Abstract
Health literacy deficits affect half the American patient population and are linked to poor health, ineffective disease management and high rates of hospitalization. Restricted literacy has also been linked with less satisfying medical visits and communication difficulties, particularly in terms of the interpersonal and informational aspects of care. Despite growing attention to these issues by researchers and policy makers, few studies have attempted to conceptualize and assess those aspects of dialogue that challenge persons with low literacy skills, i.e., the oral literacy demand within medical encounters.
The current study uses videotapes and transcripts of 152 prenatal and cancer pretest genetic counseling sessions recorded with simulated clients to develop a conceptual framework to explore oral literacy demand and its consequences for medical interaction and related outcomes. Ninety-six prenatal and 81 genetic counselors – broadly representative of the US National Society of Genetic Counselors – participated in the study. Key elements of the conceptual framework used to define oral literacy demand include: (1) use of unfamiliar technical terms; (2) general language complexity, reflected in the application of Microsoft Word grammar summary statistics to session transcripts; and, (3) structural characteristics of dialogue, including pacing, density, and interactivity. Genetic counselor outcomes include self-ratings of session satisfaction, informativeness, and development of rapport. The simulated clients rated their satisfaction with session communication, the counselor’s effective use of nonverbal skills, and the counselor’s affective demeanor during the session.
Sessions with greater overall technical term use were long and used more complex language reflected in readability indices and multi-syllabic vocabulary (measures averaging p<.05). Sessions with a high proportionate use of technical terms were characterized by shorter visits, high readability demand, slow speech speed, fewer and more dense counselor speaking turns and low interactivity (p<.05). The higher the use of technical terms, and the more dense and less interactive the dialogue, the less satisfied the simulated clients were and the lower their ratings were of counselors’ nonverbal effectiveness and affective demeanor (all relationships p<.05). Counselors’ self-ratings of informativeness were also inversely related to use of technical terms (p< .05).
Just as print material can be made more reader-friendly and effective following established guidelines, the medical dialogue may also be made more patient-centered and meaningful by having providers monitor their vocabulary and language, as well as the structural characteristics of interaction, thereby lowering the literacy demand of routine medical dialogue. These consequences are important for all patients but may be even more so for patients with restricted literacy.
Keywords: health literacy, oral literacy, patient-provider, communication, genetic counseling, USA
Introduction
Literacy deficits are widespread. The most recent National Adult Literacy Survey, with, a national representative sample of over 35,000 Americans, reported that almost half the population performs at basic or below basic levels of literacy (Kutner, Greenberg, & Baer, 2005). These levels may be considered inadequate preparation to “use print and written information to function in society, to achieve one’s goals, and to develop one’s knowledge and potential”, as literacy is defined by the Survey authors (Kutner et al., page 1, 2005). Health literacy, the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions (HHS, 2000), shows similar deficits. Reviews of health literacy studies estimate that one-quarter of patients have inadequate health literacy skills and another 20% perform at marginal levels (Paasche-Orlow, Parker, Gazmararian, Nielesen-Bohlman, & Rudd, 2005). In light of these disturbing numbers, it is not surprising that health literacy has come to the attention of researchers, policy makers and clinicians, including the Institute of Medicine (Nielsen-Bohlman, Panzer, Kindig & Institute of Medicine, 2004), the Surgeon General’s 2010 Objectives for the Nation (HHS, 2000), and American Medical Association (Schwartzberg., Van Geest, Wang, Gazmararian, Parker, Roter et al., 2004).
The consequences of restricted literacy for health are considerable. Low literacy has been linked to lower levels of self-reported health (Gazmararian, Baker, Williams, Parker, Scott, Green et al., 1999), less use of preventive care and cancer screening (Scott, Gazmararian, Williams & Baker, 2002), less effective diabetes management and more disease related complications (Schillinger, Grumback, Pietee, Wang, Osmond, Daher et al., 2002) and higher rates of hospitalization (Baker, Gazmararian, Williams, Scott, Parker, Green et al 2002; Baker, Parker, Williams, & Clark, 1998) among other health consequences (DeWalt & Pignone, 2005). There is also evidence that patients with literacy deficits, compared with other patients, have difficulty understanding and recalling complex medical information (Williams, Baker, Parker, & Nurss, 1998), experience more communication difficulties and have less satisfying medical visits, particularly in terms of the interpersonal and informational aspects of care (Baker, Parker, Williams, Pitkin, Parikh, Coates et al 1996; Bennett, Switzer, Barg, Aguirre, & Evans, 2006; Schillinger, Bindman, Wang, Stewart, Piette et al., 2004). Patients with low literacy skills appear especially vulnerable to medical intimidation and report feelings of shame and humiliation in regard to their literacy deficits (Baker et al., 1996; Parikh, Parker, Nurss, Baker, & Williams, 1996). Given the inherent power differential evident within the patient-physician relationship, it is not surprising that patients with low literacy skills are less likely to be active participants in the medical dialogue and in the decision-making process (Cooper, Beach, & Clever, 2004).
Use of technical terminology by physicians may exacerbate comprehension challenges. Many investigators have documented physician use of medical terminology and consequent patient confusion (Korsch, Gozzi, & Francis, 1968; Svarstad, 1974; Thompson, 1994). Sometimes, use of medical terms is not just a matter of understanding, but one of comfort and familiarity. For instance, when describing sexual or excretory functions, or when referring to parts of the body, some patients prefer the vernacular or slang term while others are more comfortable with a formal medical term (Williams & Ogden, 2004). Physician matching of terms to those first used by the patient, rather than the use of a particular term, was found by Williams and Ogden to lead to a variety of positive outcomes, including increased patient satisfaction, enhanced perceptions of partnership, and greater adherence with medical recommendations (Williams & Ogden, 2004).
Relevance of client literacy to genetic counseling
While the relevance of client literacy to genetics communication is less widely investigated than in general medicine, it is nonetheless important. Genetics technology is relatively new to medicine and rapidly evolving, its language is largely unfamiliar to the lay public, and genetic services are often attendant with uncertainty, anxiety, and decisional distress. Moreover, both clinical genetics visits and genetic counseling sessions tend to be informationally and conceptually dense and largely didactic in nature (Butow & Lobb, 2004; Ellington, Roter, Dudley, Baty, Upchurch, Larson, et al., 2005; Pieterse, van Dulmen, Ausems, Beemer, & Bensing 2005a; Roter, Ellington, Erby, Larson, & Dudley, 2006).
Many studies have linked limited educational background with low interest and use of genetic counseling services (Culver, Burke, Yasui, Durfy, & Press, 2001; Glanz, Grove, Lerman, Gotay, & LeMarchand, 1999). While there are many reasons why poorly educated women do not access genetic services, one may be difficulty understanding genetics-related information and concepts, like probability and cancer risk (Schwartz, Woloshin, & Welch, 1997). Others have documented that a significant portion of information communicated during genetic counseling sessions is lost to recall and subject to confusion and misunderstanding (Chapple, Campion, & May, 1997; Michie, French, Allanson, Bobrow, & Marteau 1997; Watson, Lloyd, Davidson, Meyer, Eeles, Ebbs et al., 1999). Studies in the UK (Dormandy, Michie, Hooper, & Marteau, 2005) and the Netherlands (van den Berg, Timmermans, ten Kate, van Vugt, & van der Wal, 2005) found that poorly educated women were not only less knowledgeable than others about genetic testing, but that the decisions they made in regard to genetic services were less likely to be consistent with their values.
Oral Literacy Demand Framework
While some studies have considered particular aspects of medical communication that present challenges to patients with restricted literacy, there have been few attempts to conceptualize oral literacy demand (i.e. those aspects of interaction that challenge persons with low literacy skills, including use of technical terms, general language complexity, and structural aspects of dialogue such as pacing, density and interactivity) in a comprehensive way (Nielsen-Bohlman et al., 2004). The current study was designed to make a contribution in this area by using videotapes and transcripts of genetic counseling sessions collected as part of the GC Video Project, a national study in which a representative sample of prenatal and cancer genetic counselors were recorded with simulated clients in order to describe the nature and variation of practice in the field. The objectives and design of the study and selected findings are described in more detail elsewhere (Roter, Ellington et al., 2006). The current analysis takes advantage of these data to develop a conceptual framework of the dimensions of oral literacy demand and its consequences for medical interaction and related outcomes.
