Abstract
Autism researchers have identified a set of common effective practice elements for early intervention (EI) (e.g., intensive programming). The current study examined the reported about use of common elements of effective interventions in community EI settings. Eighty EI providers reported about their programs. The majority of participants reported using common effective elements, however, the depth and quality of the use of these elements was highly variable. Taking community program structure into account in future research will facilitate the development of methodologies, which immediately fit into the context of community programming rather than requiring program adaptation for use in the real world. Recommendations for using current community program structure to improve use of evidence-based practices are discussed.
Keywords: Autism, Early intervention, Usual care, Evidence-based practices
Introduction
The number of children with autistic spectrum disorders (ASD) has increased dramatically over the past decade. Although the reason for this increase is under debate, the reality is that appropriate early intervention (EI) programs for young children with ASD are in high demand. State and local governments are struggling to provide educational services, which meet the pervasive needs of children with ASD. However, the intensity and quality of services recommended is often difficult to provide due to budgetary constraints and problems retaining staff with sufficient training and expertise in ASD intervention. Public programs have faced criticism and legal action from families concerned that their children were not receiving appropriate services (Mandlawitz, 2002).
Treatment studies suggesting substantial gains may be achieved when treatment is provided at a very early age (Lovaas, 1987; Strain & Cordisco, 1994; Mcgee, Morrier, & Daly, 1999; National Research Council (NRC), 2001) have increased emphasis on the importance of EI (i.e., treatment before the age of 4 years). While one specific treatment has not emerged as the established standard for all children with ASD, several methods have been demonstrated to be efficacious with some children in research settings. Some of these methods focus on specific behaviors while other interventions are more comprehensive in nature. However, there is little information about how these methods, developed by researchers and tested in University-based programs, are being used by or will fit into current community EI systems.
Researchers and providers across a variety of disciplines, including EI, are often frustrated by the gap between research and practice (Bondy & Brownell, 2004). In the area of ASD, researchers are skeptical about the ability and/or willingness of public programs to utilize evidence-based practices to provide quality treatment due to limited training and funding (Mcgee et al., 1999). Conversely, service providers feel that practices developed in research settings do not capture the richness and complexity of the children in their programs (Cochran-Smith & Lytle, 1999). In recent studies, community practitioners have identified pervasive skepticism about the clinical utility of research-based ASD practices due to difficulties with adaptation to clinical settings (Stahmer, Collings, & Palinkas, 2005). Barriers to translating evidence-based practices into community settings may include limited opportunities for training, a lack of autism-specific support, large caseloads, and low-program intensity. However, whether or not these barriers are real or widespread is unclear. In order to bridge the gap between research and practice, it is necessary for researchers to gain a better understanding of community environments.
One way to examine the barriers to moving efficacious practice into community settings is to look at the disparities between current practice and best practice guidelines. Autism researchers have identified a set of common effective practice elements, which cross many empirically supported treatment methods. Common elements typically agreed upon include: (1) the earliest possible start to treatment; (2) high-treatment intensity (20-30 h per week); (3) ongoing, systematic assessment, which leads to intervention choices; (4) strategies to promote generalization of learned skills; (5) structured environment with a predictable routine; (6) high levels of staff education and training; (7) active, sustained engagement of the child; (8) individualized treatment programs designed to meet a child’s needs; (9) specific curriculum content with a focus on communication, social/play skills, cognitive, self-help, and behavioral issues; and (10) high-parent involvement (Rogers, 1996; Dawson & Osterling, 1997; Dunlap, 1999; Hurth, Shaw, Izeman, Whaley, & Rogers, 1999; NRC, 2001). Some researchers also report that inclusion with typically developing peers is important (Robbins, Giordano, Rhoads, & Feldman, 1996; Tsai, 1998; NRC, 2001). These structural elements of EI programs may be as important as specific intervention techniques in improving care for children with ASD. It is currently unclear whether or not community providers are using these common structural elements. An empirical examination of practitioner use of these proposed effective elements will provide a framework for developing effective interventions that also match the context of community care.
The purpose of this investigation was to: (a) obtain EI provider reports of program structure and use of common effective practices with children who have ASD; (b) to examine differences in program structure by age of the child (toddlers age birth-to-three or preschoolers age three-to-five) and setting (in-home; classroom), (c) to examine the use of evidence-based effective program elements across two Southern California counties. Recommendations for translating evidence-based methods into community programs will be discussed.
Method
Study Design
Qualitative methods via a structured telephone interview were used to investigate the techniques employed by EI service providers working with children who have ASDs. A telephone interview approach was chosen to ensure the largest response (e.g., rather than a mailing interview) and ease of scheduling for the providers. A certificate of confidentiality was obtained from the National Institute of Health (NIH) in order to ensure providers felt comfortable providing unbiased descriptions of their programs.
