Abstract
Objectives. We examined the utility of the Veterans Health Administration (VHA) universal screening program for military sexual violence.
Methods. We analyzed VHA administrative data for 185 880 women and 4139888 men who were veteran outpatients and were treated in VHA health care settings nationwide during 2003.
Results. Screening was completed for 70% of patients. Positive screens were associated with greater odds of virtually all categories of mental health comorbidities, including posttraumatic stress disorder (adjusted odds ratio [AOR]=8.83; 99% confidence interval [CI] = 8.34, 9.35 for women; AOR = 3.00; 99% CI = 2.89, 3.12 for men). Associations with medical comorbidities (e.g., chronic pulmonary disease, liver disease, and for women, weight conditions) were also observed. Significant gender differences emerged.
Conclusions. The VHA policies regarding military sexual trauma represent a uniquely comprehensive health care response to sexual trauma. Results attest to the feasibility of universal screening, which yields clinically significant information with particular relevance to mental health and behavioral health treatment. Women’s health literature regarding sexual trauma will be particularly important to inform health care services for both male and female veterans.
The persistence of sexual violence within the US armed forces is a fact long recognized by military officials, policymakers, health care professionals, and the media. The risk of exposure to sexual violence within the military is high. The annual incidence of experiencing sexual assault is 3% among active duty women and 1% among active duty men. Sexual coercion (e.g., quid pro quo promises of job benefits or threats of job loss) and unwanted sexual attention (e.g., touching, fondling, or threatening attempts to initiate a sexual relationship) occur at an annual rate of 8% and 27%, respectively, among women and 1% and 5% among men.1 Research on deployment stress finds that such experiences constitute important duty-related hazards.2
The Veterans Health Administration (VHA) has adopted the term military sexual trauma (MST) to refer to severe or threatening forms of sexual harassment and sexual assault sustained in military service. In response to such widespread exposure in the military and the lasting deleterious consequences of sexual violence, the VHA has implemented a universal screening program for MST. For patients that screen positive, treatment for any MST-related injury, illness, or psychological condition is provided free of charge regardless of eligibility or co-pay status. These policies may represent the most comprehensive health policy response to sexual violence of any major US health care system. To our knowledge, we are the first to study the VHA’s MST program, which provides an unparalleled opportunity to investigate the feasibility and clinical utility of screening for sexual violence and provides unique data to characterize the burden of illness associated with MST.
US epidemiological data indicate significant deleterious health and mental health correlates for sexual trauma. Among traumatic events, rape holds the highest conditional risk for posttraumatic stress disorder (PTSD); these data and data specific to military samples confirm that sexual trauma poses a risk for developing PTSD as high as or higher than combat exposure.3–5 In addition to PTSD, civilian and veteran women exposed to sexual assault or sexual harassment exhibit a range of other mental health and medical conditions.6–15 These data have led to a greater awareness of sexual trauma issues among physicians and to the development of interventions and guidelines for the treatment and referral of sexual trauma in health care settings.16–18
These health sequelae may be magnified among veterans, because a number of issues uniquely associated with military settings may intensify the effect of this experience.19 Perpetrators are typically other military personnel, and victims often must continue to live and work with their assailants daily, which increases the risk for distress and for subsequent victimization. Unit cohesion may create environments where victims are strongly encouraged to keep silent about their experiences, have their reports ignored, or are blamed by others for the sexual assault, all of which have been linked to poorer outcomes among civilian assault survivors.20 Preliminary studies of MST among women veterans support this hypothesis and have found increased self-reports of depression, substance abuse, and gynecological, urological, neurological, gastrointestinal, pulmonary, and cardiovascular conditions.6,10
The VHA was first authorized to provide outreach and counseling for sexual assault to women veterans after a series of hearings on veteran women’s issues in 1992. Increased attention to these issues led Congress to extend services to male veterans shortly thereafter. In 1999, the VA’s responsibility was extended from counseling to “all appropriate [MST-related] care and services” and universal screening was initiated. Most recently, Public Law 108-422, signed in 2004, made the VA’s provision of sexual trauma services a permanent benefit. Screening programs and treatment benefits apply only to sexual trauma that occurred during military service. Each VA hospital now has a designated coordinator to oversee MST screening and treatment, and standardized training materials for MST screening are available to all VHA providers.21
Universal screening is accomplished through the use of a clinical reminder in the electronic medical record. An alert remains visible to all clinicians until screen results are entered. Documentation of a positive screen enables the provider to code the visit as MST related so that care is delivered free of charge. The extent to which these resources have encouraged providers to screen for MST has not been evaluated. Most research from civilian sectors suggest that only a minority of patients are screened for violence by their health care providers.22 However, VHA screening is integrated with standard clinical procedures, and training on the sensitive nature of MST screening is required at each VA hospital. Both of these factors are reliably associated with better screening compliance.22,23
The utility of screening policies to address this widespread veterans’ health issue is complicated because MST is not a syndrome, diagnosis, or construct associated with clear treatment indications. This stands in contrast to most other health care screening targets, such as cervical cancer or depression. Contrary to the American Medical Association’s recommendation for universal screening for violence against women,24,25 the US Preventive Services Task Force concluded that the evidence does not currently support this approach, citing a lack of intervention research and insufficient evidence that screening ultimately improves health status.26
Rebuttals to the Task Force conclusions emphasize the necessity of a broader view: violence against women is a risk or maintaining factor for a variety of health conditions and therefore a key treatment consideration for these patients.27 This perspective is especially relevant for addressing MST in the VHA health care system. Quantifying the types of health impairment associated with positive screens for MST is a first step toward evaluating the utility of universal screening. If screening detects clinically significant information, a positive screen would be an important factor in selecting appropriate treatment. Further evaluation of screening and treatment programs can then assess access to care according to the specific health outcomes found to be relevant to veteran men and women who have experienced sexual trauma.