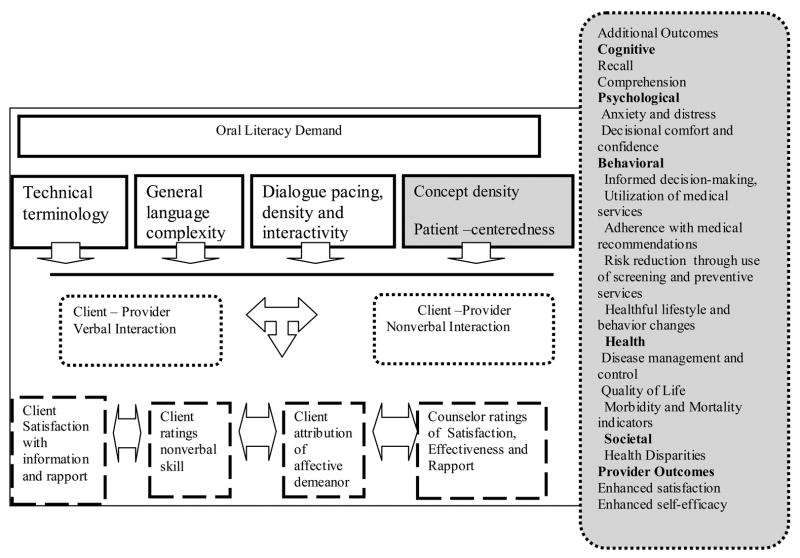
Figure 1 presents the oral literacy demand framework and the pathways through which language characteristics might influence clinician and patient visit perceptions and outcomes. As depicted in the figure, three language elements are specified: (1) technical term use; (2) general language complexity; and (3) structural characteristics of dialogue. For completeness, a fourth element is included in the framework to represent substantive content (concept density) and interaction dynamics (patient-centeredness), although not investigated here.
Figure 1.
Oral Literacy Demand within Medical Dialogue
In the context of the current genetic counseling study, technical word use is represented by a list of 7 genetics terms found in earlier work to be both difficult for poor readers and likely to be encountered during genetic counseling sessions (Erby, Roter, Larson, & Cho, The Rapid Estimate of Adult Literacy in Genetics (REAL-G): A Means to Assess Literacy Deficits in the Context of Genetics, Manuscript under review). We suggest that the greater the use of technical terms, the greater the literacy demand of the session.
The second group of measures reflects general language complexity and is directly parallel to readability assessment of print material and analysis of active versus passive voice (Doak, Doak, & Root, 1996). The readability indices are the same as those used to assess the reading demand of print material, but in this study they are applied to the dialogue transcripts. The proportion of sentences in the passive voice is used as another indicator of language complexity and formality.
Finally, dialogue is presented in three ways: pacing, density, and interactivity. There is some evidence that faster than normal speech speed adversely affects comprehension (Schmitt & Carroll, 1985), and patients in focus groups complain about the fast pace in which information is communicated to them (Bennett et al., 2006). While a patient can explicitly request that the physician slow down or repeat information, patients with low literacy skills are less likely to make requests of this kind than other patients (Bennett et al., 2006). Consequently, we suggest that rapid clinician speech raises demands for oral literacy when conveying complex information.
By dialogue density, we mean the extent of uninterrupted speech delivered by a speaker at a single turn. We know that when information in print material is presented in manageable chunks, only a few items at a time, readers are more likely to remember the information given (Ley, 1982; Doak et al., 1996). In medical visits, there also appears to be an inverse relationship between the overall amount of information given and the proportion of information a patient can recall (Ley, 1982; Roter, Hall, & Katz, 1987). We propose that a corollary in oral exchange is the informational block delivered during uninterrupted speech. Thus, the longer the speech during a clinician speaking turn, the denser the informational chunk, and the greater the oral literacy demand.
The last dialogue dimension is interactivity, defined as the rate of speaker exchange per minute of interaction throughout the session. We suggest that greater interactivity results in a more conversational exchange that provides speaking opportunities for patients, as well as a natural “breather” between informational monologues. In this regard, we consider greater interactivity as an indication of lower oral literacy demand.
In addition to specifying language characteristics of oral literacy demand, we propose pathways by which these may affect the verbal and nonverbal dynamics of medical interaction and a variety of subsequent outcomes in the current simulation study, as well as in actual medical encounters. The effect on verbal communication can be quantified through word use, grammatical summaries, and structural analysis of dialogue, as outlined above. We also suggest that oral literacy demand elements can affect the emotional tone of a medical exchange. Inasmuch as communication carries both verbal and nonverbal content, what a clinician says cannot easily be separated from how a message is conveyed nonverbally or the emotional meaning attributed to it by the receiver (Roter & Hall, 2006). Nonverbal behaviors provide the primary vehicle for emotional expression, including (among others) facial expressivity, smiling, eye contact, head nodding, postural positions (open or closed body posture and forward to backward body lean) and paralinguistic speech characteristics such as speech rate, loudness, pitch, pauses, and speech dysfluencies. All of these accompany speech and are widely recognized as conveying affective and emotional information (Knapp & Hall, 2005).
In considering these types of nonverbal messages, we suggest that the consequences of oral literacy demand on clients may be considered in conceptually distinct ways; through judgments of counselor performance (i.e., the counselor gave me all the information I needed; explained things in a way I could understand; was interested in what I had to say, etc.), judgment of nonverbal skill (i.e., the counselor effectively used eye contact, head nods, smiles, etc.), attribution of emotional state (the counselor was caring, bored, dominating, etc.). These measures are addressed in the current study and represented in the bottom left area of Figure 1.
The consequences of oral literacy demand in medical encounters with actual clients and patients may be expected to fall within a broader array of cognitive, psychological, behavioral, medical, health and social domains, as represented in the shaded area of the figure. Since emotions exert a profound influence on cognition and behavior, including recall, decision making, persuasion, information processing, and interpersonal attitudes (Roter & Hall, 2006; Roter, Frankel, Hall & Sluyter, 2006; Oatley & Jenkins, 1996), we would anticipate the consequences of oral literacy demand to include cognitive outcomes (i.e., recall and comprehension), psychological and affective outcomes (i.e., satisfaction, decisional comfort and confidence, anxiety and distress) behavioral outcomes (i.e., access and utilization of medical services, adherence with medical recommendations, informed decision making, use of screening and preventive services, healthful lifestyle and health promotion activities such as diet modification and smoking cessation, among others), medical and health outcomes reflected in disease management and control, as well as morbidity, mortality and health status effects associated with the previously noted cognitive, psychological and behavioral outcomes), and societal consequences in regard to health disparities apparent in socially and ethnically vulnerable populations.
We would also anticipate outcomes for providers related to the oral literacy demand of their sessions. These include visit satisfaction and self-ratings of performance (ability to effectively educate and counsel the patient), rapport and quality of care through patient-centeredness measures.
Based on the literature cited earlier, we pose three study hypotheses.
The first relates to the relationship among the language elements specified in Figure 1. We hypothesize a positive relationship among all oral literacy demand indicators; the greater the use of technical terms, the more complex the general language, the faster, the denser, and less interactive the session dialogue is likely to be.
The second hypothesis relates to client and spouse evaluations of sessions. We hypothesize an inverse relationship between the oral literacy demand of counseling sessions and simulated clients’ and spouses’ ratings in regard to (a) satisfaction with session communication; (b) counselors’ nonverbal communication skills; and (c) counselors’ affective demeanor.
The third hypothesis relates to counselors’ self-assessments and judgment of the sessions. In light of the predominantly didactic nature of genetic counseling practice (Roter, Ellington et al., 2006; Ellington et al 2005) and relatively little focus in training curriculum on how specifically to convey information to clients with diverse educational, socioeconomic, and ethno-cultural backgrounds (www.abgc.net, Accreditation Requirements, accessed 2-16-2007), we hypothesize no relationship between the oral literacy demand of sessions and genetic counselors’ self-assessment of their performance in: (a) meeting client’s informational needs, (b) establishing interpersonal rapport, and (c) overall session satisfaction.
