Abstract
Background
Matrix metalloproteinase (MMP) is known to be involved in the initial and progressive stages of cancer development, and in the aggressive phenotypes of cancer. This study examines the association of single nucleotide polymorphisms in promoter regions of MMP-1 and MMP-3 with susceptibility to oral squamous cell carcinoma (OSCC).
Methods
We compared 170 Japanese OSCC cases and 164 healthy controls for genotypes of MMP-1 and MMP-3.
Results
The frequency of the MMP-1 2G allele was higher and that of the 1G homozygote was lower in the OSCC cases (p = 0.034). A multivariate logistic regression analysis revealed that subjects who were 45 years old or older had a significantly increased (2.47-fold) risk of OSCC (95%CI 1.47–4.14, p = 0.0006), and those carrying the MMP-1 2G allele had a 2.30-fold risk (95%CI 1.15–4.58, p = 0.018), indicating independent involvement of these factors in OSCC. One of the key discoveries of this research is the apparent reduction of the MMP-1 1G/1G and 1G/2G genotype distributions among the early onset OSCC cases under the ages of 45 years. It should be noted that the tongue was the primary site in 86.2% of these early onset cases. This could suggest the specific carcinogenic mechanisms, i.e. specific carcinogenic stimulations and/or genetic factors in the tongue.
Conclusion
Since the 2G allele is a majority of the MMP-1 genotype in the general population, it seems to act as a genetic pre-condition in OSCC development. However this report suggests a crucial impact of the MMP-1 2G allele in the early onset OSCC.
Background
Matrix metalloproteinase (MMP)-1 (Collagenase-1) is a major proteinase of the MMP family that specifically degrades type I collagen, which is a major component of the extracellular matrix (ECM), as well as other fibrillar collagens of types II, III, V and IX [1,2]. MMP-3 (Stromelysine-1) is responsible for degradation of type IV collagen, which forms the basement membrane, and collagen V, IX, X [3]. MMP-3 also has a role in activation of proMMP-1 in tumor tissue into the active form of MMP-1 [4]. Gene expression data in our previous report demonstrated enhanced expression of MMP family genes in OSCC tissues, and suggested correlation of high expression levels of MMP-1 and MMP-3 with aggressive behavior, such as metastasis, and clinical prognosis [5]. Similar correlations have been reported in pharyngeal, colon and various other tumor types [6-8]. Colocalization of MMP-1 and MMP-3 with destruction of ECM in the invasive front of cancer tissue suggests a direct role in cancer invasion [9].
It has also been shown that a function of MMPs affects susceptibility to different kinds of carcinoma. To date, polymorphisms of the promoter domain have been described in MMP-1, -3, -9, -12 to influence the expression level of the genes [10]. A 2G type of single nucleotide polymorphism (SNP) at -1607 bp site in the promoter domain of MMP-1 creates a sequence, 5'-GGA-3,' that is the core recognition sequence of the binding site for Ets family transcription factors. The 2G type promoter results in higher transcription activity of the MMP-1 gene than does a 1G type promoter [11]. A 5A type promoter at -1171 bp site of MMP-3 is also known to have a twofold higher transcriptional activity in vitro than that of a 6A type [12]. It has been documented that the 2G type SNP of MMP-1 confers increased susceptibility to colorectal [13], ovarian [14], lung [15], endometrial [16], renal cell [17] and head and neck [18] cancers; and the 5A type SNP of MMP-3 is associated with an increased susceptibility to breast cancer [19].
An in situ hybridization study revealed that MMP-1 expression in normal oral mucosa is controlled at a low level, whereas a remarkably elevated expression level is observed in cases of oral epithelial dysplasia, which becomes even higher in cases of OSCC [20]. It has also been documented that cases of oral epithelial dysplasia showing high expression level of MMP-1 developed into OSCC at higher frequency than cases with low expression of MMP-1 [21]. Taking all the observations noted above into consideration, it seems likely that MMPs may serve as key factors in all stages of the OSCC progression from carcinogenesis in the early precancerous condition to the advanced invasive and metastatic phases.
The purpose of this study is to document the effect of genomic polymorphisms of MMP genes in the development of OSCC. We compared genotype distribution in the promoter domains of the functional SNPs that influence the transcriptional activity of MMP-1 and MMP-3 between OSCC patients and healthy control groups. Multivariate analysis was effectively used to assess correlations among parameters such as OSCC, the genotypes, age and sex. In this report, we describe the role of functional SNP of the MMP-1 gene in susceptibility to OSCC and, as a remarkable finding; we discuss the crucial impact of the MMP-1 2G allele in the development of OSCC in younger individuals.
Methods
Study subjects
The tested cases were all unrelated native Japanese comprising 170 cases of OSCC (107 males, 63 females; average age 56.5 ± 13.9 years) who were histopathologically diagnosed as differentiated squamous cell carcinoma. The controls comprised 164 (104 males, 60 females) healthy subjects who did not have a history of malignant tumors and were frequency-matched to the cases by age (± 5 years; average age 51.5 ± 14.7 years). All OSCC subjects were patients who had been treated in the Dental Department of Niigata University Medical and Dental Hospital, Special Dental Care and Oral Surgery, Shinshu University Hospital, and Division of Oral Surgery, Nagaoka Red Cross Hospital.
Blood samples were taken after obtaining the patients' informed consent to participate in the study and processed anonymously. All cases were diagnosed histopathologically as OSCC. The study protocol was approved by the ethics committees of each institution.