MST has been primarily considered a women’s issue. Men comprise the majority of the armed forces, however, and the incidence of sexual harassment and assault reported by men during military service is significant. The approach to MST should therefore attend to both women and men and examine gender associated with MST as an initial step in the development of gender-specific interventions. Ours is the first examination of nationwide screening data for MST in the VHA and directly informs continued efforts to develop a gender-specific response to the health-related costs of military service and war. Specifically, we examined 3 issues: (1) whether universal screening detects a substantial population of VHA patients who report MST, (2) whether a greater burden of medical and mental illness is found among patients who screen positive for MST compared with patients who screen negative, and (3) whether the burden of illness associated with MST varies by patient gender.
METHODS
We used VHA administrative data in a cross-sectional analysis of a national sample of VHA outpatients. We selected the sample using the VHA Outpatient Events File28 to identify 4139888 veteran men and 185880 veteran women who—during fiscal year 2003—had at least 1 outpatient visit to a VHA health care facility that reported valid MST monitoring data.
The VHA uses a clinical reminder in the patient’s electronic medical record to screen for MST. The brief screening instrument contains the following items: “While you were in the military: (a) Did you receive uninvited and unwanted sexual attention, such as touching, cornering, pressure for sexual favors, or verbal remarks?; (b) Did someone ever use force or threat of force to have sexual contact with you against your will?” These items have been validated against clinical interview using psychometrically sound assessment instruments. Question “a” has a sensitivity of .92 and specificity of .89, and question “b” a sensitivity of .89 and a specificity of .90, which suggests that the screen is accurate.29 The performance of this instrument is comparable to other widely used VA mental health screens for depression30 and PTSD.31
MST is treated as a duty-related hazard similar to combat exposure, so discrete events are grouped as a single construct in much the same way that exposure to death and dying, being shot or hurt, severe supply shortage, and other experiences are grouped together under the rubric of combat exposure. This occupational exposure framework includes the context of the unwanted sexual activity as well as the events. The construct validity of this framework is supported by a recent analysis of the factors that make up the structure of deployment stress. The study found both sexual assault and sexual harassment loaded on a single sexual trauma or harassment factor that was distinct from the general harassment factor, as well as other deployment stressors such as combat.32 The VHA codes patients as positive for MST if they respond affirmatively to either screening item.
Diagnosed physical health conditions were quantified by grouping diagnoses (according to the International Classification of Diseases, Ninth Revision33) into non-overlapping categories; we used an empirically validated comorbidity measure designed for use with large administrative data sets.34 We quantified health conditions in a similar manner, using the Mental Health and Substance Abuse Clinical Classification Software,35 which maps closely to the Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition.36
All demographic variables were abstracted from VHA administrative records. VHA administrative data are known to have high proportions of individual records that are missing race values, although recorded values have a high rate of agreement with self-reports.37 To assess the effect of missing race data on our results, we repeated all analyses for medical and mental health comorbidities excluding individuals who had missing race values. Results did not significantly differ from those we describe herein.
After determining the percentage of veteran women and men who were VHA patients screened for MST, we used the χ2 test to compare categorical demographic variables by MST status, and logistic regression to model the odds of having a known medical or mental health condition as a function of MST status among men and women. We also calculated models while adjusting for the potentially confounding effects of age and race. Because our sample size was large, we calculated 99% confidence intervals for all odds ratios to correct for the high likelihood of finding statistically significant results.
RESULTS
Descriptive Statistics
A total of 137006 (73.7%) women and 2925 615 (70.7%) men were screened for MST. Screened patients were slightly older, more likely to be White, and used more VHA care in the past year compared with patients who were not screened (median visits for women were 8 vs 3; median visits for men were 6 vs 4; P< .001 for all comparisons).
We examined data for the 134894 women and 2 900 106 men who were screened for MST, exclusive of patients who declined to answer when screened (1.5% of women and 0.9% of men; Figure 1 ▶). Table 1 ▶ describes the demographic characteristics of patients grouped by MST screening results. Women who had positive MST screens were younger, more likely to be White, and more likely to have never been married than were women who had negative screens. Women who reported MST were also more likely to have a service-connected disability (i.e., a disability caused by an injury or illness incurred in or aggravated by military service). Men who had positive MST screens were also younger, more likely to be White, and more likely to be separated, divorced, or never have been married than were men who had negative screens. Men who reported MST were also more likely to have a service-connected disability.
FIGURE 1—
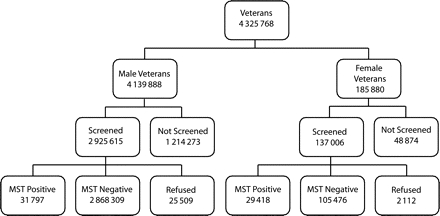
Flowchart of the military sexual trauma (MST) screening process among Veterans Health Administration outpatients: 2003.
