This lecture has traditionally been on a clinical topic, and few aspects of the clinical activity of GPs are more important than the consultation. James Mackenzie was born in 1853 into a world which could not have been more different than ours. The technological, political, environmental, therapeutic, and medical changes since his time have been absolutely astonishing, although many aspects of humanity have changed less. Indeed, it is very likely that his patients were in many respects very similar to those consulting us today. Shakespeare, after all, was writing over 400 years ago and yet we still recognise with beautiful clarity the universal truths of the human relationships in his writings.
So, if James Mackenzie and I were effectively treating the same human beings, what do we have to learn from each other? What have we gained? What have we lost? His parents were hill farmers in Perthshire, and he left school at the age of 15 to become apprentice to a pharmacist in Perth. It seems likely that the rather unsatisfactory nature of some of the medicine and advice that was offered in the pharmacy was the stimulus for his wishing to study medicine.
Student debt is nothing new, so after completing medical school he needed to earn some money before he did his house jobs. In those days house jobs were unpaid, and so he became a locum in a practice at Spennymoor, County Durham. I quote from his biography:
‘Mackenzie, fresh from his university training, beheld a daily procession of men and women, few of whom were even slightly unwell, coming to demand medicine.’1 (page 30)
The doctor he worked for had invented a special mixture of his own, consisting of burnt sugar and water, with a pinch of ginger added. This enjoyed a great reputation among the miners, and is likely to have taught him that prescribing does not always achieve its ends by means that are entirely physical. In 1879 after his junior hospital posts, James Mackenzie moved to Burnley, Lancashire and, as his biographer intriguingly words it:
‘…that step meant that all hope of shining in his profession had been abandoned. Mackenzie knew very well that GPs do not shine. They are the rank and file, the common soldiers of the army of healing.’1 (page 33)
Nevertheless, he was apparently hugely impressed by his senior partner, Dr Briggs, and couldn't understand how Dr Briggs could look at one patient and know he or she was ill and another and know there was nothing to worry about.
And so he took to his room, with textbook after textbook, encyclopaedia after encyclopaedia (these days he would have spent hours on the internet) but he couldn't find the answers. However much he studied, every day more patients would see him with conditions he couldn't name, let alone treat. In Mackenzie's own words:
‘For some years I thought that my inability to diagnose my patients' complaints was due to personal defects; but gradually I came to recognise that the kind of information I wanted did not exist.’1 (page 43)
Indeed, he found general practice increasingly frustrating. He wrote:
‘I was not long engaged in my new sphere when I realised I was unable to recognise the ailments in the great majority of my patients. For some years I went blundering on, gradually falling into a routine, [that is] giving some drug that seemed to work favourably on the patient, till I became dissatisfied with my work and resolved to try and improve my knowledge by more careful observation.’1 (page 52)
What he had recognised was something we still recognise today: the quite extraordinary mismatch between the medical textbooks and the ways in which our patients present to us. And so, in an attempt to get some clarity into his professional life, Mackenzie started on the track that would lead to his fame and his fortune. He became a GP with a special interest — and his special interest, triggered by the death from heart failure of a young woman in childbirth, became cardiology.
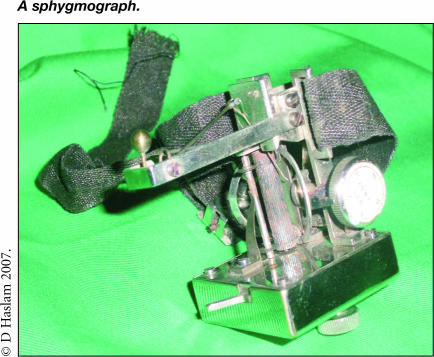
As many of us do when faced with the vast complexity of our role as GPs, he chose to simplify his task by focusing on a relatively small area. And, once he had his focus, he excelled. In 1890 he was the first doctor in the world to discover extrasystoles, a condition that had previously lead many patients to become cardiac invalids by the anxiety of their doctors, who needlessly confined them to bed to protect their hearts. He used a device that could actually measure these extrasystoles: a sphygmograph which recorded the pulse on a smoked drum, which was then varnished to preserve the record. He then developed the polygraph, a portable, clockwork, ink-writing instrument with two tambours with which he was able to record radial and jugular pulses simultaneously, and to measure the atrioventricular interval. He used the polygraph to diagnose the various types of heart block.