Interview Development
The interview was designed by the author in consultation with experts in areas of autism treatment, services research, and qualitative methodology. Initial development of the topic areas included a review of the literature on best practices in autism, as well as common elements of efficacious treatments. The NRC publication on Educating Children with Autism (NRC, 2001), and several articles examining interventions for children with autism were reviewed (Robbins et al., 1996; Dawson & Osterling, 1997; Howlin, 1998; Rogers, 1998; Tsai, 1998; Gresham, Beebe-Frankenberger, & MacMillan, 1999; Hurth et al., 1999; Iovannone, Dunlap, Huber, & Kincaid, 2003; Ozonoff, Rogers, & Hendren, 2003). Important elements of treatment and specific methodologies were taken from these initial reviews. Focus groups with EI providers were conducted to gain a clearer understanding of the methods and vocabulary used by providers. Complete results of these focus groups can be found in Stahmer et al. (2005).
Ten experts in the field of designing intervention programs for young children with ASD and assessing the quality of EI programs reviewed the questions and provided feedback on the content validity of the interview (Ollendick & Hersen, 1993). Five EI providers participated in a pilot interview, provided feedback on the relevance of the interview and the clarity of the questions. The expert consultants and pilot providers all reviewed the final version before the interviews began.
Instrument
The portion of the interview reported here consisted of 41 questions and took ∼25 min to administer. The interview consisted of four different sections including (1) provider background and experience; (2) general program information; (3) parent involvement; and (4) curriculum and goal planning. Table 1 provides a list of program areas covered.
Table 1.
Interview topic areas
| General topic | Specific areas of inquiry |
|---|---|
| Provider background and experience | Years of experience in special education/autism |
| Demographic information (age, race/ethnicity) | |
| Education level and credentials | |
| General program information | Age group and program setting |
| Classroom classification | |
| Caseload (overall number of children in program/caseload; ASD; typically developing; teacher: student ratio) | |
| Program intensity (hrs/day/wk; extended day/year) | |
| Consultation and collaboration (within the program and with other agencies/professionals; Presence of autism specialist in program) | |
| Additional therapies services (OT; speech; adaptive PE, etc.) | |
| Inclusion opportunities (type of opportunity; ratio) | |
| Parent involvement | Types of opportunities for parent involvement (if any) |
| Use of parent education or training | |
| Curriculum and goal planning | Methods of determining goals |
| Curriculum areas covered | |
| Use of assessment to measure progress/alter programs |
Sample
Participants were 80 EI providers working in both in-home and classroom settings in San Diego and Riverside counties in California. Eligible providers were the primary service provider or supervisor in an educational/EI program and had at least one child with autism in their care.
In the US, EI program funding and regulations vary depending upon the age of the child. Children under the age of three are served though Part C of the Individuals with Disabilities Act (IDEA), while children over the age of three are served by Part B of IDEA. Providers in both systems were surveyed to assess variation. In California, the Department of Developmental Disabilities provides services for infants and toddlers (Part C) while the Department of Education provides services to preschool children (Part B).
Providers working in both in-home and classroom settings were recruited through the Regional Centers (for children under 3) or School Districts (children 3-5). In-home agencies typically consist of a psychologist or other licensed professional who oversees the agency, supervisors who develop individual programs for children with autism under the supervision of the psychologist, and therapists who provide the day-to-day service under the guidance of the program supervisor. Individuals at the level of program supervisor were asked to participate. The qualifications for these individuals varies by agency, however, they typically have a BA or MA level degree as well as experience in the field of autism. In-group programs for children 0-3 the lead “teacher” in the classroom was asked to participate. The types of lead teachers in these programs may include early childhood educators or special educators, but these service providers are not usually required to have a teaching credential. For children over 3 served in school district programs the classroom teacher was recruited for participation. Teachers conform to district policies in terms of education and licensure. Service providers were invited to participate based on their role in the development of programming for the children with autism in their care as well and their role in supervision of paraprofessionals implementing interventions with these children. Since the term “teacher” carries connotations of licensure, the term “service provider” will be used to refer to the participants.
San Diego (consisting of 42 school districts) and Riverside (27 school districts) counties were selected based on their representation of urban areas expected to have sizeable populations of children with autism (populations = 2,931,714 and 1,871,950, respectively1). Interviews were conducted between November 2003 and March 2005. The California Department of Education (2004/2005 school year) reported 298 children and 476 children aged three to five served under the educational Autism category in Riverside and San Diego counties, respectively. The numbers of children under age three with ASD are not publicly available, however, smaller numbers with similar ratios to the 3-5 population is likely.
Of 42 school districts in San Diego, 22 were serving children with ASD under the age of 5 at the time of the interview. The other 20 districts either did not currently have any children with ASD enrolled, or referred to other districts for services. Providers from 18 (81%) of the districts serving children with ASD participated in the interview. Two districts (6%) did not have time to participate and two districts chose not to participate due to confidentiality concerns. San Diego County had nine infant programs contracted to serve children with ASD. Providers from eight (89%) of these programs participated in the interview. The other program director could not be reached.