TABLE 1—
Characteristics of Veterans Health Administration Outpatients, by Military Sexual Trauma (MST) Screen Results: October 1, 2002–September 30, 2003
| Women | Men | |||
| Positive MST Screen, No. (%)a | Negative MST Screen, No. (%)a | Positive MST Screen, No. (%)a | Negative MST Screen, No. (%)a | |
| Total no. | 29 418 | 105 476 | 31 797 | 2 868 309 |
| Age, y | ||||
| < 25 | 630 (2.1) | 3 034 (2.9) | 108 (0.3) | 8 332 (0.3) |
| 25–34 | 4 291 (14.6) | 14 375 (13.6) | 894 (2.8) | 57 294 (2.0) |
| 35–44 | 9 354 (31.8) | 22 163 (21.0) | 3 361 (10.6) | 146 876 (5.1) |
| 45–54 | 10 775 (36.6) | 25 792 (24.5) | 9 496 (29.9) | 483 379 (16.9) |
| 55–64 | 2 877 (9.8) | 12 183 (11.6) | 7 630 (24.0) | 639 034 (22.3) |
| ≥65 | 896 (3.0) | 9 337 (8.9) | 5 484 (17.2) | 783 948 (27.3) |
| Race/Ethnicity | ||||
| White | 14 431 (49.1) | 42 062 (39.9) | 16 640 (52.3) | 1 219 919 (42.5) |
| Black | 4 684 (15.9) | 14 040 (13.3) | 3 333 (10.5) | 239 564 (8.4) |
| Hispanic | 652 (2.2) | 1 559 (1.5) | 874 (2.7) | 55 957 (2.0) |
| Other | 229 (0.8) | 552 (0.5) | 243 (0.8) | 14 022 (0.5) |
| Unknown | 9 422 (32.0) | 47 263 (44.8) | 10 707 (33.7) | 1 338 847 (46.7) |
| Marital status | ||||
| Currently married | 9 356 (31.8) | 37 446 (35.5) | 15 825 (49.8) | 1 825 049 (63.6) |
| Separated/divorced/widowed | 11 559 (39.3) | 41 162 (39.0) | 9 741 (30.6) | 712 386 (24.8) |
| Never married | 8 120 (27.6) | 25 172 (23.9) | 5 936 (18.7) | 306 686 (10.7) |
| Unknown | 383 (1.3) | 1 696 (1.6) | 295 (0.9) | 24 188 (0.8) |
| Service-connected disability | ||||
| None | 12 211 (41.5) | 64 003 (60.7) | 19 324 (60.8) | 2 049 071 (71.4) |
| 0–50% | 9 412 (32.0) | 28 896 (27.4) | 6 735 (21.2) | 531 471 (18.5) |
| 51–100% | 7 795 (26.5) | 12 577 (11.9) | 5 738 (18.0) | 287 767 (10.0) |
Note: Having experienced MST and not having experienced MST are significantly different at P < .001 for women and men on all variables.
Mental Health Conditions
The unadjusted and age- and race-adjusted odds ratios for the association of a positive MST screen with diagnosed mental health conditions appear in Table 2 ▶. MST was significantly associated with 2 to 3 times greater odds of a mental health diagnosis, and this association was stronger among women than among men. Almost all specific mental health comorbidities were more common among patients who screened positive for MST. Although the profiles of men and women who reported MST were similar, some gender differences did emerge. PTSD had the strongest association with MST. The association of PTSD to MST was almost 3 times stronger among women than among men. The link between adjustment disorders and MST was significantly stronger among men than among women. Alcohol disorders and anxiety disorders were more common among both women and men who reported MST, but the relation to MST was significantly stronger among women than among men. The relation of MST to bipolar disorders and schizophrenia or psychoses was strong among men and women but significantly stronger among men. Our study found that several gender-linked mental health conditions typically reported in the literature as more common among women—including dissociative, eating, and depressive disorders—showed similarly robust associations with MST among women and men.