This work was all done in the course of the usual busy medical practice. And he had chosen a vital branch of medicine to specialise in — because doctors did not understand the science of irregular heartbeats they terrified their patients with their advice and prognostications.
There are plenty of conditions where we may be doing this today. We may not know it, but it is likely that some of the abnormal results that we interpret to our patients, inevitably and unintentionally causing concern as we do, will turn out to much less significant than we believe. But we will have to wait to find out which they are.
In 1897 Mackenzie described the irregularly irregular heart beat of atrial fibrillation, and subsequently began to attract the attention of the medical world (although initially he was held in highest regard only outside the UK, where they didn't realise that he was a mere GP), and he was invited to overseas conferences to present his work. Indeed, the only way he could really get taken seriously in the UK was to become a specialist, and so he moved to London, and eventually to consulting rooms in Harley Street. His career blossomed, and to his delight he was elected an FRCP in 1909, a Fellow of the Royal Society in 1915, and was honoured with a knighthood later that year.
So, it seems all the more remarkable that 2 years later, at the age of 64 years, he decided to leave London and move to St Andrews to set up an institute for research in general practice, and to address those very issues that had so eluded him at the beginning of his career. This far-sightedness is why we still honour him. He was passionate to encourage GPs to keep good records and was probably one of the first doctors to think of epidemiology other than in terms of infectious disease.
Blaming the viruses
Reading any description of his life, one is repeatedly struck by the similarities between medicine then and medicine now — not least the fact that huge numbers of patients saw themselves as unwell and presented themselves to a doctor who had little or no idea what was wrong with them. But in all my research for this lecture I have singularly failed to find the first recorded usage of the phrase ‘It's a virus’. Who knows what phrase was used before we had viruses to blame. But it is a phrase that symbolises a great deal.
Firstly, you know and I know, and our patients know, that we have frequently no real idea of what is causing the symptoms, and ‘virus’ has become a pseudo-scientific way of disguising this (even though it may occasionally and accidentally be true).
But secondly, patients often say, ‘The doctor said it was just a virus’. Ponder for a moment on that use of that word ‘just’. Every GP knows how put down we feel when people ask, ‘So are you a specialist or just a GP?’. The same happens to patients whose illness we put down to ‘just’ a virus. Words carry many more meanings than we sometimes intend.
Then and now
Despite the many changes in society, there are still similarities, as well as differences, between health care in 1880 and the present day. We still struggle with absurdly short appointment times. After all, since our new contract we have needed long enough to deal with both the patient's agenda and the doctor's agenda, which may be completely different. But on average, most practices now offer appointments of about 10 minutes per patient. Compared to Mackenzie's time, that's luxury. In 1879 at Barts in London, 120 patients were seen by the admitting physician and dismissed in 1 hour and 10 minutes: a rate of 35 seconds per patient. Another report showed that in the late 19th century, three casualty officers in one London hospital dealt with 500 patients in a morning — just think what employing doctors like this would do for the maximum 4-hour A&E waiting target.
Disease patterns were different too. In Mackenzie's time infectious disease in particular was rife: in Burnley in 1879 there were 56 deaths from scarlet fever and infant mortality was one in five.2 As well as coping with the flood of minor problems that he could not diagnose, Mackenzie's working day dealt with conditions such as pneumonia (which was frequently fatal), diphtheria, cholera, and acute rheumatism. This exemplifies the way in which health care, and the way we need to deliver it, has changed.
Simplifying greatly, we can say that health care in the UK has spent 50 years dealing with infectious disease, 50 years dealing with acute disease (often needing hospital admission), and we are now in the phase of dealing with ‘long-term medical conditions’.