Methods
Study participants
Ninety-six prenatal and eighty-one cancer genetic counselors participated in the study. The counselors were broadly representative of the National Society of Genetic Counselors membership (Roter, Ellington et al., 2006). The counselors conducted sessions with one of six female simulated clients and three male simulated spouses of African American, Hispanic, and Caucasian ethnicity, who were cross-trained to portray two different cases: (1) a woman seeking pre-amniocentesis counseling based on advanced maternal age (with or without a spouse present) and (2) a woman with a family history of breast and ovarian cancer seeking information about BRCA1/2 genetic testing (with or without a spouse present). Each simulator participated in approximately 28 sessions, ranging from 1 to 8 in a single day.
The simulators were English-speaking but the Hispanic simulated clients spoke in accented English. Four two-hour training sessions were held during which a script outline and case notes were reviewed and the simulators role-played with genetic counselors using their own words.
Simulation scenario
In all cases, the scenario included a female client with a high school education and working class background, and with a deep faith in God but no specific religious affiliation. Her spouse was a 40 year old high school graduate without a similarly strong faith in God. He was supportive of his wife but not particularly worried about genetic risks, although he did not have any more prior exposure or knowledge of genetics than his wife. Neither client nor spouse was prepared to make a decision regarding genetic testing at the session.
Common visual aids were made available for use in the sessions and counselors were told only to limit the time of their sessions as they would in their own practices.
Procedures
The genetic counselors were recruited through the National Society of Genetic Counselors general and special interest group web based list-services prior to their 2003 and 2004 national meetings and through vendor tables at the meeting. The study was described as a study of genetic counseling process and the factors influencing client outcomes, and counselors were told that participation in the project included videotape recording of a routine counseling session with a simulated client and the completion of a variety of questionnaires. Depending on the counselor’s area of expertise, the task would be pre-amniocentesis counseling or pre-test counseling for breast and ovarian cancer susceptibility. As an incentive for participation, counselors were offered $75.00 and a t-shirt with the GCVideo Project logo.
The study was approved by the Committee on Human Research of the Johns Hopkins Bloomberg School of Public Health, and all counselors gave full informed consent for their participation. Counselors were randomly assigned to clients by ethnicity and whether or not a male spouse would be present. They were then escorted to one of six rooms prepared for video recording. Following the session, both the counselor and the simulated client(s) returned to the project suite to independently complete post-session questionnaires.
Due to a variety of technical difficulties, 25 videotapes were of insufficient quality to be transcribed. Of the 152 videotapes that were transcribed and used in the current analysis, 89 address prenatal and 63 cancer genetic counseling. A professional transcription service was used and each transcript was reviewed a second time for completeness.
Measures
Oral Literacy Demand
Genetics terminology
In earlier work, we developed a print-based health literacy screening tool, the rapid estimate of adult literacy in genetics (REAL-G), patterned after the REALM but comprised of 63 genetics-related words. The word list was generated through our own genetic counseling experience, a review of common genetic counseling educational aids, and a content analysis of a sample of genetic counseling session transcripts to verify use in both the prenatal and cancer context. Based on a validation study, we found that an 8-word short form of the REAL-G worked as well as the full instrument and showed strong concurrent validity to the REALM, as well as predictive validity to recall; subjects missing at least 3 of the 8 REAL-G words (indicating below 6th grade reading level), scored significantly lower on a recall test after viewing a videotape of a genetic counseling session. (For more detail regarding concurrent and predictive validity of the REAL-G, see Erby et al., manuscript under review). The REAL-G short form includes the following eight words: variation, susceptibility, abnormality, sporadic, hereditary, mutation, chromosome, and genetic.
In the current study, we used a qualitative data software package (Atlas-Ti), to track every use of the 21 multisyllabic REAL-G words from the full instrument in the complete data set of 152 prenatal and cancer genetic counseling session transcripts, without reference to speaker. The pattern of word use within sessions was very similar to that found in the subset of short-form REAL-G words. In addition, in subsequent analysis we found that the relationships produced with the full multisyllabic list and the short list to language and dialogue elements were very similar. Since a simpler measure is always preferred over a more extensive one when the results are comparable, we present the short word list analysis here, with the exception of the word ‘genetic’ which was so ubiquitous as to make a count meaningless. Based on these results and the validity study mentioned above, we regard the REAL-G 7-word measure used in this study as a proxy for a broad list of technical terms often used in genetic counseling sessions and potentially problematic for individuals with restricted literacy.
Several variables were derived from the REAL-G measure: 1) the total number of times REAL-G words were used in the sessions, including one-time use and repetitions; 2) the number of different REAL-G words used in each session, without regard for number of repetitions; 3) the average number of times each REAL-G word was repeated within a session, and 4) the ratio of REAL-G words to the total transcript word count.
General language complexity
General language complexity and readability measures were generated for each counseling session transcript using Microsoft Word “grammar summary statistics.” These include: the total transcript word count, the average number of words per sentence, the percentage of transcript sentences in the passive voice, the Flesch Reading Ease Score ((206.835 − (1.015 × average sentence length) − (84.6 × average number of syllables per word)) and the Flesch-Kincaid (F-K) Reading Grade Level Score ((.39 × average sentence length) + (11.8 × average number of syllables per word) − 15.59)). The percentage of transcript sentences in the passive voice was used as a proxy for conversational formality. Although not directly provided with summary statistics, the average number of syllables per word (ASW) was extrapolated from the Flesch Reading Ease Score (ASW = (Flesch Reading Ease Score − 206.835) + (1.015 × Average sentence length)/(−84.6)) (Microsoft Office, 2003).
Structural measures of dialogue: pacing, density, and interactivity
Dialogue pace was estimated by the rate of speech speed in syllables per second of session time, as represented in the formula: Dialogue pace = (ASW × total transcript word count)/(session length in seconds). Length in seconds was derived from the session videotape.
Dialogue density is defined as the number of statements by each speaker divided by the number of speaker turns. The number of statements by each speaker was derived from application of the Roter Interaction Analysis System (RIAS) to the videotapes as part of the larger study. The RIAS unitizes speech as the smallest expression to which a meaningful code can be assigned, generally a complete thought, expressed by each speaker throughout a session. More detail regarding assignment of statements to mutually exclusive and exhaustive code categories that reflect the content and form of medical dialogue is available elsewhere (See www.rias.org for a bibliography of over 150 RIAS studies); in the current study only the total statement count by speaker is used (a variable with coder reliability of greater than .90) (Roter, Ellington et al., 2006). The number of speaker turns, defined as a continuous block of uninterrupted speech of a single speaker, was derived from the session transcripts. Separate turn density calculations were made for the counselor, client, and client spouse.
Dialogue interactivity was represented by the rate per minute at which the counselor exchanged the floor (with either the client or spouse), calculated as the number of counselor turns divided by the session length in minutes.
Outcomes
Post-Session Ratings by Counselors. Counselors completed the following scales after the videotape session: Satisfaction with the session in regard to: (a) Interpersonal rapport (8 items; Cronbach’s Alpha = .83) and (b) informational efficacy in meeting the needs of the client (3 items, Alpha =.74). The scales were moderately correlated with one another (Pearson correlation = .36, p<.0001). In addition, counselors rated their overall satisfaction with the session (1 item).
Post-Session Ratings by Simulated Clients and Simulated Client Spouses. The simulated client (and simulated spouse when present) independently rated the session immediately upon completion of the session. They were not trained to prefer any particular verbal or nonverbal behavior to any others.
Satisfaction with session communication: A simulated client satisfaction questionnaire used in prior work was modified for use in the current study (Roter, Hall, Kern, Barker, Cole KA, & Roca, 1995). The 14 items, measured on a 6-point Likert scale, demonstrated good internal reliability (Alpha = .96) and reflected informational and interpersonal aspects of communication.
