Abstract
Objectives
To describe the risk of work injury by socioeconomic status (SES) in hospital workers, and to assess whether SES gradient in injury risk is explained by differences in psychosocial, ergonomic or organisational factors at work.
Methods
Workforce rosters and Occupational Safety and Health Administration injury logs for a 5‐year period were obtained from two hospitals in Massachusetts. Job titles were classified into five SES strata on the basis of educational requirements and responsibilities: administrators, professionals, semiprofessionals, skilled and semiskilled workers. 13 selected psychosocial, ergonomic and organisational exposures were assigned to the hospital jobs through the national O*NET database. Rates of injury were analysed as frequency records using the Poisson regression, with job title as the unit of analysis. The risk of injury was modelled using SES alone, each exposure variable alone and then each exposure variable in combination with SES.
Results
An overall annual injury rate of 7.2 per 100 full‐time workers was estimated for the two hospitals combined. All SES strata except professionals showed a significant excess risk of injury compared with the highest SES category (administrators); the risk was highest among semiskilled workers (RR 5.3, p<0.001), followed by nurses (RR 3.7, p<0.001), semiprofessionals (RR 2.9, p = 0.006) and skilled workers (RR 2.6, p = 0.01). The risk of injury was significantly associated with each exposure considered except pause frequency. When workplace exposures were introduced in the regression model together with SES, four remained significant predictors of the risk of injury (decision latitude, supervisor support, force exertion and temperature extremes), whereas the RR related to SES was strongly reduced in all strata, except professionals.
Conclusions
A strong gradient in the risk of injury by SES was reported in a sample population of hospital workers, which was greatly attenuated by adjusting for psychosocial and ergonomic workplace exposures, indicating that a large proportion of that gradient can be explained by differences in working conditions.
Main indicators of socioeconomic status (SES) include education, income and occupational class (position in hierarchy).1 These variables tend to be highly correlated empirically and there is little consensus on which indicator would represent a more valid measure of SES.2,3
Two main theoretical approaches are present in the sociological literature, one considering social stratification due to inequalities in resources distribution and the other due to inequalities in power distribution. The first one identifies social status with social prestige, which would be best described by the access individuals have to limited resources in society, such as goods, services and knowledge.1 Researchers adopting this theoretical model have mainly used educational attainment or social prestige associated with occupation as measures of SES, because of their direct or indirect influence on access to all these types of resources. According to the second approach, the social status of individuals is best represented by their economic and political power in society, which would be the actual determinant of the distribution of resources. In this view, power is intended as control over the means of production, investments, decision making, other people's work and one's own work.4 The SES indicator mostly used by this line of research is occupational social class, constructed by reclassifying occupations on the basis of the different aspects of control over work.
Although educational level and occupational class are in general strongly correlated, some studies have found them to exert independent effects on mortality and morbidity in multivariate analyses,2,5,6 suggesting that using either SES classification alone probably results in some misclassification of the social position of individuals. Other authors have stressed the importance of developing more complete SES indicators, which should include different social features, such as social network, income and wealth, apart from occupation and education.3,7,8
Occurrence of injury at work is higher in those with lower education9,10,11 and lower occupational class.12 This inverse relationship has been attributed largely to the fact that people in higher SES strata are mainly employed in jobs with less hazardous working conditions. Many of the known risk factors for occupational injury are in fact predominant in lower status jobs; these include ergonomic exposures such as high physical workload, lifting and bending,11,13,14,15 psychosocial,10,16 and organisational features such as shiftwork, understaffing, overcrowding, work pressure, overtime level, safety climate and subcontracted work.10,17,18,19,20
However, it has also been suggested that lower education could act as an independent risk factor, through lower risk perception, which could lead to unsafe work practices,21,22 or through less access to information on hazardous jobs.23 Other individual risk factors, not apparently related to the workplace, include exercise level,24,25 marital status,18 smoking,24,26 family conflicts,18 stressful life events27 and daily hassles.28 Although some of these may also show a socioeconomic gradient, it is not clear that they exercise causal effects on workplace injury that are independent of occupational conditions.
