Abstract
Body art in the form of tattoos and piercing has become increasingly popular amongst children and teenagers, and is nowadays more socially acceptable despite media reports citing tissue destruction and death. Our study explored the awareness and experience of patients with congenital heart disease, and of cardiologists and professionals responsible for their care.
We investigated the awareness of patients with congenital heart disease and their families of the potential link between body art and endocarditis.
Methods
We distributed 600 questionnaires to patients attending paediatric cardiology clinics at Birmingham Children's Hospital between March and May 2004, asking whether they had or were planning to have body art, whether they were aware of the increased risk of endocarditis, and if they had or were planning to seek advice. The underlying cardiac conditions were divided into the following groups: complex, cyanotic, shunt, obstructive, prosthesis or regurgitant lesions.
At the same time, we approached 68 paediatric cardiologists including those looking after patients with adult congenital heart disease in all 16 UK centres, asking about the advice they would give to their patients, whether they had a standard departmental policy and if they had experience with cases of endocarditis following body art.
Results
Patient group
Of the 600 questionnaires sent out, 486 (81%) returned forms could be analysed from patients with a mean age of 8.05 years (4 weeks–38 years). A total of 87 (17.9%) children had body art: 86 had body piercing (78 ear, one eyebrow, four nasal, three umbilical) with a mean age of 12 years and one had a tattoo at 15 years. Only one had developed endocarditis after ear piercing; he had an obstructive lesion and did not seek advice prior to piercing. Fifty four (62%) patients out of 78 were not aware that they should seek advice. Thirty three (38%) sought advice: 12 asked their cardiologists (four were advised against, six were advised to take sterile precautions, and two were told that there was no need for precautions) and 21 took advice from non‐cardiology medical professionals (five were advised against, eight were advised to take sterile precautions and eight were told there was no need for precautions).
Consultant group
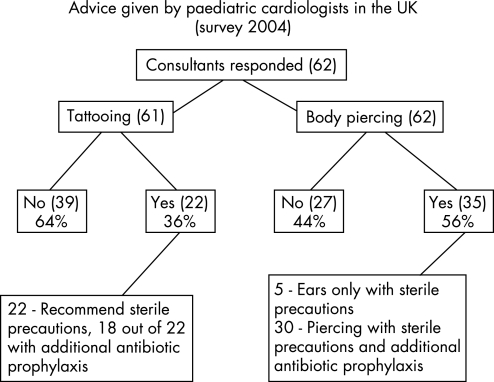
Sixty two (91%) of the 68 consultants responded to the questionnaire (fig 1). Only two (11%) of the 16 UK paediatric cardiac centres had an agreed departmental policy, 16 consultants in nine cardiac centres reported endocarditis after body piercing, and we accepted one case of endocarditis from each of the nine centres including one reported death. Three consultants from three different cardiac centres reported three additional cases of endocarditis following tattooing. The two consistent sites of body piercing associated with endocarditis were the lower lip and nose. Thirty nine consultants would give universal advice for antiseptic precautions and antibiotic prophylaxis, 22 would give a lesion‐specific advice, and one was never asked. Eight out of 16 consultants (50%) reporting endocarditis related to body art have changed their practice.
Figure 1 Advice given by paediatric cardiologists in the UK (2004 survey). Yes: would agree for the patient to have body art; No: would discourage the patient from any form of body art.
