Abstract
Objectives. We explored how income and skin color interact to influence the blood pressure of African American adults enrolled in the longitudinal Coronary Artery Risk Development in Young Adults (CARDIA) Study.
Methods. Data were derived from 1893 African American CARDIA year-15 participants who had undergone skin reflectance assessments at year 7. We adjusted for age, gender, body mass index, smoking status, and use of antihypertensive medication to examine whether year-15 self-reported family incomes, in interaction with skin reflectance, predicted blood pressure levels.
Results. Mean systolic and diastolic blood pressure levels were 117.1 (±16.07) and 76.9 (±12.5) mm Hg, respectively. After adjustment, the interaction between skin reflectance and income was significantly associated with systolic blood pressure (P< .01). Among lighter-skinned African Americans, systolic pressure decreased as income increased (b= −1.15, P<.001); among those with darker skin, systolic blood pressure increased with increasing income (b=0.10, P=.75).
Conclusions. The protective gradient of income on systolic blood pressure seen among African Americans with lighter skin is not observed to the same degree among those with darker skin. Psychosocial stressors, including racial discrimination, may play a role in this relationship.
In the United States, marked racial disparities in morbidity and mortality exist across a wide range of health indicators.1,2 Gaps in health between African Americans and White Americans are particularly pronounced for cardiovascular diseases and their related risk factors3,4 and persist despite considerable advances in clinical treatment and care.5 Rates of hypertension (blood pressure above 140/90 mm Hg) are nearly twice as high among African Americans as among Whites, and the condition tends to be more severe and to have an earlier onset among African Americans.6 This racial disparity in hypertension is also the largest contributor to broader all-cause mortality differentials between African and White Americans.7
Racial disparities in health are complex in terms of their underlying causes and are not completely understood, with a range of social–environmental factors implicated in the poorer cardiovascular health of African Americans. One such factor is socioeconomic status (SES), which is associated with cardiovascular disease risk in a gradient fashion in the United States and other developed nations and is lower on average among African Americans than among Whites.8,9 However, evidence has increasingly suggested that race and class interact in complex ways to influence health, and the magnitude of association between SES and health varies according to race.10–15
Although the relationship has been less consistent, skin color is another socially significant factor that has shown a graded association with cardiovascular health, particularly blood pressure, among African Americans.16–18 Given the social significance of skin color in United States society,19–21 it may constitute an additional factor along which SES effects on health vary.
The well-documented SES gradient in health, wherein incremental increases in economic standing are associated with improved health across the entire SES range, suggests that psychosocial stress may be an important contributor to health disparities.9,22 Because African Americans are overrepresented at the bottom of the SES ladder, some social–environmental models of health disparities have posited that economic factors are largely responsible for race gaps in health status.12 However, it is now well demonstrated that SES alone does not account for racial health disparities, and the effects of SES on health are not uniform across race groups.10,11,13,23
For example, Farmer and Ferraro13 recently demonstrated that although the SES gradient is strong for White Americans, economic success does not carry the same health benefits for African Americans. They observed a pattern of “diminishing returns”13(p192) in general health status among African Americans of higher economic standing. A similar pattern was recently observed with respect to body mass index (BMI; weight in kilograms divided by height in meters squared), an important cardiovascular risk factor. Lewis et al.14 found that, among women, racial differences in BMI were most pronounced at higher levels of education, with White women having lower BMIs than African American women.
These findings highlight the complexity of interactions among race and class and suggest that additional social–environmental factors should be considered in attempts to explain racial health disparities. An example of such a social–environmental factor is skin color.19,24 A skin color gradient in blood pressure, such that darker skin color is associated with higher average blood pressure levels, has long been observed among African Americans and other African diaspora populations.16,19,25 In the first observations of this gradient, during the 1970s, the relationship was largely attributed to genetic or unknown physiological causes.16,25
However, skin color has been shown to be an imperfect marker of proportional genetic ancestry in multiracial societies.26,27 In addition, genetic components seem to explain relatively little population-level prevalence rates of common, complex diseases such as hypertension.28 Thus, skin color is not likely to be a significant marker of differences in gene-based disease susceptibility.27
Skin color has long been recognized to carry considerable social significance in United States society, however, and many studies have noted the potential confounding effects of psychosocial factors on the skin color gradient in blood pressure.17–19,29,30 Relative to African Americans with lighter skin, it has been shown that, on average, African Americans with darker skin are employed in occupations with lower incomes and less prestige.31–33
Studies examining the potential confounding effects of economic status on the skin color gradient in blood pressure have produced mixed findings.16–18 Harburg et al. found that the relationship between skin color and blood pressure is independent of SES,16 whereas Keil et al. suggested that skin color differences in blood pressure are contingent on SES.17 Klag et al.18 found a moderating effect of SES on the association between skin color and blood pressure, with only individuals in lower socioeconomic tiers exhibiting the skin color gradient. The findings of these studies indicate that more research is needed regarding the interactive effects of skin color and SES on blood pressure among African Americans.