In Riverside County 16 of 22 school districts were serving young children with ASD at the time of the interview. Providers from eight districts (50%) participated. Of the remaining districts, three (19%) did not respond to numerous attempts to contact the special education director, one (6%) stated that there was not time to participate, and in four districts (24%), the special education directors agreed to participate but no response was received from the providers. Six infant programs served children in Riverside County. Four programs reported serving children with ASD and providers from each of these programs (100%) participated in the interview.
Procedure
Introductory letters explaining the study were sent to special education directors and infant program providers (funded through California Early Start) serving children with ASD in both counties. Follow-up phone calls were made to programs on a monthly basis until a response was received, or 1 year had passed. Special Education Directors that expressed interest in participation and were currently serving children birth to 5 years of age with ASD were asked to inform eligible providers in their programs about the project. Individual providers were then mailed an introductory letter describing the study and inviting them to participate.
Service providers in each County were contacted via telephone after they had returned their consent forms. The project coordinator made an appointment for the interview at a time most convenient for the provider. The coordinator conducted the interviews, which took ∼45 min to complete. All interviews were completed in one phone call. Providers were thanked for their time, and sent a check for $20.00 for their participation.
Data analysis
Data were analyzed using descriptive methods to determine the types of programs provided for young children with ASD. Additionally, Chi Square analyses were conducted to examine differences between the San Diego and Riverside County as well as differences in service provision to infants and toddlers (0-3) versus pre-school programs (3-5) and differences between in-home and classroom-based programs. Bivariate correlational analyses were used to examine relationships between individual school district variables and several dependent variables.
Results
Provider Characteristics
Most participating providers were White (81%), and had a mean of 10 years experience, with a range of 1-37 years in the field (see Table 2). A majority of providers served children ages 3-5 (75%). Most worked in a classroom setting (77%). Due to the larger size of the County, most respondents were from San Diego (77%). Although not depicted in the table, in Riverside County, all but one provider served children in classroom settings (95%) and most respondents worked with preschool-age children (90%). In San Diego County, 71% of providers worked in classrooms and 70% served pre-school children. There was overlap between age group and setting, with 70% of toddler providers working in-home, and 93% of preschool providers working in classrooms.
Table 2.
Provider demographics
| Age in years | Gender | Race/ethnicity | Age group | Program setting | County | Years of special education experience | Years autism experience |
|---|---|---|---|---|---|---|---|
| M = 39.34 | Male | Black = 4% | Toddler | In-Home | San Diego | M = 12 | M = 10 |
| SD = 11.14 | n = 2 | Asian = 1% | n = 21 | n = 18 | n = 63 | SD = 8.4 | SD = 7.3 |
| Range = 24-69 | Female | White = 81% | (26%) | (23%) | (77%) | Range = 1-37 | Range = 1-37 |
| n = 78 | Latino = 6% | Preschool | Classroom | Riverside | |||
| Native American = 4% | n = 59 | n = 61 | n = 17 | ||||
| Other = 4% | (74%) | (77%) | (21%) |
Provider Background and Experience
Table 3 describes overall provider education as well as education and experience by age group, setting, and County. Degree and certificates were not mutually exclusive. A majority of providers (96%) had Bachelor’s Degrees. Almost half (41%) had a Regular Education Teaching Credential, while only 16% held a Special Education Credential. About half (45%) also had a specialized certificate in either severe handicaps or learning handicaps. Very few held Doctoral Degrees (2%). Over half (55%) of the providers had a Master’s Degree. Eighteen percent had an early childhood special education credential and very few (3%) had early childhood education certificates (typically for professionals working in typical early childhood programs).
Table 3.
Provider education level by age group, setting, and County
| Education level | Total (%) | Toddler (%) | Preschool (%) | Chi square (p-values) | In-home (%) | Classroom (%) | Chi square (p-values) | Riverside (%) | San Diego (%) | Chi square (p-values) |
|---|---|---|---|---|---|---|---|---|---|---|
| AA degree | 4 | 5 | 3 | ns | 0 | 5 | ns | 18 | 0 | 11.5 (0.001) |
| BA | 96 | 95 | 96 | ns | 100 | 95 | ns | 82 | 100 | ns |
| Regular education credential | 41 | 14 | 551 | 8.5 (0.004) | 11 | 51 | 9.0 (0.003) | 29 | 44 | ns |
| Special education credential | 16 | 10 | 19 | ns | 11 | 18 | ns | 6 | 19 | ns |
| Severe hand. credential | 29 | 10 | 36 | 5.1 (0.023) | 6 | 36 | 6.27 (0.016) | 35 | 27 | ns |
| Learning hand. credential | 16 | 5 | 20 | ns | 0 | 21 | 4.59 (0.033) | 12 | 18 | ns |
| MA | 55 | 52 | 56 | ns | 56 | 54 | ns | 29 | 62 | 5.7 (0.017) |
| PhD | 2 | 5 | 2 | ns | 11 | 0 | ns | 0 | 3 | ns |
| Early childhood special education credential | 18 | 19 | 17 | ns | 11 | 20 | ns | 26 | 16 | ns |
| Early childhood education certif | 3 | 5 | 5 | ns | 0 | 3 | ns | 0 | 3 | ns |
| Autism specific degree/program | 0 | 0 | 0 | ns | 0 | 0 | ns | 0 | 0 | ns |
When comparing provider education and experience by age group and setting some differences were apparent (see Table 3). Pre-school providers were more likely to have a regular education teaching credential (p = 0.004) or a severely handicapped certificate (p = 0.023) than toddler providers. Classroom providers were more likely to hold regular education (p = 0.003), severely handicapped (p = 0.016), and learning handicapped (p = 0.003) credentials than in-home providers. These differences are likely due to differential requirements for providers in each system.
