Short abstract
Continuity of care would result in a better standard of care
As doctors working in a busy clinic alongside colleagues, we often encounter a number of patients whom we have never met before. Within the allocated time, we have to become rapidly acquainted with the patient's previous history, develop a rapport and move on to address the patient's present problems. The patient also has to quickly come to trust an unfamiliar face on the basis of their professional standing. One cannot but feel that if patients saw the same doctor at each clinic appointment, a better standard of care would result, along with a more satisfactory and effective consultation for both patient and doctor.
This sounds like common sense, and in these circumstances it is always interesting to know if there is an evidence base for the self evident. Is continuity of care important to professionals and to patients and, most important, is it clinically important? If it is, we should be making sure that our services take this into account.
Evidence in support of good continuity of care
Within the literature there has indeed been a focus on the importance of continuity of care. A number of studies have been carried out, principally in the area of general practice. Key studies in Norway showed that continuous care not only increased patient satisfaction but also allowed the doctor to accumulate knowledge that saved time, influenced their use of laboratory tests, allowed for expectant management, and to a lesser degree affected the use of medication.1,2 Patients were shown to value their relationship with their doctor more and felt they had more control over their health.2 Patients were not only more satisfied with the service, but the reduction in time and the more judicious use of investigations all improved the efficiency of the system. This was especially so in consultations with children, the elderly, patients with psychosocial problems and those with chronic diseases.1
Studies of interest have also been carried out in the United States as part of an attempt to improve the health care provided via the publicly aided Medicaid system. One of the aims was to explore if improved continuity could influence the quality of clinical care. Evidence from a randomised controlled trial suggests that it does.3 This trial was carried out in an outpatient population of elderly men and showed that improved continuity of care almost halved the number of emergency admissions and shortened the length of hospitalisation. The patients in the continuity group perceived that the providers were more knowledgeable, thorough and interested in patient education.3 Other studies have demonstrated that there is a direct positive effect on actual clinical outcomes. For example, in a cohort of adults with a diagnosis of type II diabetes, patients with higher continuity scores had better HbA1c values and more positive changes to their diets.4
There are fewer studies in children, but improved continuity has been shown to be associated with a better uptake of routine health services such as immunisation and preventative services.5 Like adults, children with diabetes have been shown to have better diabetic control with fewer acute admissions for ketoacidosis and a better uptake of screening services such as retinal and endocrine testing.6 Significantly fewer emergency department visits are also seen in children with improved continuity.7
One review article discusses the views of general practitioners on continuity.8 It suggests that the main costs for clinicians when offering increased continuity are personal commitment and high personal availability. Doctors are caught between the conflicting pressures of patient's expectations and society's demands. To be asked for personally by a patient is more satisfying than seeing a succession of patients who just want a doctor. However, this needs to be balanced against many doctors opting away from a full‐time job for life. Seeing the same patients increases job satisfaction and education but requires high personal commitment. The article emphasises that continuity is important to patients in general practice, who give it as their third priority after a doctor who listens and a doctor who sorts out problems.
The evidence, therefore, indicates that continuity is valuable and important to doctors and patients. It not only enables us to have an improved relationship with our patients but also enables us to work more effectively and, most importantly, results in improved clinical outcomes. But our health care system is very different from Medicaid in the United States, where most of this work has been carried out to improve the health of individuals from lower social classes and ethnic minorities. Before we can assume that this evidence is relevant on our side of the Atlantic, we need to know whether we have (dis)continuity of care to the same extent here in the UK.
How much continuity is there in our paediatric services?
Before this question can be answered, a tool is needed to measure it. A number of indices have been developed, such as the Sequential Continuity Index (SECON)9 and the Usual Provider Continuity Index (UPC).9 One of the most useful is the Continuity of Care Index (COCI),9 which reflects the distribution of clinic visits between clinicians (see box 1). Values range from a score of 1 (maximum continuity) which is achieved when the same doctor is seen at each clinic visit to 0 (minimum continuity) when a different doctor is seen on each occasion. The COCI has been used to assess care received by children attending paediatric clinics in Seattle, USA.7 Researchers found that the mean COCI (SD) score for children seeing attendings (consultants) was 0.4 (0.32) and the score for residents (juniors) was 0.3 (0.32). Both are some distance from ideal continuity of care.