Genotyping of MMP-1 and MMP-3
5 ml of blood was obtained from the subjects and used as the source of peripheral blood lymphocytes. 0.2% NaCl was added for destruction of red blood cells, followed by addition of TNE buffer, 10% SDS and Proteinase K (MERCK Co., Darmstadt, Germany). After incubation at 58°C for more than six hours, genomic DNA was extracted by phenol-chloroform treatment and ethanol precipitation. The reaction was performed in a 25 μl volume made up of 70 ng genomic DNA, 2.25 μl of the specific forward/reverse primer (10 μM), 1 μl of TaqMan® MGB probes (5 μM), 12.5 μl of TaqMan® Universal Master Mix (Applied Biosystems, Foster City, CA, USA). PCR cycling conditions were 10 min of initial denaturation at 95°C followed by 35 cycles of 15 sec denaturation at 92°C and 1 min of one step annealing/extension at 60°C for MMP-1 or 62°C for MMP-3 (ABI Prism® 7900 HT Sequence Detection System, Applied Biosystems). Combination of the probe/primer used for the MMP-1 SNP were: Forward primer, 5'-TGCCACTTAGATGAGGAAATTGTAGT-3' and reverse primer, 5'-ACACTTTCCTCCCCTTATGGATTC-3', TaqMan® MGB probes, FAM for 1G, 5'-ATAATTAGAAAGATATGACTTATC-3' and VIC for 2G, 5'-ATAATTAGAAAGGATATGACTTAT-3'; used for the MMP-3 SNP were: Forward primer, 5'-ACATCACTGCCACCACTCTGTT-3' and reverse primer, 5'-GGCACCTGGCCTAAAGACATT-3', TaqMan® MGB probes, FAM for 5A, 5'-AAGACATGGTTTTTC-3' and VIC for 6A, 5'-AGACATGGTTTTTTC-3'.
Statistical analysis
The Chi-square test was used to examine the differences in genotype distribution of the MMP-1 and MMP-3 promoters between the OSCC cases and control groups, and to estimate correlation or synergistic effects of MMP-1 genotypes with regard to clinical consequences as well as environmental factors among the OSCC cases. A p-value of < 0.05 was considered as statistically significant. Univariate analysis was performed by Fisher's exact test (two-sided) on gender, carrier state of MMP-1 1G allele (1G+ or 1G-) and 2G allele (2G+ or 2G-) between the OSCC and control groups. In the consideration of latent interrelations between factors, the effects of MMP-1 2G allele, age and gender were estimated by a multivariate logistic regression model. For each parameter, the OSCC risk was accounted by Odds Ratios (OR) and 95% Confidence Intervals (95% CI). All of the statistical analyses were performed using the SPSS 11.5J software package (SPSS Japan Inc., Tokyo, Japan).
Results
Genotype distributions of MMP-1 and MMP-3 promoter polymorphisms in OSCC cases and control groups
The genotype distributions of the promoter SNPs in MMP-1 and MMP-3 genes did not indicate a departure from the Hardy-Weinberg equilibrium when they were examined separately in the OSCC (n = 170) and control (n = 164) groups, or in all the samples combined (n = 334) (χ2 < 3.84, p > 0.05). The frequency of 1G/2G or 2G/2G promoter genotypes having the 2G allele, which is associated with a high MMP-1 expression level, was significantly higher in the OSCC group, and the frequency of the 1G/1G homozygote was lower than that of the control group (p = 0.034, Table 1). On the other hand, no difference in MMP-3 genotype distribution (5A/5A, 5A/6A, and 6A/6A) was detected between the OSCC case and control groups.
Table 1.
MMP-1and MMP-3 genotype distribution in OSCC cases and controls
| OSCC cases (n = 170) | Controls (n = 164) | p | |
| MMP-1 | |||
| 2G/2G | 77 (45.3) | 64 (39.0) | 0.034 |
| 1G/2G | 79 (46.5) | 71 (43.3) | |
| 1G/1G | 14 (8.2) | 29 (17.7) | |
| MMP-3 | |||
| 5A/5A | 3 (1.8) | 8 (4.9) | 0.188 |
| 5A/6A | 50 (29.4) | 54 (32.9) | |
| 6A/6A | 117 (68.8) | 102 (62.2) |
The data were analyzed by the χ2 test.