But the thing that really strikes me, even discounting the extraordinary speeds of consulting that I've quoted here, is that we are still today astonishingly busy. Almost none of the conditions that I've just listed, and which kept Mackenzie so busy, exists in our practice today, at least to any significant time-consuming degree. The British population has never been healthier. The so-called pensions crisis is a simple result of our ever-increasingly longevity. But people are still worried sick.
Worried sick
Our patients are worried sick about their health, their children's health, of conditions that they hadn't heard of last year and will have forgotten next.
This failure to have an impact on how people feel is similar to the fascinating point made by Richard Layard, in his book on happiness, who shows that in the UK, US, and Japan over the past 50 years average incomes in real terms have more than doubled, but — despite more food, more clothes, more cars, more holidays, more travel, a shorter working week, more central heating, and more health — there is absolutely no evidence that anyone is any happier.3
A similar law applies in health. The population, our patients, live longer and longer, and have every advantage known to humankind, but our surgeries are still full of patients frequently anxious about conditions they have recently read about.
This very busyness could be a real tribute to our success as doctors, or indeed it could be the opposite. But it does beg a question about what we are trying to achieve. It seems unlikely that if we work flat out, prevent everything we can prevent, screen everything we can screen, and treat everything that we can treat, there will ever come a day when we open the surgery door and no one attends because they are all well.
Clearly expectations change all the time. What is normal in one decade is intolerable in another. But at some stage we need to become clear about what we are trying to do, and what the purpose is of our profession and our specialty. It would be fascinating to know what the real reasons were for all those people who queued up to see Mackenzie (and I'm going to ignore the ones with clear-cut conditions like mitral valve disease or irregular pulses).
We have really no idea. Ourepidemiological scientific studies count the diseases, but not the worries. Not the vague symptoms, the ‘tired all the time’, or ‘while I'm here, doctor’ worries. However, it seems that there is a form of medical Parkinson's Law in action, with the work not just expanding to fill the time available, but the interpretation of the work expanding to match the interests of the doctor.
What do I mean? I doubt if many doctors will dispute the fact that the choice of treatment for some conditions is more related to the interest of the healthcare professional than to the physical signs and symptoms of the patient. As an example, just think how the management of back pain varies depending on whether you consult a physiotherapist, rheumatologist, gynaecologist, osteopath, orthopaedic surgeon, chiropractor, or GP: same back — different diagnoses.
This almost certainly applies to the problems we tackle as family doctors. Take the patient who is ‘tired all the time’. After taking a detailed history, probably taking blood tests, especially for thyroid status, checking for sleep apnoea, and all the other possible medical causes — in many cases, at least in my opinion — we end up not having a clue. And so diagnoses like chronic fatigue syndrome or post-viral syndrome get suggested. We think in medical terms. It's what we've got. It's inevitable.
But it may not necessarily be correct. We use the medical model because the medical model is what we use, even though it may not always be appropriate. Some of the problems that are brought to us arrive simply because we are there. They get brought to a doctor because there is almost no one else freely available to turn to. These days fewer and fewer people will go to their priest, or vicar, or rabbi when they are troubled, but they will come to us. We should be honoured with this trust and responsibility, but the fact that everything is our business means that it becomes increasingly difficult to know when we have succeeded.
We all know there are many ways at looking at things, and that in Rorschach tests what you see is determined by well, what you see. But I can't help but wonder if the reason we sometimes find medical solutions to people's problems is simply because that's what we do. When diagnosis is appropriate, we make a real difference. But when we get it wrong, we almost certainly do harm. There is a risk that we will turn a feeling into a disease, a risk that we clearly do not have to succumb to. After all, such action carries significant risks as well as possible benefits.
And to return to the dreadful busyness of our lives, in this era when people are generally vastly healthier than they were in Mackenzie's day we still struggle to provide good access. Mackenzie would probably have thought, with good reason, ‘If only we can cure all the patients with diphtheria, pneumonia, TB, and cholera then the 48-hour access targets should be no problem to us at all.’.
Instead, with all these conditions cured, most of us struggle to meet the demand for our time. In my own practice, and I know I have driven all my partners past and present to despair with my constant dissatisfaction with the appointment system, whatever we do there is more demand than we can provide solutions for. And, as a result, we feel and seem constantly busy. And it's not going to get any better.