Provider education and experience were also compared by County. Counties were similar in most areas. However, Riverside County providers were more likely to have an AA degree (p = 0.001) than providers in San Diego County. Providers in San Diego County providers were significantly more likely to hold a Masters degree (p = 0.017) than providers in Riverside County.
Although not depicted in the table, years of experience was analyzed by age group, setting, and County. Pre-school providers had significantly more autism experience than toddler providers (p = 0.035). Classroom providers had significantly more special education (p = 0.017) and autism experience (p = 0.041). No differences were found by County.
Program Intensity
Overall, children received an average of 14.40 h of educational services per week (range = 5-30). Children in Riverside County across settings and age groups received an average of 17.2 h per week (range = 11-30 h), which was significantly (p = 0.003) more than children in San Diego County who received an average of 13.63 h per week of service (range = 5-25 h). Pre-school children served in all settings received significantly more hours per week of service than toddlers (toddler M = 11.03, pre-school M = 15.55, p = 0.000). Similarly, classroom programs provided more hours of service than in-home programs (in-home 12.25; classroom; 16.55, p = 0.014). Figure 1 depicts an overview of the average hours per week of service by age, setting, and County.
Fig. 1.
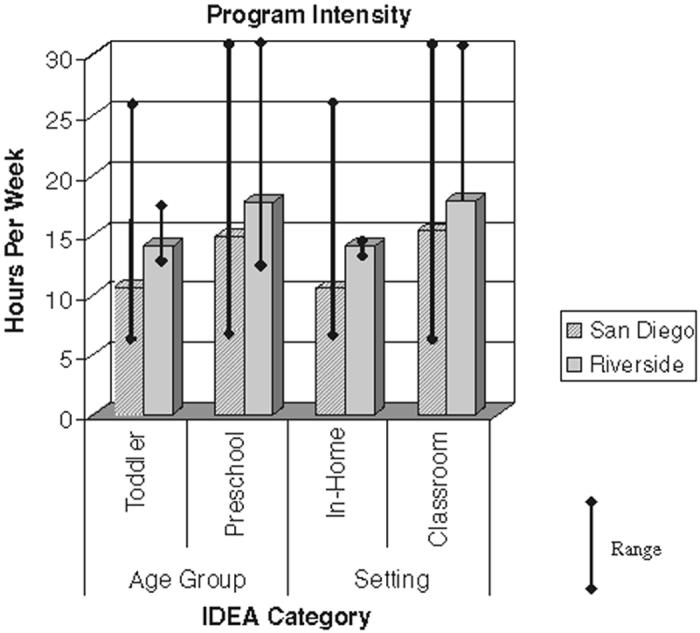
Program intensity by age group, setting, and County
Classroom programs reported serving children with autism an average of 16.25 total service hours per week. This included a mean of 15.4 h of classroom time per week (range = 5-32), and a mean of 8.9 h of extended day programs (range = 0-23). Children in classroom programs in Riverside County received significantly more service hours per week on average (M = 17.8) than children in San Diego County (15.8, p = 0.034). Children in San Diego had a wider range of service intensity (5-30 h) than children in Riverside (12-22). Toddlers served in classrooms obtained significantly fewer hours of service per week on average (M = 12.8) than pre-school children served in classrooms (M = 17.4, p = 0.005).
For children served in-home, the mean number of hours week of service was 9.3 (range = 0.5-15). In this case, toddlers received significantly more hours on average (M = 10.0) than pre-school children (M = 6.7, p = 0.035). No significant differences were found by County for in-home services although the trend was consistent with classroom programs (Riverside M = 13; San Diego M = 9).
Inclusion
Providers were asked if children with ASD in their programs had opportunities to interact with typically developing peers. Fifty-six percent of classroom providers indicated that there were typical children in the classroom. In 23% of those cases, the typical children were enrolled for the entire program. In a minority of cases, the same typically developing children were enrolled full-time (7% of programs including typical children) while in the remainder of programs with typical children, different ‘reverse mainstreamers’ came to the classroom on various days. Another 23% of programs had typical children enrolled for more then 10 h per week, 17% for 5-10 h per week, and 35% for fewer than 5 h per week.
Of those classroom programs indicating opportunities to interact with typical peers (52%), most programs offered opportunities to interact at recess (65%), during snack or lunch (17%), or at special assemblies (15%). Very few programs had formal social skills groups (4%), or utilized head start programs (8%). A few programs specifically stated that older elementary children came to the classroom as peer helpers (10%). Thirty-eight percent of in-home programs provided opportunities for interaction with typically developing peers. Opportunities typically included setting up play dates (57%) or holding parentinfant play groups (29%).
