Abstract
Objectives. Veterans Administration health care enrollment is restricted to veterans with service-connected problems and those who are poor. We sought to determine how many veterans were uninsured, trends in veterans’ coverage, and whether uninsured veterans lacked access to medical care.
Methods. We analyzed annual data from 2 federal surveys, the Current Population Survey for the years 1988 to 2005 and the National Health Interview Survey for 2002 to 2004.
Results. Nearly 1.8 million veterans were uninsured and not receiving Veterans Administration care in 2004. The proportion of working-age veterans lacking coverage peaked in 1993 at 14.2%, fell to 9.9% in 2000, and rose steadily to 12.7% in 2004. Uninsured veterans had substantial access problems; 51.4% had no usual source of care (vs 8.9% of insured veterans), and 26.5% reported failing to get needed care because of the cost (vs 4.3% of insured veterans).
Conclusions. Many US veterans are uninsured and lack adequate access to health care. Expanded funding for veterans’ care is urgently needed; only national health insurance could guarantee coverage to both veterans and their family members.
As clinicians at an urban public hospital, we often care for uninsured patients. Recently, we noted that several patients without coverage were combat veterans. We were surprised. We, and most colleagues with whom we conferred, assumed that all veterans qualify for care at Veterans Health Administration (VA) hospitals and clinics.
In fact, only a minority of veterans—those disabled by military service—are automatically eligible for VA care. The Veterans Eligibility Reform Act of 1996 opened VA enrollment to all veterans, although non-poor veterans were required to make co-payments of up to $50 per day for outpatient care. (Poor is defined by assets and an income threshold that varies with location and family size. In general, veterans earning more than $30 000 per year are not eligible for free care.) However, a July 18, 2002, memo from the deputy undersecretary for health for operations and management ordered VA regional directors to “ensure that no marketing activities to enroll new veterans occur,” citing “demand for healthcare that exceeds our resources” and “very conservative OMB [Office of Management and Budget] budget guidelines.”1 Subsequently, the secretary of veterans affairs ordered a halt to the enrollment of most nonpoor veterans as of January 17, 2003.2
We found scant data on uninsured veterans. Several studies identified the safety net function of VA care,3,4 looked at uninsured veterans in a single state,5 or offered limited data for a single year.6 An Internet posting by VA analysts offered some data on the number of uninsured veterans.7
Our encounters with uninsured veterans led us to explore 3 questions: are many veterans uninsured? Do uninsured veterans suffer problems in access to care similar to others who are uninsured? Is this a new problem?
METHODS
Data Sources
We analyzed data from 2 national surveys conducted annually by federal agencies. For data on insurance status and demographic characteristics, we analyzed the annual March Supplement (recently renamed the Annual Social and Economics Supplement) to the Current Population Survey (CPS), which collects current demographic information and data about health insurance in the previous calendar year. The CPS first collected comprehensive information on health coverage in 1988. Conducted by the Census Bureau in multiple languages, the survey includes a large sample (232 865 in 2005) representative of the US civilian noninstitutionalized population.
We considered persons to be uninsured if they reported neither public nor private insurance and denied that they had “CHAMPUS, veterans, or military health care.” (CHAMPUS [the Civilian Health and Medical Program of the Uniformed Services] is an insurance program for some active-duty and retired military personnel). To construct a time series from 1987, we analyzed veterans’ health coverage with the insurance definitions and population weights used by the Census Bureau.8
The CPS included no questions on access to care and only a single question on health status (“Would you say that your health in general is excellent, very good, good, fair, or poor?”). Therefore, we supplemented our CPS analyses with data from the 2002 to 2004 National Health Interview Surveys (NHIS).
The NHIS, conducted by the National Center for Health Statistics, interviewed 36 579 households in 2004, yielding demographic, health insurance, and some general health information on 94 460 persons. A more detailed set of health questions was asked of 31 326 adults. The 2002 and 2003 NHIS samples were of similar size. Because the NHIS samples were smaller than those of the CPS, we preferentially reported CPS results for variables that were available from both surveys.
The NHIS enumerates veterans only if they were honorably discharged from the military, thus identifying slightly fewer veterans than did the CPS. The CPS and NHIS define health insurance similarly, although the NHIS includes more detail on military and VA health care coverage. The CPS and NHIS provide weights that allowed for extrapolation of the surveys’ data to the entire US population.
