Abstract
Background
Population monitoring has been introduced in UK primary schools in an effort to track the growing obesity epidemic. It has been argued that parents should be informed of their child's results, but is there evidence that moving from monitoring to screening would be effective? We describe what is known about the effectiveness of monitoring and screening for overweight and obesity in primary school children and highlight areas where evidence is lacking and research should be prioritised.
Design
Systematic review with discussion of evidence gaps and future research.
Data sources
Published and unpublished studies (any language) from electronic databases (inception to July 2005), clinical experts, Primary Care Trusts and Strategic Health Authorities, and reference lists of retrieved studies.
Review methods
We included any study that evaluated measures of overweight and obesity as part of a population‐level assessment and excluded studies whose primary outcome measure was prevalence.
Results
There were no trials assessing the effectiveness of monitoring or screening for overweight and obesity. Studies focussed on the diagnostic accuracy of measurements. Information on the attitudes of children, parents and health professionals to monitoring was extremely sparse.
Conclusions
Our review found a lack of data on the potential impact of population monitoring or screening for obesity and more research is indicated. Identification of effective weight reduction strategies for children and clarification of the role of preventative measures are priorities. It is difficult to see how screening to identify individual children can be justified without effective interventions.
Keywords: obesity, overweight, monitoring, screening, BMI
In an effort to accurately map the growing epidemic of childhood obesity (the proportion of overweight or obese children between the ages of 2 and 10 rose from 22.7% in 1995 to 27.7% in 20031), the UK government has recently introduced population monitoring in primary schools. A nationally co‐ordinated population monitoring programme has benefits in terms of facilitating the gathering of epidemiological data. It is also a potentially useful tool for assessing the impact of health promotion programmes such as the School Fruit and Vegetable Scheme and the National Healthy Schools Programme upon prevalence of overweight and obesity (although it cannot establish a causal relationship). Current evidence suggests that preventative strategies for children can change behaviour, increasing levels of physical activity and encouraging a healthier diet, but little is known of their long‐term efficacy in reducing the prevalence of obesity.2
The UK House of Commons Health Committee report on obesity expressed particular concerns about the long‐term health consequences of obesity in children,3 and a government target has been set to halt its increase by 2010.4 The report recommended that “results should be sent home in confidence to parents, together with, where appropriate, advice on lifestyle, follow‐up, and referral to more specialised services”. This approach remains controversial. Pressure to move from population monitoring to identifying overweight and obese individuals is driven by the notion that highlighting the problem and intervening early could improve long‐term health outcomes.5 There is currently little evidence that weight reduction interventions are effective,6 and without this evidence any move towards identifying individual children appears difficult to justify. An additional difficulty arises as the limited evidence about effective interventions is derived from studies in motivated, often self‐referred populations, and caution must be exercised in extrapolating the results to a screening scenario. Current Department of Health guidance for Primary Care Trusts (PCTs)7 on measuring body mass index (BMI) in primary school children emphasises population monitoring and discourages the use of measurement to identify individual children with weight problems until such time as evidence becomes available to support the effectiveness of doing so. It is worth noting that little is known about the potential harms of monitoring overweight and obesity, either in the context of population monitoring or screening to identify individual children.
We were commissioned by the Health Technology Assessment Programme to produce a systematic review of the clinical and cost‐effectiveness of growth monitoring in children of primary school age to identify growth‐related conditions. In consideration of the rise in childhood obesity within this age range and the national debate currently being conducted in the media, we included monitoring for overweight and obesity in our assessment. This article reports our findings in relation to the clinical effectiveness of monitoring for overweight and obesity, and describes those areas where evidence is lacking and where research should be prioritised.
Methods
The systematic review was undertaken in accordance with published guidelines.8 Two reviewers screened studies for relevance independently, and full texts of studies deemed potentially relevant were ordered and assessed for inclusion by one reviewer and checked by a second. Data extraction and quality assessment were carried out using standard forms, developed and piloted a priori; data were extracted by one reviewer and checked by a second. At all stages, disagreements were resolved by consensus or consultation with a third reviewer.
All study designs (except case reports) were included. For relevance to the UK population, studies had to include children aged between 4 and 11 years in Western Europe, North America or Australia/New Zealand (excluding studies of aboriginal populations). Studies had to measure indices of overweight and obesity as part of a population‐level assessment of children's health. Accepted outcome measures were:
the effects on management and outcome (including specialist referrals),
indices of diagnostic accuracy (sensitivity and specificity) in comparison with direct measures of body fat,
any measure of the attitudes to monitoring (including surrogate measures such as uptake rate),
any measure of the human resource implications of introducing monitoring.
We did not include studies whose primary outcome measure was population prevalence, as this is already well established.
The full search strategy is available from the authors on request. Databases searched are listed in supplemental table 1 (available from http://adc.bmj.com/supplemental); no language restrictions were applied. Unpublished information on current practice and audit data were sought by directly contacting all PCT lead personnel in child health/community paediatrics and all Strategic Health Authority lead personnel in child health services in England and Wales.
