Abstract
Background
The timing of parturition in most mammals is thought to be linked to a late gestational rise in corticosteroid production by the fetal adrenal gland. We hypothesised that gestational age would be prolonged in our patients with impaired cortisol production secondary to congenital adrenal hyperplasia (CAH) due to 21‐hydroxylase deficiency.
Methods
We compared the gestational age of patients affected by salt‐wasting CAH due to 21‐hydroxylase deficiency (born 1978–2004; n = 31) with that of children with congenital hypothyroidism (born 1981–2003; n = 30) and a control group of short normal children (born 1980–2002; n = 120). Each group was compared with national (England 2002–3) and regional (2003–4) data on gestational age from hospital episode statistics. Post‐term delivery was defined as birth beyond 41 completed weeks.
Results
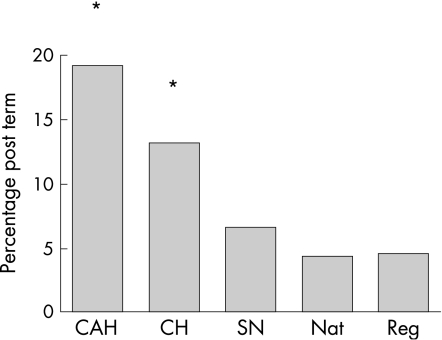
National statistics reveal a frequency of 4.4% for singleton deliveries beyond 41 weeks. In our region the frequency was 4.6%. In the group of children with CAH, the frequency of post‐term delivery was 19.3% (p<0.001). In patients with congenital hypothyroidism, the frequency was 13.3% (p = 0.02). The proportion of short children who did not have a recognised endocrinopathy born post term was comparable to national and regional data at 6.7%.
Conclusions
A prolonged gestation is more likely in pregnancies where the fetus has the salt‐wasting form of CAH. This may be due to impaired cortisol production, although other changes in steroidogenesis may also be contributory.
Keywords: congenital adrenal hyperplasia, 21‐hydroxylase deficiency, gestational age
The maturation and sustained activation of the fetal hypothalamo‐pituitary‐adrenal axis plays a major role in the onset of human parturition.1 There is an increase in the fetal plasma glucocorticoid level in most mammalian species towards the end of gestation and at the onset of labour.2,3 Glucocorticoids induce maturational changes in the fetal organs in preparation for the transition from intra‐uterine to extra‐uterine life. The rise in fetal glucocorticoids leads to an increase in intrauterine prostaglandins, which are key mediators of the events of labour.2,3
Congenital adrenal hyperplasia (CAH) due to 21‐hydroxylase deficiency is associated with impaired cortisol generation4,5 and we hypothesised that the length of gestation would be increased in patients with this disorder.
Methods
The local ethics committee granted ethical approval for this study.
CAH represents a range of severity and we selected only those patients with salt wasting, in whom cortisol synthesis would be most impaired. Patients showed the classical clinical picture of salt wasting in the first weeks of life coupled with raised 17‐hydroxyprogesterone (17‐OHP) levels.
From our service database we located 41 patients with CAH due to 21‐hydroxylase deficiency born between 1978 and 2001 on whom data on gestational age were available. Six had simple virilising CAH and were excluded from further analysis on the basis that they were able to generate sufficient cortisol to remain well postnatally. The 35 patients with salt‐wasting CAH (17 46 XX girls and 18 46 XY boys) included a set of affected twins and one affected individual who is a twin. They too were excluded because of the link between twin pregnancy and reduced gestational age. Finally, we also excluded one patient whose mother received glucocorticoid prior to the onset of labour. Information on gestational age, age at diagnosis and 17‐OHP level in the 31 remaining patients is detailed in table 1.