Recently, Gravlee et al.24,34 reported that, among adults in Puerto Rico, socially ascribed “color,” of which skin tone is a dimension, moderates the SES gradient in blood pressure. They found higher SES to be associated with lower blood pressure only among those of lighter ascribed color. A similar pattern may exist for skin pigmentation in the United States; whereas skin color is associated with SES, it is also a marker of other social realities and experiences that may affect health status, including discrimination and low social standing.19,35,36
Thus, skin color may represent an additional dimension of social variation along which health varies in the United States and, as such, may complicate the effects of SES on the health of African Americans. Similar to recent findings showing that the health benefits of higher SES are more limited for African Americans than they are for Whites,13 these benefits may also be more limited depending on one’s skin color.
We explored whether skin color is a significant moderator of the effects of SES on blood pressure among African Americans taking part in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. We sought to answer the following question: does the SES gradient in blood pressure vary among African Americans of darker skin color and those of lighter skin color?
METHODS
Data
The design of the CARDIA Study has been described in detail elsewhere.37,38 Briefly, CARDIA is a large epidemiological cohort study examining the development of cardiovascular risk factors in young adults. Data have been collected at 4 field sites: Birmingham, Ala; Chicago, Ill; Minneapolis, Minn; and Oakland, Calif. At baseline (1985–1986), 5115 African American and White participants were enrolled, and stratification was used to obtain approximately equal proportions of participants according to race (African American, White), gender, age (18–24 years, 25–30 years), and education (high school or less, more than high school) at each site. Participants were between the ages of 18 and 30 years at the time of their enrollment.
Fifteen years of data collection and 6 examination rounds have been completed, with postbaseline examinations taking place at years 2 (1987–1988), 5 (1990–1991), 7 (1992–1993), 10 (1995–1996), and 15 (2000–2001). Some loss to follow-up has occurred over the course of the study, but 74% of the surviving cohort was still enrolled during the most recent examination year (year 15). Data on a wide range of physiological and lifestyle–behavioral factors, as well as basic demographic and socioeconomic factors, have been collected at each examination.
With the exception of skin color, which was measured only during year 7 (1992–1993), our analyses focused on data from the most recent examination period (2000–2001). Analyses were restricted to participants who self-reported their race as African American; 1893 of these individuals remained enrolled in the study at year 15.
The outcome variables of interest were systolic blood pressure (SBP) and diastolic blood pressure (DBP). Resting values of these parameters were taken 3 times at each examination by trained technicians according to standard procedures. Values reflected the average of the second and third resting measurements.
Skin color measurements were obtained using a hand-held reflectance spectrophotometer that measured the percentage of light reflected from the surface of the skin. Measurements were taken on the underside of the upper arm, where pigmentation resulting from sun exposure is not likely. Higher skin reflectance scores corresponded to lighter skin color, and lower scores corresponded to darker skin color. Although amber, blue, and green filters were used to measure skin reflectance, we used data collected only with the amber filter to maintain consistency with previous CARDIA investigations.35
Measures of SES included family income and educational attainment. Self-reported annual family income was measured on a 9-point scale ranging from less than $5000 (1) to $100 000 or more (9). We treated this ordinal measure as a continuous variable in our analyses, given that the relationship between income and health was expected to be equitable across income scale points. Self-reported educational attainment was assessed on a 7-point scale ranging from less than high school (1) to professional degree (7).
Standard covariates included age, gender, smoking status (current vs other), and current use of high blood pressure medication; data on these measures were obtained through self-reports. Weight and height were measured during examinations, and we included BMI in our analyses as a covariate predictor of blood pressure.
Data Analysis
We categorized skin color into dark, medium, and light reflectance tertiles. We examined bivariate associations between skin color tertiles and participants’ sociodemographic characteristics as well as cardiovascular risk factor levels. We conducted linear regression analyses to examine bivariate associations between income and blood pressure.
