Abstract
Background
Patient work resumption after sickness absence varies even among patients with similar pathologies and characteristics. Explanations remain uncertain. One newly investigated field is “information asymmetry”, a situation in which critical information is not appropriately exchanged between stakeholders in disability management. It is hypothesised that information asymmetry between social insurance physicians and occupational physicians prolongs sickness absence.
Objectives
To assess the influence of enhanced information exchange between these physicians on patient outcome.
Methods
Non‐randomised controlled intervention study. The setting was the work inability assessment consultation of social insurance physicians in Belgium. Inclusion criteria were: employee, age 18–50, and subacute (more than one month) sickness absence. The intervention was a structured information exchange (through the use of a communication form) between the patient's social insurance physician and occupational physician. The intervention started when the patient's sickness absence reached the subacute stage, and ended when the sickness absence benefit was ceased or the duration exceeded one year. The primary outcome measure was the sickness absence benefit status of the patient assessed one year after benefit onset.
Results
Of the 1883 patients asked to enrol in the study, 1564 (84%) participated; 505 (32%) of 1564 patients were assigned to the intervention group and 1059 (68%) to the control group; 1553 (99%) of 1564 patients completed the study. In the intervention group, 86% received no sickness absence benefit at the end of the study, versus 84% in the control group (95% CI 0.91–1.15). No significant differences in other outcome parameters were obtained.
Conclusions
Information exchange between physicians may not be enough to influence work resumption among patients on sickness absence. Further research on stakeholders' information asymmetry and its effect on the outcome of patients are necessary. The complexity of information asymmetry in disability management cannot be underestimated.
Keywords: sick leave, disability, physicians
Research efforts on the sickness absence and work resumption of patients are being increasingly published.1,2,3,4 For low back pain it has been shown that early resumption of socio‐professional activities may prevent prolonged sickness absence.5 Re‐activation should be initiated at an early stage, as the prognosis for work resumption declines with time. Despite the wide distribution of this new evidence, sickness absence has not diminished.6 This is a serious problem because the impact of sickness absence is not to be underestimated. Sickness absence is costly for the patient, the social security system, and employers.7 Furthermore, sickness absence is a major health problem as it is suspected of being associated with increased morbidity and mortality.8 More research on why some patients do and others do not return to work is urgently needed.9
Our study investigates a well defined and relatively new domain in sickness absence: stakeholders' information asymmetry, a situation in which critical information is not or not appropriately exchanged between all stakeholders involved in disability management.10,11,12,13,14,15,16 The study focuses on information asymmetry between physicians.
In Belgium, the attending physician, the social insurance physician, and the occupational physician all play key roles in disability management. The attending physician is responsible for diagnosis and treatment, and completing sickness absence certification. Most general practitioners are self‐employed, work single handed, and receive a fee for service. After a short period of full wage payment by the employer (two or four weeks), employees on sick leave claim a benefit from the National Sickness and Invalidity Insurance. The Christian Sickness Fund is the social insurance company of the sickness insurance for 55% of the population in Flanders. The social insurance physician of the sickness funds evaluates the patient's inability to work by means of regular medical examinations. He has the authority to end the benefit if the patient no longer complies with the legal criteria. To enhance return to work, the social insurance physician can authorise gradual work resumption. Gradual work resumption permissions are successful but rare. This underuse is probably due to the limited information that social insurance physicians have about the possibilities of changing the patient's work hours at the workplace. The occupational physician is responsible for all health related aspects of work and has structured contacts both with employees and with the employer. He has mainly a preventive role including the prevention of work related pathologies and sickness absence. For this purpose, he regularly examines the employees (or patients) at work. He has little or no contact with patients on sickness absence, mainly due to an explicit prohibition to assess justification of sickness absence. Patients returning to work after a sickness period exceeding four weeks come in the first week of work resumption on a return to work consultation. At that time, the occupational physician evaluates if the patient can return to work. Contrary to the social insurance physician, the occupational physician also takes account of the content of the patient's job. To prevent the onset of sickness absence, he is able to organise work modifications; this has been shown to be an effective tool in preventing prolonged sickness absence duration.17 However, to operationalise work modifications for patients on sickness absence, the occupational physician lacks timely information on the sickness absence period. The occupational physician is employed by a company directly or—more often—indirectly through an external occupational health service providing services to affiliated companies. The major external occupational health service is IDEWE, which provides preventive services to 33% of the companies in Flanders.
Because of their legal roles the social insurance physician and the occupational physician possess complementary information with regard to reintegration possibilities for workers on sick leave. In theory, communication could increase reintegration possibilities, but in practice such communication seldom occurs. However, improvement of communication is an essential feature of many new interventions to improve disability outcomes.18 The limited communication practices result in a lack of information, which is especially necessary for gradual or modified work resumption.