The methodological quality of diagnostic accuracy studies was assessed using the QUADAS tool9,10 with appropriate review‐specific modifications.
Data are summarised in a narrative, and we present a summary of the available evidence against the National Screening Committee (NSC) criteria, along with a discussion of directions for future research.
Table 1 Overview of all diagnostic accuracy studies identified.
| Study details | Selection procedure | No. weighed (% of approached) | No. males (%) and ethnicity | Weighed age(s) |
|---|---|---|---|---|
| Bedogni (2003)11 | A convenience sample of children enrolled in primary and | 986 (not | 486 (49%) | 8–12 years |
| Italy | secondary schools in Modena and Parma. Year of data | reported) | ||
| collection not reported. | ||||
| Ebbeling (1999)12 | Information on children was obtained from data tapes from | 1171 (not | 585 (50%) | 6–9 years |
| USA | the NHANESII study which was carried out in 1976–1980. | reported) | ||
| Ellis (1999)13 | Selection procedure was not explicitly stated; children were | 979 (not | 406 (41%) | 3–18 years |
| USA | living in Houston, Texas. Data were collected in 1994–1996. | reported) | African American (Black) 283 | |
| European American (White) 438 | ||||
| Hispanic American (Hispanic) 258 | ||||
| Himes (1989)14 | Families in Quebec City volunteered to participate in response | 316 (not | 159 (50%) | 8–18 years |
| USA | to media notices. Year of data collection not reported. | reported) | ||
| Lazarus (1996)15 | Volunteers recruited from among siblings of outpatients | 230 (not | 119 (52%) | 4–20 years |
| Australia | or children of staff and friends at The Children's | reported) | ||
| Hospital, Sydney. Year of data collection not reported. | ||||
| Marshall (1991)16 | Children from Alberta who participated in the Canada | 540 (90%) | 266 (49%) | 7–14 years |
| Canada | fitness survey in 1981 were selected using a two‐stage | |||
| stratified sampling frame. | ||||
| Mast (2002)17 | Random sample (40%) of children in 29/32 schools in Kiel | 2286 (not | 1146 (50%) | 5–7 years |
| Germany | in 1996–1999. | reported) | ||
| Reilly (1999)18 | Unclear, though it was stated that they were representative | 240 (not | 124 (52%) | 8 years |
| UK | of Scottish children (based in Edinburgh). Year of data | reported) | ||
| collection not reported. | ||||
| Reilly (2000)19 | 4175 of approx 14 000 children in the Avon Longitudinal | 3948 (95%) | 2010 (51%) | 7 years |
| UK | Study of Pregnancy and Childhood (ALSPAC) in 1998. The | |||
| sample was representative of the birth cohort and UK, | ||||
| although slightly over‐representative of wealthier families | ||||
| and under‐representative of ethnic minorities. | ||||
| Schaefer (1998)20 | Representative sample (19%) of the population in the area of | 2554 (not | 1276 (50%) | 6–19 years |
| Germany | Heidelberg in 1989/1990. | reported) | ||
| Wickramasinghe | Not explicitly reported. The authors stated that subjects were | 138 (not | 71 (51%) | 5–15 years |
| (2005)21 | contacted via newsletters and community centres in Brisbane. | reported) | Australian Sri Lankan 42 | |
| Australia | Year of data collection not reported. | Australian White Caucasian 96 |
Results
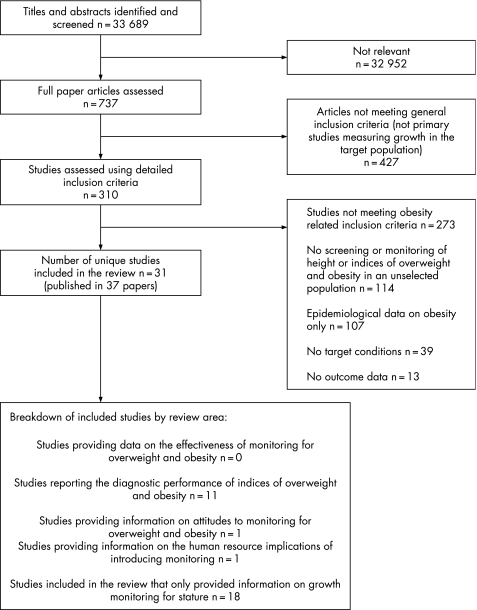
Figure 1 shows the flow of studies through the review process (including studies of growth monitoring to identify stature‐related conditions). Despite searching a wide range of sources using a search strategy optimised for sensitivity (over 30 000 records were retrieved and screened), we identified only a small number of relevant studies. It is significant that no study addressed, either directly or indirectly, the effectiveness of either population‐level monitoring or screening to identify and treat individual children.
Figure 1 Flow chart of studies through the review process (including studies of growth monitoring to identify stature‐related conditions). This study focuses on the areas covered by the studies reporting the diagnostic performance of indices of overweight and obesity, providing information on attitudes to monitoring for overweight and obesity and providing information on the human resource implications of introducing monitoring.