Table 1 Length of gestation, age at diagnosis and 17‐OHP values in patients with salt‐wasting CAH.
| Number | Year of birth | Length of gestation | Gender | Age at diagnosis (days) | 17‐OHP level (nmol/l)* |
|---|---|---|---|---|---|
| 1 | 1978 | 41 | F | 13 | 138 |
| 2 | 1983 | 41 | F | 5 | 108 |
| 3 | 1984 | 38 | M | 18 | 546 |
| 4 | 1985 | 41 | F | 4 | 393 |
| 5 | 1986 | 38 | F | 8 | 71 |
| 6 | 1988 | 40 | F | 0 (pre‐natal) | 161 |
| 7 | 1990 | 35 | F | 5 | 381 |
| 8 | 1991 | 40 | F | 2 | 187 |
| 9 | 1991 | 38 | F | 140 (20 weeks) | 449 |
| 10 | 1991 | 43 | M | 11 | 319 |
| 11 | 1992 | 40 | M | 0 (pre‐natal) | 351 |
| 12 | 1992 | 41 | F | 4 | 207 |
| 13 | 1992 | 40 | M | 38 | 140 |
| 14 | 1993 | 40 | M | 11 | 214 |
| 15 | 1994 | 40 | F | 37 | 400† |
| 16 | 1995 | 38 | M | 37 | 314† |
| 17 | 1996 | 40 | F | 45 | 152 |
| 18 | 1996 | 42 | M | 13 | 288 |
| 19 | 1997 | 40 | F | 12 | 770 |
| 20 | 1997 | 40 | F | 4 | 275† |
| 21 | 1998 | 42 | F | 52 | 227 |
| 22 | 1999 | 42 | M | 13 | 4406† |
| 23 | 1999 | 35 | M | 9 | 308 |
| 24 | 2000 | 39 | M | 11 | 2800† |
| 25 | 2000 | 41 | M | 17 | 95† |
| 26 | 2001 | 40 | M | 11 | 211 |
| 27 | 2001 | 40 | M | 16 | 85 |
| 28 | 2002 | 41 | M | 62 | 150 |
| 29 | 2003 | 42 | M | 74 | 976† |
| 30 | 2004 | 42 | M | 64 | 24† |
| 31 | 2005 | 40 | F | 4 | 487† |
*17‐OHP levels at presentation are marked with a dagger but are otherwise the highest recorded value in the local records. Normal range: 1–20 nmol/l. 17‐OHP, 17‐hydroxyprogesterone.
Data on gestational age were also assembled in two other patient groups (patients with congenital hypothyroidism and short normal children) from our clinic database. Patients with congenital hypothyroidism were expected to have a prolonged gestation and short healthy children were expected to have a normal gestational age. The 30 patients with congenital hypothyroidism were born between 1982 and 2003. All had permanent hypothyroidism and were found to have a thyroid stimulating hormone (TSH) concentration greater than 20 mIU/l as part of the neonatal screening programme (median 285 mIU/l, range 22.6 to >1000 mIU/l). All were from singleton pregnancies. The 120 short normal children were born between 1980 and 2002. All had been seen within our service and had no evidence of underlying endocrine disease on the basis of clinical, auxological and biochemical criteria and were singleton deliveries. All had more than one recorded measurement of height greater than −2.2 SDS at their first and latest recorded visits and none were treated with growth hormone.
Data on gestational age for singleton deliveries were also obtained from NHS maternity statistics, England 2002–03.6 Regional data on gestational age were obtained on request from the compilers of local hospital episode statistics. Term delivery was defined as birth between 37 and 41 completed weeks and post‐term delivery as birth after 41 completed weeks.
The data on gestational age in these groups were analysed by Minitab Version 14 using the χ2 test. Significance was set at the 5% level.
Results
National statistics demonstrate a frequency of 4.4% for deliveries beyond 41 weeks. In our region (2003–4) the frequency was similar at 4.6%. The frequency of post‐term gestation in the short normal group was 6.7%, which was also not significantly different from the regional and national data (p = 0.24 vs regional data).
However, 13.3% of babies with congenital hypothyroidism were born post term which is, as expected, greater than the regional (p<0.02) and national (p<0.02) data.
Gestational age was prolonged in patients with salt‐wasting CAH when compared to the short normal patients as well as the regional and national data, with 19.3% being born post term (p<0.001 when compared to regional data). The data are summarised in fig 1. The median gestational age was 40 weeks (range 35–43 weeks) and one female CAH pregnancy ran post term in contrast to five male pregnancies.