Association between MMP-1 promoter genotypes and various clinical parameters
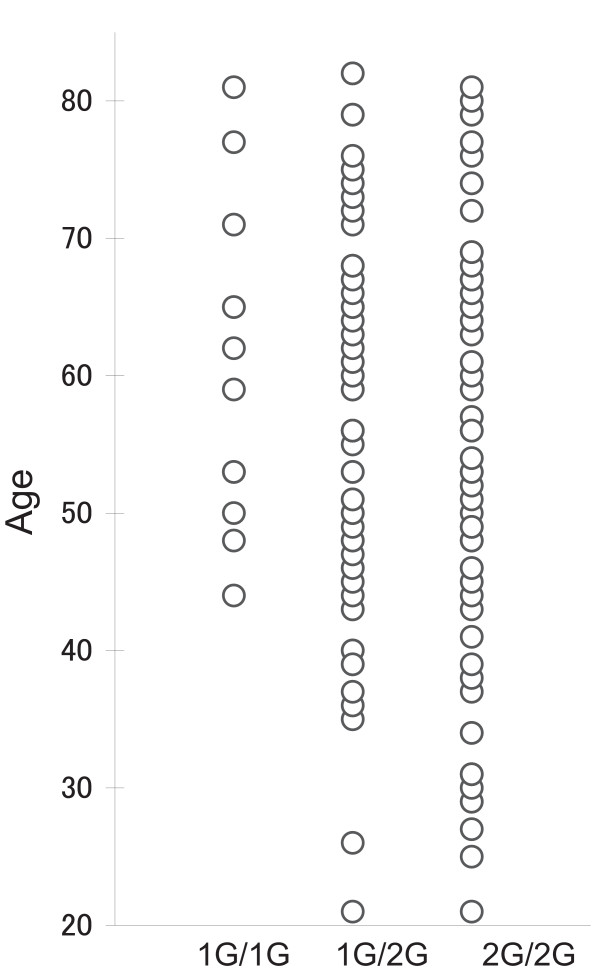
MMP-1 promoter genotypes of OSCC cases were stratified by clinical parameters including gender, age (Table 2), T category, lymph-node metastasis (N category), tumor location in the oral cavity, status of alcohol intake and smoking (Table 3). A significant association was detected only between the age and MMP-1 genotype, which suggests accumulation of older age patients with the 1G allele, or young age patients with the 2G allele. Figure 1 shows the age distribution pattern of subjects with MMP-1 promoter genotypes in OSCC groups, demonstrating a remarkable reduction of the 1G/1G and 1G/2G genotype distributions in OSCC cases less than 45 years and 35 years old. Receiver operating characteristic (ROC) curve consistently exhibited that the 45 years of age could be an optimal cutoff value of the age at which to stratify the young OSCC from the older bracket in following analyses. It was of considerable interest to notice that the MMP-1 promoter genotype has a remarkable difference in distribution between subjects over and under 45 years of age. A significant difference was demonstrated in susceptibility to OSCC in individuals less or more than 45 years old (p = 0.002, OR = 2.26, 95%CI = 1.35–3.79) (Table 4). No association was observed with the 1G allele (1G/1G and 1G/2G; p = 0.294, OR = 1.29, 95%CI = 0.84–2.00, whereas a significantly elevated risk of OSCC was exhibited with the 2G allele (2G/2G and 1G/2G; p = 0.016, OR = 2.39, 95%CI = 1.21–4.72. The environmental factors, alcohol intake and smoking status were stratified with MMP-1 genotype distributions in OSCC cases, but no significant association was demonstrated of either factor with the MMP-1 genotype distribution (Table 3).
Table 2.
Age and gender distribution in relation to alleles in cases and controls
| OSCC cases | Controls | |||||||
| 2G/2G | 1G/2G | 1G/1G | p | 2G/2G | 1G/2G | 1G/1G | p | |
| Age* | 54.8 ± 15.1 | 57.5 ± 13.2 | 60.1 ± 10.9 | 0.277 | 52.2 ± 14.8 | 52.3 ± 14.5 | 48.1 ± 14.2 | 0.387 |
| Gender# | ||||||||
| males | 46 (59.7%) | 53 (67.1%) | 8 (57.1%) | 0.570 | 38 (59.4%) | 46 (64.8%) | 20 (69%) | 0.640 |
| females | 31 (40.3%) | 26 (32.9%) | 6 (42.9%) | 26 (40.6%) | 25 (35.2%) | 9 (31%) | ||
Data are expressed as mean ± SD or number of subjects (%).
* One-way ANOVA test.
# χ2 test.
Table 3.
Relation of MMP-1 genotypes to clinical parameters and environmental factors among the OSCC cases
| 2G/2G n (%) | 1G/2G n (%) | 1G/1G n (%) | p | |
| Total | 77 (45.3) | 79 (46.5) | 14 (8.2) | |
| Gender | ||||
| Male | 46 (45.9) | 53 (47.5) | 8 (7.4) | 0.57 |
| Female | 31 (47.2) | 26 (41.3) | 6 (7.5) | |
| Age | ||||
| (years ± SD) | 54.8 ± 15.1 | 57.5 ± 13.2 | 60.1 ± 10.9 | 0.277* |
| T category | ||||
| T1-2 | 55 (45.1) | 58 (47.5) | 9 (7.4) | 0.78 |
| T3-4 | 22 (45.8) | 21 (43.8) | 5 (10.4) | |
| N category | ||||
| N0 | 50 (43.9) | 53 (46.5) | 11 (9.6) | 0.607 |
| N1-3 | 27 (48.2) | 26 (46.4) | 3 (5.4) | |
| Tumor location | ||||
| Tongue | 45 (54.9) | 31 (37.8) | 6 (7.3) | 0.260# |
| Lower gingiva | 14 (35) | 24 (60) | 2 (5) | |
| Oral floor | 6 (35.3) | 9 (52.9) | 2 (11.8) | |
| Buccal mucosa | 3 (21.4) | 9 (64.3) | 2 (14.3) | |
| Upper gingiva | 7 (53.8) | 5 (38.5) | 1 (7.7) | |
| Palate | 2 (50) | 1 (25) | 1 (25) | |
| Alcohol intake | ||||
| Drinker | 45 (45.9) | 45 (45.9) | 8 (8.2) | 0.982 |
| Non-drinker | 32 (44.4) | 34 (47.2) | 6 (8.3) | |
| Smoking status | ||||
| Smoker | 39 (44.3) | 43 (48.8) | 6 (6.8) | 0.702 |
| Non-smoker | 38 (46.3) | 36 (43.9) | 8 (9.8) |
T and N categories were according to the UICC TNM classification of malignant tumors for lip and oral cavity. The data were analyzed by the χ2.
* One-way ANOVA test.
# Fisher's exact tests.
Figure 1.
Age distribution of the MMP-1 genotypes in 170 OSCC cases between the ages of 20 and 80 years. The frequency of the 1G/1G genotype is notably low. Note the clear reduction of the 1G/1G and 1G/2G genotype distributions in individuals under the ages of 45 and 35 years, respectively.
Table 4.