Data Analysis
We performed most analyses with SAS version 8.1 (SAS Institute Inc, Cary, NC). For the NHIS data, we computed confidence intervals (CIs) and conducted a χ2 test using SUDAAN version 8.0.1 (Research Triangle Inst, Research Triangle Park, NC), which corrects for clustering caused by the complex sample design. It was not possible to compute precise CIs for the CPS, because the Census Bureau did not publicly release the clustering variables. In keeping with Census Bureau conventions, we reported univariate estimates without CIs but with the caveat that small differences should be interpreted cautiously.
We used multiple logistic regression on the 2005 CPS data to assess whether veteran status was protective against being uninsured in 2004 after we controlled for demographic covariates; we report CIs that were not adjusted for clustering. We doubt that these approximations introduced major errors. Generally, for large samples, adjustment for clustering widens the CIs only modestly. The odds ratios (ORs) that we report as statistically significant would remain so even if the CIs were increased 2 to 3 times.
For the multivariate model, we excluded persons younger than 18 years (none of whom were veterans) and persons older than 64 years (few of whom were uninsured, because of their eligibility for Medicare). We designated the probability of being uninsured as the dependent variable. Our a priori assumptions about policy-relevant predictors of health insurance coverage led us to include the following independent variables in the model: veteran status, family income below 200% of the federally defined poverty level, being older than 44 years, gender, having a job, educational attainment higher than high school graduation, and being a non-Hispanic White. We tested the model for interactions between veteran status and other independent variables; only male gender showed an interaction. Therefore, we also analyzed models stratified by veteran status. We repeated the logistic regression analysis on the 2001 CPS (for calendar year 2000, when the number of uninsured veterans was at its all-time low) to examine recent time trends.
RESULTS
Characteristics of Uninsured Veterans
In 2004, 1768377 US veterans had no health insurance and were not receiving ongoing VA care, representing 4.7% of all uninsured adults. Among all veterans, 7.7% were uninsured, including 12.7% of those older than 65 years. An additional 3.82 million members of veterans’ households were uninsured. Thus, 12.2% of uninsured Americans were veterans or members of their households.
Among the 7.56 million Vietnamera veterans, 645 628 (8.5%) lacked health insurance. Virtually all veterans of the Korean War and World War II eras were insured by Medicare, as was expected given their advanced age. Of the 8.60 million veterans of other eras (including the Gulf wars), 1 105 891 (12.9%) were uninsured.
Table 1 ▶ displays the demographic, military service, and employment characteristics of insured and uninsured veterans. Most veterans (insured as well as uninsured) were men and were older than 44 years. Uninsured veterans were poorer than those with coverage, and in univariate analysis, were much more likely to be in the labor force (i.e., holding jobs or looking for work).
TABLE 1—
Sample Demographic and Military Service Characteristics Among US Veterans, by Insurance Status 2004: Current Population Survey, Annual Social and Economic Supplement, March 2005, except data on foreign-born veterans and those who ever spent a night homeless or in jail, which came from analysis of the 2004 National Health Interview Survey
| Insured Veterans, % (n = 22.11 million) | Uninsured Veterans, % (n = 1.77 million) | |
| Women | 5.4 | 7.4 |
| Service era | ||
| World War II | 17.4 | 0.3 |
| Korean War | 14.3 | 0.7 |
| Vietnam War | 32.7 | 36.5 |
| Othera | 35.5 | 62.5 |
| Age, y | ||
| 18–44 | 16.3 | 44.5 |
| 45–64 | 40.7 | 55.2 |
| > 64 | 43.0 | 1.3 |
| Income, % of poverty level | ||
| < 150 | 11.4 | 29.9 |
| 150–249 | 17.5 | 23.4 |
| ≥250 | 71.1 | 46.7 |
| Employed | 48.8 | 64.3 |
| Unemployed or laid off | 1.9 | 8.7 |
| Foreign born | 3.6 | 4.9 |
| Ever spent a night homeless or in jail | 8.2 | 23.1 |
| In self-reported fair or poor health, by age, y | ||
| 18–24 | 5.6 | 3.7 |
| 25–44 | 7.7 | 7.9 |
| 45–64 | 18.8 | 19.1 |
| > 64 | 30.3 | NA |
Note. Because the Census Bureau does not publicly release information on the clustering variables, it was not possible to compute precise confidence intervals. Small differences should be interpreted cautiously.
aIncludes Gulf wars.
