Abstract
Objectives. We examined hospital- and patient-related factors associated with discharge against medical advice (termed self-discharge) after emergency admission to acute-care hospitals.
Methods. We analyzed data from the Nationwide Inpatient Sample of the Healthcare Cost and Utilization Project using logistic regression models to assess the relationship between self-discharge and a set of patient and hospital characteristics.
Results. Of 3 039 050 discharges in the sample, 43 678 were against medical advice (1.44%). In multivariable modeling, predictors of self-discharge included having Medicaid insurance (adjusted odds ratio [AOR]=3.32; 95% confidence interval [CI]=3.22, 3.42), having Medicare insurance (AOR=1.64; 95% CI=1.59, 1.70), urban location (AOR=1.66; 95% CI=1.61, 1.72), medium (AOR=1.25; 95% CI=1.20, 1.29) or large (AOR=1.08, 95% CI=1.05, 1.12) hospital (defined by the number of beds), shorter hospital stay (OR=0.84; 95% CI=0.84, 0.85), and African American race (AOR=1.10; 95% CI=1.07, 1.14). Teaching hospitals had fewer self-discharges (AOR=0.90; 95% CI=0.88, 0.92). Other predictors of discharge against medical advice included age, gender, and income.
Conclusions. Approximately 1 in 70 hospital discharges in the United States are against medical advice. Both hospital and patient characteristics were associated with these decisions.
Discharges against medical advice, or self-discharges, have been documented in numerous settings of health care delivery.1–7 In previous studies of such discharges, the typical patient was described as someone who was poor and had some level of substance abuse,8,9 suggesting that patients who leave the medical care system against medical advice are either members of a disenfranchised group or patients suffering from some type of mental health condition.
Previous studies did not examine the hospital characteristics associated with the likelihood of self-discharge. Furthermore, previous studies that examined these discharges were either small,10 single-site settings,9 or focused on specific medical subpopulations such as patients with HIV and substance abuse.11 None of the published studies to date examined the effect of hospital characteristics, such as size, location, hospital type (teaching vs nonteaching), and so on, on the phenomenon of self-discharge. Therefore, we conducted a retrospective analysis of a large, random, representative national sample of hospital discharges to examine the demographic and clinical characteristics of patients who left the hospital against medical advice.
METHODS
Database and Study Sample
We used 2002 data from the federally funded Nationwide Inpatient Sample of the Healthcare Cost and Utilization Project operated by the Agency for Healthcare Research and Quality. In 2002, the survey collected complete discharge information from a 20% sample of nonfederal acute-care hospitals in the United States (995 hospitals with approximately 7.9 million hospitalizations). Short-term rehabilitation hospitals, long-term care institutions, psychiatric hospitals, and alcoholism and chemical dependency treatment facilities were excluded from the sample.
The survey data contained clinical and resource-use information included in a typical discharge abstract with safeguards to protect the privacy of individual patients, physicians, and hospitals.12 We studied the patient disposition for all emergency hospitalizations of patients aged 18 to 100 years that did not end in the death of the patient (n = 3 039 050).
Statistical Analysis
The primary outcomes of interest were the proportion and risk of discharges against medical advice. Logistic regression models were used for multivariable analyses of predictors of risk of discharge against medical advice. In these models, discharge against medical advice was the dependent variable of interest, and age, gender, and presence or absence of comorbid diagnoses were the independent variables. Because individual patient income was not available from the abstracted summaries, we used the median income of the patient’s zip code as a surrogate for income stratum. Insurance payments were classified as Medicare, Medicaid, private insurance (including Health Maintenance Organizations), self-pay, no charge (patients were not billed for their medical visit as of the date of collection of these data), and other types of insurance.
Data on race/ethnicity were not available from several states (Georgia, Illinois, Kentucky, Maine, Minnesota, Nebraska, Nevada, Ohio, Oregon, Washington, and West Virginia), so the category “unknown” was created. The primary reasons for hospitalization were classified into 15 broad groups derived from the International Classification of Diseases, Ninth Revision, Clinical Modification codes.13 For example, the category mental illness comprised all discharges with codes ranging from 290 to 319. Statistical analyses were performed using Stata version 9SE (StataCorp LP, College Station, Tex).