To examine the question posed in our study (i.e., whether the effect of SES on blood pressure among African Americans varies according to the socially significant characteristic of skin color), we conducted multiple linear regression analyses testing the interactive effects of skin color and SES on blood pressure. All interaction analyses included the continuous skin reflectance variable. Models were run separately for SBP and DBP. In model 1, we tested the assumed underlying relationship between SES and blood pressure (the SES gradient). In model 2, we tested the main and interactive effects of skin color and income on blood pressure. In model 3, we added covariate data to model 2 to adjust for the effects of age, gender, smoking status, blood pressure medication use, and BMI.
When we found interactions of income and skin color with blood pressure, we repeated the modeling stratified by skin color tertile to more clearly illustrate the interactive relationship. We also examined educational level as a potential confounder but excluded this variable from the initial models as a result of its high correlation with income. Additional interactions with gender were examined as well.
Three individuals with SBP levels above 200 mm Hg were identified as outliers, and models including and not including these individuals were run to examine differences in effects. In addition, we ran models excluding individuals taking high blood pressure medication to determine whether effect sizes were altered.
RESULTS
The average skin reflectance score for our African American sample was 22.04 (±7.2). The cutoffs for skin reflectance tertiles were 18.3 between the dark and medium groups and 24.1 between the medium and light groups. By contrast, the average skin reflectance of White CARDIA participants was 46.1 (±4.1); however, the skin reflectance score ranges for the 2 groups overlapped nearly entirely (African Americans: 7.1–51.2; Whites: 14.4–56.4).
Across the 3 skin color tertiles, we found the expected gradients of decreasing blood pressure, BMI, and smoking prevalence and increasing income and education as skin color became lighter (Table 1 ▶). There were also gender differences according to skin color, with a significantly higher percentage of women in the light skin color group than in the dark skin color group.
TABLE 1—
Sociodemographic Characteristics and Cardiovascular Risk Factors Among African Americans by Skin Reflectance Tertile: Coronary Artery Risk Development in Young Adults Study, 2000–2001
| Total Sample | Dark Skin Tertile | Medium Skin Tertile | Light Skin Tertile | P for Trend | |
| Total, No. | 1893 | 635 | 636 | 622 | |
| Systolic blood pressure, mm Hg, mean (SD) | 117.1 (16.1) | 118.6 (16.3) | 117.1 (16.3) | 115.7 (15.4) | .02 |
| Diastolic blood pressure, mm Hg, mean (SD) | 76.9 (12.5) | 78.0 (12.7) | 76.5 (12.3) | 76.4 (12.7) | .08 |
| Skin reflectance score,a mean (SD) | 22.04 (7.2) | 14.9 (2.4) | 21.2 (1.6) | 30.2 (5.2) | < .001 |
| Body mass index,b kg/m2, mean (SD) | 30.49 (7.35) | 31.47 (7.96) | 30.27 (6.70) | 29.95 (7.19) | < .001 |
| Income scale score,c mean (SD) | 5.79 (2.17) | 5.57 (2.16) | 5.80 (2.15) | 6.18 (2.06) | < .001 |
| Education scale score,d mean (SD) | 2.74 (1.14) | 2.58 (1.05) | 2.72 (1.11) | 3.0 (1.24) | < .001 |
| Age, y, mean (SD) | 39.60 (3.82) | 39.60 (3.76) | 39.61 (3.74) | 39.94 (3.86) | .28 |
| Female, % | 56.12 | 44.41 | 59.12 | 68.97 | < .001 |
| Taking blood pressure medication, % | 12.46 | 14.37 | 13.41 | 9.34 | .04 |
| Current smoker, % | 52.14 | 55.58 | 50.00 | 49.28 | .09 |
Note. Skin reflectance was measured in 1992–1993; data for all other characteristics are from 2000–2001.
aHigher scores correspond to lighter skin color (see “Methods” for description of skin reflectance tertiles).
bBody mass index is weight in kilograms divided by height in meters squared.
cSelf-reported annual family income was measured on a 9-point scale, with 1 = less than $5000, 5 = $25 000–$34 999, and 9 = $100 000 or more.
d1 = less than high school, 7 = professional degree.