Our study aimed to test the link between information availability among physicians and the sickness absence outcome of patients. Within the project, social insurance physicians and occupational physicians communicated in a structured way to enhance their information availability. The most innovative part of this study is that the social insurance physician informed and involved the occupational physician in disability management during sickness absence—a period in which occupational physicians generally have little or no contact with the patient. The occupational physician was therefore able to propose workplace actions to improve work resumption possibilities. The course of the patients' sickness absence could be adjusted as it evolved rather than retrospectively criticised. While this paper focuses on disability management by intervening in the information exchange between social insurance physicians and occupational physicians, it is important to realise that many of the principles are generic and applicable in addressing communication, information exchange, and cooperation among all involved stakeholders. Therefore, this report is also relevant to worker compensation or benefit systems that differ from the Belgian system. The paper contributes to closing the gap in stakeholders' information asymmetry and its association with sickness absence and work resumption.
This report describes and discusses the results of an intervention trial wherein the effect of enhanced information exchange between Belgian social insurance physicians and occupational physicians on work resumption outcome parameters of patients on sickness absence was evaluated.
Methods
Our study was designed to test the null hypothesis that work resumption of patients on sickness absence is not associated with enhancing information exchange between social insurance physicians and occupational physicians.
In the trial's preparation phase, 15 social insurance physicians of the Christian Sickness Fund, and all 40 occupational physicians of the external occupational health services IDEWE in three regions in the North of Belgium agreed to cooperate regarding the disability management of patients on sickness absence. For these 55 physicians, regular local meetings were organised with the following objectives: (1) to encourage professional contacts between social insurance physicians and occupational physicians; (2) to optimise their mutual perception; (3) to exchange experiences and problems related to sickness absence of patients; and (4) to clarify their roles and possibilities for increasing the work resumption of patients. Patients described as having difficulties in returning to their previous workplace were discussed. Finally, during the meetings, physicians were motivated to exchange information more frequently and in a better way. A standardised communication form to enhance their communication and information exchange efforts was presented and accepted. It was agreed to implement the communication form in a prospective trial for patients on sickness absence. The trial had a single blind, non‐randomised, regionally, controlled interventional design. The study protocol was accepted by the Ethical Committee “Commissie voor Medische Ethiek OG nr. 117, Heverlee, Belgium”.
The selection and recruitment of patients in the trial took place from 1 October 2001 to 1 July 2002. The study observation period ended on 1 July 2003.
The study population consisted of those patients who were under work inability surveillance by one of the 15 social insurance physicians from the Christian Sickness Fund. Inclusion criteria were: (1) age 18–50 years; (2) employee; and (3) subacute (1–12 months) sickness absence, because patients beyond the acute stage of sickness absence have poor work resumption prognosis. To meet the latter criterion, the patient's enrolment was scheduled in parallel with the social insurance physician's second work inability assessment consultation (usually after 1–4 months' sickness absence). The only exclusion criterion was pregnancy related sickness absence because return to work is unlikely before childbirth followed by maternity leave.
Box 1: Content of questionnaire to obtain data on confounding variables for all participating patients
Demographic and socio‐economic variables: age; gender; marital status; social support; presence of close relatives on sickness absence or disability benefit; education level; financially dependent persons; current and previous financial problems; supplementary financial compensation, e.g. by private insurance; intention to involve an attorney
Health related variables: smoking, drinking, and exercise habits; length and weight to calculate body mass index; current pregnancy; mental wellbeing (General Health Questionnaire);19 pain (Chronic Pain Questionnaire)20
Work related variables: employment status; blue collar or white collar; work schema; experience in the profession and with the employer; trade union member and representative; job characteristics (Job Content Questionnaire)21
Sickness absence related variables: pathology leading to sickness absence; work relatedness of the pathology; attitude towards not being able to work; prognosis regarding work resumption; attitude towards gradual or modified return to work; attitude towards the social insurance physician and the occupational physician
A trained and blinded research interviewer enrolled the patients. He double checked all inclusions and exclusions, performed the (written) informed consent procedure, and registered reasons for non‐participation. After the social insurance physician ended the second work inability assessment consultation, the research interviewer provided the physician with a list of enrolled patients.
The intervention in our study was the use of a communication form between the social insurance physician and the occupational physician. For participating patients, the social insurance physician completed the communication form. He noted on the form the diagnosis of the patient, the presumed relationship between pathology and work conditions, the relevant information received from the attending physician, the estimated sickness absence duration, and the desirability of an active involvement of the occupational physician. At this point, the social insurance physician was not aware of group allocation as described below.
All communication forms were sent to the occupational health services IDEWE. There, an administrator performed the allocation of participating patients to intervention and control groups. Allocation was based on the occupational health service of the company where the patient was employed. When the company was affiliated to IDEWE, the patient was assigned to the intervention group. When the company employed directly an occupational physician or was affiliated to an external occupational health services other than IDEWE, the patient was assigned to the control group.