Diagnostic accuracy studies
Eleven studies provided data on the diagnostic accuracy of measures used to identify overweight and obesity in comparison with direct measurement of body fat.11,12,13,14,15,16,17,18,19,20,21 Studies varied widely in their sample size, country of origin, and the age or ages at which children were measured. An overview of the studies is presented in table 1. Reasoning that any monitoring programme would need to access simple measuring techniques, we have focussed on those studies13,14,15,16,21 that assessed BMI, weight or skinfold measures in comparison with the accepted reference standards for determining percentage body fat (x ray densitometry, hydrostatic weighing or isotope dilution).
BMI was the predominant measure of overweight and obesity evaluated. Thresholds used to define overweight and obesity varied between studies and were derived either internally from the study population, from national or other published data, or from International Obesity Taskforce (IOTF) definitions. Full details of the methods of measurement assessed and the reference standards used are presented in table 2. A number of the studies appeared to have been conducted with the aim of establishing the optimum simple measurement method for determining overweight and obesity; that is, they compared a number of different measurements or thresholds with one or more thresholds for directly measured body fat. Heterogeneity between the studies precludes any generalisations about what might be the optimum simple measure of overweight and obesity; the results of individual studies are presented in table 2.
Table 2 Results of the five diagnostic accuracy studies that assessed BMI, weight or skinfold measures in comparison with an accepted reference standard for determining percentage body fat.
| Study details, sample | Reference standard | Index measure | TP | FN | FP | TN | Sensitivity (95% CI) | Specificity (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Ellis (1999)13 | ||||||||
| Boys | BF (DXA) >85th C (I) | BMI >85th C (I) | 55 | 6 | 57 | 288 | 0.90 (0.80 to 0.95) | 0.83 (0.79 to 0.87) |
| BF (DXA) >95th C (I) | BMI >95th C (I) | 15 | 6 | 35 | 350 | 0.71 (0.50 to 0.86) | 0.91 (0.88 to 0.93) | |
| Girls | BF (DXA) >85th C (I) | BMI >85th C (I) | 81 | 5 | 85 | 402 | 0.94 (0.87 to 0.97) | 0.83 (0.79 to 0.86) |
| BF (DXA) >95th C (I) | BMI >95th C (I) | 26 | 3 | 42 | 502 | 0.90 (0.74 to 0.96) | 0.92 (0.90 to 0.94) | |
| Himes (1989)14 | ||||||||
| Boys | %BF (DXA) ⩾90th C (E) | BMI >85th C (E) | 6 | 15 | 1 | 137 | 0.29 (0.14 to 0.50) | 0.99 (0.96 to 1.00) |
| %BF from 4SF ⩾85th C (E) | 12 | 9 | 21 | 117 | 0.57 (0.37 to 0.76) | 0.85 (0.78 to 0.90) | ||
| SSF ⩾85th C (E) | 8 | 13 | 1 | 137 | 0.38 (0.21 to 0.59) | 0.99 (0.96 to 1.00) | ||
| TSF ⩾85th C (E) | 5 | 16 | 0 | 138 | 0.24 (0.11 to 0.45) | 1.00 (0.97 to 1.00) | ||
| Weight ⩾85th C (E) | 9 | 12 | 7 | 131 | 0.43 (0.24 to 0.63) | 0.95 (0.90 to 0.98) | ||
| Girls | BMI >85th C (E) | 7 | 23 | 0 | 127 | 0.23 (0.12 to 0.41) | 1.00 (0.97 to 1.00) | |
| %BF from 4SF ⩾85th C (E) | 24 | 6 | 23 | 104 | 0.80 (0.63 to 0.90) | 0.82 (0.74 to 0.88) | ||
| SSF ⩾85th C (E) | 9 | 21 | 1 | 126 | 0.30 (0.17 to 0.48) | 0.99 (0.96 to 1.00) | ||
| TSF ⩾85th C (E) | 7 | 23 | 4 | 123 | 0.23 (0.12 to 0.41) | 0.97 (0.92 to 0.99) | ||
| Weight ⩾85th C (E) | 5 | 25 | 3 | 124 | 0.17 (0.07 to 0.34) | 0.98 (0.93 to 0.99) | ||
| Lazarus (1996)15 | ||||||||
| All | %BF (DXA) ⩾85th C (I) | BMI ⩾85th C (I) | 24 | 10 | 10 | 186 | 0.71 (0.54 to 0.83) | 0.95 (0.91 to 0.97) |
| BMI ⩾90th C (I) | 21 | 13 | 2 | 194 | 0.62 (0.45 to 0.76) | 0.99 (0.96 to 1.00) | ||