Univariate analysis of predictive factors
| OSCC | Controls | p | OR (95% CI) | |
| Age | 0.002 | 2.26 (1.35–3.79) | ||
| <45 | 29 | 52 | ||
| ≧45 | 141 | 112 | ||
| Gender | 1.000 | 0.98 (0.63–1.53) | ||
| Male | 107 | 104 | ||
| Female | 63 | 60 | ||
| 1Ga | 0.294 | 1.29 (0.84–2.00) | ||
| - | 77 | 64 | ||
| + | 93 | 100 | ||
| 2Gb | 0.016 | 2.39 (1.21–4.72) | ||
| - | 14 | 29 | ||
| + | 156 | 135 |
a: 1G- denotes 2G/2G, and 1G+ denotes 1G/1G or 1G/2G. b: 2G- denotes 1G/1G, and 2G+ denotes 2G/2G or 1G/2G.
Data were analyzed by Fisher's exact test. The odds ratio and 95% CI were calculated.
Multivariate analyses of MMP-1 allele frequencies and clinical parameters
Logistic regression analysis of OSCC in relation to age, gender, and presence of the 1G and 2G alleles revealed that subjects of 45 years old and older had a 2.47-fold significantly increased risk of OSCC (p = 0.0006, 95%CI = 1.47–4.14) and that those carrying the MMP-1 2G allele had a 2.30-fold significantly elevated risk (p = 0.018, 95%CI = 1.15–4.58). Thus it was demonstrated that age and the presence of the 2G allele were independently associated with OSCC onset (Table 5).
Table 5.
Multivariate analysis of factors affecting OSCC
| A Results of factors affecting OSCC | ||||
| β coefficient | OR | 95% CI of OR | p | |
| 2G+ | 0.83 | 2.30 | (1.15–4.58) | 0.0180 |
| Age | 0.90 | 2.47 | (1.47–4.14) | 0.0006 |
| B Results showing the alleles independently associated with OSCC (adjusted for age and gender). | ||||
| Allele | β coefficient | OR | 95% CI of OR | p |
| 1G/2G | 0.782 | 2.187 | (1.06–4.51) | 0.034 |
| 2G/2G | 0.907 | 2.476 | (1.20–5.13) | 0.015 |
A: 2G+ : 2G- = 0, 2G+ = 1
Age : <45 = 0, ≧45 = 1
B: With adjustment for age and gender Alleles are included as multinomial variables with categorical coding in reference to 1G/1G allele.
% concordance = 74.9%.
Hosmer-Lemeshow Goodness-of-fit test: χ2 test = 0.996 ; p = 0.998
Discussion
In this study, we examined SNPs in the promoter regions of MMP-1 and MMP-3 genes in relation to OSCC risk with case-control analyses. Significant differences, i.e., high frequency of 2G/2G genotype and decreased frequency of 1G/1G genotype, were observed in the MMP-1 genotype distribution in OSCC cases (p = 0.034, Table 1). Similarly, in comparisons of allele frequency a significant correlation was detected between onset of OSCC and genotypes that carry the MMP-1 promoter 2G allele in homo- or hetero-form (p = 0.016, OR = 2.39, 95%CI = 1.21–4.72). MMP-1 with the 2G type promoter caused a higher expression level of MMP-1 in tissues [11]. The biological mechanism of the elevated risk of OSCC as related to the 2G allele of MMP-1 promoter includes genetic instability, which is accompanied by the cell cycle activation caused by a sequence of events led by increased MMP-1 enzyme activity, i.e. activation of tissue disruption, reconstruction and resultant release of ECM binding growth factors. The relationship between MMP-1 promoter polymorphism and risk of OSCC has been investigated by Lin et al. in a group of 121 cases [22] and by Cao et al. in a group of 96 cases [23] and by Vairaktaris et al. in a group of 156 cases [24]. Although both Lin et al. and Cao et al.reported an elevation of OSCC risk correlated with the MMP-1 2G allele, further studies were needed to reach a conclusion mainly because the numbers of cases in the previous studies were relatively small, and there were differences between these reports in background analyses on correlation with environmental risk factors, such as smoking and areca use. In this study, significant correlations were found between the presence of the MMP-1 promoter 2G allele and increased OSCC risk among 170 Japanese OSCC patients. These results are consistent with existing reports on malignant neoplasms in general. It is notable that a new finding on the molecular function of MMP-1 in the onset of OSCC was obtained from the characteristic pattern of the MMP-1 promoter genotype distribution in younger patients.
Interestingly, Vairaktaris et al. reported an increased risk of oral cancer with MMP-1 1G/2G polymorphism [24]. The discrepancy of the results of the Chinese studies and our report on one hand and the European (German and Greek) study on the other hand may be explained by the diverse ethnic background of the different studied populations. Another point of difference is the fact that their patient sample included patients with positive family history of thrombophilia.
The observed bias of the average age by the MMP-1 promoter genotype among the 170 OSCC cases of this study suggested an influence of the MMP-1 promoter 2G allele on the age of OSCC onset. The scatter plot of age on the MMP-1 promoter genotypes also revealed disappearance of the 1G/1G-genotype distribution among the OSCC cases under 45 years old. In agreement with this observation, the ROC analysis suggested that the age of 45 years is the borderline age above which a change occurs in the incidence of OSCC. Although the specific reasons for these results have not been clarified, they suggest that some kind of biological conditions related to carcinogenesis have initiated around the age of 45. Carcinogenesis is caused by synergistic effects of various factors [25,26]. The multivariate logistic regression analysis showed that aging and presence of the MMP-1 2G allele (i.e., 2G/2G or 1G/2G) are independently involved in onset of OSCC. In fact, it was clarified that the significance of the presence of the MMP-1 2G allele was lower in the subject group 45 years old or older (p = 0.238, OR = 1.65, 95% CI = 0.75–3.55), and that the impact of the allele was highly significant in the younger group, which was under 45 years old (p = 0.014, OR = 9.67, 95% CI = 1.20–78.15) (data not shown).
