallow hip socket and birthmark, dilated renal pelvis, hearing problems, fistula on neck and milk intolerance, cleft palate and epilepsy, and kidney problems.
12‐month assessment
Objective measures
Results for the CARE Index suggest that women in the intervention arm were significantly more sensitive to their babies (p = 0.04), who were significantly more cooperative (p = 0.02) (table 3).
Table 3 Effect of intervention on mother–child interaction (CARE Index): mean (SD) scores at 12 months and results of univariate and multivariate analysis of covariance adjusting for total number of risk factors.
| Measure (CARE Index scale*) | Study group | n | Mean (SD) | ANCOVA p value | MANCOVA p value |
|---|---|---|---|---|---|
| Maternal sensitivity | Control | 59 | 8.2 (3.26) | 0.03 | 0.04 |
| Home visiting | 62 | 9.27 (2.67) | |||
| Infant cooperativeness | Control | 59 | 7.92 (3.7) | 0.012 | 0.02 |
| Home visiting | 62 | 9.35 (3.08) |
ANCOVA, analysis of covariance; MANCOVA, multivariate analysis of covariance.
*A score of 12 is optimum.
No significant differences were found between the two arms on the remaining two independent measures: the HOME Inventory or Bayley Scales.
Similar numbers of child protection issues were identified in the two groups between 6 and 12 months of age (17% home visiting groups and 15% control group), but a non‐significant increase in the likelihood of placement on the child protection register or care proceedings in the intervention group (RR 2.02, 95% CI 0.46 to 2.54) and a non‐significant difference in the proportion of children being removed from the home (6% v 0%) were observed. Half of these children were returned to the home at a later date. One child died in the control group, for whom child protection concerns were raised.
Parent‐report measures
One significant group effect was identified for social support (p>0.004), indicating a greater fall‐off in social support in the control group, possibly due to the low response to this question at follow‐up. No significant group, time, or time by group effects were observed for any other parent‐report measures (table 4).
Table 4 Effect of intervention on maternal functioning: mean scores at baseline, 6 months and 12 months and results of analysis of covariance adjusting for baseline scores and total number of risk factors.
| Measure* | Study group | n | Assessment | ANCOVA p values | ||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 6 months | 12 months | Study group | Time | Time by group | |||
| Mental health (GHQ) | Control | 56 | 15.14 (7.39) | 13.96 (7.43) | 11.88 (7.24) | 0.75 | 0.026 | 0.92 |
| Home visiting | 61 | 14.98 (6.28) | 13.98 (6.69) | 12.34 (5.56) | ||||
| Social support (SSQ) | Control | 12 | 20.67 (8.47) | 14.67 (6.02) | 15 (6.37) | 0.004 | 0.45 | 0.68 |
| Home visiting | 17 | 20.41 (6.61) | 20.71 (6.62) | 19.41 (7.97) | ||||
| Self‐esteem (RSI) | Control | 55 | 28.25 (5.54) | 28.42 (5.2) | 29.42 (6.24) | 0.9 | 0.91 | 0.72 |
| Home visiting | 59 | 28.03 (5.24) | 28.53 (5.34) | 29.19 (5.39) | ||||
| Relationship with partner (GRIMS) | Control | 28 | 56.54 (10.43) | 52.96 (14.2) | 53.36 (11.03) | 0.39 | 0.29 | 0.97 |
| Home visiting | 36 | 57.61 (13.65) | 51.64 (16.31) | 51.83 (13.13) | ||||
| Self‐efficacy (SEQ) | Control | 54 | 27.28 (3.9) | 27.3 (4.48) | 28.48 (5.55) | 0.33 | 0.41 | 0.75 |
| Home visiting | 63 | 27.35 (4.97) | 27.88 (4.96) | 29.21 (4.67) | ||||
ANCOVA, analysis of covariance; GHQ, General Health Questionnaire; GRIMS, Rust Inventory of Marital State; RSI, Rosenberg Self‐Esteem Inventory; SEQ, Self‐Efficacy Questionnaire; SSQ, Social Support Questionnaire.
*Higher scores on the SSQ, RSI and SEQ indicate improvement; lower scores on the GHQ and GRIMS indicate improvement.
Economic evaluation
The mean costs per infant in the intervention and control arms were £7120 v £3874, a statistically significant difference of £3246 (bootstrapped 95% CI for the difference £1645–4803). The total costs of the intervention arm were greater because of increased home visits, phone calls to home visitors, appointments with psychologists, psychiatrists, foster care, adoption and home visitor training costs. However, there were cost savings for clinic health visiting, hospital accident and emergency visits for infants and mothers, and alcohol and drug counselling. The incremental cost per child “identified” as being ill‐treated on the basis of child protection proceedings between 6 and 12 months was £54 370.