| BMI ⩾95th C (I) | 10 | 24 | 2 | 194 | 0.29 (0.17 to 0.46) | 0.99 (0.96 to 1.00) | ||
| Boys | BMI ⩾85th C (I) | 12 | 6 | 6 | 95 | 0.67 (0.44 to 0.84) | 0.94 (0.88 to 0.97) | |
| BMI ⩾90th C (I) | 11 | 7 | 1 | 100 | 0.61 (0.39 to 0.80) | 0.99 (0.95 to 1.00) | ||
| BMI ⩾95th C (I) | 5 | 13 | 1 | 100 | 0.28 (0.12 to 0.51) | 0.99 (0.95 to 1.00) | ||
| Girls | BMI ⩾85th C (I) | 12 | 4 | 4 | 91 | 0.75 (0.51 to 0.90) | 0.96 (0.90 to 0.98) | |
| BMI ⩾90th C (I) | 10 | 6 | 1 | 94 | 0.63 (0.39 to 0.82) | 0.99 (0.94 to 1.00) | ||
| BMI ⩾95th C (I) | 5 | 11 | 0 | 95 | 0.31 (0.14 to 0.56) | 1.00 (0.96 to 1.00) | ||
| Marshall (1991)16 | ||||||||
| Boys | BF (HW) ⩾20% | 5SF ⩾85th C (E) | 36 | 9 | 23 | 198 | 0.80 (0.66 to 0.89) | 0.90 (0.85 to 0.93) |
| Relative BMI ⩾120% (E) | 31 | 14 | 16 | 205 | 0.69 (0.54 to 0.80) | 0.93 (0.89 to 0.95) | ||
| Relative weight ⩾120% (E) | 22 | 23 | 11 | 210 | 0.49 (0.35 to 0.63) | 0.95 (0.91 to 0.97) | ||
| TSF ⩾85th C (I) | 29 | 16 | 12 | 209 | 0.64 (0.50 to 0.77) | 0.95 (0.91 to 0.97) | ||
| Girls | BF (HW) ⩾25% | 5SF ⩾85th C (E) | 30 | 1 | 23 | 220 | 0.97 (0.84 to 0.99) | 0.91 (0.86 to 0.94) |
| Relative BMI ⩾120% (E) | 23 | 8 | 21 | 222 | 0.74 (0.57 to 0.86) | 0.91 (0.87 to 0.94) | ||
| Relative weight ⩾120% (E) | 18 | 13 | 12 | 231 | 0.58 (0.41 to 0.74) | 0.95 (0.92 to 0.97) | ||
| TSF ⩾85th C (I) | 21 | 10 | 16 | 227 | 0.68 (0.50 to 0.81) | 0.93 (0.90 to 0.96) | ||
| BMI >90th C I) | 93 | 35 | 170 | 2256 | 0.73 (0.64 to 0.80) | 0.93 (0.92 to 0.94) | ||
| BMI >95th C (I) | 70 | 58 | 73 | 2353 | 0.55 (0.46 to 0.63) | 0.97 (0.96 to 0.98) | ||
| Wickramasinghe (2005)21 | ||||||||
| Boys | BF (ID) >20% | BMI SDS >2 (E) | 2 | 27 | 1 | 14 | 0.07 (0.02 to 0.22) | 0.93 (0.70 to 0.99) |
| BMI >95th C (E) | 1 | 28 | 0 | 15 | 0.03 (0.01 to 0.17) | 1.00 (0.80 to 1.00) | ||
| BMI IOTF “obese” | 0 | 29 | 0 | 15 | 0.00 (0.00 to 0.12) | 1.00 (0.80 to 1.00) | ||
| Girls | BF (ID) >30% | BMI SDS >2 (E) | 1 | 18 | 0 | 33 | 0.05 (0.01 to 0.25) | 1.00 (0.90 to 1.00) |
| BMI >95th C (E) | 4 | 15 | 0 | 33 | 0.21 (0.09 to 0.43) | 1.00 (0.90 to 1.00) | ||
| BMI IOTF “obese” | 0 | 19 | 0 | 33 | 0.00 (0.00 to 0.17) | 1.00 (0.90 to 1.00) | ||
BF, body fat; BIA, bioelectrical impedance analysis; BMI, body mass index; C, centile; DXA, x ray densitometry; (E), derived from external reference data; FN, false negative; FP, false positive; HW, hydrostatic weighing; (I), derived internally from study population; IBW, ideal body weight; ID, isotope dilution; IOTF, International Obesity Taskforce; SF, skinfold; SSF, scapular skinfold; TN, true negative; TP, true positive; TSF, triceps skinfold; WH, weight for height.
None of the five studies clearly met all of the 12 QUADAS criteria. The quality assessment was limited by the poor reporting of a number of studies. The index measures and reference standards were generally well reported, with all but one study giving sufficient details to allow replication.13,15,16,21 The results of methodological quality assessment are presented in supplemental table 2 (available from http://adc.bmj.com/supplemental).
Human resource implications of monitoring
One study included information relevant to the human resource requirements of monitoring.22 This study considered general health examinations conducted at or around the time of school entry. It compared the ability of physicians with that of trained volunteers (teachers) and public health nurses to detect abnormalities in height, weight, vision, hearing, blood pressure and dental caries. No significant differences were observed.