BOX 1: The Continuity of Care Index (COCI)
COCI reflects the distribution of clinic visits between providers (ie clinicians).
Index of Continuity of Care (COCI)12
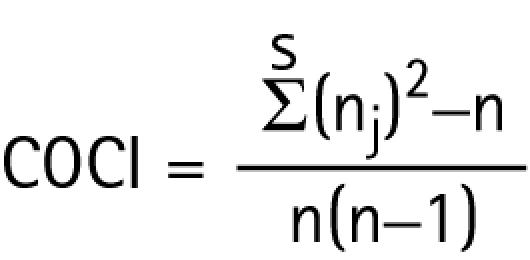 |
n = total number of visits by patient
nj = number of visits to provider j
s = total number of providers
Values range from:
1 = maximum continuity (seeing the same doctor at each clinic visit) to
0 = minimum continuity (never seeing the same doctor)
We were curious to see how the care of children in the UK compared and undertook a small survey10,11 of children attending outpatient clinics in the Leeds Teaching Hospital NHS Trust, which is a tertiary teaching centre. We chose six clinics that reflected both acute and chronic conditions, and reviewed the notes of 48 children who had attended on more than four occasions. We were interested to find that our figures were quite similar to those in the Seattle study.7 The mean COCI scores for the six clinics ranged from 0.13 to 0.41. Three of our patients had not seen the same doctor on any occasion and therefore had COCI scores of zero; 8.3% of the children had never seen their named consultant and only one patient had perfect continuity. While these results may not be typical of clinics elsewhere in the UK, they probably do reflect the difficulties of maintaining continuity within the present structure of the NHS, where changes in society and professional developments are squeezing out traditional continuity of care. Hopefully, continuity is better in district hospitals where there may be more staff employed on a permanent basis, and less trainees working.
What are paediatricians' and patients' views on the importance of continuity of care?
The literature indicates that continuity of care is important, but how is it perceived and valued by the principal players – consultants, junior doctors and the patients themselves? We have attempted to explore this issue by surveying paediatricians and patients attending paediatric clinics in Yorkshire.10,11 All 109 paediatric consultants were contacted, and a surprising 92% responded to our postal survey. This high response rate in itself suggested that continuity of care is an area of considerable interest. Ninety (83%) ranked continuity as one of their top three priorities when running an out‐patient clinic, a result that was greatly at variance with the levels of continuity we had found on notes review.
Patients and their families appear to have similar views to consultants. We asked a limited sample of parents and adolescents to complete a questionnaire while they were waiting to be seen in clinics in the Leeds Teaching Hospitals NHS Trust.10,11 All 19 were keen to take part, and more than half reported that they felt it was important to see the same doctor at each appointment. They did not necessarily want this to be the consultant, and indeed, only five thought it was important to see the consultant regularly. They commented that continuity helps build up trust and confidence in the doctor and that they were likely to be provided with more consistent advice. Continuity was certainly important for the three adolescents who all said they wanted to see the same doctor at clinic appointments. This may be of particular relevance given that compliance can be such a difficult issue in this age group. Their comments included: ”So the doctor and the patient have a bond”, ”trust him and he is nice” and ”because they know me”.
We went on to question junior doctors to see how their view of continuity of care compared with that of their senior colleagues. It seems that here there was a difference. Once again the response rate was high at 83%. However only 31 (49%) of the 64 who responded ranked continuity in their top three priorities for running a paediatric clinic. It is interesting to speculate why this may be so. We wonder whether one reason may be that they are not exposed to continuity in their training and so are not learning the value of a successful long‐term doctor–patient relationship. This problem is recognised in the United States and is being addressed through the introduction of continuity clinics where patients are allocated to each resident and seen throughout the period of their training. This allows doctors time to follow a patient over a number of years and to experience the benefits of a long‐term relationship.
Why is continuity of care so poor?
The evidence suggests that improving continuity brings benefits both in terms of clinical outcomes and cost effectiveness. Consultants and patients sense its importance and it could be argued that we should aim for 100% continuity for our patients. Yet it seems to occur in a very limited way in practice. There are a number of reasons why this may be so. Some reasons are structural and others relate to issues regarding training and the junior doctor's need for adequate exposure to a variety of patients and their problems.