TABLE 2—
Age- and Race-Adjusted Odds of Mental Health Diagnoses as a Function of Screening Postive for Military Sexual Trauma (MST) Among Veterans Health Administration Outpatients: October 1, 2002–September 30, 2003
| Women | Men | |||
| OR (99% CI) | AOR (99% CI) | OR (99% CI) | AOR (99% CI) | |
| Any mental disorder | 3.63 (3.50, 3.76) | 2.91 (2.80, 3.02) | 3.12 (3.03, 3.21) | 2.44 (2.37, 2.52) |
| Adjustment disorders | 1.69 (1.56, 1.83) | 1.39 (1.28, 1.51) | 2.41 (2.24, 2.59) | 1.72 (1.60, 1.86) |
| Anxiety disorders | 2.20 (2.10, 2.32) | 1.84 (1.75, 1.93) | 2.45 (2.34, 2.56) | 1.95 (1.87, 2.04) |
| PTSD | 11.82 (11.18, 12.50) | 8.83 (8.34, 9.35) | 4.12 (3.97, 4.27) | 3.00 (2.89, 3.12) |
| Attention-deficit/conduct/disruptive | 2.63 (2.11, 3.28) | 1.87 (1.49, 2.34) | 4.07 (3.38, 4.89) | 2.56 (2.13, 3.08) |
| Delirium/dementia/amnestic | 0.61 (0.52, 0.71) | 1.11 (0.94, 1.31) | 1.04 (0.94, 1.14) | 1.26 (1.15, 1.39) |
| Disorders of infancy or childhood | 2.34 (1.25, 4.37) | 2.20 (1.13, 4.27) | 2.54 (1.58, 4.09) | 1.95 (1.21, 3.15) |
| Impulse-control disorders | 3.40 (2.39, 4.84) | . . . | 3.23 (2.64, 3.95) | 1.95 (1.59, 2.38) |
| Dissociative disorders | 7.47 (5.29, 10.54) | 4.97 (3.50, 7.07) | 5.81 (3.81, 8.84) | 3.61 (2.37, 5.51) |
| Eating disorders | 4.13 (3.30, 5.15) | 3.05 (2.43, 3.83) | 4.06 (2.43, 6.81) | 2.77 (1.65, 4.66) |
| Psychogenic disorders | 2.41 (1.52, 3.81) | . . . | 2.54 (1.56, 4.12) | 1.96 (1.20, 3.19) |
| Sexual disorders and dysfunction | 1.76 (1.34, 2.31) | 1.37 (1.03, 1.81) | 1.43 (1.33, 1.54) | 1.30 (1.21, 1.40) |
| Sleep disorders | 1.97 (1.54, 2.53) | 1.66 (1.28, 2.16) | 1.56 (1.24, 1.96) | 1.27 (1.01, 1.61) |
| Somatoform disorder | 2.48 (2.21, 2.77) | 1.86 (1.66, 2.09) | 2.80 (2.47, 3.18) | 1.83 (1.61, 2.08) |
| Bipolar disorders | 3.12 (2.92, 3.33) | 2.25 (2.10, 2.41) | 4.30 (4.06, 4.56) | 2.72 (2.56, 2.89) |
| Depressive disorders | 2.93 (2.83, 3.04) | 2.33 (2.24, 2.42) | 2.87 (2.78, 2.96) | 2.21 (2.14, 2.29) |
| Personality disorders | 4.60 (4.21, 5.01) | 3.11 (2.84, 3.40) | 5.77 (5.34, 6.24) | 3.42 (3.16, 3.70) |
| Schizophrenia and psychoses | 1.91 (1.77, 2.05) | 1.65 (1.52, 1.78) | 3.31 (3.15, 3.47) | 2.41 (2.30, 2.54) |
| Alcohol disorders | 3.28 (3.03, 3.55) | 2.33 (2.15, 2.53) | 2.67 (2.56, 2.79) | 1.75 (1.67, 1.84) |
| Drug abuse | 2.97 (2.73, 3.23) | 2.12 (1.94, 2.31) | 3.32 (3.16, 3.49) | 2.09 (1.98, 2.20) |
| Suicide and intentional self-inflicted injury | 2.96 (2.01, 4.37) | 2.15 (1.45, 3.21) | 5.34 (4.04, 7.05) | 2.93 (2.22, 3.88) |
Note. OR = odds ratio; CI = confidence interval; AOR = adjusted odds ratio; PTSD = posttraumatic stress disorder. An OR greater than 1 indicates that patients with MST were more likely to be diagnosed with that condition than were patients without MST. This difference is statistically significant at P < .01 if the 99% CI does not include 1.
Medical Conditions
The unadjusted and age- and race-adjusted odds ratios for the association of a positive MST screen with medical diagnoses are presented in Table 3 ▶. Several medical conditions were significantly associated with MST, although the magnitude and consistency of effect was smaller than for mental health conditions. For both women and men, liver disease and chronic pulmonary disease showed moderate associations with MST, and the magnitude of these relationships did not differ by gender. For women, obesity, weight loss, and hypothyroidism were significantly associated with MST. Among men, AIDS was significantly more common among men who reported MST.
TABLE 3—
Age- and Race-Adjusted Odds of Medical Diagnoses as a Function of Screening Postive for Military Sexual Trauma (MST) Among Veterans Health Administration Outpatients: October 1, 2002–September 30, 2003
| Women | Men | |||
| OR (99% CI) | AOR (99% CI) | OR (99% CI) | AOR (99% CI) | |
| Any medical disorders | 0.86 (0.83, 0.89) | 1.05 (1.02, 1.09) | 0.84 (0.82, 0.87) | 0.98 (0.95, 1.01) |
| Congestive heart failure | 0.40 (0.32, 0.51) | 0.88 (0.71, 1.10) | 0.76 (0.70, 0.83) | 0.95 (0.87, 1.03) |
| Valvular disease | 0.70 (0.60, 0.83) | 0.98 (0.83, 1.17) | 0.71 (0.63, 0.81) | 0.91 (0.80, 1.03) |
| Pulmonary circulation disease | 0.62 (0.36, 1.05) | 0.99 (0.56, 1.75) | 1.05 (0.73, 1.50) | 1.17 (0.82, 1.68) |
| Peripheral vascular disease | 0.47 (0.38, 0.57) | 0.99 (0.80, 1.23) | 0.70 (0.65, 0.76) | 0.89 (0.82, 0.97) |
| Hypertension | 0.69 (0.66, 0.72) | 0.97 (0.93, 1.02) | 0.82 (0.79, 0.84) | 0.93 (0.90, 0.96) |
| Paralysis | 0.88 (0.67, 1.14) | 0.83 (0.63, 1.10) | 1.12 (0.95, 1.32) | 1.01 (0.85, 1.19) |