For intervention group patients, the communication form was delivered to the occupational physician of IDEWE. He completed the information and described possible workplace actions (e.g. ergonomic advice; the solution of harassment problems or workplace conflicts; the possibility of temporary provision of work modifications or gradual work resumption) if the social insurance physician requested his active involvement. He returned the form to the social insurance physician. At the next (mostly often monthly) work inability assessment consultation, the social insurance physician updated the information and returned the form to the occupational physician. The communication form also included contact data of both physicians, making information exchange by telephone possible. We encouraged both physician groups to register all exchanged information on the communication form. This circular and individual information exchange procedure was repeated until one of the following events: sickness absence benefit was ceased; sickness absence benefit duration exceeded one year; or drop‐out occurred for other reasons (e.g. the patient transferred to another sickness fund; the patient died; the patient retired; the patient became unemployed; the company where the patient was employed changed to another occupational health services provider).
For control group patients, the communication form was delivered to the researcher and no circular individual information exchange procedure was initiated although it could occur. Patients did not receive a copy of completed communication forms.
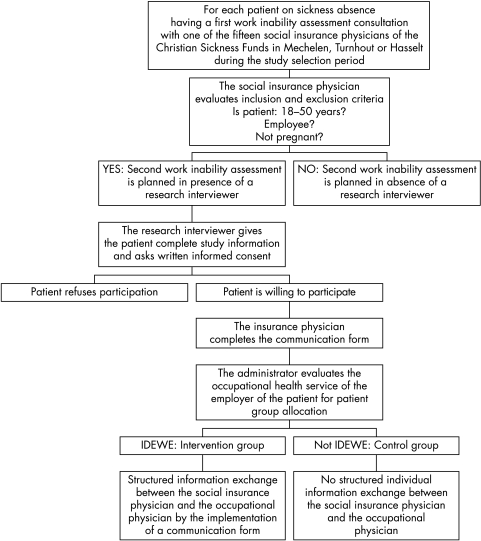
A flow chart showing the progress of participating patients through the trial is presented in fig 1. During the entire trial, social insurance physicians and occupational physicians continued participating in the regular local meetings, at which application of the communication form was encouraged.
Figure 1 The progress of participating patients through the trial.
The final evaluation was scheduled for one year after the onset of the sickness absence benefit of the participating patient. Eight outcome parameters were obtained from the sickness fund. The primary outcome parameter was the sickness absence benefit status of the patient. The benefit status was scored categorically (sickness absence benefit dependent versus sickness absence benefit non‐dependent). The score resulted in a rate of non‐dependence on benefit. Further, seven secondary outcome parameters were assessed. For individuals non‐dependent on benefit, actual work status was provided to calculate work resumption rate. For all individuals, the number of sickness absence benefit periods during the study period was counted. Cumulative sickness absence benefit duration was calculated for all individuals: for benefit periods exceeding the study year, the end of the benefit period was adjusted to the final assessment moment (censored values). The percentage reduction of those on sickness absence benefit was plotted as the cumulative benefit duration of the patients receiving benefit. The number of patients using a gradual work resumption permission granted by social insurance physicians was registered, resulting in a gradual work resumption rate. The duration of gradual work resumption and the duration of sickness absence benefit prior to gradual work resumption were calculated.
Data on confounding variables for outcome parameters originated from: (1) information from the social insurance physician on the communication form regarding the pathology of the patient (answers to the open question were categorised by the researcher into three pathology classes: orthopaedic, psychologic/psychiatric, or other) and the presence of a presumed relationship between the pathology and the work conditions (yes/no); and (2) information from the patient provided on an anonymous survey conducted at enrolment to the study. The survey included 56 questions on 31 items. Three questions on age, employment status, and current pregnancy, to retest for the main inclusion and exclusion criteria, were spread through the survey. Wherever possible, Dutch translated versions of English standardised instruments with demonstrated measurement properties were used (box 1). Outcome results were corrected for these confounding variables.
Sample size was calculated prior to the start of the study and indicated a need for at least 370 subjects in the intervention and the control groups, respectively. The calculation was based on a minimum important difference in the primary outcome parameter. We considered a decrease of the rate of benefit dependence with 40% (from 18.0% to 10.8%) socially relevant (α = 0.05 two‐side; β = 0.20 one‐side; p1 = 0.180; Δ = 0.072; p2 = 0.108; n = 370). To protect the minimum target sample, we chose to use a broad time period of selection and recruitment (from October 2001 to July 2002) rather than by closing the trial when each cohort reached the minimum number of patients. A pilot study indicated that a nine month time period of selection and recruitment was sufficient to include 500 subjects in the intervention and the control groups, respectively.
Analyses were performed using SPSS. For all analyses, p < 0.05 was considered statistically significant. In a first step of the analysis, the intervention and the control groups were compared for their outcome parameters using the t test, χ2 or Fisher's exact test, and Mann‐Whitney U test. Curves of the percentage reduction of those on sickness absence benefit were obtained by survival analysis (Kaplan Meier) and compared using the log rank test. In a second step, the study groups were compared for all confounding variables, applying the above mentioned descriptive analysis techniques. In a third step, a (binary logistic) regression model was made to control the primary outcome parameter (sickness absence benefit status) for those confounding variables that showed significant difference between the two study groups in step two. In a fourth step, a regression model was made to control the primary outcome parameter for each potential confounding variable. In a fifth step, regression models to study interactions were made. For the primary outcome parameter, three variables were entered in the model: a confounding variable; the study group; and the interaction “confounding variable × study group”. This step was done for all confounding variables. In a sixth step, for significant interactions, analyses were performed in the subgroups of the confounding variable (stratified analyses). In a seventh step, a regression model was made to control significant stratified results for confounding variables which showed significant difference between the study groups in step two.