Figure 1 Percentage of deliveries born post term in the three patient groups under review in our service compared to regional and national norms. CAH, congenital adrenal hyperplasia; CH, congenital hypothyroid; SN, short normals; Nat and Reg, national and regional data, respectively. The asterisks highlight data that are significantly different from the national and regional norms (p<0.05).
Discussion
The length of gestation in CAH was assessed by Price and colleagues in 1971.7 They studied 19 children with CAH due to 21‐hydroxylase deficiency from 12 families. Unaffected siblings were used as controls and no significant differences in the length of gestation were reported. The small study numbers, the inclusion of mineralocorticoid‐sufficient children and the use of a genetically related control group may have had some bearing on the results. More recently, Gidlöf and colleagues in 20078 studied 114 patients with CYP21 defects (CYP21 being the gene that is typically commonly mutated in 21‐hydroxylase deficiency). They found that the gestational age of boys but not of girls was prolonged when compared to a control group and that there was a relationship between genotype and gestational age in affected girls but not in boys.
What is already known on this topic
The activity of the fetal hypothalamo‐pituitary‐adrenal axis influences the length of gestation.
Congenital adrenal hyperplasia due to 21‐hydroxylase deficiency is associated with impaired cortisol generation.
What this study adds
Congenital adrenal hyperplasia due to 21‐hydroxylase deficiency is associated with a prolonged gestational age.
This may reflect impaired cortisol production by the fetal adrenal gland.
We have compared the gestational age of a group of children with 21‐hydroxylase deficiency with national and regional statistics as well as a group of short normal children without a recognised endocrinopathy. A group of children with congenital hypothyroidism, an established cause of lengthened gestation,9 was included as a positive control. We found a highly significant increase in the proportion with longer gestational age in patients with salt‐wasting CAH due to 21‐hydroxylase deficiency. There were six patients in our clinic data with simple virilising CAH and it is of note that their gestational age was not prolonged (median of 38 weeks, range 36–40 weeks), suggesting that gestational age may also be influenced by the severity of the underlying genetic defect.
There is an increase in fetal glucocorticoid production due to maturation and sustained activation of the hypothalamo‐pituitary axis (HPA) towards the end of gestation in most primates. An increase in placental corticotrophin‐releasing hormone (CRH) production results in increased maternal and fetal cortisol generation.2 The increased fetal cortisol production enhances placental CRH release through a positive feedback mechanism. An increase in placental 11β hydroxysteroid dehydrogenase 2 (11β‐HSD2) activity also results in a greater conversion of maternal cortisol to cortisone and an increase in fetal adrenocorticotrophic hormone (ACTH) production with further maturation of the fetal adrenal gland. The surge of glucocorticoids is thought to be an integral part of a cascade of events leading to the onset of parturition. Bio‐active glucocorticoids in the final 10–15 days prior to delivery induce maturational change in fetal organs such as lungs, liver, kidney and gut. Recent evidence suggests that the rise in fetal glucocorticoids mediates the increase in intra‐uterine prostaglandin production through direct and indirect activation of prostaglandin H synthase (PGHS) type 2.1 Prostaglandins may promote membrane rupture or pass through the membrane to act at the underlying cervix and myometrium and facilitate cervical ripening and myometrial contractility.
In CAH, in addition to potential glucocorticoid deficiency, glucocorticoid bioactivity may be limited by high levels of 21‐deoxycortisol in the fetal circulation, based on evidence for attenuation of glucocorticoid feedback in an adrenal tumour generating this steroid.10
Fetal HPA maturation and a local intrauterine increase in cortisol also results in increased placental oestradiol production.2,3 Production of oestriol is markedly increased in pregnancies with CAH, due to increased production of fetal precursors. The role of oestrogens of fetal origin in the determination of human parturition length is uncertain. Preterm delivery is associated with increased maternal plasma and salivary oestriol,2 whilst in steroid sulphatase deficiency, where oestriol levels are very low, gestation length is extended.11 Increased oestrogen production in CAH may therefore counter, to some extent, prolongation of pregnancy due to glucocorticoid deficiency.