RESULTS
Baseline Characteristics of the Sample
Table 1 ▶ summarizes study sample baseline characteristics. Briefly, our sample included 3 039 050 discharges, of which 43 678 were self-discharges (1.44%). Self-discharged patients were more likely to be younger (P< .001), men (P<.001), non-White (P<.001), and in a lower income category (P < .001) than were patients with routine discharges. The mean length of stay was shorter for patients discharged against medical advice (2.9 days vs 5.1 days; P< .001) than for other patients.
TABLE 1—
Baseline Characteristics of the Study Sample (n=3039050): Nationwide Inpatient Sample of the Healthcare Cost and Utilization Project, 2002
| Patients Who Left Hospital Against Medical Advice | Patients Who Were Formally Discharged | P | |
| Total, No. | 43 678 | 2 995 372 | |
| Age, y, mean ± SD | 47 ± 16 | 61 ± 20 | <.001 |
| Male gender, % | 62.8 | 44.7 | <.001 |
| Median income of patient’s home zip code, % | <.001 | ||
| < $25 000 | 2.34 | 97.66 | |
| $25 000–$34 999 | 1.6 | 98.4 | |
| $35 000–$44 999 | 1.43 | 98.57 | |
| ≥ $45 000 | 1.2 | 98.8 | |
| Primary health insurance, % | <.001 | ||
| Private | 1.07 | 98.93 | |
| Medicaid | 3.42 | 96.58 | |
| Medicare | 0.75 | 99.25 | |
| No chargea | 3.12 | 96.88 | |
| Other | 1.98 | 98.02 | |
| Self-pay | 4.49 | 95.51 | |
| Race/ethnicity, % | <.001 | ||
| White | 1.28 | 98.72 | |
| African American | 2.35 | 97.65 | |
| Hispanic | 1.7 | 98.3 | |
| Other | 1.76 | 98.24 | |
| Unknown | 1.2 | 98.8 | |
| Hospital type | <.001 | ||
| Nonteaching | 1.37 | 98.63 | |
| Teaching | 1.53 | 98.47 | |
| Location, % | <.001 | ||
| Rural | 1.02 | 98.98 | |
| Urban, nonteaching hospital | 1.48 | 98.52 | |
| Urban, teaching hospital | 1.55 | 98.45 | |
| Hospital size,b % | <.001 | ||
| Small | 1.23 | 98.77 | |
| Medium | 1.7 | 98.3 | |
| Large | 1.37 | 98.63 | |
| Length of hospital stay, days, mean ± SD | 2.9 ± 5 | 5.1 ± 6 | <.001 |
| No. of diagnoses, mean ± SD | 5.4 ± 3 | 6.5 ± 3 | <.001 |
| No. of procedures, mean ± SD | 0.7 ± 1 | 1.3 ± 2 | <.001 |
| Total hospital charge, $, mean ± SD | 11 400 ± 18 739 | 18 740 ± 30 733 | <.001 |
aThese patients were not billed for their medical visit as of the date of collection of these data.
bCategorized by number of beds.
On average, patients discharged against medical advice had fewer procedures (0.7 vs 1.2; P< .001) and fewer diagnoses (5.4 vs 6.5; P< .001) and lower hospital charges than did those with routine discharges (P< .001). The largest primary diagnostic category associated with discharge against medical advice was mental health disorder (Figure 1 ▶). Patients with cancer and other neoplastic diseases were the least likely to be discharged against medical advice (P< .001).
FIGURE 1—
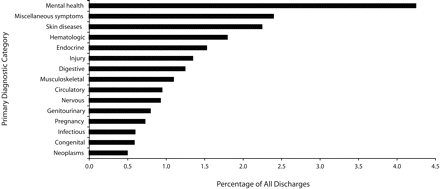
The proportion of hospitalized patients leaving acute-care hospitals against medical advice, by their primary diagnostic category: Nationwide Inpatient Sample of the Healthcare Cost and Utilization Project, 2002
Note. P < .001 for tests of heterogeneity.
Age- and Gender-Adjusted Analyses
After we adjusted for age, female gender was associated with 50% less risk of discharge against medical advice compared with men (odds ratio [OR] = 0.49; 95% confidence interval [CI] = 0.48, 0.50). Table 2 ▶ shows the age- and gender-adjusted risk analyses. Patients from higher-income neighborhoods were less likely to be discharged against medical advice, and those with no insurance (i.e., self-pay) or Medicaid insurance were approximately 3 times as likely as other patients to be discharged against medical advice.