Nonverbal behavior: Judgment of the genetic counselor’s nonverbal communication effectiveness was assessed on a 6-point Likert scale (not at all effective to very effective) for the following behaviors: eye contact; smiles; head nods; appropriateness of facial expressions to the communication; body lean; seating position; use of touch; responsiveness to nonverbal cues; responsiveness to verbal cues; and, effective use of pauses and silence (10 items; Alpha = .91).
Affective demeanor. Judgments of the genetic counselor’s demeanor were assessed using 15 semantic differential items (e.g., caring/uncaring; engaged/bored; 15 items with Alpha = .95).
While the three scales shared a good deal of variance, (Pearson correlations ranged from .78 – .83, p<.0001), they were treated separately in this analysis since they were conceptually distinct as described in our Figure 1 framework, and showed some differences in their relationship to other variables.
Relationship between counselors’ and simulators’ ratings
Counselors’ self ratings and simulators’ ratings were largely uncorrelated with the following exceptions. Counselors’ rating of rapport was significantly related to spouse ratings of affective demeanor (r = .27, p<.05); the relationship to client ratings were suggestive, but not significant (r = .14, p<.11) and a similar relationship was evident between counselors’ satisfaction and clients’ ratings of demeanor (r = .13, p<.10).
Analysis
Statistical analyses were conducted using Intercooled Stata 8.2 (Stata Corporation, 2004). Descriptive statistics were calculated on all study variables, including the mean, range, and standard deviation. Given the dearth of studies examining the elements of oral literacy demands within the medical dialogue, the general analytic approach for all three hypotheses was an exploratory bivariate analysis. Pearson’s correlation coefficients were first calculated between each pair of variables in the following categories: readability statistics, interaction structure, and use of key genetic terms. Pearson’s correlations were also calculated between variables within each category of oral literacy demand and each one of the three types of simulated client ratings of the sessions. These analyses were conducted separately for female simulated clients and for their male counterparts (when present). Likewise, correlation coefficients were calculated for items within all three categories of oral literacy demand paired with genetic counselor self-ratings of the session.
Under usual circumstances, we would account for the clustering of clients within counselors to estimate a counselor effect, assuming a characteristic counseling style would be evident across all of the counselor’s clients. However, the use of simulated clients in this study was intended to standardize the case from one counselor to the next by considering the simulators as interchangeable. Our previous analysis found few differences between individual simulated clients (Erby, 2005). Consequently, we chose to disregard the clustering and present the more straightforward analysis.
Results
Variation in language
Use of REAL-G words
Counselors varied a great deal in the use of the REAL-G words, as shown by Table 1. The most commonly used word, “chromosome” was used in 85% (n= 129) of the sessions, repeated on average 27 times in each session and as often as 78 times. The least frequently used word “susceptibility” was found in 13% of sessions and was repeated an average of 5 times. Also reflected in the table is a summary of REAL-G word use throughout the session transcripts. An average session used three different REAL-G words although as many as 6 of the words were used together in a single session. Some combination of the terms were used an average of 39 times per session, with a range from 0 to 129 times (there were 2 sessions in which no REAL-G words were used). As a matter of perspective, it is interesting to note that total use of REAL-G words comprised only slightly more than 1/2 % (.0058) of all transcript words, with a range of 0 to 4%.
Table 1.
The use of REAL-G words in 152 genetic counseling sessions
| REAL-G words | Overall REAL-G word use per session (mean repetitions of word) | Range of REAL-G use per session | Number of Sessions in which the word is used (% of sessions) |
|---|---|---|---|
| susceptibility | 97 (5.1) | 1–15 | 19 (13%) |
| variation | 81 (2.5) | 1–10 | 32 (21%) |
| abnormality | 150 (4.4) | 1–13 | 34 (22%) |
| sporadic | 166 (3.7) | 1–17 | 45 (30%) |
| hereditary | 552 (8.2) | 1–45 | 67 (44%) |
| mutation | 1357 (15.4) | 1–87 | 88 (58%) |
| chromosome | 3450 (26.8) | 1–78 | 129 (85%) |
|
REAL-G Word Summary
Overall REAL-G use Different REAL-G words used REAL-G word repetitions ratio of REAL-G to all session words |
Mean (SD)
39 (23) 3 (1) 20 (13) 0.0058 (.005) |
Range
0–129 0–6 3 –78 0 – 0.04 |
|
General language complexity
The readability statistics applied to the 152 session transcripts reflect an average Flesch-Kincaid Reading Level of 6.7, with a range from 4th to 11th grade, as reflected in Table 2. The average number of syllables per word was a modest 1.5, and only 4% of dialogue sentences were in the passive tense; however, sentences were long, averaging over 13 words per sentence (range 8.6 – 24.7).
Table 2.
Means (SD) and Ranges of Grammar indicators and Dialogue Structure
| Mean (SD) | Range | |
|---|---|---|
| Language Complexity | ||
| Average syllables per word | 1.45 (.05) | 1.35–1.57 |
| Average words per sentence | 13.6 (2.9) | 8.6–24.7 |
| F-K reading grade level | 6.7 (1.1) | 4.3–11.0 |
| Flesch Reading Ease Score | 70.5 (4.1) | 58.5–79.7 |
| % of passive sentences | 0.04 (0.02) | 0.01–0.11 |
| Dialogue Pacing | ||
| Length of visit (minutes) | 48.3 (13.8) | 23–92.2 |
| Syllables per second | 3.8 (0.6) | 1.7 – 4.8 |
| Words per second | 2.5 (.37) | 1.1 – 3.3 |
| Dialogue Density | ||
| Number of counselor turns | 117 (58) | 22 – 382 |
| Number of client turns | 109 (59) | 17 – 382 |
| Number of spouse turns | 23 (17) | 0 – 92 |
| Density of counselor turns (number of thoughts expressed per turn) | 6.8 (3.0) | 2.3 – 18.8 |
| Density of client turns (number of thoughts expressed per turn) | 1.4 (.52) | .49 – 3.5 |
| Density of spouse turns (number of thoughts expressed per turn) | 1.5 (.88) | 0 – 4.5 |
| Dialogue Interactivity | ||
| Interactivity (counselor turns per minute) | 2.3 (1.0) | 0.6–6.0 |
Dialogue pacing, density, and interactivity
Also reflected by Table 2 are a variety of dialogue structures. The sessions were quite long with an overall average of 48.3 minutes (range 23–92 minutes). Dialogue pace was estimated by a calculation of number of words expressed per session second (averaged 2.5; range 1.1 – 3.3) and number of syllables expressed per second (3.8; range 1.7– 4.8). Since these measures were based on overall session length and word analysis, they do not differentiate the contribution of individual speakers.
The number of speaker turns is equivalent in dyadic exchanges but there is far less symmetry in 3-way conversations, as reflected by Table 2. Counselors averaged 117 speaking turns over all sessions; 125 when with clients alone and 107 when in sessions that included a client and spouse. Clients averaged 109 turns; 124 turns in sessions without a spouse and 90 when the spouse was present. Spouses averaged 23 turns. These numbers reflect a primary pattern of exchange in which both clients and spouse directed their statements to the counselor, eliciting a counselor response, rather than to one another. The rate of counselor turn taking averaged a little over two turns per session minute, but this varied a good deal ranging from less than .6 to 6.0 turns per minute.
Counselors’ communication was substantially denser than that of either client or spouse. On average, counselors made almost seven statements per speaking turn (range 2.3 – 18.8), while clients and spouse communicated more sparingly, averaging 1.4 and 1.5 statements per turn, respectively.
The relationships between REAL-G word use, language complexity, and dialogue characteristics
As is evident in Table 3, sessions with a high frequency of REAL-G word use are long and demanding in terms of language complexity as reflected in readability indices, but show no relationship to dialogue structure. The number of different REAL-G words used (regardless of repetitions) presents a different pattern; while these sessions are also long, they are characterized by slow speech and dense counselor turns. There is little relationship between this measure and language complexity, in fact, there is a tendency toward the use of fewer multi-syllabic words in these sessions. The relative contribution of REAL-G words to the total dialogue shows the most consistent relationships to both language and dialogue characteristics, even though as noted earlier REAL-G words comprised only a small proportion of total transcript words (averaging 1/2%). Nevertheless, sessions with a greater ratio of REAL-G to total words in the dialogue were shorter and characterized by complex language, fewer and denser counselor turns, slow speech speed, and low interactivity.