When all providers were asked, 38% said that some children with ASD in their programs also attended community preschools as part of their educational program. About half of those children had inclusion support. The mean number of days per week that children attended community preschool was 3.25 with a range of 1-5. Toddlers were more likely to attend community preschools (60%) than preschool children (30%, p = 0.018). Similarly, in-home programs participants were more likely to attend a community preschool (37%) than classroom students (30%). However, pre-school programs were more likely to have typically developing children as part of their classroom program (83%) than toddler programs (45%, p = 0.001). Riverside County providers were more likely to report having typical peers in their programs (94%) than San Diego County programs (67%, p = 0.029).
Classroom Classification
Ninety percent of the classroom programs served children ages 3-5. Approximately 30% of classroom-based programs served a mixed group of special education children, 19% served only children with ASD, 15% were classified as severely handicapped, 16% were classified as learning handicapped, 5% were identified as inclusion programs, 2% as one-on-one programs, and 10% as sensory-based classrooms. There were no significant differences by County for any of these variables. However, it appeared there was a trend toward more children in San Diego County being served in autism-specific programs (50%) than in Riverside (8.89%). Toddlers may have been more likely to be served in programs serving children with a variety of disabilities (68%) than preschool children (26%) although this difference was not statistically significant.
Consultation and Collaboration
Providers were asked about collaboration with individuals in outside agencies. Collaboration might include working with the agency to provide services, or ensuring coordinated service across agencies. A small majority of providers (58%) reported collaborating with other agencies to provide ASD services. These agencies included the Department of Developmental Services (61%), school districts (47%), private agencies serving children with ASD (25%), and insurance companies (6%).
Eighty-two percent of providers indicated that they had an autism specialist or consultant available to their program. Significantly more programs in San Diego County reported having autism specialists (82%) than in Riverside County (58%, p = 0.004). There was no difference in the availability of autism specialists by age group or setting.
Additional Therapies and Services
Providers were asked about additional therapies children with ASD in their programs typically received through the provider’s program. Providers reported that children often received occupational therapy (86%), speech therapy (86%), one-on-one therapies (80%), behavior management services (71%), adaptive PE (68%), sensory integration training (67%), transportation services (64%), assistive technology/devices (59%), social skills groups (53%), vision services (25%), and music therapy (18%). These services were included in the number of service hours.
Parent Involvement and Parent Education
Almost all of the providers interviewed (96%) stated that their program offered opportunities for parent involvement. There were no differences by age group, setting or County. Seventy-three percent reported offering parent education in their programs. Providers in toddler programs were significantly more likely to provide parent education (100%) than providers in preschool programs (78%, p = 0.007). Ninety percent of in-home providers indicated that they worked with both parent and child during home visits. Significantly more San Diego County providers reported providing parent education programs (85%) than those in Riverside County (53%, p = 0.004).
The types of involvement and education opportunities reported included observation of the child’s program (34%), classes or workshops on specific strategies (24%), home visits (23%), volunteer opportunities (20%), parent support groups (19%), opportunities to practice techniques with feedback outside a home visit (16%), participation in team meetings (14%) and communication such as communication notebooks, newsletters or written materials (10%).
Curriculum and Goal Planning
Providers were asked to describe how goals were determined in their programs. All providers mentioned a team approach or use of the IEP/IFSP process for goal development. Fifty-six percent mentioned the use of standardized assessment tools and 59% mentioned informal assessment. A wide variety of specific assessment tools were mentioned. Ninety-three percent indicated they used these assessments to develop goals and assess program progress. Eighty percent reported altering a child’s program at least monthly, typically due to a child needing more challenging goals.
Providers listed the five most important curriculum areas for children with ASD. Overall, 94% listed communication and language skills as a top area, 86% stated that social and play skills were very important. Other areas of agreement included self-help skills (48%), behavioral issues (38%), motor skills (35%), sensory issues (24%), pre-academic skills (24%), and readiness to learn (24%).
Discussion
This paper provides one of the first examinations of “treatment-as-usual” EI programs for children with ASD. These provider interview data shed light on the experience and education of EI caregivers as well as the nature and structure of community programs and may be useful in helping researchers and providers alike learn to embed evidence-based practices foryoung children with ASD into community programs. These data highlight the extreme variability in programming found in a relatively small geographic area. Providers reported huge variability in intensity of programming, provider training and support, program setting, and the use of inclusion practices.
The intensity of the programming for the majority of children served in the community providers surveyed was well below the recommend 25 h per week (NRC, 2001). The comprehensive programs examined in the NRC report provided from 12 to 40 h per week of service, with only two of the programs providing fewer than 25 h per week. In contrast, the community programs examined for the current project provided an average of 15 h per week, with some children receiving as few as 5 h per week. Only two (1%) programs offered 25 or more hours per week, and only ten (13%) had 20 or greater hours. A majority of programs did include additional services such as speech and occupational therapy, music therapy, and adaptive PE, which were captured in the total number of hours of service provided by the educational program.