The healthcare sector is one of the industries in the US at highest risk, with yearly rates of 9.7 recordable injury and illness cases per 100 workers in hospitals and 12.6 in nursing homes.29 There were almost 14 million healthcare workers in 2003, representing nearly 10% of the US working population, with a substantial proportion of women (more than 75% of the workers) and racial/ethnic minorities (30% in the US).30 Of these, almost six million were employed in hospitals.30 The wide range of jobs, such as nurses, aides, laundry and food workers, health technicians, clerks, administrators, doctors and clinical scientists, involve very different socioeconomic positions and working conditions. This highly diverse workforce offers an opportunity, at least in principle, to disentangle the respective influences of SES, working conditions and demographic characteristics on injury rates. For this purpose, a new SES classification specific for the healthcare industry, which was explicitly based on power distribution—namely, the responsibility level typical of each job title, but also included education as a prestige‐based measure was developed.
Therefore, the objectives of this study were:
to evaluate the predictive value of SES on the risk of Occupational Safety & Health Administration (OSHA)‐recordable workplace injuries in a sample of the Massachusetts hospital workforce and
to assess whether any differences in the risk of injury by SES could be explained by psychosocial, physical or organisational factors at work.
Methods
Data collection
This study was carried out within a larger project that was investigating socioeconomic disparities in health among healthcare workers, “Promoting healthy and safe employment in healthcare”.31 The study population consisted of all subjects aged at least 18 years, working in two moderate‐size private hospitals in northeastern Massachusetts. Administrative data on the workforce, collected from both hospitals' workforce rosters, included information on department, job title, hourly wage, hours worked per week, gender, race/ethnicity, age, date of hire and place of residence of each worker as of spring 2002. All job titles were codified according to the US Standard Occupational Classification system by an expert coder. Median age, gender ratio and proportion of non‐white or Latino workers were computed for each job from the roster data.
The research team independently developed a classification of SES in five classes, specific for the healthcare industry, on the basis of responsibility level and minimal education required to perform a certain job (table 1). Each job title was assigned to one of five categories: administrators, professional, semiprofessional, skilled and semiskilled workers. Nurses were included in the “professional” category, but, after a preliminary analysis showing that their exposure profile and their risk of injury were different from those of professionals, they were treated as a separate subgroup, and also because they represented such a large subgroup of professionals (71%) that their results would have obscured those on the remaining jobs in this category.
Table 1 Sociodemographic characteristics of the workers employed in two private hospitals, Massachusetts, 2002.
| Hospital 1 | Hospital 2 | p Value* | |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Age (years) | 42.3 (12.9) | 40.6 (12.9) | <0.001 |
| Hours worked per week | 25.2 (16.2) | 25.3 (15.4) | 0.40 |
| Hourly wage | 21.3 (12.7) | 19.9 (9.1) | 0.006 |
| n (%) | n (%) | p Value† | |
| Female gender | 1086 (80.2) | 1422 (82.7) | 0.08 |
| Non‐white ethnicity | 119 (8.8) | 250 (14.5) | <0.001 |
| Per diem workers | 301 (22.2) | 371 (21.6) | 0.66 |
| Occupational class | <0.001 | ||
| 6—Administrators | 49 (3.6) | 10 (0.6) | |
| 5—Professionals | 171 (12.6) | 184 (10.7) | |
| 4—Nurses | 336 (24.8) | 532 (30.9) | |
| 3—Semiprofessionals | 300 (22.2) | 284 (16.5) | |
| 2—Skilled workers | 396 (29.3) | 562 (32.7) | |
| 1—Semiskilled workers | 102 (7.6) | 148 (8.6) | |
| Total | 1354 (100.0) | 1720 (100.0) |
*Mann–Whitney two‐sample test.
†χ2 test.
OSHA logs of occupational injuries and illnesses were obtained from the hospitals; they included injuries recorded during 1997–2001 for hospital 1 and during 1998–2002 for hospital 2. OSHA logs contain information on job title of the injured worker, as well on the type of accident, nature and agent of the injury, body part injured and the direct consequences of the injury (days away from work and restricted work days) as of the time that the injury was recorded. Job titles in the OSHA logs were linked to the facility job roster and the SES classification developed by the research team.