Discussion
The European Research Commission was alarmed by the reports of two death at the end of 2002. They carried out an extensive study and found that up to 50% of body piercings can lead to acute infection. The existing regulations in EU member states were limited to the use of gloves and sterilisation of equipment but did not tackle the issue of the sterility of materials, dyes and colours, their purity or the need for proper toxicological and risk evaluation. The EU regulatory review of May 20031 pointed out that some chemicals used in tattoos are industrial pigments suitable for automobile paint or printers' ink. The following are complications from actual reported cases related to body art, from data collected by the European Commission:
Viral infections: hepatitis, HIV
Bacterial infections: impetigo, toxic shock syndrome, tetanus, venereal ulcer, tuberculosis
Fungal infections: sporotrichosis, zygomycosis
Allergic reactions: cutaneous irritation, urticaria
Granulomateus/lichenoid reactions
Pseudolymophoma
Lymphadenopathy
Skin lesions: photosensitisation, phototoxicity, melanoma, skin cancer
In the UK, businesses carrying out cosmetic body piercing are under local authority control and are regulated by the 1988 act (updated 2003), section 120 of which has attempted to address the changes in Europe,2 although the issues of stud sterility and the safety of the materials used for permanent colours were not tackled. Children under the age of 16 years are not able to consent lawfully to a body piercing. A statutory minimum age of consent for tattooing (18 years of age) is specified in the Tattooing Minors Act 1969.2 The introduction of a minimum age of consent to body piercing might result in children piercing themselves or each other in an unsafe and unhygienic manner or going to unregulated businesses either here or abroad, bearing in mind that some organisms, such as Staphylococcus aureus, can induce infective endocarditis even in structurally normal hearts3 and in a more recent case report, after oral piercing.4 Cetta et al conducted a survey5 and found that 23% of patients had piercing‐related infections 1 week to 3 years post‐implant but no endocarditis. A more recent review looked at the infections including endocarditis caused by body piercing and tattoos.6
While it was worrying that most patients in our group did not seek advice before having body art, it is of greater concern that those who did seek advice were given such widely varying recommendations, from avoidance of body art altogether to taking no precautions at all.
Most of the paediatric cardiologists were not aware that tattooing could lead to endocarditis. Two felt that the risk of persistent occult bacteraemia would not be eliminated by antibiotic prophylaxis at the time of body piercing and they would rather recommend treatment if the site in question showed any sign of inflammation. Most paediatric cardiologists, including those dealing with adult congenital heart disease patients, did not routinely offer advice about body art.
It is debatable whether the responsibility lies with the cardiologist. We think it should lie principally with the practitioners of body art. On the other hand, doctors should be aware of the risks involved, so that they can give clear advice (if they are consulted) on the risks of this cosmetic but potentially lethal practice.
The British Association of Antimicrobial Chemotherapy (BSAC) recently published new recommendations in relation to antibiotic prophylaxis for cardiac patients.7 Serious concerns have been raised by both paediatric and adult cardiac professionals in the UK in response to this publication. As a result of these concerns, NICE is currently reviewing the evidence and the guidelines for antimicrobial prophylaxis for patients with heart disease (British Congenital Cardiac Association; personal communication). We would hope that this will cover the issues related both to body piercing and tattooing in addition to dental procedures.
Conclusion
Better knowledge and education about the link between body art and endocarditis is required in order to provide guidelines for doctors and patients. Further data are needed to establish the true extent of this problem, but in an increasingly litigious society, with growing media attention regarding the potential link between body art and infective endocarditis, there appears to be no consensus amongst professionals as to the correct advice to give to individuals at risk.
NICE guidelines are awaited, along with an agreed policy between UK paediatric and adult congenital cardiac centres. For the time being, in our own practice we strongly discourage all forms of body art and we recommend antibiotic prophylactic cover where individuals cannot be dissuaded, with strong advice for prompt treatment of any signs of subsequent infection.
Footnotes
Competing interests: None.
References
- 1.European Commission Regulatory review on the safety of tattoos, body piercing and related practices. May 2003. Available from http://ec.europa.eu/consumers/cons_safe/news/eis_tattoo_reg_052003_en.pdf (accessed 23 August 2007)
- 2.DH Local Government Act 2003. Regulation of cosmetic piercing and skin‐colouring businesses. Guidance on section 120 and schedule 6. London: Department of Health Publications, 20041–22.
- 3.Ramage I J, Thomson R B, Wilson N. Fashion victim: infective endocarditis after nasal piercing. Arch Dis Child 199777183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dubose J, Preatt J W. Victim of fashion: endocarditis after oral piercing. Curr Surg 200461(5)474–477. [DOI] [PubMed] [Google Scholar]
- 5.Cetta F, Graham L C, Lichtenberg R C.et al Piercing and tattooing in patients with congenital heart disease: patient and physician perspectives. J Adolesc Health 199924160–162. [DOI] [PubMed] [Google Scholar]
- 6.Handrick W, Nenoff P, Muller H.et al Infections caused by piercing and tattoos – a review. Wien Med Wochenscher 2003153(9–10)194–197. [DOI] [PubMed] [Google Scholar]
- 7.Gould F K, Elliott T S J, Foweraker J.et al Guidelines for the prevention of endocarditis: report of the Working Party of the British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother 200657(6)1035–1042. [DOI] [PubMed] [Google Scholar]