Table 3.
Correlations between readability statistics, interaction structure and use of key genetic terms
| All genetic terms | # of different terms | Mean repetitions per term | Ratio of REAL-G to all transcript words | Number of counselor turns | Density of counselor turns | Interactivity (turns per minute) | |
|---|---|---|---|---|---|---|---|
| Language Complexity | |||||||
| Average syllables per word | .16 * | −.15+ | .13 | .12 | .16 * | −.30 *** | .22** |
| Average words per sentence | .10 | .05 | .02 | .20* | −.51*** | .57*** | −.58*** |
| F-K reading grade level | .19* | −.03 | .09 | .27** | −.47 *** | .47 *** | −.54*** |
| Flesch Reading Ease Score | −.24** | .11 | −.15+ | −.29*** | .23** | −.16+ | .27** |
| % of passive sentences | −.006 | .04 | −.06 | .08 | −.36 *** | .40 *** | −.39*** |
| Dialogue Pacing | |||||||
| Length of visit (minutes) | .25** | .30*** | −.06 | −.18* | .53 *** | −.11 | .07 |
| Syllables per second | −.01 | −.18* | .13 | −.26** | .38 *** | −.30 *** | .47*** |
| Dialogue Density | |||||||
| Number of counselor turns | .11 | .05 | .06 | −.25** | _ | −.67 *** | .83*** |
| Density of counselor turns | .10 | .20* | −.12 | .40*** | −.67 *** | _ | −.74*** |
| Dialogue Interactivity | |||||||
| Interactivity(counselor turns/minute) | −.03 | −.08 | .07 | −.24** | 83*** | −.74*** | _ |
p < .10;
p< .05;
p< .01;
p<.001
Also reflected in Table 3 is the relationship among dialogue elements. Session interactivity, the rate of turn exchange per session minute, was associated with lower levels of language complexity, faster speech speed and less dense counselor turns. Turn density was largely inverse to interactivity; it was associated with greater language complexity and slower speech speed. Neither interactivity nor turn density were significantly associated with session length. The number of speaking turns was related to session length, turn density and interactivity; the more turns exchanged the longer the visit, the less dense the turns, and the more interactive the session.
Genetic Counselor self-ratings of communication effectiveness
As seen in Table 4, the counselors’ overall satisfaction with the session was associated with greater use of different REAL-G words, fewer repetitions of these words, and slower speech speed. Counselor self-assessment of how well they met the information needs of the simulated clients was negatively related to both overall REAL-G word use and REAL-G repetitions, but not the number of different REAL-G words. Informativeness was also negatively related to language complexity reflected in the readability indices and the use of long, passive sentences. Finally, the counselors’ rating of interpersonal rapport was related to greater use of multi-syllabic words and a tendency to fewer repetitions of REAL-G words.
Table 4.
Correlations between counselors’ self-ratings and session communication
| Genetic Counselor Self-Ratings (n=157) | |||
|---|---|---|---|
| Literacy Measures | Visit Satisfaction | Informativeness | Interpersonal Rapport |
| REAL-G Measures | |||
| All REAL-G words | .00 | −.21* | −.11 |
| Unique REAL-G words | .20* | −.01 | .08 |
| Mean REAL-G repetitions | −.21* | −.20* | −.16+ |
| Ratio of REAL-G words to total transcript words | .10 | −.11 | .07 |
| Language Complexity | |||
| Average syllables per word | .04 | −.12 | .20* |
| Average words per sentence | −.06 | −.22* | −.08 |
| Flesch-Kincaid Reading Grade level | −.05 | −.30*** | .01 |
| Flesch Reading Ease | .01 | .28** | −.14 |
| % passive sentences | .06 | −.21* | .14 |
| Dialogue Pacing | |||
| Session length | −.06 | 0 | −.08 |
| Syllables/second | −.20* | −.12 | −.09 |
| Dialogue Density | |||
| Number of turns | −.03 | .01 | −.03 |
| Turn density | .04 | −.09 | .01 |
| Dialogue Interactivity | |||
| Interactivity (turns per minute) | −.07 | .02 | −.02 |
p < .10;
p< .05;
p< .01;
p<.001
Simulated Clients’ ratings of the sessions
Table 5 presents simulated client and spouse ratings of satisfaction with the counselors’ verbal communication, nonverbal effectiveness, and affective demeanor. The pattern of ratings was similar for both clients and spouses; satisfaction and nonverbal effectiveness was related to longer sessions, lower language complexity reflected in both readability indices as well as the use of shorter and fewer passive sentences, lower turn density, greater number of turns overall, and greater interactivity. Both clients and spouse ratings of the counselors’ affective demeanor were associated with lower turn density and more turns. However, the spouses’ ratings were more strongly related to dialogue elements than those of the client, and also included an association between demeanor and interactivity. Female clients seemed somewhat more sensitive to use of the passive voice than were spouses.
Table 5.
Correlations between literacy measures and simulated client ratings of communication effectiveness
| Simulated client ratings (n=147) | Simulated spouse ratings (n=63) | |||||
|---|---|---|---|---|---|---|
| Literacy Measures | Nonverbal behavior | Satisfaction with communication | Affect | Nonverbal behavior | Satisfaction with communication | Affect |
| REAL-G Variables | ||||||
| All REAL-G words | −.05 | −.06 | −.08 | −.05 | .06 | .00 |
| Unique REAL-G words | −.02 | −.05 | −.13 | .01 | .15 | .00 |
| Mean REAL-G repetitions | −.03 | .00 | .03 | .05 | −.04 | .09 |
| Ratio of REAL-G words to total transcript words | −.15+ | −.18+ | −.07 | −.19 | −.03 | −.22 |
| Language Complexity | ||||||
| Average syllables per word | −.07 | −.10 | −.09 | −.13 | −.12 | −.05 |
| Average words per sentence | −.19* | −.21* | −.08 | −.21+ | −.08 | −.10 |
| Flesch-Kincaid Reading Grade level | −.23** | −.28*** | −.12 | −.31* | −.15 | −.13 |
| Flesch Reading Ease | .21* | .26** | .14+ | .31* | .19 | .13 |
| % passive sentences | −.24** | −.29*** | −.19* | −.27* | −.24+ | −.16 |
| Dialogue Pacing | ||||||
| Session length | .15* | .15* | .08 | .20+ | .24* | .11 |
| Syllables/second | .02 | .00 | .00 | .04 | .03 | .09 |
| Dialogue Density | ||||||
| Number of turns | .31*** | .35*** | .15+ | .43** | .40** | .35** |
| Turn density | −.35*** | −.40*** | −.19* | −.39** | −.39** | −.41** |
| Interactivity | ||||||
| Interactivity (turns per minute) | .28** | .30*** | .12 | .38** | .35** | .36** |
p < .10;
p< .05;
p< .01;
p<.001
Discussion
Our study goes beyond language complexity and related readability indices applied to dialogue to include novel approaches to both the quantification of technical term use and the exploration of dialogue dimensions of pacing, density and interactivity. Some of our ideas regarding dialogue density and dialogue interactivity have parallels to print assessment as suggested by Doak and colleagues in regard to information chunking and interactive strategies to actively engage readers (Doak et al., 1996). In regard to chunking, Doak and colleagues suggest that readers can not comfortably process more than 5 pieces of information at a time; in our study the average turn density for counselors was 6.8 statements, suggesting that the information load each time a counselor spoke may exceed what can be easily remembered. We also note a parallel in terms of interactivity. For instance, Doak and colleagues suggest that reader engagement with print material may be enhanced through question/answer formats, quizzes, brainstorming exercises, and risk self assessment. While the mode of interactivity is obviously different in print and dialogue, we suggest that the rate of speaker exchange similarly demands active attention and engagement of speakers in a reciprocal process of informational evaluation and response.