With an ever-healthier population whom we are seeing more frequently than ever, we also need to ask what potential harm are we doing. We do what we do. We follow the guidelines. We offer the advice, but we rarely stop to ask precisely what is it we are actually aiming for.
Role of the GP
I believe it is now well accepted that much of our state of wellbeing as humans is derived from cultural and social influences rather than simply the absence of disease. But when we get someone through our door, we now feel a duty — driven by a complex mix of ethical, altruistic, legal, and financial reasons — to screen them for conditions they didn't know about, and offer lifelong treatment for something that might never have happened. And we then wonder why we are busy. Clearly some conditions (hypertension being a good example) justify this approach, but we still need to remember the warnings of excessive confidence in the potential for prevention that were so eloquently described by Petr Skrabanek and James McCormack.4
The patients who consult me bring a complex mix of feelings and fears. They present these to me in a frequently confusing mixture of words and body language. At some stage I may take a blood test and the answer will be given to me with certainties and decimal points. The information I receive from my patients is ‘analogue’, but our guideline and computer-driven responses are frequently digital. Sometimes this is appropriate, as in the clearly-defined diagnosis of diabetes, but frequently it is not.
Those who are as passionate about music and electronic gadgetry, as I am, believe that something very special may be lost in digital as opposed to analogue recording. As Neil Young once said:
‘Sound is like water. Analogue is a warm bucketful slowly poured over your head and digital is the same water, same bucket only this time it's ice cubes dumped quickly. I know which is more pleasing to me.’5
And I suspect it is so with our medical analysis of the problems that our patients bring. The clarity appears to be astonishing but, as with music, something sensitive seems to be lost. It is all too easy to be seduced by the science of our role. James Mackenzie clearly felt overwhelmed by the complexity of patient presentation, and started to invent gadgets — world beating, astonishingly important gadgets too — but this focus on the simple and measurable was carried out because the complexity of so much of what we do is not simply measurable.
In its early years, the founders of our Royal College made, I believe, a similar understandable choice. They needed to be taken seriously. Our speciality was denigrated by all the other specialties. And so we focused on the things that the other specialties were particularly good at: the science, the statistics, the P-values, the digital rather than the analogue. In no way does this decry the value of serious research and, obviously, much quantitative research is ‘analogue’, but the risk is there.
But as many wise GPs have always known, and as is becoming clearer by the day, the world is not as clear-cut as many would like to make it. This is beautifully summed up by the McNamara Fallacy (Box 1).6
Box 1. The McNamara Fallacy.
-
▸
The first step is to measure whatever can be easily measured. This is OK as far as it goes.
-
▸
The second step is to disregard that which can't be easily measured or to give it an arbitrary quantitative value. This is artificial and misleading.
-
▸
The third step is to presume that what can't be measured easily really isn't important. This is blindness.
-
▸
The fourth step is to say that what can't be easily measured really doesn't exist. This is suicide.
While it is absolutely correct that when there are certainties of diagnosis, of guidelines, of evidence-based medicine, then we owe it to our patients to give them the best possible care. But we make a real mistake if we think that our patients are their conditions. We all scoff at the remaining old-fashioned and less enlightened hospital colleagues who talk about the diabetic in the first bed, or the interesting shoulder, but much of the time we too also forget the complexities of our patient's lives.
In Mackenzie's day, doctors had precious few effective therapies, and so the patient — the person — was all-important. The extraordinary improvement in what medicine is able to do has led to a shift from the patient being the most important, to the disease being most important. (While we talk, of course, of the importance of patient centredness.) Faced with a template, there is a risk that the patient becomes the condition. There is a risk that we are focusing on the diagnosis, not the person — but it is people who come to consult us.
Clearly we do need to record the biomedical. We absolutely owe it to our patients to offer the best possible biomedical care. But our concentration must be on the human in front of us, not on our computer. More than anything we need to shut up and listen. Indeed, I would suggest that there needs to be a slot on all future computer templates that says, ‘Shut up and listen’.