Of course, these interviews did not capture services children received through other agencies, private insurance or self-pay. Up to 90% of children with ASD receive additional services outside of their primary EI program (Thomas, Morrissey, & McLaurin, 2004). Therefore, coordination between systems of care may be as important to effective care as the use of evidencebased practice and is likely to be lacking in community services (NRC, 2001). In the current survey, only about half of the providers reported collaborating with other agencies. Very little information is available in the literature about agency collaboration, how various treatments work together, and how consistency (or lack of consistency) in treatment for young children with ASD affects outcomes. The call for increased intensity of service may be placing a financial burden on all educational programs offered by public school districts and EI programs (Jacobson & Mulick, 2000). If intensity is to increase to recommended levels, then agencies such as school districts, Departments of Developmental Services, Mental Health agencies, public or private insurance agencies and community practitioners providing programming on a fee-for-service basis must collaborate to provide coordinated programming. Increasing the number of hours but duplicating service or offering programming which may be confusing or nonproductive for the child is not likely to be effective. Specification of responsibility for various aspects of a child’s program, such as social skills, behavioral issues, family interaction, etc., could be specified and then coordinated. This may help spread the burden of funding increased services across a variety of funding sources.
Training and support was also an area of variability that may greatly affect intervention quality and effectiveness. Although half of the providers interviewed had a Master’s level education, many did not carry any specialized credentials. Providers in Riverside County were more likely to have associate degrees rather than higher levels of education. This may be due to the fact that many children with autism in Riverside County were placed in programs with typically developing children; therefore, the education level of the teachers in the programs was more in line with those of early childhood educators rather than special educators. The level of autism-specific support given to these providers is unclear. The level of experience also varied widely, although many providers had a great deal of ASD experience. Providers working with children ages 3-5 had more autism experience. This may be due to the greater likelihood that children in the older age range have a formal diagnosis, and the fact that it is only in recent years that children have been diagnosed with ASD at very young ages. A large majority of programs reported having an autism specialist available for support, which may supplement education and training. However, the definition of ‘autism specialist’ was left to the provider and the education and experience of theses ‘specialists’ remains unclear. A survey of autism specialists would be very helpful. It may be that these specialists provide training as well as develop programming for children with ASD.
Program setting may also affect community program use of evidence-based practices. Approximately threefourths of the providers served children in classroom settings. Some of them did have the staff to provide individual (one-to-one) programming within the classroom, but most of the time children were seen in group situations. This is very important because many of the evidence-based interventions for ASD were developed in one-on-one settings. Examples include discrete trial training (Lovaas, 1987), pivotal response training (Schreibman & Koegel, 2005), and floor time (Greenspan & Wieder, 1997) among others.
Several model programs described by the NRC that provide the basis for many of the common effective elements of practice, however, are classroom-based (NRC, 2001). The difficulty with translating these programs into community settings is that very few of them have developed treatment manuals or guidelines, which can be implemented by community providers. Additionally, many community programs served children with a variety of disabilities, including ASD. Providers, although they support individualization, may wish to use techniques and classroom practices with wide applicability. This may be especially true for toddler classroom programs, which are more likely to be noncategorical and include typically developing children. Currently very few evidence-based practices for ASD have been empirically tested with children who have varying disabilities. An understanding of commonalities and differences across methods used for a variety of disabilities (e.g., autism and language delay) would be helpful to providers (Bondy & Brownell, 2004). Providers would then be able to better choose specific methods that would both fit their programs and be beneficial to the changing mix of children enrolled.
Another area of variability in services is the inclusion of typically developing children in programming. Over half of school-based programming had some typically developing children as part of the school day, but fewer than half of those programs had typically developing children enrolled at least 10 h per week. Many programs reported that children with ASD had opportunities to play with typical Kindergarteners during recess, which may not be developmentally appropriate or truly support the development of peer relationships. Many children also attended a typical preschool, however very few of those children had support in the typical programs. It is unlikely that children with ASD will develop social relationships or improve interaction and play skills simply by being around typically developing peers (Strain, McGee, & Kohler, 2001). Providers and paraprofessionals may need education in methods of collaborating with community programs and well as methods of improving interaction with typical peers. Given that many programs do not have access to typically developing peers of the same age as the children with ASD, systems changes may need to be developed which involve providing child care in EI programs or involving community preschools in trainings which allow support of children with ASD.