Overall, we found a positive relationship among oral literacy demand indicators. In regard to our first study hypothesis, we found that the greater the use of REAL-G words, the more complex general language was in terms of readability indices and the denser and less interactive the session dialogue. Speech speed, however, did not increase with other oral literacy demand elements as expected; in fact, counselors tended to slow down when using more REAL-G words and when communicating through infrequent, dense turns. We found an interesting contrast in how REAL-G words were used. Sessions marked by many different REAL-G terms tended to be long with the counselors delivering a good deal of information in dense turns, at a slow pace. In contrast, the sessions characterized by high REAL-G words relative to other interaction were short with information presented slowly using complex language, over fewer speaking turns, thus marking the sessions as dense and non-interactive. These sessions may reflect a narrow focus on the technical and biomedical aspects of genetics and testing creating a “lecture like” feel to the interaction.
On the whole, both simulated clients’ and spouses’ ratings were inversely related to oral literacy demand, consistent with the second study hypothesis. Clients’ and spouses’ ratings of satisfaction and counselors’ nonverbal effectiveness were lower when the counselors used complex passive language with dense, long speaking turns and low dialogue interactivity. For spouse, these measures also related to negative ratings of counselors’ affective demeanor. Essentially, the simulators did not like it when counselors delivered, what for all intents and purposes, were lectures. The one aspect of literacy demand that clients did not consistently evaluate negatively was REAL-G word use; overall frequency of these words were not related to session ratings, however, when the use of REAL-G words was high relative to other interaction, simulated client ratings were negative. This suggests it was not the use of the words that created a negative impression on the simulators, but the relative emphasis on these words in regard to everything else that might be discussed during the session. In other analysis of this data we found that simulated clients’ satisfaction with communication, the counselor’s affective demeanor, and the counselor’s use of nonverbal skills was highest when the counselors addressed emotional and psychosocial issues during their sessions, along with the related biomedical issues (Roter, Ellington et al., 2006).
The third study hypothesis anticipated no relationship between the oral literacy demand of sessions and genetic counselors’ satisfaction and self-assessment of their performance in meeting client’s informational needs and establishing interpersonal rapport. We were wrong. Counselor’s self-ratings of informativeness were inversely related to overall REAL-G use and language complexity, including readability indices and use of the passive voice. This suggests that counselors recognized that going into “lecture mode” as described above was an ineffective way to educate a client.
Counselors’ ratings of rapport were higher when the counselor used more multi-syllabic words. We are not sure what to make of it. It is possible that a sense of connection with the client, perhaps related to an assumption of similarities in background and a breadth of general knowledge, led to fewer efforts at simplification. This interpretation is also consistent with the trend linking rapport and fewer REAL-G repetitions, again suggesting that these exchanges may be at a less basic level than others.
It is interesting to note that none of the counselors’ self-ratings were correlated with dialogue elements (except speech speed), suggesting that they were not very sensitive to the direct impact of interactivity and turn density on the communication experience of their clients. In fact, as evidenced by the scant relationships between counselors’ self-ratings and simulator ratings, it seems safe to conclude that counselors were largely unaware of their clients’ perceptions. To some extent, this may be a function of the counselors’ strong didactic focus; the counselors were “on message” so much that they may have lost sight of the importance of engaging the client and spouse in a conversation.
The patterns of associations found in this study suggest that client and spouse ratings were primarily affected by how information was communicated rather than the actual content. In contrast, counselors’ focus seemed to be largely on content and not the interactive dynamic through which the message was delivered. Several aspects of counselors’ delivery may have acted to widen the gap between counselor and client in this regard. For instance, when concentrating, people tend to look away; they inhibit eye contact and shift eye gaze as a way to sharpen their attention and enhance information retrieval (Galluscio & Paradzinski, 1995). It is possible, then, that just at the time when clients were looking to the counselors for affective cues, the counselors were looking away. Consequently, the counselors may have created an impression of impersonality and detachment, much like someone delivering a lecture, as they struggled to articulate their message. This may be interpreted by clients searching for affective cues as a lack of attentiveness and nonverbal insensitivity. The counselors may not be fully aware of this impression because they are, in fact, distracted by the challenges of message construction. The focus “on message” may translate to a shift of focus away from the client.
Limitations
Several limitations of our study need to be considered. While the study included a large number of practicing genetic counselors, the counseling sessions were artificial in that they were videotaped at a national conference and the clients were actors. Nevertheless, the majority of counselors reported that their session did not differ very much from their usual practice (Roter, Ellington et al., 2006). Moreover, the session length was comparable to reports of actual practice; the prenatal sessions averaged 45 minutes (range = 25 to 83 minutes) while cancer sessions lasted 50 minutes (range = 23 to 92 minutes) (Butow & Lobb, 2004; Pieterse, van Dulmen, Ausems, Beemer & Bensing, 2005b; Hamby, 2001; Kemel, 2000).
Also related to issues of generalizability and reliability is how consistently the simulators performed across sessions and the degree to which their performance was similar to the behavior of actual genetic counseling clients. Indications from our analysis of simulator reliability found that performance did not vary significantly from session to session or over time (Erby, 2005). It is possible that our actors developed and applied different criteria to their evaluations than actual clients since they are, after all actors. Moreover, there are some judgments that would be too difficult for the simulators. For this reason, we did not have the simulators attempt to recall specific information communicated during the sessions. Repeated exposure to the same information may have also acted to diminish the clients’ focus on the substantive content of the sessions.
While the simulators described themselves as having a high school education and as being unfamiliar with genetic concepts, we do not know if their behavior was similar to that of an actual client with restricted literacy. The actors were trained not to ask questions (other than those that were scripted) or initiate discussion unless the counselor explicitly encouraged them to elaborate concerns. In this regard, we believe their behavior was consistent with what would be expected of clients with limited educational background.
A question may be raised in regard to our REAL-G word count. It is possible that the simulators might have repeated genetic terms used by the counselor and thereby inflated the transcript assessment of REAL-G word use. We checked this by sampling 21 (10 cancer and 11 prenatal) session transcripts in which overall REAL-G use was especially high. We found that the simulators infrequently used REAL-G words and any contribution they made to the REAL-G count was minimal.
IMPLICATIONS
Just as print material can be made more reader-friendly and effective following established guidelines (Doak et al., 1996), the medical dialogue may also be made more effective and “patient-friendly” by attending to language characteristics and interactivity. The relationships found among the oral literacy dimensions suggest that genetic counselors need to monitor not only their vocabulary and the complexity of their language but also the interactive structure of their dialogue. These findings are also likely to apply to the broader context of medical dialogue, and in this regard, we encourage physician and genetic counselor training programs to include a focus on enhanced interactivity as well as the simplification of language.
Acknowledgments
Funding for this research was provided by the National Human Genome Research Institute, 1R01HG002688-01A1. We are grateful to the many genetic counselors that devoted their time and energy to participate in the Genetic Counseling Video Project and the hard work and enthusiasm of the study’s nine simulated clients. We would also like to thank Rita Johnson, Colleen Brown, Juhee Cho, and Julia Morgan for their help in preparing and coding the transcripts and Saul Waller for his help in the literature review.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Debra L. Roter, Johns Hopkins School of Hygiene & Public Health, droter@jhsph.edu
Lori H Erby, Johns Hopkins, lerby@jhsph.edu.
Susan Larson, Johns Hopkins, slarson@jhsph.edu.
Lee Ellington, University of Utah.