As concrete causes of OSCC, mainly tobacco smoking and alcohol usage and, in some cases, viral infections have attracted attention as environmental causative factors [25,27]. It has been suggested that tobacco smoking and alcohol usage alone may not explain the mechanism of the entire early onset of OSCC, because the duration of exposure to these risk factors in young OSCC patients is shorter than in the older group, and also because there are some cases with stable incidence that have no known risk factors [28]. The association with smoking and habitual drinking has been supported as the risk factors of OSCC, which generally shows a higher incidence in older age, but other investigators believe that the mechanism of the early onset OSCC is fundamentally different from that of elderly onset OSCC [25]. Cao et al. considered the relationship with smoking as a behavioral risk factor and the MMP-1 2G allele as a genetic risk factor in the OSCC group [23]. In lung cancer, it has been similarly shown that a genetic factor of the MMP-1 promoter 2G allele increases the risk of cancer that occurs in a tobacco-usage-dependent manner only in cases with a history of tobacco use. These reports support the role of MMP-1 promoter polymorphism as an endogenous background factor, in contrast to exogenous environmental factors [15]. However, no evidence to support a notion of synergistic interactions between risk factors, such as habitual smoking and drinking and MMP-1 promoter polymorphism in OSCC cases, was shown in this study. Further investigations with regard to frequency and duration of exposure are required to consider interactions between environmental factors and multiple genetic background factors.
Examples are known of malignant neoplasms caused by genetic factors, for example, mutations in RB in Retinoblastoma [29], p53 in Li-Fraumeni Syndrome [30], and APC in familial adenomatous polyposis [31]. There are also reports of mutations in BRCA1 and BRCA2, which affect familial breast cancer occurrence, though their penetrance is low [32]. These are neoplasms that are all caused by loss-of-function mutations in molecules functionally classified as tumor-suppressor genes, and they are characterized by familial, juvenile or young onset and may be multicentric or bilateral. Although incidents are rare in the population, they are examples of germline mutations that directly involve heterofamilial tumorigenesis.
By contrast, the MMP-1 promoter 2G allele is a genetic polymorphism that exists at the high allele frequency of 80% to 90% in the general population. It is possible to call this a hereditary trait that is shared among races or humans in general. Other genetic factors that are classified into similar polymorphism as MMP-1 have also been reported, such as Cyclin D1 (CCND1) in head and neck squamous cell carcinoma (HNSCC) and colorectal cancer [33,34], xeroderma pigmentosum complementary group D (XPD), DNA damage binding protein 2 (DDB2), and MMP-9 in lung cancer [35-37]. Similar to the effects of mutations in tumor suppressor genes, diversity in gene expression level and molecular structure caused by genetic polymorphisms affect monitoring and repair mechanism of DNA replication, as well as control of the cell cycle, ultimately resulting in genetic instability. The common mechanism of carcinogenesis caused by those genetic factors is an elevated carcinogenic risk due to this genetic instability.
As examples of genetic polymorphisms that affect onset age of cancers other than that examined in this study, some reports discuss MMP-1 and DDB2 in lung cancer [15,36], and CCND1 in HNSCC and colorectal cancer [33,34]. These genetic factors, on the other hand, are present in patients with cancer as well as in the general population at certain frequencies. Therefore, it is hard to conclude that these genetic factors are the primary factors in early onset carcinogenesis, unlike germline single-gene mutations in Rb and APC that induce juvenile or early onset of cancers with high penetrance. Aging brings exposure to various carcinogenic factors and is associated with inevitable accumulation of genetic and epigenetic modifications of genes. These accumulations interact synergistically with biological background factors on the host side, and consequently cancer may develop [26,38]. It seems that inherited genetic factors play a larger role in development of early onset cancer that has undergone a relatively short duration of exposure to carcinogen through environment and lifestyle habits. Therefore, it is conceivable that the impact of these genetic factors would appear more directly in younger than in older cases, although we still expect a synergistic involvement of various environmental and genetic factors. Nevertheless, because of the disappearance ofthe MMP-1 1G allele distribution observed in the OSCC cases with a clear boundary under the age of 45 years, the MMP-1 promoter 2G allele should be recognized as an essential genetic precondition for the development of early onset OSCC.
It is said that an onset age of 45 years and younger accounts for about 6% of OSCC cases [27]. It should be noted that in this study we found that the tongue was the primary site in 25 cases (86.2%) of 29 early onset OSCC cases in individuals under 45 years old. This primary site was obviously different from that in patients 45 years old and older in whom we noted 57 cases of tongue cancer (40.4%) out of 141 OSCC cases. Similar tendencies have been reported in previous studies [39,40]. These findings suggest the possibility that each primary tumor sites in the oral cavity may be associated with differences in cancer susceptibility, specific carcinogenic stimulation, or genetic background. However, no environmental or genetic factors specific to a particular site of the oral mucosa have been identified for OSCC. It is conceivable that it would be important to carry out further investigations on genetic and environmental risk factors for each anatomical site of the oral regions, though we are not able to discuss this aspect of OSCC because the number of cases was inadequate in this study.
Conclusion
The number of cases in this study was relatively small; therefore, the conclusions may still be contingent upon confirmation in a larger study. To evaluate the conclusive impact of MMP-1 on OSCC risk, a sufficiently large number of cases or consistency among results from multiple age adjusted studies would be needed. Furthermore, although the MMP-1 promoter SNP-based determination of OSCC susceptibility has the potential to become a useful clinical tool, it is necessary to add a greater diversity of information for practical use. In the future, improvements in diagnosis of susceptibility and clinical application could become possible by incorporating multiple genetic and environmental risk factors into the prediction model for cancer occurrence. Information about the risk of various types of malignant neoplasm as well as OSCC is useful for prevention and early detection of cancer or for monitoring of postoperative recurrence. A diagnostic system for evaluating cancer risk is vital not only for improvement in treatment techniques but also as a theoretical foundation to build strategies for cancer prevention.