Results
A total of 1883 patients were asked to participate. Data on 16 (0.8%) of 1883 patients were excluded from analysis because they did not meet inclusion and exclusion criteria. Data on 1867 (99.2%) of 1883 patients were analysed.
A total of 303 (16%; inter‐region range: 14–18%) of 1867 patients refused to participate, mainly due to doubts about the employer's or occupational physician's positive impact on return to work management or lack of interest in research.
A total of 1564 (84%) of 1867 patients participated. Twenty per cent (n = 317) had a sickness absence benefit duration of 1–2 months at enrolment to the study; duration was 2–4 months in 73% (n = 1139), and 4–12 months in 7% (n = 108). Mean benefit duration at study enrolment, age, and gender distribution were not significantly different from non‐participants.
Of the 1564 patients, 505 (32%) were assigned to the intervention group, 1059 (68%) to the control group. Characteristics of participating patients are summarised in table 1.
Table 1 Main characteristics of the participating patients and a comparison of the characteristics of patients assigned to the intervention group and the control group.
| Characteristic | Total participants | Intervention group | Control group |
|---|---|---|---|
| n = 1564 | n = 505 | n = 1059 | |
| Age in years: mean±SD (median) (range) | 38±7.7 (39) (18–50) | 39±7.2 (40) (19–50) | 38±7.9 (39) (19–50) |
| Age class in % (n = 1564, n = 505, n = 1059): 18–24 y/25–34 y/35–45 y/>45 y | 6/24/45/25 | 4/21/49/27* | 7/25/44/24 |
| Gender in % (n = 1564, n = 505,n = 1059): male/female | 50/50 | 41/59* | 54/46 |
| Marital status in % (n = 1454, n = 483, n = 971): married or co‐habit/single | 77/23 | 79/21 | 76/24 |
| Social support from friends or relatives in difficult times in % (n = 1429, n = 472, n = 957): yes/no | 92/8 | 92/8 | 92/8 |
| Close relative on sickness absence or disability benefit in % (n = 1440, n = 480, n = 960): yes/no | 23/77 | 23/77 | 23/77 |
| Highest education level in % (n = 1445, n = 480, n = 965): elementary/3 y secondary/secondary/advanced | 15/24/47/14 | 16/23/47/14 | 15/25/47/13 |
| Financially dependent persons in % (n = 1450, n = 479, n = 971): yes/no | 51/49 | 51/49 | 51/49 |
| Financial problems since the onset of sickness absence benefit dependence in % (n = 1449, n = 480, n = 969): yes/no | 15/85 | 15/85 | 15/85 |
| Financial problems prior to sickness absence benefit dependence in % (n = 1472, n = 473, n = 954): yes/no | 3/97 | 3/97 | 3/97 |
| Supplementary financial compensation in % (n = 1442, n = 472, n = 970): yes/no | 11/89 | 10/90 | 11/89 |
| Intention to involve an attorney in % (n = 1446, n = 480, n = 966): yes/no/maybe | 2/90/8 | 2/90/8 | 2/89/9 |
| Smoking habits in % (n = 1453, n = 482, n = 971): smoker/non‐smoker | 41/59 | 35/65* | 45/55 |
| Drinking habits in % (n = 1411, n = 472, n = 939): weekly number of consumptions: <3/3–9/>9 | 65/21/14 | 66/21/13 | 64/22/14 |
| Exercise habits in % (n = 1362, n = 455, n = 907): weekly sport activity of at least 30 minutes: <1/1–2/>2 | 46/35/19 | 45/35/20 | 47/35/18 |
| Body mass index in % (n = 1424, n = 470, n = 954): <20/20–24/25–29/30–39/>39 | 9/46/32/12/1 | 9/46/31/13/1 | 8/47/33/12/1 |
| Work status in % (n = 1455, n = 483, n = 972): blue collar/white collar | 71/29 | 70/30 | 72/28 |
| Work schema in % (n = 1456, n = 481, n = 975): full time/part time | 73/27 | 64/36* | 78/22 |
| Experience in the current profession in % (n = 1446, n = 479, n = 967): <1 y/1–5 y/>5 y | 8/22/70 | 6/20/73* | 9/23/68 |
| Experience at the current employer in % (n = 1449, n = 482, n = 971): <1 y;1–5 y/>5 y | 10/27/63 | 7/24/70* | 12/29/59 |
| Trade union member in % (n = 1450, n = 482, n = 968): yes/no | 79/21 | 77/23 | 80/20 |
| Trade union representative in % (n = 1096, n = 353, n = 743): no/yes | 19/81 | 17/83 | 20/80 |
| Pathology leading to sickness absence evaluated by patient in % (n = 1432, n = 474, n = 958): orthopaedic/psychological–psychiatric/other | 61/20/19 | 58/21/20 | 64/18/18 |
| Pathology leading to sickness absence evaluated by social insurance physician in % (n = 1554, n = 504, n = 1050): orthopaedic/psychological–psychiatric/other | 62/19/19 | 60/20/20 | 63/19/18 |
| The presence of a relationship between the pathology and the work conditions assessed by the patient in % (n = 1432, n = 474, n = 958): absolutely not/a little/a lot/completely | 36/30/15/19 | 34/33/16/17 | 38/28/14/20 |
| The presence of a relationship between the pathology and the work conditions assessed by the social insurance physician in % (n = 1554, n = 504, n = 1050): no/yes | 76/24 | 77/23 | 76/24 |
| Regret not being able to work in % (n = 1422, n = 472, n = 950): a lot/quite a lot/not that much/not at all | 48/45/6/1 | 44/50/6/1* | 51/42/6/1 |
| Prognosis regarding work resumption assessed by the patient in % (n = 1366, n = 456, n = 910): within 1 month/within 1–3 months/not in the following 3 months/never | 49/31/11/9 | 47/31/13/10 | 50/30/11/9 |
*p<0.05 for comparison intervention group with control group.