Psychosocial, ergonomic and organisational exposures were assigned to the hospital workers through the O*NET job–exposure matrix, V.4.0.32 This is a national, online database (http://www.onetcenter.org), which is administered and sponsored by the US Department of Labor's Employment and Training Administration33 and replaces the Dictionary of Occupational Titles. More than 400 variables describe each job title in O*NET, grouped in 6 main dimensions: worker characteristics, worker requirements, experience requirements, occupation requirements, occupation characteristics and occupation specific. O*NET scores for each selected variable range from 1 to 5 or 1 to 7 and represent the average of the expert ratings or worker's responses for each job title. The job classification used in O*NET is specific to this database but can be crosswalked to the Standard Occupational Classification 2000 coding system. Hospital jobs not found in the O*NET database (29 of 143 job codes) were excluded from analyses that included O*NET occupational exposures.
Exposure variables of interest were selected from the O*NET database (table 2) on the basis of the risk factors for injuries identified from previous research. Seven variables were used singly and five scales were constructed from combinations of multiple O*NET items. One composite scale was the sum of several physical demand variables, while the rest corresponded to psychosocial conditions at work such as psychological demands, job control, social support (job content questionnaire34), intrinsic and extrinsic rewards (effort–reward imbalance35). Psychological demands and job control were examined either individually or as the job strain ratio (demands divided by control). Since these exposure scales had varying ranges they were all divided into quintiles for comparability. Mean quintiles were computed among all jobs in each SES stratum.
Table 2 Selected O*NET exposure variables, internal consistency of composite scores in the job–exposure matrix and Spearman correlation coefficients between socioeconomic status and quintiles of selected exposure scores in O*NET job–exposure matrix: 114 jobs in two private hospitals, Massachusetts, 2002 .
| Exposure | O*NET variable(s) | Cronbach's α | Spearman's r coefficient | p Value |
|---|---|---|---|---|
| Psychological demands | Abilityim20, abilityim21, abilitylv20, abilitylv21, values09 | 0.79 | 0.23 | 0.003 |
| Decision latitude | Values07, values15, values16, values19, values25, values27 | 0.92 | 0.69 | <0.001 |
| Job strain ratio | Ratio of psychological demands by decision latitude | –0.51 | <0.001 | |
| Rewards | Values13, values20, values10, values18, values22 | 0.84 | 0.63 | <0.001 |
| Coworkers support | Values14 | 0.31 | 0.001 | |
| Supervisor support | Values23, values24 | 0.76 | –0.45 | 0.001 |
| Noise level | Context11 | –0.19 | 0.02 | |
| Uncomfortable temperature extremes | Context12 | –0.09 | 0.25 | |
| Hazardous equipment | Context21 | –0.07 | 0.35 | |
| Time bending or twisting the body | Context30 | –0.16 | 0.04 | |
| Time kneeling, crouching, stooping or crawling | Context27 | –0.13 | 0.10 | |
| Capacity to exert force | Abilitylv32, abilitylv33, abilitylv34, abilitylv35, abilitylv36, abilitylv37, abilitylv38 | 0.96 | –0.23 | 0.004 |
| Pause frequency | Values09 | –0.18 | 0.02 |
Data analysis
Sociodemographic differences between the two hospital workforces were tested using the Mann–Whitney two‐sample statistic for continuous variables (age, number of hours worked per week and hourly wage) and χ2 statistics for differences in categorical proportions (gender, ethnicity, per diem schedule and SES). Spearman correlation coefficients between O*NET exposure scores and SES were computed on 114 jobs. Trends in exposure scores across SES strata were evaluated through a linear regression model using variance‐weighted least squares, in which homogeneity of variance in different categories is not assumed. Since O*NET is a one‐dimensional matrix, using occupation but not industrial sector as the key entrance to the job description, jobs not specific to healthcare (eg, cook, dishwasher, janitor and secretary) could present a higher likelihood of exposure misclassification than the healthcare‐specific job titles. To assess whether this occurred, the correlation between O*NET exposures and SES was examined separately for healthcare‐specific and non‐specific jobs. Likewise, the risk of injury associated with O*NET exposures was analysed separately for the two job groups.
The association between SES and work injuries was evaluated using a retrospective design. Workforce rosters before 2002 were not available; therefore, the actual workforces were used to represent denominators for previous years, assuming that the relative proportions of workers by job title and SES had remained relatively constant across the years. Injury rates were analysed as frequency records using job code or job group (SES level) as the unit of analysis. Each worker was considered to contribute to the denominator according to the number of hours worked per week. Per diem workers, who lacked this information in the administrative database, were assigned the average number of hours per week (18.6 h/week) reported by per diem participants in a questionnaire survey at one of the hospitals. By using the Poisson regression modelling, relative risks (RRs) of injury and number of work days lost by SES stratum were assessed using administrators as the reference category and computing rate ratios with 95% Poisson CIs. The trend in risk was assessed through linear regression of the coefficients obtained from the Poisson regression, using the coefficient standard errors as weights.