In a multivariate analysis of nonelderly adults in the 2005 CPS (Table 2 ▶), veterans were less likely to be uninsured than were nonveterans (OR = 0.621; 95% CI = 0.578, 0.664). Other predictors of coverage were higher income (above 199% of the federally defined poverty level), older age (age 44 and older), more education (greater than high school education), and being non-Hispanic and White. Although holding a job showed no relationship to insurance status after we controlled for multiple other factors, colinearity with income made this finding suspect. Men were significantly more likely to be uninsured (OR = 1.429; CI = 1.388, 1.471), although in the stratified analysis this was true only for nonveterans.
TABLE 2—
Multivariate Predictors of Being Uninsured Among Nonelderly Adults in 2004: Current Population Survey, Annual Social and Economic Supplement, March 2005.
| OR (95% CI) | |
| Being a veteran | 0.621 (0.578, 0.664) |
| Having income > 199% of poverty level | 0.349 (0.337, 0.361) |
| Having more than a high school education | 0.463 (0.446, 0.480) |
| Being non-Hispanic White | 0.508 (0.493, 0.523) |
| Being older than 44 y | 0.643 (0.620, 0.667) |
| Being male | 1.429 (1.388, 1.471) |
| Having a job | 0.976 (0.942, 1.010) |
Note. OR = odds ratio; CI = confidence interval.
Data from the 2004 NHIS, which included more detail on military and VA coverage than did the CPS, showed that 7.2% of honorably discharged veterans were uninsured. An additional 7.8% of veterans reported receiving VA care, nearly half of whom (3.3% of veterans, 738000 people) had no other coverage.
Barriers to Care for Uninsured Veterans
We used the NHIS data to explore access to care during the past year for uninsured veterans aged 18 to 64 years and compared their access to that of insured veterans and uninsured nonveterans in the same age group. Because analyses of the NHIS data for 2002, 2003, and 2004 yielded virtually identical findings, we reported only the 2004 results (Table 3 ▶).
TABLE 3—
Self-Reported Access to Care and Functional Limitations Within the Past Year Among Nonelderly and Nonveterans, by Insurance Status: United States, 2004 National Health Interview Survey
| Insured Veterans, % (95% CI) | Uninsured Veterans, % (95% CI) | Uninsured Nonveterans, % (95% CI) | |
| Needed but did not get care because of cost | 4.3** (3.5, 5.1) | 26.5 (22.1, 30.9) | 22.1 (21.1, 23.1) |
| Delayed care because of cost | 6.6** (5.7, 7.5) | 31.2 (26.7, 35.7) | 26.3* (25.3, 27.4) |
| Could not afford prescription | 5.5** (4.3, 6.7) | 25.1(19.3, 30.9) | 23.9 (22.7, 25.1) |
| Could not afford eyeglasses | 5.3** (4.2, 6.5) | 20.8(15.7, 25.9) | 17.5 (16.2, 18.8) |
| No office visit in past year | 15.5** (13.6, 17.4) | 49.1 (42.7, 55.4) | 45.5 (43.9, 47.1) |
| Did not get preventive care | 51.8** (44.6, 59.1) | 66.4 (58.1, 74.7) | 69.8 (67.5, 72.2) |
| No usual place to go when sick | 8.9** (7.3, 10.5) | 51.4 (44.6, 58.1) | 48.9 (47.1, 50.6) |
| No contact with any health professional | 14.9**(13.1, 16.7) | 44.9 (38.5, 51.3) | 42.3 (40.7, 43.9) |
| Any functional limitation | 36.7* (34.6, 38.9) | 30.7 (25.1, 36.3) | 24.4* (22.9, 25.9) |
Note. CI = confidence interval. Nonelderly was defined as a person between the ages of 18 and 64 years.
* P < .05, for difference relative to uninsured veterans; **P < .01, for difference relative to uninsured veterans.