Systolic Blood Pressure
Results for model 1 demonstrated the presence of the expected socioeconomic gradient in SBP in our sample; that is, higher incomes were associated with lower SBP levels (Table 2 ▶). Results for model 2 showed that the interaction between continuous skin reflectance and income was a statistically significant predictor of SBP. Results for model 3, the full regression model, showed that this effect remained significant after we controlled for potential confounders. The unstandardized parameter estimate for the interaction between skin color and income remained virtually unchanged after adjustment for age, gender, BMI, smoking status, and blood pressure medication use.
TABLE 2—
Unstandardized Parameter Estimates From Linear Regression Models With Systolic and Diastolic Blood Pressure as Dependent Variables: Coronary Artery Risk Development in Young Adults Study, 2000–2001
| Model 1, b (SE) | Model 2, b (SE) | Model 3, b (SE) | |
| Systolic blood pressure | |||
| Income | –0.37 (0.18)* | 1.28 (0.64)* | 1.19 (0.61) |
| Skin reflectancea | 0.27 (0.18) | 0.37 (0.17)* | |
| Income × Skin Reflectancea | –0.07 (0.03)* | –0.07 (0.03)** | |
| Body mass indexb | 0.35 (0.06)** | ||
| Age | 0.47 (0.11)** | ||
| Gender | –3.57 (0.84)** | ||
| Blood pressure medication use | 9.32 (1.25)** | ||
| Current smoking | 0.67 (0.81) | ||
| R2 | 0.002* | 0.009** | 0.12** |
| Diastolic blood pressure | |||
| Income | –0.13 (0.14) | 0.42 (0.51) | 0.22 (0.50) |
| Skin reflectancea | 0.04 (0.14) | 0.10 (0.14) | |
| Income × Skin Reflectancea | –0.02 (0.02) | –0.02 (0.02) | |
| Body mass index | 0.22 (0.05)** | ||
| Age | 0.32 (0.09)** | ||
| Gender | –3.85 (.-0.68)** | ||
| Blood pressure medication use | 6.81 (1.01)** | ||
| Current smoking | –0.74 (0.66) | ||
| R2 | 0.0005 | 0.002 | 0.08** |
Note. In model 1, we tested the assumed underlying relationship between socioeconomic status and blood pressure (the socioeconomic status gradient). In model 2, we tested the main and interactive effects of skin color and income on blood pressure. In model 3, we added covariate data to adjust for the effects of age, gender, smoking status, blood pressure medication use, and body mass index.
aContinuous measure of skin reflectance.
bBody mass index is weight in kilograms divided by height in meters squared.
* P < .05; **P < .01.
When educational level was included as a potential confounder in model 3, the interaction between income and skin color was again virtually unchanged (b = −0.07; 95% confidence interval [CI] = −0.12, −0.01). Exclusion of individuals taking hypertension medication also did not significantly alter the effect of the interaction (b = −0.06; 95% CI = −0.12, −0.01). In addition, when the 3 outliers that were excluded from the analyses just described were included in the full model, the effect of the interaction remained statistically significant (b = −0.06; 95% CI = −0.11, −0.01). A test assessing whether there was a 3-way interaction with gender showed that the Income × Skin Color term was a stronger predictor of SPB among women (b = −0.08; 95% CI = −0.16, −0.01) than among men (b = −0.04; 95% CI = −0.12, 0.04); however, this gender difference was not statistically significant (b = 0.00; 95% CI = −0.02, 0.02).
To explore further the effect of the main interaction, we ran separate models for the dark and light skin color groups (Table 3 ▶). After adjusting for potential confounders, we found that income was a significant predictor of SBP levels in the light skin group, with each unit increase in income associated with more than a full point decrease in SBP. Across the range of lowest to highest incomes, there was a difference of more than 9 mm Hg in SBP among those with light skin (Figure 1 ▶). By contrast, income was positively, but not significantly, associated with SBP in the dark skin color group, with a difference of 0.8 mm Hg across the income range. Figure 1 ▶ also illustrates that, at the lowest income levels, individuals with light skin actually had the highest average predicted SBP levels.
TABLE 3—
Unstandardized Parameter Estimates From Separate Skin Color Tertile Linear Regression Models With Systolic Blood Pressure as the Dependent Variable: Coronary Artery Risk Development in Young Adults Study, 2000–2001
| Dark Skin Tertile | Light Skin Tertile | |
| Total, No. | 481 | 469 |
| Income, b (SE) | 0.10 (0.33) | –1.15 (0.32)** |
| Body mass index,a b (SE) | 0.26 (0.09)** | 0.36 (0.09)** |
| Age, b (SE) | 0.57 (0.19)** | 0.46 (0.17)** |
| Gender, b (SE) | –3.72 (1.46)* | –2.98 (1.43)* |
| Blood pressure medication use, b (SE) | 9.13 (2.08)** | 9.96 (2.28)** |
| Current smoking, b (SE) | 2.08 (1.45) | –0.08 (1.32) |
| R2 | 0.09** | 0.11** |
aBody mass index is weight in kilograms divided by height in meters squared.