Attitudes to monitoring
One study assessed attitudes to monitoring overweight and obesity.23 The study aimed to gather baseline BMI data in order to identify a low cost method of detecting obesity that would be acceptable to schools. A total of 252 children aged 9–10 years participated in the one‐off measurement. There were three (1.2%) refusals to participate; parental consent was obtained on an opt‐out basis. The study was conducted in the context of a lesson on measurement and was designed to minimise negative impacts. The results of a questionnaire, sent to teachers and school nurses, suggested general satisfaction. It should be noted, however, that this was a small study, using an approach that had been conceived with a view to minimising negative impacts. Further, no attempt to elicit the views of the participating children was reported.
Assessment against National Screening Committee criteria
An assessment of monitoring to identify childhood overweight and obesity is presented against the NSC criteria in table 3. Deficiencies and uncertainties in the evidence mean that monitoring which aims to identify and treat individuals does not currently meet the majority of the criteria.
Table 3 Assessment of monitoring to identify childhood overweight and obesity against the National Screening Committee (NSC) criteria.
| NSC criteria | Summary of the evidence | Authors' summary opinion |
|---|---|---|
| The condition | ||
| The condition should be an important health problem. | Childhood obesity is an important health problem with the UK prevalence at | Fully satisfied |
| 27.7% and significant co‐morbidities.5,24,25 It is linked to continued obesity | ||
| and morbidity and mortality in adulthood.5 | ||
| The epidemiology and natural history of the condition, | Childhood obesity has been linked to societal changes relating to nutrition | Partially satisfied |
| including development from latent to declared disease, | and a sedentary lifestyle.24 There is evidence of persistence into adulthood, | |
| should be adequately understood and there should be | but evidence on thresholds of BMI that link with later morbidity is limited. | |
| a detectable risk factor or disease marker, and a latent | ||
| period or early symptomatic stage. | ||
| All cost‐effective primary prevention strategies should | Primary prevention is promising, cost‐effectiveness is currently unproven and | Not satisfied ‐ |
| have been implemented as far as practicably possible. | larger trials are urgently needed. It is impossible to determine if all cost‐effective | insufficient data |
| primary prevention strategies have been implemented. | ||
| The test | ||
| There should be a simple, safe, precise and validated | Ascertainment of weight and calculation of BMI is safe and simple, but BMI is a | Partially satisfied |
| screening test. | poor predictor of obesity compared with densitometrically defined measures of | |
| fat mass and evidence on thresholds of BMI that link with later morbidity is limited. | ||
| The distribution of test values in the target population should | Thresholds for obesity are arbitrarily defined. More research is needed to | Not satisfied ‐ |
| be known and a suitable cut‐off level defined and agreed. | determine a threshold for referral based on morbidity. | insufficient data |
| The test should be acceptable to the population. | Weight can be measured in a sensitive and acceptable way,23 but careful | Not satisfied ‐ |
| consideration would need to be given to any screening of weight to identify | insufficient data | |
| obese children; data on the acceptability to the population of measurement, | ||
| either for population monitoring or to identify individual children, are notably | ||
| lacking. There may be variation in refusal rates and acceptability according to | ||
| age, ethnicity and gender. | ||
| There should be an agreed policy on the further diagnostic | There is no agreed policy regarding investigation of identified obese children | Not satisfied |
| investigation of individuals with a positive test | for morbidity. There are no evidence based treatments currently available. | |
| result and on the choices available to these individuals. | ||
| The treatment | ||
| There should be an effective treatment or intervention for | There is a currently a lack of proven long‐term effective treatment for obesity.6 | Not satisfied |
| patients identified through early detection, with evidence | ||
| of early treatment leading to better outcomes than late | ||
| treatment. | ||
| There should be agreed evidence based policies covering | There is no consensus on when to refer or which treatments might be most | Not satisfied |
| which individuals should be offered treatment and the | beneficial, and the appropriate treatment is unclear. | |
| appropriate treatment to be offered. | ||
| Clinical management of the condition and patient outcomes | No clear clinical management pathways exist for children identified as being | Not satisfied |
| should be optimised by all health care providers | overweight or obese. Guidance from the National Institute for Clinical | |
| prior to participation in a screening programme. | Excellence (NICE) is due to be published in November 2006. | |
| The screening programme | ||
| There must be evidence from high quality randomised | There are no randomised controlled trials comparing screening with not | Not satisfied ‐ |
| controlled trials that the screening programme | screening for obesity. | insufficient |
| is effective in reducing mortality and morbidity. | data | |
| There should be evidence that the complete | There is no strong evidence on the attitudes of health professionals, children and | Not satisfied ‐ |
| screening programme (test, diagnostic procedures, | parents to screening to detect obesity. | insufficient |
| treatment/intervention) is clinically, socially and ethically | data | |
| acceptable to health professionals and the public. | ||
| The benefit from the screening programme should | The review did not locate any studies describing the relative benefits/harms of | Not satisfied ‐ |
| outweigh the physical and psychological harm. | screening for obesity. Taken in conjunction with a measure (BMI) that is likely to | insufficient |
| generate false positives, the balance of benefits and harms is unknown. The | data | |