| Other neurological disorders | 0.97 (0.86, 1.09) | 0.96 (0.85, 1.09) | 1.03 (0.94, 1.13) | 1.06 (0.96, 1.16) |
| Chronic pulmonary disease | 1.20 (1.13, 1.27) | 1.27 (1.19, 1.35) | 1.08 (1.03, 1.13) | 1.16 (1.11, 1.22) |
| Diabetes without chronic complications | 0.83 (0.77, 0.89) | 1.06 (0.98, 1.14) | 0.91 (0.87, 0.95) | 0.98 (0.94, 1.03) |
| Diabetes with chronic complications | 0.80 (0.68, 0.94) | 1.07 (0.90, 1.28) | 1.06 (0.98, 1.15) | 1.08 (1.00, 1.17) |
| Hypothyroidism | 0.82 (0.77, 0.88) | 1.11 (1.04, 1.19) | 0.90 (0.83, 0.97) | 1.08 (1.00, 1.17) |
| Renal failure | 0.48 (0.36, 0.64) | 0.72 (0.54, 0.98) | 0.73 (0.65, 0.82) | 0.87 (0.77, 0.97) |
| Liver disease | 1.66 (1.35, 2.03) | 1.30 (1.05, 1.60) | 1.90 (1.71, 2.11) | 1.26 (1.13, 1.40) |
| Peptic ulcer disease and bleeding | 0.67 (0.21, 2.12) | . . . | 1.07 (0.61, 1.88) | 1.12 (0.63, 1.97) |
| AIDS | 1.38 (0.88, 2.17) | . . . | 6.05 (5.24, 6.97) | 3.68 (3.19, 4.26) |
| Lymphoma | 0.54 (0.32, 0.90) | 0.71 (0.42, 1.21) | 0.83 (0.62, 1.11) | 0.92 (0.69, 1.24) |
| Metastatic cancer | 0.47 (0.27, 0.87) | 0.65 (0.36, 1.15) | 0.94 (0.70, 1.27) | 1.08 (0.80, 1.46) |
| Solid tumor without metastasis | 0.67 (0.59, 0.76) | 0.97 (0.85, 1.11) | 0.72 (0.67, 0.78) | 0.99 (0.92, 1.06) |
| Rheumatoid arthritis/collagen vascular disease | 0.87 (0.76, 1.00) | 0.96 (0.83, 1.10) | 0.93 (0.79, 1.08) | 0.99 (0.85, 1.16) |
| Coagulopathy | 0.79 (0.59, 1.05) | 1.00 (0.74, 1.35) | 0.81 (0.68, 0.97) | 0.88 (0.74, 1.05) |
| Obesity | 1.29 (1.23, 1.36) | 1.13 (1.07, 1.19) | 1.13 (1.08, 1.19) | 1.00 (0.95, 1.05) |
| Weight loss | 0.94 (0.76, 1.16) | 1.29 (1.03, 1.61) | 1.06 (0.90, 1.24) | 1.11 (0.95, 1.30) |
| Fluid and electrolyte disorders | 0.96 (0.82, 1.13) | 1.07 (0.90, 1.28) | 1.11 (0.97, 1.26) | 1.14 (1.00, 1.29) |
| Chronic blood loss anemia | 1.20 (0.62, 2.29) | . . . | 0.94 (0.40, 2.24) | 1.08 (0.46, 2.57) |
| Iron deficiency anemia | 0.86(0.78, 0.94) | 0.91 (0.83, 0.99) | 0.84 (0.77, 0.90) | 0.99 (0.92, 1.08) |
Note. OR = odds ratio; CI = confidence interval; AOR = adjusted odds ratio; PTSD = posttraumatic stress disorder. An OR greater than 1 indicates that patients with MST were more likely to be diagnosed with that condition than were patients without MST. This difference is statistically significant at P < .01 if the 99% CI does not include 1.
DISCUSSION
Our results suggest that universal screening for sexual trauma is feasible and yields valuable information to clinicians and administrators regarding health care for sexually traumatized women and men. The VHA universal screening program for MST screened over 70% of all patients, a rate commensurate with other screening-related performance measures collected by VHA in the same fiscal year: 80% for alcohol screening, 75% for tobacco counseling, and 90% for cervical cancer screening. Screening data indicate that MST is prevalent among veterans who seek VA health care, and as such, represents an important issue for VHA facilities. Approximately 22% of screened veteran women reported MST, which represents 29418 patients. Sexual trauma, including MST, is often viewed as primarily a women’s health issue and the proportion of positive screens among male patients is significantly lower than among women, only slightly over 1%. However, because the majority of VHA patients are men, this prevalence results in a detected clinical population of 31797 patients, comparable in size to the MST population of female patients. Given the size of the clinical population of veterans reporting these experiences, it is clear that medical knowledge relevant to providing care for victims of sexual harassment and assault is an important issue within VHA, for male as well as female patients.
Positive screens for MST were associated most strongly with mental health conditions. MST was associated with more than double the likelihood of receiving a mental health diagnosis and was statistically linked to a range of mental health conditions. In general, the relation of MST to mental health comorbidities was significantly stronger among women than among men. Among women, MST was most strongly related to PTSD, dissociative disorders, eating disorders, and personality disorders, diagnoses that are reliably observed among trauma-exposed individuals.34,38 Dissociative disorders and personality disorders were also among the conditions with the strongest link to MST for men. The link between MST and suicide and intentional self-harm (over twice as common among women and men who report MST) suggests the need for heightened awareness of and screening for suicide risk in this population.