Discussion
The results of this study suggest that early home visiting based on the Family Partnership Model can improve the sensitivity and attunement of high‐risk mothers to their infants and infant cooperativeness. However, because there were no significant differences between the two groups for most of the large number of outcomes measured, it is possible that this one positive finding occurred by chance. Most of the findings favoured the intervention group, but lacked statistical significance, suggesting that the study may also have been underpowered.
Focus group discussions with the health visitors delivering the intervention37 and in‐depth one‐to‐one interviews with participating mothers38 provide a contrasting insight into the effect of the programme from that offered by the quantitative data.38,39 Although these qualitative data cannot provide evidence of overall effectiveness, they suggest that the participants experienced changes, that would not have been captured with the standardised outcome instruments used in this trial.
What is already known on this topic
Home visiting programmes can be an effective means of improving parenting and a range of other important outcomes for high‐risk parents and their babies.
Their role in preventing abuse is disputed in part because of the issue of surveillance bias.
Little evidence exists on their effectiveness in the UK.
What this study adds
The results provide tentative evidence to suggest that intensive home visiting by UK‐based health visitors during the perinatal period can improve parenting and increase the identification of infants in need of early removal from the home in vulnerable families.
These findings need further investigation, including longer‐term follow‐up, to assess the extent to which these outcomes are worth the incremental costs.
This home visiting programme seemed to have increased the number of cases of abuse identified in the intervention arm. This outcome is often treated as an example of surveillance bias. An alternative view recognises such an outcome as a valuable secondary prevention of the deleterious consequences of abuse. Improvements in health visitors' sensitivity to abusive parenting may have enabled them to institute child protection proceedings at an earlier stage in the child's life, reducing the length of exposure to damaging environments by placing infants with substitute parents during the first year of life. Such a view is supported by new research, which suggests that abused children adopted in infancy fare much better than children adopted after 4 years of age.39 The one death in the control group about which there were child protection concerns did not achieve statistical significance because of the small sample size, but may nevertheless have been an important finding.
Conclusions
This study provides evidence to suggest that this intensive home visiting programme may improve parenting in vulnerable families and increase identification of abuse and neglect in infancy for an added cost of £3246 per child. Further follow‐up is needed to identify potential sleeper effects and to assess the longer‐term effect on child abuse. Meanwhile, uncertainty surrounding the results means that the case for provision is not strong, and suggests the need for further research both to confirm the findings and possibly to increase the efficacy of the programme.
Abbreviations
RCT - randomised controlled trial
Footnotes
Funding: Department of Health, Nuffield Foundation.
Competing interests: None.
References
- 1.Early Child Care Research Network Child care and child development: results of the NICHD Study of early child care and youth development. New York: Guildford Press, 2005
- 2.National Research Council and Institute of Medicine From neurons to neighborhoods: the science of early childhood development. Committee on Integrating the Science of Early Childhood Development. In: Shonkoff JP, Phillips DA, eds, Board on children, youth and families, commission on behavioral and social sciences and education. Washington, DC: National Academy 2000 [PubMed]
- 3.Patterson G R, DeBaryshe B D, Ramsey E. A developmental perspective on antisocial behaviour. Am J Psychol 198944329–335. [DOI] [PubMed] [Google Scholar]
- 4.Robins L N, Rutter M C. eds. Straight and devious pathways from childhood to adulthood. Cambridge: Cambridge University Press, 1990
- 5.Egeland B. Mediators of the effects of child maltreatment on developmental adaptation in adolescence. In: Cicchetti D, Toth L, eds. Developmental perspectives on trauma: theory, research, and intervention Rochester, NY: University of Rochester, 1997
- 6.Stewart‐Brown S, Shaw R. The roots of social capital: relationships in the home during childhood and health in later life. In: Morgan A, Swann C, eds. Social capital for health: issues of definition, measurement and links to health London: Health Development Agency, 2004
- 7.Stewart‐Brown S L, Fletcher L, Wadsworth M E J. Parent‐child relationships and health problems in adulthood in three national birth cohort studies. Eur J Public Health 200515640–646. [DOI] [PubMed] [Google Scholar]