Abbreviations
Matrix metalloproteinase (MMP), single nucleotide polymorphism (SNP), oral squamous cell carcinoma (OSCC), odds ratio (OR), 95% Confidence Intervals (95% CI), receiver operating characteristic curve (ROC), head and neck squamous cell carcinoma (HNSCC).
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
RN, MN participated in the design of the study. RN, MN and AAN drafted and wrote the manuscript. NK participated in the statistical analysis. RN, MN and AAN participated in the production of genotype data. RN, MN, KK, MO and HK participated in the acquisition and interpretation of data. RN, MI, HF, TK and AAN participated in the experimental studies. RN, MN, AAN, HH and SS carried out the clinical studies. SC, HY and RT participated in the review of the study. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
The authors thank the staff of the Division of Dental Clinic and Oral Surgery of Nagaoka Red Cross Hospital for their contribution in collecting samples and the clinical data set. This investigation was supported by grants from the Japan Society for the Promotion of Science (Grants-in-Aid for Scientific Research; no. 12791235 and no. 18592171).
Contributor Information
Rishiho Nishizawa, Email: ni4zawa@hsp.md.shinshu-u.ac.jp.
Masaki Nagata, Email: nagata@dent.niigata-u.ac.jp.
Arhab A Noman, Email: arhabn@dent.niigata-u.ac.jp.
Nobutaka Kitamura, Email: nktmr@m12.alpha-net.ne.jp.
Hajime Fujita, Email: fujita1@dent.niigata-u.ac.jp.
Hideyuki Hoshina, Email: hoshina@dent.niigata-u.ac.jp.
Takehiko Kubota, Email: kubota@dent.niigata-u.ac.jp.
Manami Itagaki, Email: ita@dent.niigata-u.ac.jp.
Susumu Shingaki, Email: shigaki@dent.niigata-u.ac.jp.
Makoto Ohnishi, Email: namakoto@dent.niigata-u.ac.jp.
Hiroshi Kurita, Email: hkurita@hsp.md.shinshu-u.ac.jp.
Kouji Katsura, Email: katsu@dent.niigata-u.ac.jp.
Chikara Saito, Email: ckrsaito@dent.niigata-u.ac.jp.
Hiromasa Yoshie, Email: yoshie@dent.niigata-u.ac.jp.
Ritsuo Takagi, Email: takagi@dent.niigata-u.ac.jp.
References
- Ziober BL, Turner MA, Palefsky JM, Banda MJ, Kramer RH. Type I collagen degradation by invasive oral squamous cell carcinoma. Oral oncology. 2000;36:365–372. doi: 10.1016/S1368-8375(00)00019-1. [DOI] [PubMed] [Google Scholar]
- Kerkela E, Saarialho-Kere U. Matrix metalloproteinases in tumor progression: focus on basal and squamous cell skin cancer. Experimental dermatology. 2003;12:109–125. doi: 10.1034/j.1600-0625.2003.120201.x. [DOI] [PubMed] [Google Scholar]
- Impola U, Uitto VJ, Hietanen J, Hakkinen L, Zhang L, Larjava H, Isaka K, Saarialho-Kere U. Differential expression of matrilysin-1 (MMP-7), 92 kD gelatinase (MMP-9), and metalloelastase (MMP-12) in oral verrucous and squamous cell cancer. The Journal of pathology. 2004;202:14–22. doi: 10.1002/path.1479. [DOI] [PubMed] [Google Scholar]
- Brinckerhoff CE, Rutter JL, Benbow U. Interstitial collagenases as markers of tumor progression. Clin Cancer Res. 2000;6:4823–4830. [PubMed] [Google Scholar]
- Nagata M, Fujita H, Ida H, Hoshina H, Inoue T, Seki Y, Ohnishi M, Ohyama T, Shingaki S, Kaji M, et al. Identification of potential biomarkers of lymph node metastasis in oral squamous cell carcinoma by cDNA microarray analysis. International journal of cancer. 2003;106:683–689. doi: 10.1002/ijc.11283. [DOI] [PubMed] [Google Scholar]
- Murray GI, Duncan ME, O'Neil P, McKay JA, Melvin WT, Fothergill JE. Matrix metalloproteinase-1 is associated with poor prognosis in oesophageal cancer. The Journal of pathology. 1998;185:256–261. doi: 10.1002/(SICI)1096-9896(199807)185:3<256::AID-PATH115>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- Shiozawa J, Ito M, Nakayama T, Nakashima M, Kohno S, Sekine I. Expression of matrix metalloproteinase-1 in human colorectal carcinoma. Mod Pathol. 2000;13:925–933. doi: 10.1038/modpathol.3880169. [DOI] [PubMed] [Google Scholar]
- Shima I, Sasaguri Y, Kusukawa J, Yamana H, Fujita H, Kakegawa T, Morimatsu M. Production of matrix metalloproteinase-2 and metalloproteinase-3 related to malignant behavior of esophageal carcinoma. A clinicopathologic study. Cancer. 1992;70:2747–2753. doi: 10.1002/1097-0142(19921215)70:12<2747::AID-CNCR2820701204>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- Kurahara S, Shinohara M, Ikebe T, Nakamura S, Beppu M, Hiraki A, Takeuchi H, Shirasuna K. Expression of MMPS, MT-MMP, and TIMPs in squamous cell carcinoma of the oral cavity: correlations with tumor invasion and metastasis. Head & neck. 1999;21:627–638. doi: 10.1002/(SICI)1097-0347(199910)21:7<627::AID-HED7>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- Ye S. Polymorphism in matrix metalloproteinase gene promoters: implication in regulation of gene expression and susceptibility of various diseases. Matrix Biol. 2000;19:623–629. doi: 10.1016/S0945-053X(00)00102-5. [DOI] [PubMed] [Google Scholar]