TABLE 2—
Age- and Gender-Adjusted Correlates of Discharge Against Medical Advice in Acute-Care Hospitals (n = 2953364): Nationwide Inpatient Sample of the Healthcare Cost and Utilization Project, 2002
| OR (95% CI) | P | |
| Median income of patient’s home zip code, $ | ||
| < 25 000 (Ref) | 1 | |
| 25 000–34 999 | 0.74 (0.71, 0.77) | <.001 |
| 35 000–44 999 | 0.67 (0.64, 0.69) | <.001 |
| ≥ 45 000 | 0.58 (0.56, 0.60) | <.001 |
| Primary health insurance | ||
| Private (Ref) | 1 | |
| Medicaid | 2.99 (2.90, 3.07) | <.001 |
| Medicare | 1.46 (1.42, 1.51) | <.001 |
| No chargea | 2.35 (2.13, 2.58) | <.001 |
| Other | 1.57 (1.49, 1.65) | <.001 |
| Self-pay | 3.28 (3.18, 3.38) | <.001 |
| Race/ethnicity | ||
| White (Ref) | 1 | |
| African American | 1.35 (1.31, 1.38) | <.001 |
| Hispanic | 0.90 (0.86, 0.93) | <.001 |
| Other | 1.04 (0.99, 1.09) | <.001 |
| Unknown | 0.85 (0.83, 0.87) | <.001 |
| Hospital type | ||
| Nonteaching (Ref) | 1 | |
| Teaching | 0.96 (0.94, 0.97) | <.001 |
| Location | ||
| Rural (Ref) | 1 | |
| Urban | 1.41 (1.37, 1.46) | <.001 |
| Hospital sizeb | ||
| Small (Ref) | 1 | |
| Medium | 1.25 (1.21, 1.30) | <.001 |
| Large | 1.02 (0.99, 1.06) | .167 |
Note. OR = odds ratio; CI = confidence interval.
a These patients were not billed for their medical visit as of the date of collection of these data.
bCategorized by number of beds.
Among the racial/ethnic categories, compared with White patients, African American patients had a 35% higher risk of discharge against medical advice, and Hispanics had about a 10% lower risk. Urban hospitals, both teaching and nonteaching, had more self-discharges than did other hospitals. The risk was lower in the smallest and the largest hospital-size categories compared with medium-sized hospitals.
Multivariable Results
Results from multivariable modeling are summarized in Table 3 ▶. Older age, female gender, higher level of income, and non–African American racial/ethnic categories were associated with lower risk of self-discharge. Other predictors of discharge against medical advice included Medicaid insurance (adjusted OR [AOR] = 3.32; 95% CI = 3.22, 3.42) and Medicare insurance (AOR = 1.64; 95% CI = 1.59, 1.70). Urban hospitals (AOR = 1.66; 95% CI = 1.61, 1.72) and hospitals of medium (AOR = 1.25; 95% CI = 1.20, 1.29) or large (AOR = 1.08; 95% CI = 1.05, 1.12) size (categorized by number of beds) were associated with higher risk of self-discharge, but teaching hospitals (AOR = 0.90; 95% CI = 0.88, 0.92) had fewer discharges against medical advice than did nonteaching hospitals. Self-discharges were associated with shorter length of hospital stay (OR=0.84; 95% CI=0.84, 0.85). African American race was a positive predictor of discharge against medical advice (AOR=1.10; 95% CI=1.07, 1.14).