Of the 1564 patients, 1553 (99%) completed the study. Eleven (1%) patients (three in intervention group and eight in control group) dropped out the study: 6 (0.4%) transferred to another sickness fund, 3 (0.2%) died, and 2 (0.1%) retired during the trial. The drop‐out rate among physicians was zero.
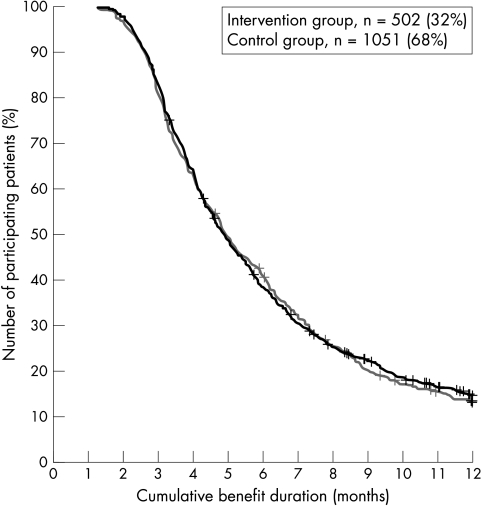
The primary outcome results in group comparison, without correction for confounding variables, revealed no statistically significant difference: in the intervention group, 86% received no sickness absence benefit at the end of the study, versus 84% in the control group. No significant differences in the other seven outcome parameters were obtained. The results are summarised in tables 2 and 3, and fig 2.
Table 2 Outcome results of parameters expressed as rates.
| Parameter | Intervention group | Control group | Group comparison | |
|---|---|---|---|---|
| n = 502 | n = 1051 | p value | RR (95% CI) | |
| Rate of non‐dependence on benefit in % (n) | 85.7 (432) | 84.0 (888) | 0.41 | 1.02 (0.91–1.15) |
| Work resumption rate in % (n) | 89.6 (372) | 87.4 (728) | 0.27 | 1.03 (0.93–1.13) |
| Only one benefit period rate in % (n) | 85.3 (431) | 84.5 (895) | 0.68 | 1.01 (0.90–1.14) |
| Gradual work resumption rate in % (n) | 10.3 (52) | 8.3 (88) | 0.22 | 1.24 (0.52–2.97) |
For all rates, the denominator was the total number of patients completing the study and assigned to the intervention group (n = 502) or to the control group (n = 1051).
Table 3 Outcome results of parameters expressed as durations.
| Parameter | Intervention group | Control group | Group comparison | |
|---|---|---|---|---|
| n = 502 | n = 1051 | p value | Mean difference (95% CI) | |
| Median of cumulative benefit duration in days (mean±SD) (range) | 151 (182±97.7) (40–365) | 150 (182±98.1) (41–365) | 0.89 | 1.02 (0.89–1.16) |
| Median of gradual work resumption duration in days (mean±SD) (range) | 62 (82±73.5) (0–309) | 62 (87±78.4) (0–341) | 0.98 | 1.02 (0.56–1.87) |
| Median of pre‐gradual work resumption benefit duration in days (mean±SD) (range) | 106 (143±91.4) (4–365) | 120 (138±85.6) (21–365) | 0.94 | 1.05 (0.54–2.05) |
Figure 2 Group comparison curves of the percentage reduction of those on sickness absence benefits. The curves reflect the velocity by which individuals ended the sickness absence benefit. Comparison of the curves for intervention group and control group revealed nearly identical curves (p = 0.72, hazard ratio (exp β) = 1.02, 95% CI 0.87–1.09).