| potential harms of labelling children as obese should be set against the current | ||
| lack of effective long‐term treatments. | ||
| The opportunity cost of the screening programme | There is some evidence that primary prevention may be a cost‐effective approach | Not satisfied ‐ |
| should be economically balanced in relation to | to managing obesity in the population. There is a great deal of uncertainty | insufficient |
| expenditure on medical care as a whole. | regarding monitoring and treating obesity, and further research is needed. | data |
| There should be a plan for managing and monitoring | A plan and associated standards would need to be developed. | Not satisfied |
| the screening programme and an agreed set of | ||
| quality assurance standards. | ||
| Adequate staffing and facilities for testing, diagnosis, | Given uncertainties about the definition of obesity and appropriate treatments, | Not satisfied |
| treatment and programme management should be made | the requirements in terms of staff and facilities are unclear. | |
| available prior to the commencement of the screening | ||
| programme. | ||
| All other options for managing the condition should | Further research on methods of preventing obesity and the cost‐effectiveness | Not satisfied |
| have been considered (eg, improving treatment, | of various methods remains to be investigated. | |
| providing other services) to ensure that no more cost | ||
| effective intervention could be introduced or current | ||
| interventions increased within the resources available. | ||
| Evidence based information, explaining the | The effect of providing information about monitoring for obesity has not been | Not satisfied |
| consequences of testing, investigation and treatment, | investigated. | |
| should be made available to potential participants to | ||
| assist them in making an informed choice. | ||
| Public pressure for widening the eligibility criteria | There is no strong evidence comparing screening intervals or thresholds. | Not satisfied |
| for reducing the screening interval, and for increasing | ||
| the sensitivity of the testing process, should be | ||
| anticipated. Decisions about these parameters | ||
| should be scientifically justifiable to the public. | ||
Discussion
Statement of principal findings
It is clear that monitoring to detect and treat individual overweight and obese children does not currently meet the NSC criteria. Although childhood obesity is an important public health issue with increasing prevalence and important consequences (co‐morbidities of obesity in childhood include type 2 diabetes, hypertension, dyslipidaemia, emotional and behavioural problems, asthma and sleep apnoea),24,25,26 uncertainties concerning its definition and appropriate treatment mean that most of the screening criteria have not been met. There remains, however, a fundamental question as to whether or not the NSC criteria are a valid tool for assessing general health monitoring programmes such as monitoring overweight and obesity or monitoring children's growth. Abnormalities of stature or weight are not, in themselves, disease states and therefore, arguably, monitoring children's health with respect to these parameters should not be considered a screening exercise. Nonetheless, a rigorous approach to clarifying harms and benefits is required.
Despite its failure to meet the NSC criteria, monitoring levels of childhood overweight and obesity in the population may have inherent informative value. The importance of consistent data gathering and the availability of local data to inform planning and resource targeting are recognised in Department of Health guidance to PCTs,7 although it should be noted that population data cannot provide evidence of the effectiveness of resource targeting. If data gathered in monitoring programmes could be linked to individuals, it might also prove useful in clarifying the risk relationship between childhood BMI and long‐term morbidity and mortality into adulthood. However, the value of moving from population monitoring to screening to identify and treat individual children remains, at best, questionable; it is fundamentally dependent on benefits outweighing harms. The effectiveness of treatment is currently doubtful and the potential harms of either monitoring or screening are poorly researched. In the light of this, current models of self‐referral appear the best basis for attempts to treat obesity and should continue. The use of the population monitoring programme to identify individual children and provide information to parents and carers, as recommended in the UK House of Commons Heath Committee report on obesity,3 would represent a move towards screening that would be difficult to justify on the basis of current evidence.
Strengths and weaknesses of the study
Our review provides the first systematic evaluation of the available data on monitoring for overweight and obesity in children. The strengths of the study lie in its use of rigorous systematic review methodology to address an important aspect of child health. The review included a comprehensive search strategy and extensive attempts to obtain unpublished studies, but was unable to provide definitive information on the value of monitoring childhood overweight and obesity for a number of reasons. Firstly, and perhaps most significantly, no controlled studies were found evaluating monitoring versus no monitoring for the detection and treatment of overweight and obesity. Secondly, although 11 studies providing data on the diagnostic accuracy of measurement techniques were identified, these studies had a number of methodological limitations. More importantly, these studies are more informative on the limitations of BMI (and other measures) as indicators of overweight and obesity in one‐off comparisons with direct measures of body fat than on the more important question of whether monitoring for overweight and obesity using BMI (or any alternative surrogate measure of body fat) can provide a useful predictor of long‐term morbidity and mortality, or is a useful exercise when compared with no monitoring. The limitations of BMI as a one‐off screening tool are clear but are not of direct relevance to the utility of long‐term monitoring.