Uninsured veterans fared no better than other uninsured Americans on most measures of access and had markedly worse access than did insured veterans. For instance, 26.5% of uninsured veterans reported needing but not getting care because of costs versus 22.1% of other uninsured Americans and only 4.3% of insured veterans. Nearly half (49.1%) of uninsured veterans had no office visit within the past year, compared with 45.5% of other uninsured Americans and only 15.5% of insured veterans. Preventive care use was low for all respondents. Approximately two thirds (66.4%) of uninsured veterans said they did not receive preventive care anywhere versus 69.8% of other uninsured Americans and 51.8% of insured veterans.
Veterans who reported VA care but no other coverage were similar to insured veterans in their utilization of care (data not shown), although they were sicker, poorer, and slightly more likely to report unmet medical needs than insured veterans.
Trends in Uninsured Rates
Table 4 ▶ and Figure 1 ▶ display the number of uninsured veterans each year since 1987. The number peaked in 1993, when 2.63 million veterans had no coverage and 14.2% of nonelderly veterans were uninsured. During the mid-and late 1990s, the proportion of veterans aged 18 to 64 years who lacked coverage declined, reaching a low of 9.9% in 2000. Since 2000, this proportion has risen again to 12.7%, the highest since 1997.
TABLE 4—
Numbers of Uninsured Elderly and Nonelderly Veterans and Nonveterans From 1987–2004: Current Population Survey, March Supplement (renamed Annual Social and Economics Supplement) for years 1988 through 2005
| Year | Uninsured Veterans, in millions, No. (%) | Living Veterans, in millions, No. | Uninsured Nonveterans, % | Uninsured Nonelderly Nonveterans, % | Uninsured Nonelderly Veterans, % |
| 1987 | 2.31 (8.5) | 27.08 | 13.4 | 15.8 | 10.7 |
| 1988 | 2.30 (8.6) | 29.93 | 14.0 | 16.7 | 11.0 |
| 1989 | 2.23 (8.3) | 26.75 | 14.2 | 16.9 | 10.8 |
| 1990 | 2.54 (9.5) | 26.75 | 14.5 | 17.5 | 12.8 |
| 1991 | 2.42 (9.1) | 26.68 | 14.7 | 18.0 | 12.5 |
| 1992 | 2.45 (9.3) | 26.24 | 15.3 | 19.1 | 12.9 |
| 1993 | 2.63 (10.1) | 26.13 | 15.9 | 19.3 | 14.2 |
| 1994 | 2.39 (9.2) | 26.13 | 15.8 | 19 | 13.2 |
| 1995 | 2.34 (9.2) | 25.47 | 16.0 | 19.5 | 13.7 |
| 1996 | 2.07 (8.3) | 25.14 | 16.4 | 19.6 | 12.3 |
| 1997 | 2.14 (8.5) | 25.13 | 16.9 | 20.3 | 12.8 |
| 1998 | 2.01 (8.3) | 24.34 | 17.1 | 20.4 | 12.4 |
| 1999 | 1.90 (7.9) | 24.99 | 16.3 | 19.7 | 12.1 |
| 2000 | 1.48 (6.3) | 23.63 | 14.7 | 18.3 | 9.9 |
| 2001 | 1.62 (6.8) | 23.70 | 15.3 | 19.2 | 10.8 |
| 2002 | 1.70 (7.3) | 23.35 | 16.0 | 20.2 | 11.6 |
| 2003 | 1.69 (7.4) | 23.07 | 16.3 | 20.9 | 11.9 |
| 2004 | 1.77 (7.7) | 22.88 | 16.4 | 21.1 | 12.7 |
Note. Nonelderly was defined as a person between the ages of 18 and 64 years; elderly was defined as a person 65 years or older. Because the Census Bureau did not publicly release information on the clustering variables, it was not possible to compute precise confidence intervals. Thus, small differences should be interpreted cautiously.
FIGURE 1—
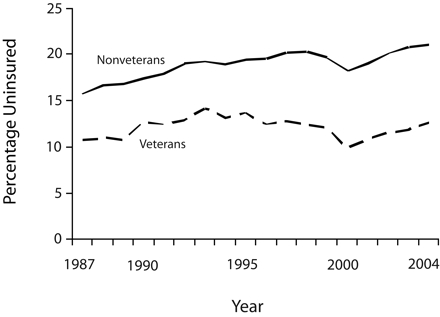
Percentage of veterans and nonveterans aged 18 to 64 years who lacked health coverage: 1987–2004.