* P < .05; **P < .01.
FIGURE 1—
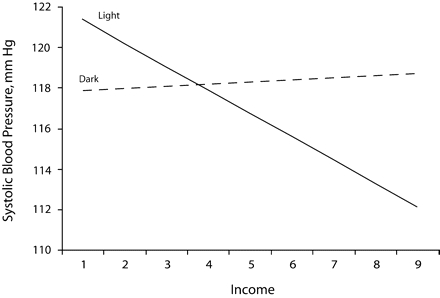
Relationship between income and systolic blood pressure among African Americans with dark and light skin: Coronary Artery Risk Development in Young Adults Study, 2000–2001.
Note. Blood pressure was adjusted for body mass index (i.e., weight in kilograms divided by height in meters squared), age, gender, use of antihypertensive medications, and smoking status. Self-reported annual family income was measured on a 9-point scale, with 1 = less than $5000, 5 = $25 000–$34 999, and 9 = $100 000 or more. The slope of the relationship was statistically significant among those with light skin but not among those with dark skin.
Diastolic Blood Pressure
Model 1 showed that the SES gradient for DBP was not pronounced in our sample (Table 2 ▶). The effect of income on DBP was in the expected negative direction but was not statistically significant (b = −0.13; 95% CI = −0.40, 0.15). Models 2 and 3 showed that the effect of the interaction between skin color and income on DBP was in the same direction as the effect for SBP, but it did not reach statistical significance alone or after we adjusted for potentially confounding effects. The inclusion of educational level as a confounding variable also did not change the effect of the skin color and income interaction substantially. In addition, as with SBP, no statistically significant gender interactions were found for DBP.
DISCUSSION
Our findings support the hypothesis that skin color moderates the effect of SES on SBP levels among African Americans. Among those with light skin, we observed the expected socioeconomic gradient with income, paralleling the well-documented pattern seen among White Americans.13 However, among those with darker skin, no effect of income on blood pressure was observed. These findings suggest that, with respect to blood pressure, the protective effects of economic success are not as prevalent among darker-skinned African Americans as they are among those with lighter skin. Our results also suggest that the association between skin color and blood pressure is not merely an artifact of SES, nor does skin color interact with SES in a simple additive fashion to influence blood pressure. Rather, we found that differences in skin color are associated with different patterns of socioeconomic relationships with blood pressure.
It is likely that chronic psychosocial stress was an important contributor to the income gradient in SBP observed among African Americans with lighter skin. Chronic stress is often cited as playing a key role in the socioeconomic gradient in health,9,22 with lower SES thought to be associated with a range of psychosocial stressors that may adversely affect mental and physical health. Recent meta-analyses suggest that psychosocial correlates of low SES, such as depression and perceived stress, convey risks for adverse cardiac events that are equal to or greater than other conventional coronary artery disease risk factors.39,40
Less intuitive is the absence of the SES gradient among African Americans with darker skin. The earlier findings of Klag et al.18 suggested that the combination of darker skin and lower SES could represent a double burden of psychosocial stressors contributing to higher blood pressure. However, our findings indicate that skin tone, and the social experiences that it indexes, interacts with SES in a way that is more complex than the case with additive effects.
In a 1978 editorial published in the Journal, Tyroler and James36 suggested that both within and without the African American community, skin color serves as a means through which individual status and worth are evaluated. They stated that skin color is “a primary determinant of whether an individual’s chances for full human development are to be circumscribed or maximized.”36(p1170) Similarly, Dressler,19 drawing on Weberian theories of social closure, suggested that darker skin color is an important characteristic “by which individuals are excluded from participation in higher status groups.”15(p65) Thus, skin color is a signifier of socially ascribed status and value that works in concert with, but also extends beyond, simple economic markers.