Only very limited data were available on the human resource implications of monitoring growth and/or overweight and obesity, although a number of important issues concerning training, costs and referral were identified.
The potential harms which may arise from labelling children as overweight or obese, or from raised personal and peer group awareness generated by population monitoring without identification, are an important and understudied area. We identified just one study that specifically assessed attitudes to monitoring and this was conducted in a context expressly designed to minimise negative impact.23
Meaning of the study: implications for policy makers
The relative benefits and harms of monitoring have not been determined and the effectiveness of current treatments is doubtful. Given these and other uncertainties, a move from population monitoring towards screening to identify and treat individual overweight and obese children could not currently be justified under the NSC criteria. A consistent approach to population level monitoring and the collection of local data is likely to be useful in providing epidemiological data and guiding planning and resource allocation for preventative and general health promotion strategies, but cannot be used to reliably determine the effectiveness of such strategies. Policy makers also need to consider the extent to which it is appropriate to evaluate general health monitoring programmes against the NSC criteria.
Current Department of Health guidance to PCTs7 focuses on population monitoring and discourages the giving out of BMI results to parents and carers or children. Involvement in healthy schools programmes is encouraged and it has been suggested that this may be a route for providing feedback to parents27; providing “whole school” information, on a regular basis, in the context of the healthy schools programme could increase awareness without moving from monitoring to screening and the identification of individual children. However, the potential harms of stigmatisation arising from raised peer group awareness remain a consideration.
Unanswered questions and future research
Funding for UK research into the relative benefits and harms of using monitoring to identify and treat overweight and obesity in childhood should be of a high priority before any move away from population monitoring and towards screening is considered. Particular emphasis should be given to randomised controlled trials to identify effective weight reduction strategies for children. Research should measure long‐term outcomes (sustained weight loss, co‐morbidities and mortality into adulthood). Evidence that an effective intervention can be offered is a prerequisite to the introduction of screening.
Preventative strategies are promising in terms of effectiveness2 and attractive to policy makers and the general public, but they are currently unproven and larger and longer‐term trials are urgently needed. The generation of reliable, local prevalence data from population monitoring may help in targeting preventative strategies and evaluating their impact. The impact of effective prevention strategies on the need to use monitoring to identify and treat individual children should also be considered.
Current knowledge of the long‐term medical consequences of childhood obesity is limited. Establishing long‐term epidemiological studies is now a high priority. These should help elucidate which children are most at risk of obesity persisting into adulthood and consequent adverse outcomes. Such studies could utilise data from population monitoring programmes if these data were collected in a manner which could be linked to individuals. This would clarify the role of parameters such as BMI, which can be monitored in community settings, in determining those children most at risk.
What is already known on this topic
Childhood obesity is an important and growing health problem in the UK.
Obesity in children can have significant consequences for health and well‐being in the short term and into adulthood.
The effectiveness of interventions to treat childhood obesity remains doubtful, to date. Preventative strategies can change behaviour and promote healthier lifestyles, but their long‐term impact is unknown.
What this study adds
Funding for UK research into effective interventions to treat overweight and obese children is a high priority; it is difficult to justify measures to identify individual children without evidence of effective interventions.
Primary prevention offers a promising approach to tackling childhood obesity, but is currently unproven.
More large scale, well designed studies are urgently needed in this area. If effective treatments can be identified, effort should be focused upon methods of identifying overweight and obese children without stigmatisation and upon defining the appropriate target population.
Conclusions
Our review found a lack of data on the potential impact of monitoring for overweight and obesity in children; more research is indicated. Identification of effective weight reduction strategies for children and clarification of the role of preventative measures are priorities. Long‐term studies of the predictors of obesity‐related co‐morbidities in adulthood are warranted. This would clarify the role of parameters such as BMI in determining those children most at risk.
Supplementary Material
Abbreviations
BMI - body mass index
IOTF - International Obesity Taskforce
NSC - National Screening Committee
PCT - Primary Care Trust
Footnotes
This project was funded by the NIHR Health Technology Assessment Programme (project number 04/09/02) and will be published in full in Health Technology Assessment. See the HTA Programme website for further project information (http://www.hta.nhsweb.nhs.uk/).
Competing interests: None.
Ethics approval: Not required.
The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the Department of Health.
References
- 1.Jotangia D, Moody A, Stamatakis E.et alObesity among children under 11. London: Joint Health Surveys Unit, National Centre for Social Research, 2005, Available from http://www.dh.gov.uk/PublicationsAndStatistics/ (accessed 5 March 2007)
- 2.Summerbell C D, Waters E, Edmunds L D.et al Interventions for preventing obesity in children. In: Cochrane Library, Issue 3. Chichester: John Wiley, 2005 [DOI] [PubMed]
- 3.House of Commons Health Committee Obesity: third report of session 2003–04. London: Stationery Office, 2004, Available from http://www.publications.parliament.uk/pa/cm200304/cmselect/cmhealth/cmhealth.htm (accessed 5 March 2007)
- 4.Department of Health Children and young people: starting on the right path. In: Choosing health:making healthy choices easier. London: Stationery Office, 200440–75.