TABLE 3—
Results From Multivariable Modeling for Predictors of Discharge Against Medical Advice in Acute-Care Hospitals (n = 2 953 364): Nationwide Inpatient Sample of the Healthcare Cost and Utilization Project, 2002
| OR (95% CI) | P | |
| Each year of increasing age | 0.974 (0.974, 0.975) | <.001 |
| Women compared with men | 0.46 (0.45, 0.47) | <.001 |
| Median income of patient’s home zip code, $ | ||
| < 25 000 (Ref) | 1 | |
| 25 000–34 999 | 0.82 (0.79, 0.85) | <.001 |
| 35 000–44 999 | 0.73 (0.70, 0.76) | <.001 |
| ≥ 45 000 | 0.67 (0.64, 0.70) | <.001 |
| Primary health insurance | ||
| Private (Ref) | 1 | |
| Medicaid | 3.32 (3.22, 3.42) | <.001 |
| Medicare | 1.64 (1.59, 1.70) | <.001 |
| No chargea | 2.25 (2.03, 2.49) | <.001 |
| Other | 1.64 (1.56, 1.74) | <.001 |
| Self-pay | 3.28 (3.18, 3.38) | <.001 |
| Race/ethnicity | ||
| White (Ref) | 1 | |
| African American | 1.10 (1.07, 1.14) | <.001 |
| Hispanic | 0.66 (0.63, 0.68) | <.001 |
| Other | 0.90 (0.86, 0.95) | <.001 |
| Unknown | 0.85 (0.82, 0.87) | <.001 |
| Location | ||
| Rural (Ref) | 1 | |
| Urban | 1.66 (1.61, 1.72) | <.001 |
| Hospital type | ||
| Nonteaching (Ref) | 1 | |
| Teaching | 0.90 (0.88, 0.92) | <.001 |
| Hospital sizeb | ||
| Small (Ref) | 1 | |
| Medium | 1.25 (1.20, 1.29) | <.001 |
| Large | 1.08 (1.05, 1.12) | <.001 |
| Length of stay | 0.85 (0.84, 0.85) | <.001 |
Note. OR = odds ratio; CI = confidence interval.
a These patients were not billed for their medical visit as of the date of collection of these data.
bCategorized by number of beds.
In previous studies, patients with a mental health diagnosis were overrepresented in the cohorts of patients with discharges against medical advice. Therefore, we repeated the multivariable model, excluding patients with an admission diagnosis of a mental health disorder. This had a negligible effect on the ORs. The AOR for African American to White went from 1.10 to 1.16, suggesting that the African American patients’ increased risk of self-discharge might not be explained by a higher proportion of African American patients with a mental health diagnosis. In the race/ethnicity category “other,” the AOR also increased, from 0.90 to 0.96, and was no longer statistically significant, because the CIs crossed 1.0 (95% CI = 0.91, 1.01).
DISCUSSION
This was one of the largest studies ever to examine patient self-discharges. In this nationally representative study, we found that 1.44% of urgent hospitalizations ended in patients leaving against medical advice. Patients discharged against medical advice were, in general, younger in age, men, and of low socioeconomic status. More African Americans than members of other racial/ethnic groups were self-discharged. Self-discharged patients also had shorter stays and underwent fewer medical procedures than did patients with routine discharges. Medicaid insurance status was associated with higher risk of self-discharge even after adjusting for the effects of age, gender, race, income, length of stay, location, size, and teaching status of the hospital. Urban hospitals and hospitals of medium or large size were associated with higher risk, and teaching hospitals with lower risk of discharge against medical advice.
We found a relationship between hospital characteristics and the rate of discharges against medical advice. It is not clear why urban location and medium or large size were associated with higher risk and teaching status with lower risk of self-discharge. One possible explanation might be that these hospitals are more likely to have mental health services that attract more mental health patients than are smaller and more rural hospitals. However, this relationship persisted even after we excluded the diagnosis of mental health condition from the analysis. The negative association between teaching status of a hospital and lower risk of self-discharge was also unexpected. Because teaching hospitals are often highly specialized hospitals that provide tertiary care, perhaps their patients are less likely to leave against medical advice, fearing that they might not be able to get better care elsewhere. In-depth studies are needed to examine and explain the observed association between hospital characteristics and the patients’ risk of self-discharge.
The relationship between younger age and the propensity to leave the hospital against medical advice has been described before.9 Similarly, one previous study reported non-White racial/ethnic category to be associated with the risk of self-discharge.5 Franks and Fiscella analyzed a large database from California, Florida, and New York and found no relationship between race/ethnicity and self-discharge after adjusting for individual and hospital socioeconomic factors.14 They also reported that Hispanic patients and patients from other ethnic groups were less likely than were White patients to be discharged against medical advice. The reasons are not known. Patients from other ethnic minorities may be culturally more accepting of the health care system. Another hypothesis is that African American patients’ perceptions of disrespect and of receiving unfair treatment in the health care system may underlie their higher frequency of self-discharge.15
The overall rate of self-discharge we observed in this large sample is similar to the 0.8% to 2.2% reported in the United States by other studies.9,16–18 In a case–control study of 472 patients who were discharged against medical advice from the general medical wards and 1113 patients with routine hospital discharges, Weingart et al. reported male gender and Medicaid insurance status to be associated with discharge against medical advice.9 Our observations and those of others5,9,17 confirm these findings.