Conditions such as dissociation, personality disorders, and self-harm comprise a constellation of symptoms associated with childhood trauma or other chronic, prolonged exposure to trauma.39–41 The robust association of these disorders with MST could suggest that the possibly prolonged nature of the exposure in the military social context may affect individuals in a manner similar to family violence. Exposure to early trauma, frequent among veterans,42 may also predispose patients to both revictimization by way of MST43 and greater risk for these mental health problems following revictimization.44 Extant research with women suggests MST frequently co-occurs with childhood or civilian sexual assault, but these events do not account for observed relations between MST and persistent traumatic stress. For example, approximately 30.3% of women sexually assaulted in the military also report sexual assault while a civilian, and 16.8% report childhood sexual abuse.43 The diagnosis of PTSD, however, is more common among women veterans with a military sexual trauma than among those who report other traumatic events or other sexual assaults. Furthermore, the effects of previous trauma or civilian sexual assault do not account for the strong relation observed between MST and PTSD.43,45 Additional research on the characteristics of MST exposures and their context in lifetime trauma, especially those that include samples of men, will help further clarify these issues.
VHA facilities are mandated to provide benefits for all aspects of MST-related care. Our data suggest that most of these services will be specialty mental health services. Mental health providers should be familiar with the clinical issues related to MST for both men and women.21 Given the strong associations between positive MST screens and trauma-related disorders (e.g., PTSD adjusted odds ratio [AOR] = 8.83 for women; AOR = 3.00 for men), treatment of PTSD secondary to sexual trauma will be especially important. For these and other conditions associated with MST, positive screens could increase access to care. The implementation of an MST treatment benefit would enable providers to offer tailored interventions that integrate MST into case conceptualizations and treatment plans. Evaluations of the clinical effect of universal screening should include measurement of the access to and benefit from mental health services for a variety of related conditions.
Behavioral factors can play an important role in the pathogenesis of most of the medical disorders that emerged as related to MST (e.g., liver disease, chronic lung disease, weight-related disorders, and HIV), further emphasizing the potential benefits of mental health services for MST-exposed veterans. Health behaviors that increase risks for these conditions, such as smoking, alcohol use, drug use, risky sexual behaviors, and unhealthy eating patterns, are more common among trauma-exposed patients than among nonexposed patients.46,47 Regardless of the path to the association, the demonstrated link between a positive screen for MST and a subset of the medical conditions provides further evidence of the extensive public health burden associated with sexual trauma in the military. Our findings highlight the importance of screening for a history of interpersonal violence, including MST, in behavioral health counseling and health care delivery.
Limitations
The data from our study should be interpreted with some caution. They are cross-sectional, and although we know that exposure to MST occurred during military service before VA health care, the temporal order of MST and the onset of potentially chronic comorbidities cannot be precisely discerned. These results only indicate that specific types of conditions are significantly overrepresented among women and men who report MST, and the results are clinically useful in caring for patients who experienced sexual trauma in the military. Comparison of screen results with the high rates of severe harassment and sexual assault documented among the armed forces1 and prevalence rates from other studies of MST10,14 suggests that the VHA’s current MST screening may underdetect such experiences. Therefore, these data may represent conservative estimates of the true prevalence of MST among veteran VHA patients. Inclusion of some patients with undetected MST in our “no MST” group would tend to dilute the strength of our findings. If so, the relation of MST to medical and mental health conditions may be more robust than observed in these data. As research into the VHA’s MST screening program continues and VHA becomes more expert at screening for these sensitive issues it will be possible to obtain more-accurate prevalence estimates of MST and associated clinical conditions among the women and men in VA health care.
Conclusions
Our study results are a first step in elucidating the significant burden of illness associated with MST. They can inform implementation of MST treatment benefits by the VHA and are relevant to VHA health care practice and policy. Sexually victimized patients are often reluctant to disclose to providers unless asked,48 and these data indicate that a relatively simple and time-efficient intervention can facilitate disclosure of this clinically relevant information. Mental health program planning can address the specific needs of MST-exposed patients and tailor programs to patient gender. Behavioral health interventions may be especially relevant to the medical needs of MST patients and may help reduce excess morbidity. The VHA is caring for increasing numbers of younger veterans, veteran women, and combat-exposed veterans as postdeployment troops return from Iraq and Afghanistan. These changing demographics suggest that MST will continue to be an important issue for VHA facilities and that universal screening programs are likely to continue to detect important clinical needs among the large population of MST-exposed patients.
The VHA response to MST is necessarily focused on screening, detection, and secondary prevention, because primary prevention of MST is outside the domain of VA health care. Growing awareness and knowledge of MST, coupled with reports about continued instances of MST in current military conflicts, has led to augmentation of primary prevention efforts within the military, so that the issue is not chiefly addressed within VHA treatment programs. In 2004, the Department of Defense launched the Sexual Assault Prevention and Response Office, a single point of accountability on sexual assault policy for the military. Similar coordinated prevention efforts by the military—to target the severe forms of sexual harassment included in the definition of MST—would help to address this important public health issue.
The VHA’s universal screening program and mandated MST-related treatment benefit represent unprecedented policies toward ameliorating the significant public health burden associated with experiences of sexual harassment and assault during military service. Even as military prevention programs continue to develop, our data indicate that the population of sexually traumatized men and women under the care of the VHA is alarmingly large and suffers from substantial morbidity. Continued outreach and education programs can help veterans understand the widespread nature of this problem and the resources available through VA. Education about MST is also relevant for providers in the private sector who may provide care to the growing numbers of returning veterans, most of whom do not use VA health care. The Department of Defense and the private sector must monitor education, outreach, and treatment programs of the VHA to gauge the success of efforts to prevent MST. Ongoing attention by scientists, policy-makers, and VHA and military leaders is required to address this important public health issue.