- 8.Acheson D.Independent inquiry into inequalities in health. London: The Stationery Office, 1998
- 9.European Commission Improving the mental health of the population: towards a strategy on mental health for the European Union. Brussels: Green Paper, European Commission, 2005
- 10.Department of Health National Service Framework for children, young people and maternity services. London: The Stationery Office, 2004
- 11.National Institute for Mental Health in England Making it possible: improving mental health and well‐being in England. London: NIMHE, 2005
- 12.Department for Education and Skills Every child matters. London: The Stationery Officer, 2004
- 13.Angold A, Costello E. Developmental epidemiology. Epidemiol Rev 19951774–82. [DOI] [PubMed] [Google Scholar]
- 14.Bull J, McCormick G, Swann C.et alAnte‐ and post‐natal home‐visiting programmes: a review of reviews. London: HAD, 2004
- 15.Davis H, Dusoir T, Papadopoulou K.et al Child and family outcomes of the European Early Promotion Project. Int J Mental Health Promot 2005763–81. [Google Scholar]
- 16.McAuley C, Knapp M, Beecham J.et alEvaluating the outcomes and costs of home‐start support to young families experiencing stress: a comparative cross‐nation study. York: Joseph Rowntree Foundation, 2004
- 17.Wiggins M, Oakley A, Roberts I.et al Postnatal support for mothers living in disadvantaged areas: a randomised controlled trial and economic evaluation. Health Technol Assess 200481. [DOI] [PubMed] [Google Scholar]
- 18.Morrell C J, Siby H, Sewart P.et al Costs and effectiveness of community postnatal support workers: randomised controlled trial. BMJ 2000321593–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davis H, Day C, Bidmead C.The parent adviser training manual. London: Harcourt Assessment, 2002
- 20.Netten A, Curtis L.Unit costs of health and social care. Canterbury: Personal Social Services Research Unit, University of Kent at Canterbury, 2004
- 21.Treasury H M.The green book. London: The Stationery Office, HMSO, 2003
- 22.Crittenden P M.CARE‐Index infant and toddlers. Coding manual. USA: Family Relations Institute, 2001
- 23.Goldberg D P.General Health Questionnaire 28. Windsor, UK: NFER‐Nelson, 1981
- 24.Cox J L, Holden J M, Sagovsky R. Detection of postnatal depression: development of the 10‐item Edinburgh Postnatal Depression Scale. Br J Psychiat 1987150782–786. [DOI] [PubMed] [Google Scholar]
- 25.Bavolek S J.Handbook for the adult‐adolescent parenting inventory. Eau Claire, WI: Family Development Resources, 1986
- 26.Gibaud‐Wallston J, Wandersman L P. Development and utility of the parenting sense of competence scale. Paper presented at the Meeting of the American Psychological Association, Toronto 1978
- 27.Pridham K F, Chang A S. What Being the Parent of a Baby is Like: revision of an instrument. Res Nurs Health 198912323–329. [DOI] [PubMed] [Google Scholar]
- 28.Sarason I G, Levine H M, Basham R B.et al Assessing social support: the Social Support Questionnaire. J Personal Soc Psychol 198344127–139. [Google Scholar]
- 29.Rust J, Bennum I, Crowe M.et alThe Golombok Rust Inventory of Marital State. Windsor, UK: NFER‐Nelson, 1988
- 30.Carey W B, McDebitt S C. Revision of the Infant Temperament Questionnaire. Pediatrics 197861735–739. [PubMed] [Google Scholar]
- 31.Jerusalem M, Schwarzer R. Self‐efficacy as a resource factor in stress appraisal processes. In: Schwarzer R, ed. Self‐efficacy: Thought control of action Washington, DC: Hemisphere, 1992195–213.
- 32.Terry D J. Stress, coping and adaptation to new parenthood. J Soc Personal Relationships 19918527–547. [Google Scholar]
- 33.Bradley R, Caldwell B. Home observation for measurement of the environment: a revision of the pre‐schoolscale. Am J Mental Defic 197084235–244. [PubMed] [Google Scholar]
- 34.Briggs‐Gowan M J, Carter A S.The Brief Infant‐Toddler Social and Emotional Assesment (BITSEA) manual. New Haven, CT: Department of Psychology, Yale University, 2001
- 35.Bayley N.Bayley Scales of Infant Development. San Antonio, TX: Psychological, 2000
- 36.Carey W B, McDebitt S C. Revision of the Infant Temperament Questionnaire. Pediatrics 197861735–739. [PubMed] [Google Scholar]
- 37.rocklehurst N, Barlow J, Kirkpatrick S.et al The contribution of health visitors to supporting vulnerable children and families through intensive home visiting. Community Prac 200477175–179. [Google Scholar]
- 38.Kirkpatrick S, Barlow J, Stewart‐Brown S.et al Working in partnership: vulnerable women's perceptions of health visitors following participation in an intensive home visiting study. J Child Abuse Review. In press
- 39.Kaniuk J, Steele M, Hodges J. Report on a longitudinal research project, exploring the development of attachments between older, hard‐to‐place children and their adopters over the first two years of placement. Adoption Fostering. 2004: 28, 61–7. (Cited in Paz I, Jones D, Byrne G. Child maltreatment, child protection and mental health. Curr Opin Psychiatry 200518411–421. [DOI] [PubMed] [Google Scholar]