It is very sad — but our digital-templated world poses a real risk of missing the analogue subtlety of our patients' lives. And if you consider the fact that most certainties since Mackenzie's time have proved to be transient, and that human complexity has remained permanent, then we must ensure that we do keep some baby when the bathwater has been thrown away.
As GPs, and particular as GPs with an interest in communication as most are in the College, we do try to address much of this. After all, if we are to understand the full subtlety of what our patients bring us, then the answer must lie in communication, communication, communication. And we have made huge strides in our teaching and understanding of this topic. There is so much that we can be proud of.
But learning to consult by using a consultation skills checklist fills me with despair. Nothing is more bizarre or dispiriting than seeing GP registrars who tape checklists from their good consulting recipe books onto their computer monitors to ensure that they do everything that their assessment demands. The absolute essence of a good consultation is empathy: the ability to see the world through the eyes of one's patients. I am sure it is this ability that triggers comments like, ‘I always feel better for seeing that doctor’; comments that seem totally disconnected from diagnosis or prescription. Something that is as rarely researched, which is puzzling, as making people feel better might just be one of the reasons we exist.
And so the essence of teaching and learning quality consultation should not be imitation — the surface skills that can be switched on and off.
Teaching young and not-so-young doctors the importance of establishing eye contact should be patronisingly insulting. We should instead simply be teaching them to empathise to listen, to care — the rest will follow. The reverse is not necessarily true.
Simply working through a checklist of behaviours (greet the patient, establish eye contact, don't interrupt) can never be enough, and may damage the very human contact that the doctors would hope to achieve. Michael O'Donnell has recently pointed out that actors would never learn to act by simply learning mechanistic skills (such as establishing eye contact).7 They would try and get inside the skin of the character. They would need to understand both how their character feels and thinks and ticks, and how the characters they are interacting with feel and think.
Illness and disease
This simple human act of empathising and caring cannot be underestimated. After all, only about 40% of new disorders seen by GPs evolve into recognised disease.8 And even when they do, GPs have to treat illness rather than disease. Understanding disease is the focus of much basic medical training.
But understanding illness is quite different. It means understanding the feelings of regret, guilt, fear, betrayal, loneliness, and all the other emotions that turn the same disease into different illnesses in different people.
Getting the consultation right is perhaps more important than it has ever been. After all, there are still real time pressures. Even though consultations are longer, there is so much more to do. And I also wonder if for much of the time we are now in the business of creating suffering, rather than alleviating it.
James Mackenzie devoted his life to the relief of suffering. In the same way that I have talked about the difference between disease and illness, I sometimes wonder whether our obsession with screening for disease has had the side effect of creating illness. This wouldn't be a problem if we were discussing it, but while we know the impact of statins on cholesterol, we need to know much more about the impact of all this activity on the whole person.
Mr Jones consults the doctor with a sore throat. The doctor's computer triggers a reminder that he hasn't had his blood pressure checked recently. His blood pressure is borderline, so he has a fasting cholesterol blood test. This is high, and in many cases he will be started on statins.
The only suffering we are relieving in the above example is a potential future episode of suffering. This may be noble, it may be correct, and it may be damaging. After all, these screening and preventative activities are not without risk. We have an extraordinary capacity for over-simplification.
Take hormone replacement therapy — if HRT makes someone feel better, so that she sleeps better, and as a result doesn't have a road accident, how do we measure that benefit, that non-existent event that didn't happen, but which saved her life?
Take sunshine — if someone gets a suntan, feels better about how they look, has the confidence to take steps in life that might not have happened, how do we set that against the risk of melanoma? We can't. We don't. But, my God, we are certain that some things are dangerous.
Guidelines
As far as I can gather, the next guidance from NICE (set to form the basis of cardiovascular screening) will lead to three-quarters of middle-aged men being treated with statins. And it's not just statins — 10% of the entire population over 50 years of age will need treatment for stages 3–5 chronic renal disease.