Comparison of rates of outcome parameters in the intervention group and control group, without correction for imbalance in data on confounding variables, revealed no statistically significant differences.
Comparison of mean duration of outcome parameters in the intervention group and control group, without correction for imbalance in confounding variables, revealed no statistically significant differences.
Comparison of data on confounding variables showed that the intervention group had a higher proportion of: patients aged 45–50 years (p = 0.01); females (p < 0.01); part‐time workers (p < 0.01); workers with longer experience at the current employer (p < 0.01) and in the profession (p = 0.03); workers with higher job security (p < 0.01); and workers with more exposure to moving or lifting very heavy loads (p < 0.01) and to toxic substances (p = 0.03). In the intervention group fewer individuals smoked (p < 0.01), more individuals regretted not being able to work (p = 0.04), and more individuals did not know the occupational physician (p < 0.01) (table 1).
Analyses of regression models showed that the primary outcome result did not change after controlling for these 11 confounding variables or after controlling for all potential confounders.
Interaction analyses and stratified evaluations revealed that the intervention decreased the rate of benefit non‐dependence for patients employed by their current employer for less than one year from 90% (n = 104) in the control group to 75% (n = 24) in the intervention group (employer experience × study group: p = 0.04; <1 year employer experience group: p = 0.04). However, this difference did not persist after controlling for the 11 confounding variables.
Discussion
The current study, enhancing information availability between social insurance physicians and occupational physicians, revealed no positive effect on the work resumption outcome parameters of patients on subacute sickness absence. The isolated significant finding, for patients with a short length of employment, did not persist after controlling for confounders and may have arisen from multiple testing. Therefore, we cannot exclude the possibility that the null hypothesis is true, meaning that work resumption of patients on sickness absence is not associated with physicians' information availability.
The main strength of this study is its innovative character—it focuses on stakeholders' information asymmetry in sickness absence. The issue of sharing information with all stakeholders and the impact on rehabilitation is a universally important one to occupational health practice. Another strength is that the patient sample covers patients with all kinds of disorders and working for all types of companies, free to handle return to work after sickness absence according to their own specific work resumption policy. Thirdly, the intervention was initiated for patients in the subacute sickness absence phase—the phase considered as the most appropriate and as a main principle for success in return to work management.11 Fourthly, outcome parameter data were objective, complete, and reliable. Finally, drop‐outs, which are a typical problem with longitudinal design, were negligible.
The main weakness of this study is the non‐randomised allocation of patients into intervention and control groups. This was partly avoided by correcting the results for over 30 confounding variables. However, data on confounding variables gathered through employees' self‐report and physician's communication forms may be influenced by their attitudes and expectations. Next, it is possible that factors influencing outcome were not included in the confounding variables. Compared to the overall industry distribution in Flanders, IDEWE over‐represents companies in the public sector (institutions of local, regional, and national authorities). Therefore, the intervention group may have included more employees from the public sector. There is limited evidence that public sector employment is associated with better prognosis for return to work.22 We cannot exclude that this difference affected results by enhancing the expression of the intervention on work resumption rate in the intervention group. Another weakness is that the presence of some information exchange for a minority of control group patients cannot be excluded. Furthermore, a selection bias by patients refusing participation cannot be excluded. Finally, the reader must appreciate that the authors do not claim the data to be widely representative: the study was conducted in three Belgian regions. Caution should be exercised in extrapolating results to other countries, varying by socio‐cultural differences, labour exit patterns, rehabilitation measures, jurisdictional differences in physicians' roles, level of benefit payments for both sickness absence and disability, and unemployment, and in social welfare and retirement systems.
We compared our study results with those of other studies. Some published articles in this field report broad interventions programmes including the improvement of stakeholders' communication.23,24 These return to work studies show positive results on sickness absence outcome, but further research is needed to identify what specific components of the broad intervention programmes were the most beneficial. Fewer published articles exist on the impact of positive intervention trials on work resumption in which the researchers concentrated primarily on the communication between stakeholders. Haase et al implemented systematic cooperation practices between occupational physicians and rehabilitation physicians. Time towards work resumption and the number of sickness absence days in the year after discharge from the rehabilitation clinic decreased significantly. However, these results were obtained by comparing the intervention group to a historical control group, making conclusions debatable.25 Of better quality was Scheel and colleagues' randomised controlled intervention study for low back pain patients on sickness absence for more than 16 days in Norway. Traditional case management was compared with structured communication and coordination between the general practitioner, the National Insurance Administration, the patient, and the employer of the patient. The passive intervention scheme improving stakeholders' information availability did not increase the use of active sick leave (a type of gradual work resumption) significantly. A more active approach, including an occupational physical therapist actively assisting, arranging, and coordinating active sick leave and communication between all parties, increased the use of active sick leave significantly.26 However, further analysis showed that none of the intervention schemes influenced sickness absence duration or return to work rate.27 Recently, Faber et al also reported lack of a positive effect on patient sickness absence after intervening in stakeholders' information asymmetry. Their intervention consisted of an inter‐physician communication training programme for occupational physicians and general practitioners, teaching the use of a cooperation protocol for low back pain patients on sickness absence for 3–12 weeks in the Netherlands. The effect of the implementation of the protocol was evaluated in a non‐randomised controlled intervention study. Patients in the intervention group resumed work significantly later.28
The trials by Scheel et al and Faber et al both underline our results. We report the lack of positive findings on patients' sickness absence after intervening in physicians' information asymmetry. One possible explanation is that the Belgian legal framework limited the chances of success. Legal obstructions included: the explicit prohibition of occupational physicians assessing the justification of individual sickness absences resulting in little or no contact with patients on sickness absence; the overall responsibility of the patient's employer for prevention management limiting the occupational physician's role to that of an advisor; the lack of financial incentives for companies or employers to encourage gradual or modified work resumption; the unclear legislation and inflexible administrative procedure for gradual work resumption; the indistinctness of information exchange and cooperation legislation; and the necessity for the informed consent of the patient. This study facilitated recent legislation adaptations aiming to overcome some of the obstructions, but the effects are still to be evaluated.