One mode through which skin color may serve as a marker for social exclusion is direct discrimination. It has been suggested that darker-skinned African Americans experience more racism than those with lighter skin.20,41 Darker-skinned individuals with higher incomes may have had to overcome more barriers to reach their economic position than those with lighter skin, and they may face more daily experiences of racism in a social class dominated by Whites. Indeed, the ethnographic work of Feagin and Sikes42 suggests that middle-class African Americans encounter widespread racism in their everyday lives and in their interactions with predominantly White institutions.
Moreover, African Americans who are economically successful are likely to encounter and challenge occupational and residential segregation on a regular basis,42,43 and African Americans with darker skin may be more likely to experience these challenges. Our results are consistent with those recently reported by Gravlee et al.24 among Puerto Rican adults; in that study, discrimination was also suggested to play a role in the higher blood pressure of individuals of darker socially ascribed “color” and higher SES.
Another concept useful in interpreting our findings is that of status inconsistency, according to which an individual’s social status is multidimensional and inconsistencies between status components can result in stress.44,45 Dressler19 found that inconsistencies between skin color (as a marker of social status) and material lifestyle resulted in higher blood pressure among a small sample of African Americans, particularly those with dark skin and high material status. Similarly, Gravlee and Dressler34 found that inconsistencies between self-perceived skin color and actual skin pigmentation were associated, in interaction with SES, with variations in blood pressure among adults in Puerto Rico. Our findings can be interpreted in a status incongruity framework, in that the highest SBP levels were seen among individuals in the 2 groups most inconsistent in terms of social position: the light skin–low income group and the dark skin–high income group.
Limitations
Our study involved several limitations. First, we did not explicitly investigate racial discrimination as a potential mediator of the observed relationships. Some studies have shown that self-reported experiences of discrimination are associated with physical and mental health status.46 However, in a previous study in which CARDIA data were used, Krieger et al.35 found the relationship between skin color and discrimination to be complex and mediated by gender, social class, and coping style. In a separate study, Krieger and Sidney47 reported that the relationship between self-reported discrimination and blood pressure among CARDIA participants was similarly complicated.
It has been suggested that racism experiences are difficult to measure because of reporting bias as well as the institutional, rather than interpersonal, nature of some forms of discrimination.48,49 Given these complexities, we did not examine self-reported discrimination as a potential mediator in our analyses. Future research should explore this aspect of the relationship, as well as other more subtle and insidious forms of racism and yet unmeasured or unidentified factors that may prevent African Americans with darker skin from realizing the health benefits of economic success.
A second limitation of our study is that the overall variance in blood pressure explained by our analyses was relatively low (DBP, 8%; SBP, 12%). This finding emphasizes the complex and multifactorial nature of blood pressure variation,50 of which our study investigated only a portion. Future research should incorporate additional covariates of blood pressure and cardiovascular risk. Finally, our results do not explain variation into clinically relevant, or hypertensive, blood pressure ranges. However, a meta-analysis of 61 prospective epidemiological studies showed that the relationship between blood pressure and morbidity and mortality risk is continuous across the entire blood pressure range, beginning as low as 115/75 mm Hg.51 Therefore, minor variation above a normal mean blood pressure level, such as that observed in this study, can be a highly significant indicator of increased health risk.
Conclusions
Within-race health differences often do not receive the same research attention as between-race differences.36 However, multiple axes of physical, economic, and social variation exist within socially constructed race groups. Determining how these multiple aspects of variation within racial or ethnic groups influence health outcomes such as blood pressure will eventually allow a better understanding of differences between groups. Assessments of these dimensions will also contribute to developing a social “epidemiology of everyday life”52(p352) that can enhance understanding of the social determinants of disease. Future research should continue to explore the proximate psychosocial mechanisms linking skin color and blood pressure, as well as the complex interactions among social factors affecting interracial and intra-racial health disparities.
Acknowledgments
The Coronary Artery Risk Development in Young Adults Study is supported by the National Heart, Lung, and Blood Institute (contracts N01-HC-48047, N01-HC-48048, N01-HC-48050, and N01-HC-95095).
Human Participant Protection All examinations were approved by the institutional review boards at the participating institutions, and informed consent was obtained from each study participant.
Peer Reviewed
Contributors E. Sweet completed the analyses and led the writing. T. W. McDade assisted with the analyses and writing. C. I. Kiefe and K. Liu helped to interpret findings and review drafts of the article.