Reasons Patients Leave Against Medical Advice
Typically, patients are admitted to the hospital with their full voluntary consent. There is an unwritten, implicit contract between the patient and the physician that presumes that (1) the hospitalization is aimed at the betterment of the patient’s health, which is more important than the business the patient might need to attend to outside the hospital; (2) the patient will stay in the hospital as long as necessary but no longer; (3) only the physician has the knowledge and skills to decide when to discharge the patient; and (4) the patient’s preferences will be taken into account when making the decision of when to discharge. It might be that patients decide to leave against medical advice when they perceive that this contract is not honored. Reports suggest that in some instances hospital stays may last longer than necessary, regardless of the severity of the patient’s acute illness, and that these longer hospital stays are not always associated with worse or better patient outcomes.19–21 On some occasions, patients refuse to wait for the administrative delays in the discharge process. On other occasions, pressing domestic or social concerns may lead patients to leave the hospital before their physicians believe they are ready.
Patients may leave against medical advice because they disagree with their physician’s judgment of their health status (e.g., “I feel fine; therefore, I am well enough to leave the hospital”). A more serious cause of self-discharge arises when there is a conflict between the caregivers and the patient. Patients may come to the hospital already suspicious of the system and with previous bad experiences with providers. This could explain, in part, why some patients from racial/ethnic minorities and those from low-income communities who are socially marginalized are more at risk for leaving against medical advice. Patients with a history of substance abuse who have encountered previous experiences of inadequate treatment for their addiction or withdrawal are also at higher risk for self-discharge.17 These patients’ discharges may arise from the patients’ perception of the customer service, respect, and quality of care received. Major determinants of this perception are the cultural background of the patient and the health care team and hospital factors not available in our study.
Public Health Significance of Discharges Against Medical Advice
From a public health and social justice perspective, it is important to minimize, if not eliminate, discharges against medical advice. Understanding the characteristics of patients who leave the hospital against medical advice and gaining insight into their reasons are important because resource allocation, delivery of medical care, and quality of care are affected. Previous studies have shown that self-discharged patients are at high risk for re-admissions with resultant longer hospital stays and ultimately higher costs of care.8 These patients are also at high risk for poor follow-up care for unresolved medical issues.9,17
Higher rates of discharges against medical advice in general or in special populations (e.g., racial/ethnic minorities) may signify shortcomings of the system that need to be addressed to improve quality of care for all patients. Furthermore, racial differences in self-discharges could imply that health care delivery systems need to be more culturally sensitive toward the patients they serve.
Limitations
Our results should be interpreted with several limitations in mind. The database we used lacked information on the reasons patients were discharged against medical advice. Therefore, we were unable to distinguish discharges that reflected expressions of genuine patient preference from those that reflected patient reactions to mistreatment or inadequate treatment. For instance, patients who left one system or hospital to seek better treatment in another hospital could not be identified in our database.
We could not evaluate the short-term or the long-term consequences of self-discharges. Such information would have been helpful in interpreting the clinical relevance of the issue. We also did not assess severity of illness and its relationship with self-discharges, but a previous study showed no correlation between disease severity and such discharges.5
Conclusions
In a random national sample of more than 3 039 050 discharges from acute-care hospitals, we found that the rate of discharge against medical advice was 1.44% and that younger age, male gender, low socioeconomic status, and African American race were associated with such discharges. Prospective primary data collection studies are needed to better understand why patients leave the hospital against medical advice and the clinical implications of this decision.
Acknowledgments
This study was funded by the VA Health Services Research and Development Office, the Robert Wood Johnson Foundation, the National Institutes of Health (grant K12 HD049109).
The authors thank Kim Hansen for editorial input.
Note. The contents of this article are solely the responsibility of the authors and do not represent the official view of the National Institutes of Health.
Human Participant Protection No protocol approval was necessary for this study.
Peer Reviewed
Contributors S. A. Ibrahim and E. Krishnan originated the study and supervised all aspects of its implementation. S. A. Ibrahim drafted the article. C. K. Kwoh contributed ideas, interpreted findings, and reviewed drafts of the article. E. Krishnan conducted all the analyses.