We behave as if this is wonderful — that we are really clever and noble in being able to offer the population protection. But it isn't that straightforward. There are plenty of difficulties — not least people remembering or being bothered to take medication. With heart disease, study after study has shown that patients are nowhere as enthused about all this medication as their doctors are for prescribing it, with discontinuation rates of lipid-lowering therapy up to 50% after 1 year and 85% after 2 years.9 So, the fact that we can offer prevention isn't as simple as it seems.
And at the same time the real causes of disease can get ignored. While doing a home visit on one of my patients, a visiting relative said he was really worried that he had run out of blood pressure tablets and asked whether I could prescribe some urgently. This man was 23 stone in weight, stuck into an armchair, surrounded by cans of lager, a full ash tray by his side, and a huge portion of fish and chips on his knee. But it was the pills that he needed to keep his heart healthy!
This isn't just absurd. It is important. To me it perfectly highlights the tendency to treat health simply as something that involves doctors and requires treatments. But health is far more than this. When the entire population is on statins and cancer-preventing drugs and we have turned obesity into an entirely medical condition, and so on and on and on, will we ask ‘when is enough, enough?’.
What is it all for?
What exactly are we trying to do? Donald Irvine has described beautifully what we want from a doctor:
‘Evidence is abundant that the public want doctors who are technically competent; give them the best possible clinical outcome; are as safe as possible; are kind, courteous, and respectful; and involve them in decisions about their care.’10
But the ‘How we should do it’ doesn't answer the ‘What?’. What are we for? In Mackenzie's time, and indeed today, many would answer: ‘The relief of suffering’. In our modern culture of general practice many might think this naïve. The doctors in James Mackenzie's time were unable to make most of the diagnoses of the conditions that their patients were experiencing, simply because most of these conditions had not yet been discovered. The same very clearly applies to us, although we don't realise it yet. The medical journals in 50 years will be full of conditions that you and I have never heard of, but exist today undiscovered.
Doctors in the past had virtually no effective investigation or drugs. Nevertheless, the people and populations they served believed they were hugely valuable — a fascinating paradox. We do have powerful drugs, and clever diagnoses. But maybe the part of the consultation that ultimately matters the most to many patients is the part that we have downplayed in our search for scientific truths and recordable data.
As a paper in the Royal College of Physicians' journal Clinical Medicine said in 2003:
‘The good consultation should always leave a patient with an increase in self-esteem and perhaps some alleviation of their symptoms as well. Our forebears knew that their clinical skill in the consultation was paramount, given that their medications were often ineffective and functioned solely as placebos. The skillful consultation itself often has a placebo effect, depending on the bedside manner.’11
There is a risk that we are creating a form of general practice that will not permit the placebo effect to work. I have already stressed that I believe it is working much of the time, and we will only realise this when research shows us that the treatments we are using are ineffective. People probably trust us because of all those consultations where nothing much seemed to happen. Irrespective of what we did therapeutically, they got better. When someone consults you with something potentially serious, and you either reassure or treat, why do they trust you?
We all know the fantastic statistics about levels of trust in GPs. But we need to understand why people trust us. Trust is so important in our work, but it isn't something we get issued with automatically with our MRCGP exam pass. Trust has to be earned, and there can be few better ways to earn trust than by getting it right. We often get it right for a whole range of conditions where the patient would have got better anyway (often the consultations that we discuss at coffee break time were strictly speaking not necessary), but getting it right certainly builds the relationship. And then when something serious does turn up in the patient's life, we have credit in the bank.
I believe we are trusted, because we've earned the trust. We've earned it by seeing them four times a year on average for things that frequently didn't matter, and being approachable and available and mostly kind. Denis Pereira Gray has talked about how these levels of contact add up, but the future of general practice is making such repeated contact less likely.12
We know that continuity of care increases patient satisfaction, reduces hospitalisations, emergency department use, inappropriate prescribing, and inappropriate diagnostic testing, and improves the receipt of preventative services. And so it is intriguing that so many initiatives seem to reduce continuity: walk-in centres, access targets, and huge practices to name but three. What worries me for the future is that if we don't see patients for the minor conditions and unhappiness, the non-existent viruses, and the puzzling anxieties, then the first time we meet them will be when the potential big illness arrives. When this happens, why should anyone trust his or her GP? What will we have earned? Will the risk sink still function?1
But, for as long as we are dealing with patients who have learned that the doctor is a trusted member of the community who, by and large, gets it right, and who cares for them, then we will surf on the professional trust built up from their childhoods. A generation in the future, when no one has experienced this model of care, why will people trust GPs then? How will we earn our place in society?