- 5.Reilly J J, Methven E, McDowell Z C.et al Health consequences of obesity. Arch Dis Child 200388748–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Summerbell C D, Ashton V, Campbell K J.et al Interventions for treating obesity in children. In: The Cochrane Library, Issue 3. Chichester: John Wiley, 2005 [DOI] [PubMed]
- 7.Department of Health Measuring childhood obesity: guidance to Primary Care Trusts. London: Department of Health, 2006, Available from http://www.dh.gov.uk/PublicationsAndStatistics/ (accessed 5 March 2007)
- 8.NHS Centre for Reviews and Dissemination Undertaking systematic reviews of research on effectiveness: CRD's guidance for those carrying out or commissioning reviews. 2nd ed. York: NHS Centre for Reviews and Dissemination, 2001
- 9.Whiting P, Rutjes A W S, Reitsma J B.et al The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 2003325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whiting P, Westwood M, Rutjes A W S.et al Evaluation of QUADAS, a tool for the quality assessment of diagnostic accuracy studies. BMC Med Res Methodol 200669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bedogni G, Iughetti L, Ferrari M.et al Sensitivity and specificity of body mass index and skinfold thicknesses in detecting excess adiposity in children aged 8–12 years. Ann Hum Biol 200330132–139. [DOI] [PubMed] [Google Scholar]
- 12.Ebbeling C B, Backstrand J R, Rodriguez N R. Screening indices for pediatric obesity. Nutr Res 199919805–815. [Google Scholar]
- 13.Ellis K J, Abrams S A, Wong W W. Monitoring childhood obesity: assessment of the weight/height2 index. Am J Epidemiol 1999150939–946. [DOI] [PubMed] [Google Scholar]
- 14.Himes J H, Bouchard C. Validity of anthropometry in classifying youths as obese. Int J Obes 198913183–193. [PubMed] [Google Scholar]
- 15.Lazarus R, Baur L, Webb K.et al Body mass index in screening for adiposity in children and adolescents: systematic evaluation using receiver operating characteristic curves. Am J Clin Nutr 199663500–506. [DOI] [PubMed] [Google Scholar]
- 16.Marshall J D, Hazlett C B, Spady D W.et al Validity of convenient indicators of obesity. Hum Biol 199163137–153. [PubMed] [Google Scholar]
- 17.Mast M, Langnase K, Labitzke K.et al Use of BMI as a measure of overweight and obesity in a field study on 5–7 year old children. Eur J Nutr 20024161–67. [DOI] [PubMed] [Google Scholar]
- 18.Reilly J J, Savage S A H, Ruxton C H S.et al Assessment of obesity in a community sample of prepubertal children. Int J Obes Relat Metab Disord 199923217–219. [DOI] [PubMed] [Google Scholar]
- 19.Reilly J J, Dorosty A R, Emmett P M. Identification of the obese child: adequacy of the body mass index for clinical practice and epidemiology. Int J Obes Relat Metab Disord 2000241623–1627. [DOI] [PubMed] [Google Scholar]
- 20.Schaefer F, Georgi M, Wuhl E.et al Body mass index and percentage fat mass in healthy German schoolchildren and adolescents. Int J Obes Relat Metab Disord 199822461–469. [DOI] [PubMed] [Google Scholar]
- 21.Wickramasinghe V P, Cleghorn G J, Edmiston K A.et al Validity of BMI as a measure of obesity in Australian white Caucasian and Australian Sri Lankan children. Ann Hum Biol 20053260–71. [DOI] [PubMed] [Google Scholar]
- 22.Welch N M, Saulsbury F T, Kesler R W. The value of the preschool examination in screening for health problems. J Pediatr 1982100232–234. [DOI] [PubMed] [Google Scholar]
- 23.Routh K, Denley J, Rao J N. A low cost method for measuring the prevalence of childhood obesity [unpublished report]. Birmingham: Department of Public Health, North Birmingham Primary Care Trust, 2005
- 24.Rudolf M C J. The obese child. Arch Dis Child Ed Pract 200489ep57–ep62. [Google Scholar]
- 25.Watson K. A study to assess the feasibility of establishing a robust surveillance system to determine prevalence, trends and variations in childhood overweight and obesity in Wolverhampton [Masters in Public Health dissertation]. Birmingham: University of Birmingham, 2005
- 26.Reilly J J, Methven E, McDowell Z C.et al Health consequences of obesity. Arch Dis Child 200388748–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Child Growth Foundation Annual BMI checks in schools workshop (convened by the Child Growth Foundation), at the Institute of Child Health, London. 17th June 2005. Available from http://www.childgrowthfoundation.org/Pdf%20Files/J‐17Report.pdf (accessed 5 March 2007)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.