Acknowledgments
This work was supported by the Department of Veterans Affairs Epidemiology Research and Information Center and by Veterans Affairs Health Services Research and Development (grant IAE 05-291).
The authors thank Charles Maynard, PhD, for technical assistance and Barry Owen for his comments on drafts of this article.
Note. The funding sources had no role in study design, data collection, analysis, or interpretation, article preparation, or decision to publish the article.
Human Participation Protection This study was approved by the institutional review board of the Administrative Panel on Human Subjects in Medical Research, Stanford University.
Peer Reviewed
Contributors R. Kimerling conceptualized the study and wrote the article. K. Gima performed the data analysis. All authors collaborated on study conceptualization, interpreted the findings, and reviewed and edited drafts of the article.
References
- 1.Lipari RN, Lancaster AR. Armed Forces 2002 Sexual Harassment Survey. Arlington, Va: Defense Manpower Data Center; 2003.
- 2.Vogt DS, Pless AP, King LA, King DW. Deployment stressors, gender, and mental health outcomes among Gulf War I veterans. J Trauma Stress. 2005; 18(2):115–127. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psych. 1995;52: 1048–1060. [DOI] [PubMed] [Google Scholar]
- 4.Wolfe J, Sharkansky EJ, Read JP, Dawson R, Martin JA, Ouimette PC. Sexual harassment and assault as predictors of PTSD symptomatology among US female Persian Gulf War military personnel. J Interpers Viol. 1998;13(1):40–57. [Google Scholar]
- 5.Kang H, Dalager N, Mahan C, Ishii E. The role of sexual assault on the risk of PTSD among Gulf War veterans. Ann Epidemiol. 2005;15(3):191–195. [DOI] [PubMed] [Google Scholar]
- 6.Hankin CS, Skinner KM, Sullivan LM, Miller DR, Frayne S, Tripp TJ. Prevalence of depressive and alcohol abuse symptoms among women VA outpatients who report experiencing sexual assault while in the military. J Trauma Stress. 1999;12(4):601–612. [DOI] [PubMed] [Google Scholar]
- 7.Ouimette PC, Kimerling R, Shaw J, Moos RH. Physical and sexual abuse among women and men with substance use disorders. Alcohol Treat Q. 2000; 18:7–17. [Google Scholar]
- 8.Murdoch M, Nichol KL. Women veterans’ experiences with domestic violence and with sexual harassment while in the military. Arch Fam Med. May. 1995; 4(5):411–418. [DOI] [PubMed] [Google Scholar]
- 9.Ullman SE, Brecklin LR. Sexual assault history and suicidal behavior in a national sample of women. Suicide Life Threat Behav. 2002;32(2):117–130. [DOI] [PubMed] [Google Scholar]
- 10.Frayne SM, Skinner KM, Sullivan LM, et al. Medical profile of women Veterans Administration outpatients who report a history of sexual assault occurring while in the military. J Wom Health Gend Med. 1999; 8(6):835–845. [DOI] [PubMed] [Google Scholar]
- 11.Golding JM. Sexual assault history and limitations in physical functioning in two general population samples. Res Nurs Health. 1996;19:33–44. [DOI] [PubMed] [Google Scholar]
- 12.Golding JM. Sexual-assault history and long-term physical health problems: evidence from clinical and population epidemiology. Curr Dir Psychol Sci. 1999;8: 191–194. [Google Scholar]
- 13.Schneider KT, Swan S, Fitzgerald LF. Job-related and psychological effects of sexual harassment in the workplace: empirical evidence from two organizations. J Appl Psychol. 1997;82(3):401–415. [DOI] [PubMed] [Google Scholar]
- 14.Skinner KM, Kressin NM, Frayne SM, et al. Prevalence of military sexual assault among female Veteran Administration outpatients. J Interpers Viol. 2000;15: 291–310. [Google Scholar]
- 15.Magley VJ, Hulin CL, Fitzgerald LF, DeNardo M. Outcomes of self-labeling sexual harassment. J Appl Psychol. 1999;84(3):390–402. [DOI] [PubMed] [Google Scholar]
- 16.Rickert VI, Edwards S, Harrykissoon SD, Wiemann CM. Violence in the lives of young women: clinical care and management. Curr Wom Health Rep. 2001;1(2):94–101. [PubMed] [Google Scholar]
- 17.McGrath ME, Hogan JW, Peipert JF. A prevalence survey of abuse and screening for abuse in urgent care patients. Obstet Gynecol. 1998;91:511–514. [DOI] [PubMed] [Google Scholar]
- 18.Diaz A, Edwards S, Neal WP, et al. Obtaining a history of sexual victimization from adolescent females seeking routine health care. Mt Sinai J Med. 2004; 71(3):170–173. [PubMed] [Google Scholar]
- 19.Niebuhr R. Sexual harassment in the military. In: O’Donohue W, ed. Sexual Harassment: Theory, Research, and Treatment. Needham Heights, Mass: Allyn & Bacon; 1997;250–262.