Even as I say these words, I am aware that ‘trust’ can be a concept that sounds patronising. Are not doctors and patients equal? Should our relationship not be based on sharing of information and mutual decision making? Does this not render trust an antiquated concept? As so many of my patients still say, ‘I'm not sure — what do you think, doctor?’.
Mackenzie believed firmly in the importance of basing medical education in the community, and the money from his estate was used to help found the first chair of general practice in the world, at Edinburgh University in 1963. Mackenzie's biography was titled The Beloved Physician.1 Mackenzie was beloved because he cared.
That's what most of our patients want. Of course they want and need us to have high levels of knowledge, to be competent, and professional, and to be able to diagnose their rashes, to be their advocates in times of trouble, to be guided by research and study, as we straddle the twin religions of art and science, but most of all they want us to care.
It's not for nothing that the College motto is Cum Scientia Caritas. Caring is a difficult concept to measure. We all know that in general we measure what we can see, and not necessarily the things that matter. But for all our digital sophistication we must never forget that one of the lessons of history is that while the scientific truths are constantly changing, the human truths appear to be eternal.
Acknowledgments
I would like to thank all my colleagues at Ramsey Health Centre, doctors and staff, for their remarkable support and encouragement over very many years, and particularly my partner Dr Simon Brown, for his advice on early drafts of this lecture. Thanks too, as ever, to my wife, Barbara, for her patient support and invaluable advice
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Macnair Wilson R. The beloved physician. London: John Murray; 1926. [Google Scholar]
- 2.Mair A. Sir James Mackenzie M.D. 1853–1925 general practitioner. Edinburgh: Churchill Livingstone; 1973. [Google Scholar]
- 3.Layard R. Happiness: lessons from a new science. London: Penguin Books; 2006. [Google Scholar]
- 4.Skrabanek P, McCormick J. Follies and fallacies in medicine. 3rd edn. Glasgow: Tarragon Press; 1998. [Google Scholar]
- 5.Young N. This week's music quote. bmusic Newsletter No. 96. http://www.bmusic.com.au/links/whatsnew/newsletters/archives/newsno96.html (accessed 6 Nov 2007)
- 6.Handy C. The empty raincoat: making sense of the future. London: Random House; 1995. [Google Scholar]
- 7.O'Donnell M. Doctors as performance artists. J R Soc Med. 2005;98(7):323–324. doi: 10.1258/jrsm.98.7.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosser WW. Application of evidence from randomised controlled trials to general practice. Lancet. 1999;352:661–664. doi: 10.1016/S0140-6736(98)09103-X. [DOI] [PubMed] [Google Scholar]
- 9.LaRosa JH, LaRosa JC. Enhancing drug compliance in lipid-lowering treatment. Arch Fam Med. 2000;9:1169–1175. doi: 10.1001/archfami.9.10.1169. [DOI] [PubMed] [Google Scholar]
- 10.Irvine D. Success relies on winning hearts and minds. BMJ. 2006;333(7575):965–966. doi: 10.1136/bmj.39010.463044.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Watkins P. The placebo effect. Clin Med. 2003;3(5):397–398. doi: 10.7861/clinmedicine.3-5-397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pereira Grey D. Forty-seven minutes a year for patients. Br J Gen Pract. 1998;48(437):1816–1817. [PMC free article] [PubMed] [Google Scholar]
- 13.Haslam D. ‘Schools and hospitals’ for ‘education and health’. BMJ. 2003;326(7383):234–235. doi: 10.1136/bmj.326.7383.234. [DOI] [PMC free article] [PubMed] [Google Scholar]