References
- 1.Keppel KG, Pearcy JN, Wagener DK. Trends in racial and ethnic-specific rates for the health status indicators: United States, 1990–98. Stat Notes. 2002;23:1–16. [PubMed] [Google Scholar]
- 2.Kramer H, Conghan WP, Goff D, et al. Racial/ethnic differences in hypertension and hypertension treatment and control in the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Hypertens. 2004;17:963–970. [DOI] [PubMed] [Google Scholar]
- 3.Hayes DK, Greenlund KJ, Denny CH, Croft JB, Keenan NL. Racial/ethnic and socioeconomic disparities in multiple risk factors for heart disease and stroke—United States, 2003. MMWR Morb Mortal Wkly Rep. 2005;54:113–117. [PubMed] [Google Scholar]
- 4.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–1241. [DOI] [PubMed] [Google Scholar]
- 5.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States. JAMA. 2003;290:199–206. [DOI] [PubMed] [Google Scholar]
- 6.American Heart Association. African Americans and Cardiovascular Diseases—Statistics. Dallas, Tex: American Heart Association; 2004.
- 7.Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. N Engl J Med. 2002;347:1585–1592. [DOI] [PubMed] [Google Scholar]
- 8.Adler NE, Ostrove JM. Socioeconomic status and health: what we know and what we don’t. Ann N Y Acad Sci. 1999;896:3–15. [DOI] [PubMed] [Google Scholar]
- 9.Seeman TE, Crimmins E. Social environment effects on health and aging. Ann N Y Acad Sci. 2001; 954:88–117. [DOI] [PubMed] [Google Scholar]
- 10.Krieger N, Rowley DL, Herman AA, Avery B, Phillips MT. Racism, sexism, and social class: implications for studies of health, disease, and well-being. Am J Prev Med. 1993;9:82–122. [PubMed] [Google Scholar]
- 11.Williams DR. Race/ethnicity and socioeconomic status: measurement and methodological issues. Int J Health Serv. 1996;26:483–505. [DOI] [PubMed] [Google Scholar]
- 12.Williams DR. Race, socioeconomic status, and health: the added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896:173–188. [DOI] [PubMed] [Google Scholar]
- 13.Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60:191–204. [DOI] [PubMed] [Google Scholar]
- 14.Lewis TT, Everson-Rose SA, Sternfield B, Karavolos K, Wesley D, Powell LH. Race, education, and weight change in a biracial sample of women at midlife. Arch Intern Med. 2005;165:545–551. [DOI] [PubMed] [Google Scholar]
- 15.Dressler WW, Bindon JR. The health consequences of cultural consonance: cultural dimensions of lifestyle, social support, and arterial blood pressure in an African American community. Am Anthropologist. 2000;102:244–260. [Google Scholar]
- 16.Harburg E, Gleibermann L, Roeper P, Schork MA, Schull WJ. Skin color, ethnicity, and blood pressure I: Detroit Blacks. Am J Public Health. 1978;68:1177–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keil JE, Tyroler HA, Sandifer SH, Boyle E. Hypertension: effects of social class and racial admixture. Am J Public Health. 1977;67:634–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klag MJ, Whelton PK, Coresh J, Grim CE, Kuller LH. The association of skin color with blood pressure in US Blacks with low socioeconomic status. JAMA. 1991; 265:599–602. [PubMed] [Google Scholar]
- 19.Dressler WW. Social class, skin color, and arterial blood pressure in two societies. Ethn Dis. 1991;1:60–77. [PubMed] [Google Scholar]
- 20.Hall RE. The Euro-Americanization of race: alien perspective of African Americans vis-à-vis trivialization of skin color. J Black Stud. 2005;36:116–128. [Google Scholar]
- 21.Hall R. The bleaching syndrome: African Americans’ response to cultural domination vis-à-vis skin color. J Black Stud. 1995;26:172–184. [Google Scholar]
- 22.Siegrist J, Marmot M. Health inequalities and the psychosocial environment—two scientific challenges. Soc Sci Med. 2004;58:1463–1473. [DOI] [PubMed] [Google Scholar]
- 23.Dressler WW, Oths KS, Gravlee CC. Race and ethnicity in public health research: models to explain health disparities. Annu Rev Anthropol. 2005;34:231–252. [Google Scholar]
- 24.Gravlee CC, Dressler WW, Bernard R. Skin color, social classification, and blood pressure in southeastern Puerto Rico. Am J Public Health. 2005;95:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boyle E. Biological patterns in hypertension by race, sex, body weight, and skin color. JAMA. 1970; 213:1637–1643. [PubMed] [Google Scholar]