In addition to the structural and educational aspects of programming described above, parent involvement in treatment has been a common element in many evidence-based programs for children with autism ever since researchers found that generalization and maintenance of behavior changes were improved when parents were trained and continued interventions at home and in the community (Lovaas, Koegel, Simmons, & Long, 1973). Clearly, EI providers agree that this is an important aspect to treatment for children with ASD as most of them reported including parents in some way. However, again the type and intensity of this involvement was extremely variable across programs. Some programs offered parent education in specific intervention methods, which included practice with feedback and was rather intensive. For some programs parent involvement simply consisted of communication notebooks from home to school. In-home providers often conducted intervention in conjunction with the parents and appeared to have more opportunities for teaching. Some school programs had specified time set aside to conduct home visits. A few larger districts offered workshops specifically designed to help parents use intervention techniques at home. Helping providers understand the types of parent involvement that will most affect outcomes (e.g., learning specific techniques which can facilitate skill generalization; Schreibman & Koegel, 2005) and finding creative ways to incorporate training into school programs would help this area of effective treatment move forward.
An area of strong agreement between research and practice may be intervention goals. Providers listed goal and curriculum areas, which were very similar to those reported as important in the research literature. This area of agreement may facilitate the implementation of evidence-based practices. This similarity in areas of importance suggests that providers may be open to interventions, which address areas such as communication and social skills as well as comprehensive interventions, which address a wide range of skills. There also appears to be an openness toward the use of assessment to monitor programming, and the research community may be able to provide specific assessment tools which would be user friendly in community programs as well as clearly direct providers toward specific strategies, interventions and goals.
Conclusion
Autism researchers have a unique opportunity to more efficiently meet the needs of this growing population by incorporating community stakeholder perspectives at a relatively early stage of intervention effectiveness trials. In research examining the translation of evidence-based children’s mental health treatments to usual care, Dr. John Weisz (Weisz, Chu, & Polo, 2004) suggests that early collaboration with providers is paramount. “To create the most robust, practice-ready treatments, the field (mental health) may need to consider a shift from the traditional (medical) model to a model that brings treatments into the crucible of clinical practice early in their development and treat testing in the practice settings as a sequential process, not as a single final phase” (Weisz et al., 2004) (p. 304). The current context of community care examined in this project had many of the basic structural elements needed for effective care for children with autism.
Data from these interviews indicate that researchers must provide diverse packages of evidence-based treatments in order to meet the needs of community EI providers. For example, programs serving young tod-dlers with ASD may require a focus on intervention strategies that can be conducted at home, in a one-on-one setting, and can include direct parent involvement. For preschool children, strategies must be useful in classrooms serving children with varying disabilities and functioning levels. However, even in these classroom programs, the teacher: child ratio was relatively high, indicating that structured and one-on-one strategies may be implemented even in group programs. Information on ASD and specific intervention strategies might be relatively easily disseminated in MA and credentialing programs. However, toddler providers had highly varied backgrounds, and lead providers to rely heavily on paraprofessionals therefore adequate resources for training these additional providers is necessary. Strategies, which can be successfully implemented in typical preschools by providers with early childhood coursework are needed. This may be especially true in more rural counties without specified ASD programs. In San Diego County, children in smaller districts can go to larger districts with established ASD programs. In rural areas of the country this is not the case. Therefore preschool and general special education teachers will need additional support to serve children with ASD. More information is needed on the role of the “autism specialist.” These specialists, if appropriately trained, may provide a method for ongoing system improvement, personnel training, and quality control in urban and rural settings.
These data provide information regarding specific program elements used in community programming. Targeting areas of agreement with evidence-based practice may help researchers move these programs into community settings more successfully. Taking community program structure into account in future research will facilitate the development of methodologies, which immediately fit into the context of community programming rather than requiring program adaptation for use in the real world.
Acknowledgments
This research was supported by a Child and Adolescent Services Research Grant number K01 MH65325-01 from the National Institute of Mental Health. The author would like to thank Nicole Collings, Dorothy Borszack-Vega, and Rachel Enkey for their assistance with the interview development, interview implementation, and data entry and analyses; Laura Schreibman, Mark Appelbaum, Andrew Bondy, Michelle Sullivan, the students and UCSD Autism Laboratory, the staff at Children’s Toddler School for assistance with question development, modification, and piloting the interview; and the journal editors for their insightful suggestions. Finally, the author thanks the service providers for taking time out of their busy schedules to provide valuable insight and information to the field through participation in this research.
Footnotes
Based on July 1, 2004 estimated population by US Census Bureau.