- 20.Kilpatrick DG. Rape victims: detection, assessment and treatment. Clin Psychol. 1983;36(4):92–95. [Google Scholar]
- 21.Turner C, Frayne S, eds. Military Sexual Trauma. Washington, DC: Department of Veterans Affairs Employee Education System; 2004.
- 22.Waalen J, Goodwin MM, Spitz AM, Petersen R, Saltzman LE. Screening for intimate partner violence by health care providers barriers and interventions. Am J Prev Med. 2000;19(4):230–237. [DOI] [PubMed] [Google Scholar]
- 23.Wiist WH, McFarlane J. The effectiveness of an abuse assessment protocol in public health prenatal clinics. Am J Public Health. 1999;89:1217–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Council on Scientific Affairs, American Medical Association. Violence against women: relevance for medical practitioners. JAMA. 1992;267(23): 3184–3189. [PubMed] [Google Scholar]
- 25.Diagnosis and Management of Family Violence. Washington, DC: American Medical Association; June 2005.
- 26.Screening for family and intimate partner violence: recommendation statement. Ann Intern Med. 2004;140(5):382–386. [DOI] [PubMed] [Google Scholar]
- 27.Nicolaidis C. Screening for family and intimate partner violence. Ann Intern Med. 2004;141(1):81–82. [DOI] [PubMed] [Google Scholar]
- 28.VIReC. Research User Guide: FY2003 VHA Medical SAS outpatient datasets. Hines, Ill: VA Information Resource Center, Health Services Research and Development Service, Edward J Hines Jr. VA Hospital; 2003.
- 29.McIntyre LM, Butterfield MI, Nanda K, et al. Validation of a trauma questionnaire in veteran women. J Gen Int Med. 1999;14(3):186–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lowe B, Kroenke K, Grafe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res. 2005;58(2):163–171. [DOI] [PubMed] [Google Scholar]
- 31.Prins A, Ouimette PC, Kimerling R, et al. The primary care PTSD screen: development and operating characteristics. Prim Care Psychiat. 2004;9:9–14. [Google Scholar]
- 32.King DW, King LA, Vogt DS. Manual for the Deployment Risk and Resilience Inventory (DRRI): A Collection of Measures for Studying Deployment-Related Experiences of Military Veterans. Boston, Mass: National Center for PTSD; 2003.
- 33.International Classification of Diseases, Ninth Revision, Clinical Modification for Hospitals. Eden Prairie, Minn: Ingenix; 2006.
- 34.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. [DOI] [PubMed] [Google Scholar]
- 35.Billings J. Software for Use of the Emergency Department Classification Algorithm. Rockville, Md: Agency for Health Care Research and Quality; 2003. Publication 03-0027.
- 36.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington DC: American Psychiatric Association; 1994.
- 37.Kressin NR, Chang B-H, Hendricks A, Kazis LE. Agreement between administrative data and patients’ self-reports of race/ethnicity. Am J Public Health. 2003; 93(10):1734–1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bremner JD, Brett E. Trauma-related dissociative states and long-term psychopathology in posttraumatic stress disorder. J Trauma Stress. 1997;10(1):37–49. [DOI] [PubMed] [Google Scholar]
- 39.Battle CL, Shea MT, Johnson DM, et al. Childhood maltreatment associated with adult personality disorders: findings from the collaborative longitudinal personality disorders study. J Personal Disord. 2004;18: 193–211. [DOI] [PubMed] [Google Scholar]
- 40.Ford JD. Disorders of extreme stress following war-zone military trauma: associated features of post-traumatic stress disorder or comorbid but distinct syndromes? J Consult Clin Psychol. 1999;67(1):3–12. [DOI] [PubMed] [Google Scholar]
- 41.Sabo AN. Etiological significance of associations between childhood trauma and borderline personality disorder: Conceptual and clinical implications. J Personal Disord. 1997;11(1):50–70. [DOI] [PubMed] [Google Scholar]
- 42.Rosen LN, Martin L. The measurement of childhood trauma among male and female soldiers in the US Army. Mil Med. 1996;161(6):342–345. [PubMed] [Google Scholar]
- 43.Suris A, Lind L, Kashner TM, Borman PD, Petty F. Sexual assault in women veterans: an examination of PTSD risk, health care utilization, and cost of care. Psychosom Med. 2004;66(5):749–756. [DOI] [PubMed] [Google Scholar]
- 44.Arata CM. From child victim to adult victim: a model for predicting sexual revictimization. Child Maltreat. 2000;5:28–38. [DOI] [PubMed] [Google Scholar]
- 45.Yaeger D, Himmelfarb N, Cammack A, Mintz J. DSM-IV diagnosed posttraumatic stress disorder in women veterans with and without military sexual trauma. J Gen Intern Med. 2006;21(suppl 3):S65–S69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) study. Am Journal Prev Med. 1998;14:245–258. [DOI] [PubMed] [Google Scholar]
- 47.Buckley TC, Mozley SL, Bedard MA, Dewulf AC, Greif J. Preventive health behaviors, health-risk behaviors, physical morbidity, and health-related role functioning impairment in veterans with post-traumatic stress disorder. Mil Med. 2004;169(7):536–540. [DOI] [PubMed] [Google Scholar]
- 48.Friedman LS, Samet JH, Roberts MS, Hudlin M, Hans P. Inquiry about victimization experiences. A survey of patient preferences and physician practices. Arch Intern Med. 1992;152(6):1186–1190. [DOI] [PubMed] [Google Scholar]