Other explanations concern the methods used to address the problem. Investigation of the communication forms revealed that social insurance physicians did not ask for the active involvement of the occupational physician on behalf of 243 (48%) of 505 intervention group patients, resulting in a less intense involvement of the occupational physician as hoped for. Maybe the use of a communication form was a suboptimal intervention, meaning that interventions should go further than improving information exchange and aim at real cooperation where physicians jointly pursue solutions for patients on sickness absence.26 Further research on communication models should also include the attending physician. The support of the attending physician may be a crucial and necessary condition to motivate the patient towards work resumption. Another recommendation is not to neglect the time aspect. Communication probably takes time. To achieve faster return to work, the intervention should take a minimum of time to be a solution for the (perceived) delay caused by the (perceived) poor communication.
In general, more research on information asymmetry in disability management and its effect on the outcome of patients on sickness absence is necessary. In countries where occupational physicians are not playing a major role for the patients' return to work after sickness absence, there could be an exchange of information between the patient's general practitioner, the social physician and the company regarding which working situations the patient should avoid.
Main messages
Many stakeholders, including many physicians, are involved in the guidance of the patient on sickness absence towards work resumption (disability management). Communication, information exchange, and collaboration between these physicians are considered to be necessary conditions to make disability management successful. Information asymmetry refers to the situation in which critical information is not or not appropriately exchanged. Information asymmetry between Belgian social insurance physicians and occupational physicians is believed to hinder disability management for patients on sickness absence.
The use of a communication form, enhancing information exchange between Belgian social insurance physicians and occupational physicians, did not result in improved patient work resumption outcome.
Intervention studies on return to work are sparse despite the fact that sickness absence is a major socioeconomic problem. Trials in this field focusing on communication between physicians are even sparser. More research on stakeholders' information asymmetry and its effect on sickness absence outcome are needed. Randomised controlled trials are necessary to confirm the current negative study results.
Policy implications
Research projects aiming to investigate stakeholders' information asymmetry and their complex relation to the sickness absence course of patients are needed urgently.
The findings in this study imply no supportive measures to enhance physicians' information exchange or collaboration practices.
In conclusion, the current analysis has highlighted the potential for assessing work resumption outcomes in the form of a traditional versus a standardised information exchange strategy, as well as many of the challenges associated with such an undertaking. Enhancing information exchange between physicians with the aim of improving patients' sickness absence outcome proved to be very complex.
Acknowledgements
We would like to thank both the Christian Sickness Fund and the Occupational Health Services IDEWE for implementing the study protocol. The social insurance physicians and occupational physicians participated in the regular local inter‐physician meetings and implemented the communication form. The nurses assessed the written informed consent procedure. The administrative staff ensured the assignment of patients to intervention and control groups, and coordinated the exchange of communication forms.
We would like to thank the Department of Insurance, Environmental, and Occupational Medicine, Katholieke Universiteit Leuven, Belgium for providing practical, technical, and material support.
We would like to thank the Occupational Health Services IDEWE for funding the trial.
Footnotes
Funding: The occupational health service IDEWE, which funded the trial, had no involvement in study design; collection, analysis, interpretation of data; writing of the report; or in the decision to submit the paper for publication. The Department of Insurance, Environmental, and Occupational Medicine, Katholieke Universiteit Leuven, Belgium provided practical, technical, and material support. The authors' work was independent of the funders.