Relative to other working-age adults (and in absolute terms), veterans’ coverage improved between 1993 and 2000. Before 1993 and after 2000, uninsured rates for the 2 groups moved in tandem, although veterans’ rates remained lower.
In logistic regression models derived from 2001 CPS data (for health insurance in 2000), veteran status was somewhat more protective against being uninsured (OR = 0.519; CI = 0.476, 0.562) than in 2004 when the OR was 0.621, confirming that veterans’ coverage advantage has declined in recent years.
DISCUSSION
Our analysis indicates that 1.8 million veterans are uninsured. Like the other 45 million uninsured persons in the United States, uninsured veterans forgo needed doctor visits, preventive care, medications, and other services.
The lack of health insurance among veterans, although long standing, appears to be worsening. Despite a shrinking population of working-age veterans, the number who were uninsured increased by nearly 300 000 between 2000 and 2004.
Several factors may have caused this increase. A ban on marketing VA services to new enrollees in 2002, followed by the narrowing of eligibility for VA care in early 2003, may be partially responsible. However, populationwide trends (e.g., the erosion of employment-based coverage since 2000)8 probably contributed. Conversely, the dip in the number of uninsured veterans during the late 1990s coincided with both an economic boom and an expansion of VA eligibility under the Veterans Eligibility Reform Act of 1996.
Several caveats apply to our findings. First, some veterans may have misunderstood questions in the CPS and failed to report that they were receiving VA health services. If so, our CPS-based analysis would overstate the number of uninsured veterans. However, the NHIS included much more detailed questions about military and veteran health care and yielded only slightly lower estimates of the number of uninsured veterans than those of the CPS. Even this slight discrepancy probably reflects the fact that only honorably discharged veterans were classified as veterans in the NHIS, whereas all veterans were included in the CPS definition. Because both surveys were household based, veterans who were homeless (approximately 200000),9 incarcerated (approximately 225000),9 or institutionalized at the time of the survey were excluded. Veterans whom we classified as uninsured reported as many problems in access to care as did other uninsured individuals, indicating that these veterans were functionally uninsured.
Small year-to-year changes in the number of uninsured veterans in the CPS should be interpreted cautiously because the Census Bureau’s data collection methods underwent several minor revisions. In the 1993 CPS and 2003 CPS (data years 1992 and 2002, respectively) the population weights were readjusted to reflect unanticipated population shifts discovered in the 1990 and 2000 censuses. Although these adjustments modestly affected the year-to-year changes, they should not have distorted longer-term trends or findings in the most recent years. In 1993, computer-assisted interviewing replaced pencil-and-paper methods. The Census Bureau shifted its definitions of health insurance slightly, including a redesign of the health insurance questionnaire in 1995 and the decision in 1998 to begin classifying individuals reporting only Indian Health Service coverage as uninsured. These definitional changes had opposite and negligible effects on estimates of the total number of uninsured persons.
Although the precise number of uninsured veterans and the exact magnitude of the recent upswing are uncertain, it is clear that many veterans are uninsured and that their numbers are increasing. This is particularly worrisome because the influx of casualties from current conflicts may further strain VA resources.
Addressing the problem of uninsured veterans by expanding VA eligibility is, in some respects, attractive. The VA appears to offer more-equitable care10 of equivalent11 or higher quality12–14 compared with that of private sector alternatives.
However, massive capital investments in new VA facilities would be needed to provide care for uninsured veterans, many of whom live far from existing VA facilities. Creating VA capacity throughout the nation would, in many cases, entail the unnecessary duplication of existing nonfederal hospitals and clinics. Moreover, even such a massive VA expansion would still leave millions of veterans’ family members uncovered.
The predicament of uninsured veterans is typical of the health care dilemma facing many working families. Like other uninsured adults, most uninsured veterans are low- to middle-income workers who may be too poor to afford private coverage but are not poor enough to qualify for Medicaid or free VA care. The VA provides a safety net for some of the mostly male veteran population and accounts for much of the advantage in insurance coverage that veterans enjoy compared with nonveterans. As with the safety net programs that predominantly enroll women and children (Medicaid and sCHIP [State Children’s Health Insurance Program]),15 however, many fall through the gaps.