- Rutter JL, Mitchell TI, Buttice G, Meyers J, Gusella JF, Ozelius LJ, Brinckerhoff CE. A single nucleotide polymorphism in the matrix metalloproteinase-1 promoter creates an Ets binding site and augments transcription. Cancer research. 1998;58:5321–5325. [PubMed] [Google Scholar]
- Ye S, Eriksson P, Hamsten A, Kurkinen M, Humphries SE, Henney AM. Progression of coronary atherosclerosis is associated with a common genetic variant of the human stromelysin-1 promoter which results in reduced gene expression. The Journal of biological chemistry. 1996;271:13055–13060. doi: 10.1074/jbc.271.22.13244. [DOI] [PubMed] [Google Scholar]
- Hinoda Y, Okayama N, Takano N, Fujimura K, Suehiro Y, Hamanaka Y, Hazama S, Kitamura Y, Kamatani N, Oka M. Association of functional polymorphisms of matrix metalloproteinase (MMP)-1 and MMP-3 genes with colorectal cancer. International journal of cancer. 2002;102:526–529. doi: 10.1002/ijc.10750. [DOI] [PubMed] [Google Scholar]
- Kanamori Y, Matsushima M, Minaguchi T, Kobayashi K, Sagae S, Kudo R, Terakawa N, Nakamura Y. Correlation between expression of the matrix metalloproteinase-1 gene in ovarian cancers and an insertion/deletion polymorphism in its promoter region. Cancer research. 1999;59:4225–4227. [PubMed] [Google Scholar]
- Zhu Y, Spitz MR, Lei L, Mills GB, Wu X. A single nucleotide polymorphism in the matrix metalloproteinase-1 promoter enhances lung cancer susceptibility. Cancer research. 2001;61:7825–7829. [PubMed] [Google Scholar]
- Nishioka Y, Kobayashi K, Sagae S, Ishioka S, Nishikawa A, Matsushima M, Kanamori Y, Minaguchi T, Nakamura Y, Tokino T, et al. A single nucleotide polymorphism in the matrix metalloproteinase-1 promoter in endometrial carcinomas. Jpn J Cancer Res. 2000;91:612–615. doi: 10.1111/j.1349-7006.2000.tb00989.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirata H, Naito K, Yoshihiro S, Matsuyama H, Suehiro Y, Hinoda Y. A single nucleotide polymorphism in the matrix metalloproteinase-1 promoter is associated with conventional renal cell carcinoma. International journal of cancer. 2003;106:372–374. doi: 10.1002/ijc.11229. [DOI] [PubMed] [Google Scholar]
- Hashimoto T, Uchida K, Okayama N, Imate Y, Suehiro Y, Hamanaka Y, Ueyama Y, Shinozaki F, Yamashita H, Hinoda Y. Association of matrix metalloproteinase (MMP)-1 promoter polymorphism with head and neck squamous cell carcinoma. Cancer letters. 2004;211:19–24. doi: 10.1016/j.canlet.2004.01.032. [DOI] [PubMed] [Google Scholar]
- Ghilardi G, Biondi ML, Caputo M, Leviti S, DeMonti M, Guagnellini E, Scorza R. A single nucleotide polymorphism in the matrix metalloproteinase-3 promoter enhances breast cancer susceptibility. Clin Cancer Res. 2002;8:3820–3823. [PubMed] [Google Scholar]
- Sutinen M, Kainulainen T, Hurskainen T, Vesterlund E, Alexander JP, Overall CM, Sorsa T, Salo T. Expression of matrix metalloproteinases (MMP-1 and -2) and their inhibitors (TIMP-1, -2 and -3) in oral lichen planus, dysplasia, squamous cell carcinoma and lymph node metastasis. British journal of cancer. 1998;77:2239–2245. doi: 10.1038/bjc.1998.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan RC, Macabeo-Ong M, Shiboski CH, Dekker N, Ginzinger DG, Wong DT, Schmidt BL. Overexpression of matrix metalloproteinase-1 and -9 mRNA is associated with progression of oral dysplasia to cancer. Clin Cancer Res. 2004;10:6460–6465. doi: 10.1158/1078-0432.CCR-04-0656. [DOI] [PubMed] [Google Scholar]
- Lin SC, Chung MY, Huang JW, Shieh TM, Liu CJ, Chang KW. Correlation between functional genotypes in the matrix metalloproteinases-1 promoter and risk of oral squamous cell carcinomas. J Oral Pathol Med. 2004;33:323–326. doi: 10.1111/j.1600-0714.2004.00214.x. [DOI] [PubMed] [Google Scholar]
- Cao ZG, Li CZ. A single nucleotide polymorphism in the matrix metalloproteinase-1 promoter enhances oral squamous cell carcinoma susceptibility in a Chinese population. Oral oncology. 2006;42:32–38. doi: 10.1016/j.oraloncology.2004.08.015. [DOI] [PubMed] [Google Scholar]
- Vairaktaris E, Yapijakis C, Derka S, Serefoglou Z, Vassiliou S, Nkenke E, Ragos V, Vylliotis A, Spyridonidou S, Tsigris C, et al. Association of matrix metalloproteinase-1 (-1607 1G/2G) polymorphism with increased risk for oral squamous cell carcinoma. Anticancer research. 2007;27:459–464. [PubMed] [Google Scholar]