Competing interests: none
References
- 1.Williams R M, Westmorland M. Perspectives on workplace disability management: a review of the literature. Work 20021987–93. [PubMed] [Google Scholar]
- 2.Krause N, Frank W, Dasinger L.et al Determinants of duration of disability and return‐to‐work after work‐related injury and illness: challenges for future research. Am J Ind Med 200140464–484. [DOI] [PubMed] [Google Scholar]
- 3.Krause N, Lund T. Returning to work after occupational injury. In: Barling J, Frone M, eds. The psychology of workplace safety. Washington: APA Books, 2003
- 4.Turner J, Franklin G, Turk D. Predictors of chronic disability in injured workers: a systematic literature synthesis. Am J Ind Med 200038707–722. [DOI] [PubMed] [Google Scholar]
- 5.Tveito T H, Hysing M, Eriksen H R. Low back pain interventions at the workplace: a systematic literature review. Occup Med 2004543–13. [DOI] [PubMed] [Google Scholar]
- 6.Staal J B, Hlobil H, van Tulder M W.et al Occupational health guidelines for the management of low back pain: an international comparison. Occup Environ Med 200360618–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boden L I, Galizzi M. Economic consequences of workplace injuries and illnesses: lost earnings and benefit adequacy. Am J Ind Med 199936487–503. [DOI] [PubMed] [Google Scholar]
- 8.Vingård E, Alexanderson K, Norlund A. Consequences of being on sick leave. Scand J Public Health 2004S63207–215. [DOI] [PubMed] [Google Scholar]
- 9.Alexanderson K, Norlund A. Future need for research. Scand J Public Health 2004S63256–258. [DOI] [PubMed] [Google Scholar]
- 10.Margoshes B. Disability management and occupational health. Occupational Medicine: State of the Art Reviews 199813693–703. [PubMed] [Google Scholar]
- 11.Frank J, Sinclair S, Hogg‐Johnson S.et al Preventing disability from work‐related low‐back pain. New evidence gives new hope—if we can just get all the players onside. CMAJ 19981581625–1631. [PMC free article] [PubMed] [Google Scholar]
- 12.Scheel I, Birger K, Herrin J.et al Active sick leave for patients with back pain. All the players onside, but still no action. Spine 200227654–659. [DOI] [PubMed] [Google Scholar]
- 13.Buijs P, van Amstel R, van Dijk F. Dutch occupational physicians and general practitioners wish to improve cooperation. Occup Environ Med 199956709–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anema J, van der Giezen A, Buijs P.et al Ineffective disability management by doctors is an obstacle for return‐to‐work: a cohort study on low back pain patients sicklisted for 3–4 months. Occup Environ Med 200259729–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Verbeek J, Spelten E, Kammeijer M.et al Return to work of cancer survivors: a prospective study into the quality of rehabilitation by occupational physicians. Occup Environ Med 200360352–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van der Weide W E, Verbeek J, van Dijk F. Relation between indicators for quality of occupational rehabilitation of employees with low back pain. Occup Environ Med 199956488–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krause N, Dasinger L, Neuhauser F. Modified work and return to work: a review of the literature. J Occup Rehabil 19988113–139. [Google Scholar]
- 18.Pransky G, Shaw W, Franche R.et al Disability prevention and communication among workers, physicians, employers, and insurers—current models and opportunities for improvement. Disabil Rehabil 200411625–634. [DOI] [PubMed] [Google Scholar]
- 19.Goldberg D. (1992). General Health Questionnaire (GHQ‐12). Windsor: NFER‐NELSON,
- 20.Von Korff M, Dworkin S, Le Resche L. Graded chronic pain status: an epidemiologic evaluation. Pain 199040279–291. [DOI] [PubMed] [Google Scholar]
- 21.Karasek R. Job demands; job decision latitude, and mental strain: implications for job redesign. Adm Sci Q 197924285–308. [Google Scholar]
- 22.Teasell R, Bombardier C. Employment‐related factors in chronic pain and chronic pain disability. Clin J Pain 200117S39–S45. [DOI] [PubMed] [Google Scholar]
- 23.Arnetz B, Sjögren B, Rydéhn B.et al Early workplace intervention for employees with musculoskeletal‐related absenteeism: a prospective controlled intervention study. J Occup Environ Med 2003455499–506. [DOI] [PubMed] [Google Scholar]
- 24.Wiesel S, Boden S, Feffer H. A quality‐based protocol for management of musculoskeletal injuries. A ten‐year prospective outcome study. Clin Orthop 1994301164–176. [PubMed] [Google Scholar]
- 25.Haase I, Riedl G, Birkholz L.et al Verzahnung von medizinischer rehabilitation und beruflicher reintegration. Arbeidsmed Socialmed Umweltmed 200237331–335. [Google Scholar]
- 26.Scheel I, Birger K, Herrin J.et al A call for action. A randomized controlled trial of two strategies to implement active sick leave for patients with low back pain. Spine 200227561–566. [DOI] [PubMed] [Google Scholar]
- 27.Scheel I, Hagen K, Herrin J.et al Blind faith? The effects of promoting active sick leave for back pain patients: a cluster‐randomized controlled trial. Spine 2002272734–2740. [DOI] [PubMed] [Google Scholar]
- 28.Faber E, Bierma‐Zeinstra S, Burdorf A.et al In a controlled trial training general practitioners and occupational physicians to collaborate did not influence sickleave of patients with low back pain. J Clin Epidemiol 20055875–82. [DOI] [PubMed] [Google Scholar]