There is no doubt that continuity is now being eroded by all the pressures on junior doctors' hours. The vast majority of junior doctors within paediatrics are now working a shift pattern, with time spent on night shifts as well as time off to recuperate. Their ability to attend a clinic regularly is compromised and they are not able to build up their own patient load alongside their supervising consultant. They are also being rotated through different posts regularly and so there is simply not the time to build up continuity within the clinics they attend.
Another issue that affects continuity of care occurs when consultants work together in joint specialty clinics. Patients may then be seen by anyone in the team without consideration for continuity. Clinicians probably argue that this allows for more diverse input into a particular case. Perhaps this needs to be better balanced against the benefits that increased personal continuity would provide. Input from other clinicians is important, but this could be gained by discussion of the case outside the clinic.
What can we do to improve continuity of care?
There are a number of ways that continuity of care could be improved. Forward planning would help, particularly around shift rotas and annual leave. When there are several doctors involved in a clinic, individual clinic lists can avoid patients seeing a different member of the team each time they visit. This means making an effort to organise the lists, rather than relying on a clinic clerk to randomly allocate patients or doctors simply picking up the notes of the next patient who arrives in the clinic.
More efforts such as these can be made to increase continuity, but in a teaching hospital continuity is never going to be perfect. We need to ensure that better communication underpins the way we work in the clinic. Setting aside time for pre‐ or post‐clinic meetings can help. This allows for brief discussion of cases, which may pre‐empt problems and allow for smoother and shorter appointments. In the United States, residents are often required to review and summarise patients' notes in advance of a clinic so a plan is made before the patient arrives. Less precious clinic time is then spent reading through notes, thus allowing better quality time with the patient. While many consultants hold meetings after the clinic to ensure that the team knows what has occurred during the appointment, patients are generally unaware of this. It might help to let patients know that this occurs. When they see a doctor they have not met before, they would then know that the consultant would be aware of their progress and that the doctor they are seeing knows their previous history.
Abbreviations
COCI - Continuity of Care Index
SECON - Sequential Continuity Index
UPC - Usual Provider Continuity Index
Footnotes
Competing interests: None.
References
- 1.Hjortdahl P, Borcchgrevink C F. Continuity of care: influence of general practitioners' knowledge about their patients on use of resources in consultations. BMJ 19913031181–1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hjortdahl P, Laerum E. Continuity of care in general practice: effect on patient satisfaction. BMJ 19923041287–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wasson J H, Sauvigne A E, Mogielnicki P.et al Continuity of outpatient medical care in elderly men. JAMA 19842522413–2417. [PubMed] [Google Scholar]
- 4.Parchman M L, Pugh J A, Noel P H.et al Continuity of care, self‐management behaviours, and glucose control in patients with type 2 diabetes. Med Care 200240137–144. [DOI] [PubMed] [Google Scholar]
- 5.O'Malley A S, Forrest C B. Continuity of care and delivery of ambulatory services to children in community health clinics. J Community Health 199621159–174. [DOI] [PubMed] [Google Scholar]
- 6.Christakis D A, Feudtner C, Pihoker C.et al Continuity and quality of care for children with diabetes who are covered by Medicaid. Ambul Pediatr 2001199–103. [DOI] [PubMed] [Google Scholar]
- 7.Christakis D A, Mell L, Koepsell T D.et al Association of lower continuity of care with greater risk of emergency department use and hospitalisation in children. Pediatrics 2001103524–529. [DOI] [PubMed] [Google Scholar]
- 8.Freeman G, Hjortdahl P. What future for continuity of care in general practice? BMJ 19973141870–1873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eriksson E A, Mattsson L. Quantitative measurement of continuity of care. Med Care 198321(9)858–875. [DOI] [PubMed] [Google Scholar]
- 10.Sudhakar‐Krishnan V. How important is continuity of care to paediatricians and their patients? MMedSci dissertation. University of Leeds 2005
- 11.Sudhakar‐Krishnan V, Rudolf M. How important is continuity of care to paediatricians and their patients? Arch Dis Child 2006A76G199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bice T W, Boxerman S B. A quantitative measure of continuity of care. Med Care 197715(4)347–349. [DOI] [PubMed] [Google Scholar]