- Llewellyn CD, Johnson NW, Warnakulasuriya KA. Risk factors for squamous cell carcinoma of the oral cavity in young people – a comprehensive literature review. Oral oncology. 2001;37:401–418. doi: 10.1016/S1368-8375(00)00135-4. [DOI] [PubMed] [Google Scholar]
- Kuwano H, Kato H, Miyazaki T, Fukuchi M, Masuda N, Nakajima M, Fukai Y, Sohda M, Kimura H, Faried A. Genetic alterations in esophageal cancer. Surgery today. 2005;35:7–18. doi: 10.1007/s00595-004-2885-3. [DOI] [PubMed] [Google Scholar]
- Herrero R, Castellsague X, Pawlita M, Lissowska J, Kee F, Balaram P, Rajkumar T, Sridhar H, Rose B, Pintos J, et al. Human papillomavirus and oral cancer: the International Agency for Research on Cancer multicenter study. Journal of the National Cancer Institute. 2003;95:1772–1783. doi: 10.1093/jnci/djg107. [DOI] [PubMed] [Google Scholar]
- Llewellyn CD, Johnson NW, Warnakulasuriya KA. Risk factors for oral cancer in newly diagnosed patients aged 45 years and younger: a case-control study in Southern England. J Oral Pathol Med. 2004;33:525–532. doi: 10.1111/j.1600-0714.2004.00222.x. [DOI] [PubMed] [Google Scholar]
- Lee WH, Bookstein R, Hong F, Young LJ, Shew JY, Lee EY. Human retinoblastoma susceptibility gene: cloning, identification, and sequence. Science. 1987;235:1394–1399. doi: 10.1126/science.3823889. [DOI] [PubMed] [Google Scholar]
- Wong P, Verselis SJ, Garber JE, Schneider K, DiGianni L, Stockwell DH, Li FP, Syngal S. Prevalence of early onset colorectal cancer in 397 patients with classic Li-Fraumeni syndrome. Gastroenterology. 2006;130:73–79. doi: 10.1053/j.gastro.2005.10.014. [DOI] [PubMed] [Google Scholar]
- Nishisho I, Nakamura Y, Miyoshi Y, Miki Y, Ando H, Horii A, Koyama K, Utsunomiya J, Baba S, Hedge P. Mutations of chromosome 5q21 genes in FAP and colorectal cancer patients. Science. 1991;253:665–669. doi: 10.1126/science.1651563. [DOI] [PubMed] [Google Scholar]
- Golshan M, Miron A, Nixon AJ, Garber JE, Cash EP, Iglehart JD, Harris JR, Wong JS. The prevalence of germline BRCA1 and BRCA2 mutations in young women with breast cancer undergoing breast-conservation therapy. American journal of surgery. 2006;192:58–62. doi: 10.1016/j.amjsurg.2005.12.005. [DOI] [PubMed] [Google Scholar]
- Huang WS, Tang R, Lin PY, Changchien CR, Chen JS, Chiang JM, Yeh CY, Wang JY, Hsieh LL. Impact of the cyclin D1 A870G polymorphism on susceptibility to sporadic colorectal cancer in Taiwan. Diseases of the colon and rectum. 2006;49:602–608. doi: 10.1007/s10350-005-0311-6. [DOI] [PubMed] [Google Scholar]
- Zheng Y, Shen H, Sturgis EM, Wang LE, Eicher SA, Strom SS, Frazier ML, Spitz MR, Wei Q. Cyclin D1 polymorphism and risk for squamous cell carcinoma of the head and neck: a case-control study. Carcinogenesis. 2001;22:1195–1199. doi: 10.1093/carcin/22.8.1195. [DOI] [PubMed] [Google Scholar]
- Liang G, Xing D, Miao X, Tan W, Yu C, Lu W, Lin D. Sequence variations in the DNA repair gene XPD and risk of lung cancer in a Chinese population. International journal of cancer. 2003;105:669–673. doi: 10.1002/ijc.11136. [DOI] [PubMed] [Google Scholar]
- Hu Z, Shao M, Yuan J, Xu L, Wang F, Wang Y, Yuan W, Qian J, Ma H, Wang Y, et al. Polymorphisms in DNA damage binding protein 2 (DDB2) and susceptibility of primary lung cancer in the Chinese: a case-control study. Carcinogenesis. 2006;27:1475–1480. doi: 10.1093/carcin/bgi350. [DOI] [PubMed] [Google Scholar]
- Hu Z, Huo X, Lu D, Qian J, Zhou J, Chen Y, Xu L, Ma H, Zhu J, Wei Q, et al. Functional polymorphisms of matrix metalloproteinase-9 are associated with risk of occurrence and metastasis of lung cancer. Clin Cancer Res. 2005;11:5433–5439. doi: 10.1158/1078-0432.CCR-05-0311. [DOI] [PubMed] [Google Scholar]
- Ha PK, Califano JA. Promoter methylation and inactivation of tumour-suppressor genes in oral squamous-cell carcinoma. The lancet oncology. 2006;7:77–82. doi: 10.1016/S1470-2045(05)70540-4. [DOI] [PubMed] [Google Scholar]
- Shiboski CH, Schmidt BL, Jordan RC. Tongue and tonsil carcinoma: increasing trends in the U.S. population ages 20–44 years. Cancer. 2005;103:1843–1849. doi: 10.1002/cncr.20998. [DOI] [PubMed] [Google Scholar]
- Myers JN, Elkins T, Roberts D, Byers RM. Squamous cell carcinoma of the tongue in young adults: increasing incidence and factors that predict treatment outcomes. Otolaryngol Head Neck Surg. 2000;122:44–51. doi: 10.1016/S0194-5998(00)70142-2. [DOI] [PubMed] [Google Scholar]