References
- Bondy E, Brownell MT. Getting beyond the research to practice gap: Researching against the grain. Teacher Education and Special Education. 2004;27:47–56. [Google Scholar]
- Cochran-Smith M, Lytle S. Relationships of knowledge and practice: Teacher learning in communities. In: Iran-Nejar A, Pearson PD, editors. Review of research in education. American Educational Research Association; Washington, DC: 1999. pp. 249–305. [Google Scholar]
- Dawson G, Osterling J. Early intervention in autism: Effectiveness, common elements of current approaches. In: Guralnick MJ, editor. The effectiveness of early intervention: Second generation research. Paul H. Brookes; Baltimore: 1997. pp. 307–326. [Google Scholar]
- Dunlap G. Consensus, engagement, and family involvement for young children with autism. Journal of the Association for Persons With Severe Handicaps. 1999;24:222–225. [Google Scholar]
- Greenspan SI, Wieder S. Developmental patterns and outcomes in infants and children with disorders in relating and communicating: A chart review of 200 cases of children with autistic spectrum diagnoses. Journal of Developmental and Learning Disorders. 1997;1:87–141. [Google Scholar]
- Gresham FM, Beebe-Frankenberger ME, MacMillan DL. A selective review of treatments for children with autism: Description and methodological considerations. School Psychology Review. 1999;28:559–575. [Google Scholar]
- Howlin P. Practitioner review: Psychological and educational treatments for autism. Journal of Child Psychology and Psychiatry. 1998;39:307–322. [PubMed] [Google Scholar]
- Hurth J, Shaw E, Izeman SG, Whaley K, Rogers SJ. Areas of agreement about effective practices among programs serving young children with autism spectrum disorders. Infants and Young Children. 1999;12:17–26. [Google Scholar]
- Iovannone R, Dunlap G, Huber H, Kincaid D. Effective educational practices for students with autism spectrum disorders. Focus on Autism and Other Developmental Disabilities. 2003;18:150–165. [Google Scholar]
- Jacobson JW, Mulick JA. System and cost research issues in treatments for people with autistic disorders. Journal of Autism and Developmental Disorders. 2000;30:585–593. doi: 10.1023/a:1005691411255. [DOI] [PubMed] [Google Scholar]
- Lovaas OI. Behavioral treatment and normal educational and intellectual functioning in young autistic children. Journal of Consulting and Clinical Psychology. 1987;55:3–9. doi: 10.1037//0022-006x.55.1.3. [DOI] [PubMed] [Google Scholar]
- Lovaas OI, Koegel R, Simmons JQ, Long JS. Some generalization and follow-up measures on autistic children in behavior therapy. Journal of Applied Behavior Analysis. 1973;6:131–166. doi: 10.1901/jaba.1973.6-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandlawitz MR. The impact of the legal system on educational programming for young children with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2002;32:495–508. doi: 10.1023/a:1020502324718. [DOI] [PubMed] [Google Scholar]
- Mcgee GG, Morrier MJ, Daly T. An incidental teaching approach to early intervention for toddlers with autism. Journal of the Association for Persons with Severe Handicaps. 1999;24:133–146. [Google Scholar]
- National Research Council . Educating children with autism. National Academy Press; Washington, DC: 2001. [Google Scholar]
- Ollendick TH, Hersen M. General psychology series. Vol. 167. Allyn & Bacon; Needham Heights, MA: 1993. Child and adolescent behavioral assessment. Handbook of child and adolescent assessment; pp. 3–14. [Google Scholar]
- bOzonoff S, Rogers SJ, Hendren RL. Autism spectrum disorders: A research review for practitioners. American Psychiatric Publishing Inc.; Washington, DC: 2003. [Google Scholar]
- Robbins FR, Giordano S, Rhoads S, Feldman RS. Preschool children with autism: Current conceptualizations and best practices. In: Feldman RS, editor. The psychology of adversity. University of Massachusetts Press; Amherst, MA: 1996. pp. 63–90. [Google Scholar]
- Rogers SJ. Early intervention in autism. Journal of Autism and Developmental Disorders. 1996;26:243–246. doi: 10.1007/BF02172020. [DOI] [PubMed] [Google Scholar]
- Rogers SJ. Empirically supported comprehensive treatments for young children with autism. Journal Clinical Child Psychology. 1998;27:168–179. doi: 10.1207/s15374424jccp2702_4. [DOI] [PubMed] [Google Scholar]
- Schreibman L, Koegel RL. Training for parents of children with autism: Pivotal responses, generalization, and individualization of interventions. In: Hibbs ED, Jensen PS, editors. Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice. 2nd ed. American Psychological Association; Washington, DC: 2005. pp. 605–631. [Google Scholar]
- Stahmer AC, Collings NM, Palinkas LA. Early intervention practices for children with autism: Descriptions from community providers. Focus on Autism and Other Developmental Disabilities. 2005;20:66–79. doi: 10.1177/10883576050200020301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strain P, Cordisco L. LEAP Preschool. In: Harris SL, Handleman JS, editors. Preschool education programs for children with autism. PRO-ED; Austin, TX: 1994. pp. 225–244. [Google Scholar]
- Strain P, McGee G, Kohler FW. Early childhood inclusion: Focus on change. Paul H. Brooks; Baltimore, MD: 2001. Inclusion of children with autism in early intervention settings: An examination of rationale, myths, and procedures. [Google Scholar]
- Thomas K, Morrissey J, McLaurin C. A look at autism service use across North Carolina; Paper presented in symposium: A services research perspective on autism. American Public Health Association 132nd Annual Meeting; Washington, DC. 2004. [Google Scholar]
- Tsai LY. Pervasive developmental disorders briefing paper. NICHCY; Washington, DC: 1998. [Google Scholar]
- Weisz JR, Chu BC, Polo AJ. Treatment dissemination and evidence-based practice: Strengthening intervention through clinician-researcher collaboration. Clinical Psychology: Science and Practice. 2004;11(3):300–307. [Google Scholar]