- 26.Parra FC, Amado RC, Lambertucci JR, Rocha J, Antunes CM, Pena SDJ. Color and genomic ancestry in Brazilians. Proc Natl Acad Sci. 2003;100:177–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parra EJ, Kittles RA, Shriver MD. Implications of correlations between skin color and genetic ancestry for biomedical research. Nat Genet. 2004;36(suppl 11): S54–S60. [DOI] [PubMed] [Google Scholar]
- 28.Cooper RS, Kaufman JS, Ward R. Race and genomics. N Engl J Med. 2003;348:1166–1170. [DOI] [PubMed] [Google Scholar]
- 29.Keil JE, Sutherland SE, Knapp RG, Tyroler HA, Pollitzer WS. Skin color and mortality. Am J Epidemiol. 1992;136:1295–1302. [DOI] [PubMed] [Google Scholar]
- 30.Murray RF. Skin color and blood pressure: genetics or environment? JAMA. 1991;265:639–640. [PubMed] [Google Scholar]
- 31.Hill M. Color differences in the socioeconomic status of African American men: results of a longitudinal study. Soc Forces. 2000;78:1437–1460. [Google Scholar]
- 32.Hughes M, Hertel BR. The significance of color remains: a study of the life chances, mate selection, and ethnic consciousness of Black Americans. Soc Forces. 1990;68:1105–1120. [Google Scholar]
- 33.Keith VM, Herring C. Skin tone and stratification in the Black community. Am J Sociol. 1991;97:760–778. [Google Scholar]
- 34.Gravlee CC, Dressler WW. Skin pigmentation, self-perceived color, and arterial blood pressure in Puerto Rico. Am J Hum Biol. 2005;17:195–206. [DOI] [PubMed] [Google Scholar]
- 35.Krieger N, Sidney S, Coakley E. Racial discrimination and skin color in the CARDIA Study: implications for public health research. Am J Public Health. 1998; 88:1308–1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tyroler HA, James SA. Blood pressure and skin color. Am J Public Health. 1978;68:1170–1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cutter GR, Burke GL, Dyer AR, et al. Cardiovascular risk factors in young adults: the CARDIA baseline monograph. Control Clin Trials. 1991;12:1S–77S. [DOI] [PubMed] [Google Scholar]
- 38.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116. [DOI] [PubMed] [Google Scholar]
- 39.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45:637–651. [DOI] [PubMed] [Google Scholar]
- 40.Yusuf S, Hawken S, Ounpuu S, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART Study): case-control study. Lancet. 2004;364:953–962. [DOI] [PubMed] [Google Scholar]
- 41.Klonoff EA, Landrine H. Is skin color a marker for racial discrimination? Explaining the skin color-hypertension relationship. J Behav Med. 2000;23:329–338. [DOI] [PubMed] [Google Scholar]
- 42.Feagin JR, Sikes MP. Living with Racism: The Black Middle-Class Experience. Boston, Mass: Beacon Press; 1994.
- 43.Steinberg S. Turning Back: The Retreat From Racial Justice in American Thought and Policy. Boston, Mass: Beacon Press; 1995.
- 44.Dressler WW. Social consistency and psychological distress. J Health Soc Behav. 1988;29:79–91. [PubMed] [Google Scholar]
- 45.McDade TW. Status incongruity in Samoan youth: a biocultural analysis of culture change, stress, and immune function. Med Anthropol Q. 2002;16:123–150. [DOI] [PubMed] [Google Scholar]
- 46.Jackson JS, Brown TN, Williams DR, Torres M, Sellers SL, Brown K. Racism and the physical and mental health status of African Americans: a thirteen year national panel study. Ethn Dis. 1996;6:132–147. [PubMed] [Google Scholar]
- 47.Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA Study of young Black and White adults. Am J Public Health. 1996;86:1370–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ruggiero KM, Mitchell JP, Krieger N, Marx DM, Lorenzo ML. Now you see it, now you don’t: explicit versus implicit measures of the personal/group discrimination discrepancy. Psychol Sci. 2000;11:511–514. [DOI] [PubMed] [Google Scholar]
- 49.Gee GC. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. Am J Public Health. 2002;92:615–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. JAMA. 2003;289:2560–2571. [DOI] [PubMed] [Google Scholar]
- 51.Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 52.Kaplan GA, Lynch JW. Is economic policy health policy? Am J Public Health. 2001;91:351–353. [DOI] [PMC free article] [PubMed] [Google Scholar]