We too, like Gidlöf and colleagues,8 found that prolonged gestation was more noticeable in males than in females (33% vs 6%), although the numbers in the two groups are relatively small. Gestational age is known to be slightly longer in males than females and 17‐OHP has been shown to prevent preterm delivery; it is therefore possible that the difference between CAH patients and controls is linked to alterations in androgen and 17‐OHP levels.8 The sex difference, if real, cannot easily be ascribed to alterations in androgen production alone because increased androgen generation is a feature of both girls and boys with 21‐hydroxylase deficiency, as is the increase in 17‐OHP concentrations. Unfortunately we were unable to obtain data on cortisol, 17‐OHP or androgen levels at birth that could be compared with gestational age. The association between genotype and gestational age in girls in the study by Gidlöf and colleagues8 underlines the importance of studying the relationship between genotype, biochemistry and gestational age in a large number of pregnancies.
In summary, gestational age was prolonged in our cohort of patients with CAH due to 21‐hydroxylase deficiency. We suspect that this is linked to alterations in cortisol generation, although changes in androgen, oestrogen and 17‐hydroxylated cortisol precursor production may also be important.
Abbreviations
ACTH - adrenocorticotrophic hormone
11β‐HSD2 - 11β hydroxysteroid dehydrogenase 2
CAH - congenital adrenal hyperplasia
CRH - corticotrophin‐releasing hormone
HPA - hypothalamo‐pituitary axis
17‐OHP - 17‐hydroxyprogesterone
PGHS - prostaglandin H synthase
TSH - thyroid stimulating hormone
Footnotes
Competing interests: None.
References
- 1.Whittle W L, Patel F A, Alfaidy N.et al Glucocorticoid regulation of human and ovine parturition: the relationship between fetal hypothalamic‐pituitary‐adrenal axis activation and intrauterine prostaglandin production. Biol Reprod 2001641019–1032. [DOI] [PubMed] [Google Scholar]
- 2.Weiss G. Endocrinology of parturition. J Clin Endocrinol Metab 2000854421–4425. [DOI] [PubMed] [Google Scholar]
- 3.Smith R. Parturition. N Engl J Med 2007356271–283. [DOI] [PubMed] [Google Scholar]
- 4.Ghizzoni L, Bernasconi S, Virdis R.et al Dynamics of 24‐hour pulsatile cortisol, 17‐hydroxyprogesterone, and androstenedione release in prepubertal patients with nonclassic 21‐hydroxylase deficiency and normal prepubertal children. Metabolism 199443372–377. [DOI] [PubMed] [Google Scholar]
- 5.Miller W L. Clinical review 54: genetics, diagnosis, and management of 21‐hydroxylase deficiency. J Clin Endocrinol Metab 199478241–246. [DOI] [PubMed] [Google Scholar]
- 6.HESonline Hospital episode statistics. http://www.hesonline.nhs.uk (accessed 9 May 2007)
- 7.Price H V, Cone B A, Keogh M. Length of gestation in congenital adrenal hyperplasia. J Obstet Gynaecol Br Commonw 197178430–434. [DOI] [PubMed] [Google Scholar]
- 8.Gidlöf S, Weddel A, Nordenström A. Gestational age correlates to genotype in girls with CYP21 deficiency. J Clin Endocrinol Metab 200792246–249. [DOI] [PubMed] [Google Scholar]
- 9.Medda E, Olivieri A, Stazi M A.et al Risk factors for congenital hypothyroidism: results of a population case‐control study (1997–2003). Eur J Endocrinol 2005153765–773. [DOI] [PubMed] [Google Scholar]
- 10.Ismail A A A, Burr W A, Taylor N F.et al Elevated plasma adrenocorticotropin (ACTH) with adrenal hyperplasia: a new factor in ACTH regulation? J Clin Endocrinol Metab 199173752–757. [DOI] [PubMed] [Google Scholar]
- 11.Taylor N F. Review: placental sulphatase deficiency. J Inherit Metab Dis 19825164–175. [DOI] [PubMed] [Google Scholar]