References
- 1.Baile WF, Brinker JA, Wachpress JD, Engel BT. Signouts against medical advice. J Behav Med. 1979;2: 85–92. [DOI] [PubMed] [Google Scholar]
- 2.Jankowski CB, Drum DE. Diagnostic correlates of discharge against medical advice. Arch Gen Psychiatry. 1977;34:153–155. [DOI] [PubMed] [Google Scholar]
- 3.Jones AA, Himmelstein DU. Leaving a county hospital against medical advice. JAMA. 1979;242: 2758. [PubMed] [Google Scholar]
- 4.Long JP, Marin A. Profile of patients signing against medical advice. J Fam Pract. 1982;15: 551–556. [PubMed] [Google Scholar]
- 5.Saitz R, Ghali WA, Moskowitz MA. Characteristics of patients with pneumonia who are discharged from hospital against medical advice. Am J Med. 1999;107: 507–509. [DOI] [PubMed] [Google Scholar]
- 6.Dalrymple AJ, Fata M. Cross-validating factors associated with discharges against medical advice. Can J Psychiatry. 1993;38:285–289. [DOI] [PubMed] [Google Scholar]
- 7.Vander Stoep A, Bohn P, Melville E. A model for predicting discharge against medical advice from adolescent residential treatment. Hosp Community Psychiatry. 1991;42:725–728. [DOI] [PubMed] [Google Scholar]
- 8.Anis AH, Sun H, Guh DP, Palepu A, Schechter MT, O’Shaughnessy MV. Leaving hospital against medical advice among HIV-positive patients. CMAJ. 2002;167: 633–637. [PMC free article] [PubMed] [Google Scholar]
- 9.Weingart SN, Davis RB, Phillips RS. Patients discharged against medical advice from a general medicine service. J Gen Intern Med. 1998;13:568–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hwang SW, Li J, Gupta R, Chien V, Martin RE. What happens to patients who leave hospital against medical advice. CMAJ. 2003;168:417–420. [PMC free article] [PubMed] [Google Scholar]
- 11.Chan ACH, Palepu A, Guh DP, et al. HIV-positive injection drug users who leave the hospital against medical advice: the mitigating role of methadone and social support. Acquir Immune Defic Syndr. 2004;35: 56–59. [DOI] [PubMed] [Google Scholar]
- 12.Healthcare Cost and Utilization Project. Overview of the Nationwide Inpatient Sample. Available at: http://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed October 4, 2007.
- 13.International Classification of Diseases, Ninth Revision, Clinical Modification. Hyattsville, Md: National Center for Health Statistics; 1980. DHHS publication PHS 80-1260.
- 14.Franks P, Fiscella K. Effect of patient socioeconomic status on physician profiles for prevention, disease management, and diagnostic testing costs. Med Care. 2002;40:717–724. [DOI] [PubMed] [Google Scholar]
- 15.Blanchard J, Lurie N. R-E-S-P-E-C-T: patient reports of disrespect in the health care setting and its impact on care. J Fam Pract. 2004;53:721–730. [PubMed] [Google Scholar]
- 16.Smith DB, Telles JL. Discharges against medical advice at regional acute care hospitals. Am J Public Health. 1991;81:210–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jeremiah J, O’Sullivan P, Stein MD. Who leaves against medical advice? J Gen Intern Med. 1995;10: 403–405. [DOI] [PubMed] [Google Scholar]
- 18.Saitz R, Ghali WA, Moskowitz MA. The impact of leaving against medical advice on hospital resource utilization. J Gen Intern Med. 2000;15:103–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DeCoster C, Roos NP, Carriere KC, Peterson S. Inappropriate hospital use by patients receiving care for medical conditions: targeting utilization review. CMAJ. 1997;157:889–896. [PMC free article] [PubMed] [Google Scholar]
- 20.Kalant N, Berlinguet M, Diodati JG, Dragatakis L, Marcotte F. How valid are utilization review tools in assessing appropriate use of acute care beds? CMAJ. 2000;162:1809–1813. [PMC free article] [PubMed] [Google Scholar]
- 21.Flintoft VF, Williams JI, Williams RC, Basinski AS, Blackstien-Hirsch P, Naylor CD. The need for acute, subacute and nonacute care at 105 general hospital sites in Ontario. Joint Policy and Planning Committee Non-Acute Hospitalization Project Working Group. CMAJ. 1998;158:1289–1296. [PMC free article] [PubMed] [Google Scholar]