The disturbing scene of returning soldiers left without care is a stark reminder that the United States is a nation bound by mutual obligations and shared responsibility. We owe veterans care not because they can pay for it nor because they are heroes but—as their sacrifices remind us—because members of a society are obligated to serve and protect each other.
Acknowledgments
This study was carried out on a volunteer basis without funding. None of the authors are employed by or receive funding from the Veterans Health Administration or the Department of Defense.
Human Participant Protection This study involved secondary analysis of public-use data, and no protocol approval was required.
Peer Reviewed
Contributors D. U. Himmelstein and S. Woolhandler originated the project, obtained data, performed the data analysis, and drafted the article. K.E. Lasser, D. McCormick, D.H. Bor, and J. W. Boyd helped to originate the project, review analyses, and revise the article.
References
- 1.Department of Veterans Affairs. Status of VHA enrollment and associated issues (memorandum). Available at: http://www.talkingpointsmemo.com/docs/veterans.affairs.1.html. Accessed September 11, 2006.
- 2.Walsh E. VA cuts some veterans’ access to health care: huge backlog, long waits prompt decision. Washington Post. January 17, 2003:A21.
- 3.Liu C-F, Maciejewski ML, Sales AEB. Changes in characteristics of veterans using the VHA health care system between 1996 and 1999. Health Res Policy Syst. 2005;3:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilson NH, Kizer KW. The VA health care system: an unrecognized national safety net. Health Aff (Millwood). 1997;16:200–204. [DOI] [PubMed] [Google Scholar]
- 5.Jonk YC, Call KT, Cutting AH, O’Connor H, Bansiya V, Harrison K. Health care coverage and access to care: the status of Minnesota’s veterans. Med Care. 2005;43:769–774. [DOI] [PubMed] [Google Scholar]
- 6.Woolhandler S, Himmelstein DU, Distajo R, et al. America’s neglected veterans. Intl J Health Serv. 2005; 35:313–323. [DOI] [PubMed] [Google Scholar]
- 7.Stockford D, Martindale M, Pane GE. Uninsured Veterans and the Veterans Health Administration Enrollment System 2003. Presented at: 12th Federal Forecasters Conference; April 18, 2002; Washington, DC. Available at: http://www1.va.gov/vhareorg/ffc/2002/Stockfordffc02.pdf. Accessed September 13, 2007.
- 8.US Bureau of the Census. Historical health insurance tables. Available at: http://www.census.gov/hhes/www/hlthins/historic/index.html. September 13, 2007.
- 9.National Coalition for Homeless Veterans. Background and statistics. Available at: http://www.nchv.org/background.cfm. Accessed February 12, 2007.
- 10.Jha AK, Shlipak MG, Hosmer W, Frances CD, Browner WS. Racial differences in mortality among men hospitalized in the Veterans Affairs health care system. JAMA. 2001;285:297–303. [DOI] [PubMed] [Google Scholar]
- 11.Petersen LA, Normand S-L T, Daley J, McNeil BJ. Outcome of myocardial infarction in Veterans Health Administration patients as compared to Medicare patients. N Engl J Med. 2000;343:1934–1941. [DOI] [PubMed] [Google Scholar]
- 12.Asch SM, McGlynn EA, Hogan MM, et al. Comparison of quality of care for patients in the Veterans Health Administration and patients in a national sample. Ann Int Med. 2004;141:938–945. [DOI] [PubMed] [Google Scholar]
- 13.Petersen LA, Normand S-LT, Leape LL, McNeil BJ. Comparison of use of medications after acute myocardial infarction in the Veterans Health Administration and Medicare. Circulation. 2001;104:2898. [DOI] [PubMed] [Google Scholar]
- 14.Kerr EA, Gerzoff RB, Krein SL, et al. Diabetes care quality in the Veterans Affairs health care system and commercial managed care: the TRIAD Study. Ann Intern Med. 2004;141:272. [DOI] [PubMed] [Google Scholar]
- 15.US Bureau of the Census. Historical health insurance tables. Available at: http://www.census.gov/hhes/www/hlthins/historic/hihistt2.html. Accessed February 12, 2007.