References
- Baker DW, Parker RM, Williams MV, Pitkin K, Parikh NS, Coates W, et al. The health care experience of patients with low literacy. Archives of Family Medicine. 1996;5(6):329–334. doi: 10.1001/archfami.5.6.329. [DOI] [PubMed] [Google Scholar]
- Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. Journal of General Internal Medicine. 1998;13(12):791–798. doi: 10.1046/j.1525-1497.1998.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. American Journal of Public Health. 2002;92(8):1278–1283. doi: 10.2105/ajph.92.8.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett IM, Switzer J, Barg F, Aguirre A, Evans K. “Breaking it down”: patient-clinician communication and prenatal care among African American women of low and higher literacy. Annals of Family Medicine. 2006;4(4):334–340. doi: 10.1370/afm.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butow PN, Lobb EA. Analyzing the process and content of genetic counseling in familial breast cancer consultations. Journal of Genetic Counseling. 2004;13(5):403–424. doi: 10.1023/B:JOGC.0000044201.73103.4f. [DOI] [PubMed] [Google Scholar]
- Chapple A, Campion P, May C. Clinical terminology: Anxiety and confusion amongst females undergoing genetic counseling. Patient Education and Counseling. 1997;32(1–2):81–91. doi: 10.1016/s0738-3991(97)00065-7. [DOI] [PubMed] [Google Scholar]
- Cooper LA, Beach MC, Clever SL. Participatory decision-making in the medical encounter and its relationship to patient literacy. In: Schwartzberg J, Van Geest J, Wang C, Gazmararian J, Parker R, Roter D, Rudd R, Schillinger D, editors. Understanding Health Literacy: Implications for Medicine and Public Health. Chicago, IL: AMA Press; 2004. pp. 101–118. [Google Scholar]
- Culver J, Burke W, Yasui Y, Durfy S, Press N. Participation in breast cancer genetic counseling: The influence of educational level, ethnic background, and risk perception. Journal of Genetic Counseling. 2001;10(3):215–231. [Google Scholar]
- Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, et al. Rapid estimate of adult literacy in medicine: A shortened screening instrument. Family Medicine. 1993;25(6):391–395. [PubMed] [Google Scholar]
- Davis TC, Arnold C, Berkel HJ, Nandy I, Jackson RH, Glass J. Knowledge and attitude on screening mammography among low-literate, low-income women. Cancer. 1996;78(9):1912–1920. doi: 10.1002/(sici)1097-0142(19961101)78:9<1912::aid-cncr11>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- DeWalt DA, Pignone M. Health literacy and health outcomes: Overview of the literature. In: Schwartzberg J, Van Geest J, Wang C, Gazmararian J, Parker R, Roter D, Rudd R, Schillinger D, editors. Understanding Health Literacy. Chicago: AMA Press; 2005. pp. 205–227. [Google Scholar]
- Dexter ER, LeVine SE, Velasco PM. Maternal schooling and health-related language and literacy skills in rural Mexico. Comparative Education Review. 1998;42(2):139–162. doi: 10.1086/447493. [DOI] [PubMed] [Google Scholar]
- Doak C, Doak L, Root J. Teaching Patients with Low Literacy Skills. 2. Philadelphia, PA: J. B. Lippincott Company; 1996. [Google Scholar]
- Dormandy E, Michie S, Hooper R, Marteau TM. Low uptake of prenatal screening for Down syndrome in minority ethnic groups and socially deprived groups: A reflection of women’s attitudes or a failure to facilitate informed choices? International Journal of Epidemiology. 2005;34(2):346–352. doi: 10.1093/ije/dyi021. [DOI] [PubMed] [Google Scholar]
- Ellington L, Roter DL, Dudley W, Baty BJ, Upchurch R, Larson S, et al. Communication analysis of BRCA1 genetic counseling. Journal of Genetic Counseling. 2005;14(5):377–386. doi: 10.1007/s10897-005-3660-3. [DOI] [PubMed] [Google Scholar]
- Erby LAH. Doctoral Dissertation. The Johns Hopkins Bloomberg School of Public Health; 2005. Understanding the genetic counseling process: The use of simulated clients in examining the genetic counseling interaction. [Google Scholar]
- Farmer SA, Roter DL, Higgenson IJ. Chest pain: Communication of symptoms and history in a London emergency department. Patient Education and Counseling. 2006;63(1–2):138–144. doi: 10.1016/j.pec.2005.09.009. [DOI] [PubMed] [Google Scholar]
- Galluscio EH, Paradzinski P. Task specific conjugate lateral eye movements. Perceptual and Motor Skills. 1995;81:755–762. doi: 10.2466/pms.1995.81.3.755. [DOI] [PubMed] [Google Scholar]
- Gazmararian JA, Baker DW, Williams MV, Parker RM, Scott TL, Green DC, et al. Health literacy among Medicare enrollees in a managed care organization. Journal of the American Medical Association. 1999;281(6):545–551. doi: 10.1001/jama.281.6.545. [DOI] [PubMed] [Google Scholar]
- Gee JP. Social linguistics and literacies. London: Taylor and Francis Ltd; 1996. [Google Scholar]
- Geller G, Doksum T, Bernhardt BA, Metz SA. Participation in breast cancer susceptibility testing protocols: Influence of recruitment source, altruism, and family involvement on women’s decisions. Cancer Epidemiology Biomarkers and Prevention. 1999;8(4):377–382. [PubMed] [Google Scholar]
- Glanz K, Grove J, Lerman C, Gotay C, LeMarchand L. Correlates of intentions to obtain genetic counseling and colorectal cancer genetic testing among at-risk relatives from three ethnic groups. Cancer Epidemiology Biomarkers and Prevention. 1999;8(4):329–336. [PubMed] [Google Scholar]
- Hallowell N, Green JM, Statham H, Murton F, Richards M. Recall of numerical risk estimates and counselees’ perceptions of the importance of risk information following genetic counseling for breast and ovarian cancer. Psychology, Health and Medicine. 1997;2(2):149–159. [Google Scholar]
- Hamby L. Master’s thesis. The Johns Hopkins School of Hygiene and Public Health; 2001. Discussions of personal meaning in pre-amniocentesis genetic counseling. [Google Scholar]
- HHS U.S. Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. Washington, DC: U.S. Department of Health and Human Services; 2000. [Google Scholar]
- Kemel Y. Master’s thesis. The Johns Hopkins School of Hygiene and Public Health; 2000. What happens during the prenatal genetic counseling session: Exploratory study of genetic counseling. [Google Scholar]
- Kessler S. Psychological aspects of genetic counseling: VI. A critical review of the literature dealing with education and reproduction. American Journal of Medical Genetics. 1989;34(3):340–353. doi: 10.1002/ajmg.1320340310. [DOI] [PubMed] [Google Scholar]
- Knapp ML, Hall JA. Nonverbal Communication in Human Interaction. 6. Belmont, CA: Wadsworth; 2005. [Google Scholar]
- Korsch BM, Gozzi EK, Francis V. Gaps in doctor-patient communication: I. Doctor-patient interaction and patient satisfaction. Pediatrics. 1968;42(5):855–871. [PubMed] [Google Scholar]
- Kutner M, Greenberg E, Baer J. (NCES 2006-470). U.S. Department of Education. Washington, DC: National Center for Education Statistics; 2005. A first look at the literacy of America’s adults in the 21st century. Washington, DC: U.S. Government Printing Office. [Google Scholar]
- Lerman C, Daly M, Masny A, Balshem A. Attitudes about genetic testing for breast-ovarian cancer susceptibility. Journal of Clinical Oncology. 1994;12(4):843–850. doi: 10.1200/JCO.1994.12.4.843. [DOI] [PubMed] [Google Scholar]
- LeVine R, Dexter E, Velasco P, LeVine S, Joshi A. Maternal literacy and health care in three countries: a preliminary report. Health Transition Review. 1994;4(2):186–191. [PubMed] [Google Scholar]
- Ley P. Patients’ understanding and recall in clinical communication failure. In: Pendleton D, Hasler J, editors. Doctor-Patient Communication. Academic Press; 1982. pp. 89–108. [Google Scholar]
- Manion OG. PhD Dissertation. University of Michigan: 1953. An application of readability formulas to oral communication. [Google Scholar]
- McKinlay JB. Who is really ignorant—Physician or patient? Journal of Health and Social Behavior. 1975;16(1):3–11. [PubMed] [Google Scholar]
- Michie S, French D, Allanson A, Bobrow M, Marteau TM. Genetic counseling: information given, recall and satisfaction. Patient Education and Counseling. 1997;32(1–2):93–100. doi: 10.1016/s0738-3991(97)00068-2. [DOI] [PubMed] [Google Scholar]
- Microsoft Systems. Readability scores. http://office.microsoft.com/assistance/hfws.aspx?AssetID=HP05. Microsoft Office, 2003.
- Nielsen-Bohlman L, Panzer AM, Kindig DA, editors. Health literacy: A prescription to end confusion. Washington, D.C: The National Academies Press; 2004. Institute of Medicine Committee on Health Literacy. [PubMed] [Google Scholar]
- Oatley K, Jenkins JM. Understanding Emotions. Cambridge, MA: Blackwell; 1996. [Google Scholar]
- Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielesen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. Journal of General Internal Medicine. 2005;20(2):175–184. doi: 10.1111/j.1525-1497.2005.40245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parikh NS, Parker RM, Nurss JR, Baker DW, Williams MV. Shame and health literacy: the unspoken connection. Patient Education and Counseling. 1996;27(1):33–39. doi: 10.1016/0738-3991(95)00787-3. [DOI] [PubMed] [Google Scholar]
- Pieterse A, Ausems M, van Dulmen AM, Beemer FA, Bensing J. Initial cancer genetic counseling consultation: change in counselees’ cognitions and anxiety, and association with addressing their needs and preferences. American Journal of Medical Genetics. 2005a;137(1):27–35. doi: 10.1002/ajmg.a.30839. [DOI] [PubMed] [Google Scholar]
- Pieterse A, van Dulmen AM, Ausems M, Beemer FA, Bensing JM. Communication in cancer genetic counselling: does it reflect counselees’ previsit needs and preferences? British Journal of Cancer. 2005b;92(9):1671–1678. doi: 10.1038/sj.bjc.6602570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieterse A, van Dulmen AM, Beemer FA, Ausems M, Bensing J. Tailoring communication in cancer genetic counseling through individual video-supported feedback: a controlled pretest-posttest design. Patient Education and Counseling. 2006;60(3):326–335. doi: 10.1016/j.pec.2005.06.009. [DOI] [PubMed] [Google Scholar]
- Press N, Browne CH. Risk, autonomy, and responsibility: informed consent for prenatal testing. Hastings Center Report. 1995;25(3 Suppl):S9–S12. [PubMed] [Google Scholar]
- Roter DL, Hall JA, Katz NR. Relations between physicians’ behaviors and analogue patients’ satisfaction, recall, and impressions. Medical Care. 1987;25(5):437–451. doi: 10.1097/00005650-198705000-00007. [DOI] [PubMed] [Google Scholar]
- Roter DL, Hall JA, Kern DE, Barker LR, Cole KA, Roca RP. Improving physicians’ interviewing skills and reducing patients’ emotional distress. A randomized clinical trial. Archives of Internal Medicine. 1995;25155(17):1877–84. [PubMed] [Google Scholar]
- Roter D. Health Literacy and the Patient Provider Relationship. In: Schwartzberg J, Van Geest J, Wang C, Gazmararian J, Parker R, Roter D, Rudd R, Schillinger D, editors. Understanding Health Literacy: Implications for Medicine and Public Health. Chicago: AMA Press; 2004. pp. 87–100. [Google Scholar]
- Roter D, Ellington L, Erby LH, Larson S, Dudley W. The Genetic Counseling Video Project (GCVP): Models of practice. American Journal of Medical Genetics, Part C, Seminars in Medical Genetics. 2006;142(4):209–220. doi: 10.1002/ajmg.c.30094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roter DL, Frankel RM, Hall JA, Sluyter D. The expression of emotion through nonverbal behavior in medical visits. Mechanisms and outcomes. Journal of General Internal Medicine. 2006;21(Suppl 1):S28–S34. doi: 10.1111/j.1525-1497.2006.00306.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roter DL, Hall JA. Doctors Talking to Patients/Patients Talking to Doctors: Improving Communication in Medical Visits. 2. Westport, CT: Praeger Publishing; 2006. [Google Scholar]
- Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, et al. Association of health literacy with diabetes outcomes. Journal of the American Medical Association. 2002;288(4):475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- Schillinger D, Piette J, Grumbach K, Wang F, Wilson C, Daher C, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Archives of Internal Medicine. 2003;163(1):83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- Schillinger D, Bindman AB, Wang F, Stewart A, Piette J. Functional health literacy and the quality of physician-patient communication among diabetes patients. Patient Education and Counseling. 2004;52(3):315–323. doi: 10.1016/S0738-3991(03)00107-1. [DOI] [PubMed] [Google Scholar]
- Schmitt JF, Carroll MR. Older listeners’ ability to comprehend speaker-generated rate alteration of passages. Journal of Speech and Hearing Research. 1985;28(2):309–312. doi: 10.1044/jshr.2802.309. [DOI] [PubMed] [Google Scholar]
- Schwartz LM, Woloshin S, Welch HG. The role of numeracy in understanding the benefit of screening mammography. Annals of Internal Medicine. 1997;127(11):966–972. doi: 10.7326/0003-4819-127-11-199712010-00003. [DOI] [PubMed] [Google Scholar]
- Schwartzberg J, Van Geest J, Wang C, Gazmararian J, Parker R, Roter D, Rudd R, Schillinger D, editors. Understanding Health Literacy. Chicago: AMA Press; 2004. [Google Scholar]
- Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Medical Care. 2002;40(5):395–404. doi: 10.1097/00005650-200205000-00005. [DOI] [PubMed] [Google Scholar]
- Snow C. Linguistic development as related to literacy. Early Intervention and Culture. In: Eldering L, Leseman P, editors. Preparation for literacy: the interface between theory and practice. Netherlands National Commission for UNESCO; 1993. pp. 133–48. [Google Scholar]
- Stata Corporation. Stata statistical software. College Station, TX: 2004. [Google Scholar]
- Street B. Literacy in theory and practice. Cambridge: Cambridge University Press; 1984. [Google Scholar]
- Suchman AL, Roter D, Green M, Lipkin M., Jr Physician satisfaction with primary care office visits. Collaborative Study Group of the American Academy on Physician and Patient. Medical Care. 1993;31(12):1083–1092. doi: 10.1097/00005650-199312000-00002. [DOI] [PubMed] [Google Scholar]
- Svarstad BL. Doctoral dissertation. Department of Sociology, University of Wisconsin; Madison, Wisconsin: 1974. The doctor-patient encounter: An observational study of communication and outcome. [Google Scholar]
- Tambor ES, Bernhardt BA, Rodgers J, Holtzman NA, Geller G. Mapping the human genome: An assessment of media coverage and public reaction. Genetics in Medicine. 2002;4(1):31–36. doi: 10.1097/00125817-200201000-00006. [DOI] [PubMed] [Google Scholar]
- Thompson TL. Interpersonal communication and health care. In: Knapp ML, Miller GR, editors. Handbook of interpersonal communication. 2. Thousand Oaks, CA: Sage; 1994. pp. 696–725. [Google Scholar]
- Van den Berg M, Timmermans DRM, ten Kate LP, van Vugt JMG, van der Wal G. Are pregnant women making informed choices about prenatal screening? Genetics in Medicine. 2005;7(5):332–338. doi: 10.1097/01.gim.0000162876.65555.ab. [DOI] [PubMed] [Google Scholar]
- Watson M, Lloyd S, Davidson J, Meyer L, Eeles R, Ebbs S, et al. The impact of genetic counseling on risk perception and mental health in women with a family history of breast cancer. British Journal of Cancer. 1999;79(5–6):868–874. doi: 10.1038/sj.bjc.6690139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams MV, Parker RM, Baker DW, Parikh NS, Pitkin K, Coates WC, et al. Inadequate functional health literacy among patients at two public hospitals. Journal of the American Medical Association. 1995;274(21):1677–1682. [PubMed] [Google Scholar]
- Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease. A study of patients with hypertension and diabetes. Archives of Internal Medicine. 1998;158(2):166–72. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- Williams N, Ogden J. The impact of matching the patient’s vocabulary: a randomized control trial. Family Practice. 2004;21(6):630–635. doi: 10.1093/fampra/cmh610. [DOI] [PubMed] [Google Scholar]