In a separate analysis, without the 29 jobs not found in the O*NET job–exposure matrix, O*NET exposure variables were included as independent variables, together with indicator terms for SES strata. The risk of injury was modelled using SES alone, each exposure variable alone and then each exposure in combination with SES. Exposure scores were treated as continuous variables, assuming linearity of the increase in risk across quintiles.
Finally, all exposures were tested for statistical significance together with SES in one model; variables were included in the model in decreasing order according to their crude coefficient on the risk of injury and were retained if they were significant (p = 0.05) or changed the coefficients of other variables >20%. The “best‐fit” model was the one with the smallest deviance from the saturated model and the highest proportion of variance explained (R2).
Results
Workforce rosters included information on 1354 workers at hospital 1 and 1720 workers at hospital 2 (table 1). Subjects employed at hospital 1 were older and had a higher average hourly salary than those working at hospital 2. They also included fewer women and minority workers.
In the period examined, 834 injuries were recorded in the OSHA log system, 309 in hospital 1 (1997–2001) and 525 in hospital 2 (1998–2002). The most frequent causes of injuries were to be struck by or against objects (39%) and overexertion (21%), followed by contact with biological agents (7%) and falls (3%); about 5% of cases represented chronic conditions, mainly musculoskeletal disorders. The most frequent consequences of the accidents were cuts, lacerations, needle sticks and punctures (35%); strains and sprains (23%); and bruises and contusions (6.7%). Body parts that were most often injured were the hand or fingers (10.4%), eye (3.7%), knee (3.2%) and back (13.5%). Injuries without lost working days represented 65% of total injuries, and 20% caused an absence from work for >3 days.
An overall yearly injury rate of 7.2 (95% CI 6.7 to 7.7) per 100 full‐time workers was estimated for the two hospitals combined. The rate was 2.5 (95% CI 2.3 to 2.8) for injuries with at least one lost work day. The rate of injury in hospital 2 was higher than in hospital 1 (RR 1.33, 95% CI 1.16 to 1.54); this excess risk was slightly reduced controlling for SES (RR 1.26), job median age (RR 1.18) or job ethnicity ratio (RR 1.21), but not gender ratio.
All five composite scores from the O*NET variables demonstrated high internal consistency by Cronbach's α (table 2). Force exertion, kneeling and bending, and exposure to noise, heat and hazardous equipment were positively correlated with all correlation coefficients above 0.40. Among psychosocial exposures, the job strain ratio was highly associated with both extrinsic/intrinsic rewards (r = –0.61) and supervisor support (r = 0.47).
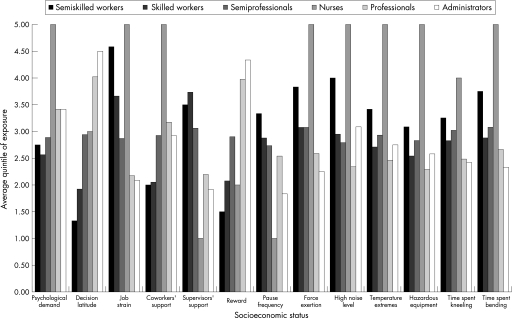
In general, working conditions were less favourable in the lower SES strata, except for psychological demands, supervisor support and pause frequency (fig 1). However, the exposure of nurses to psychosocial and physical hazards was more similar to or even higher than workers in the lower SES categories, with the highest level of exposure for all risk factors evaluated except low decision latitude and low rewards. SES was significantly correlated with all O*NET exposures evaluated, except with local temperature extremes (too high or low), working with hazardous equipment and time spent kneeling, crouching, stooping or crawling (table 2). These results were confirmed by means of linear regression modelling, except that the association with time spent kneeling, crouching, stooping or crawling became stronger and statistically significant in this analysis (data not shown). The correlation between SES and most O*NET exposures was similar among jobs specific and non‐specific to healthcare. Exceptions were a few physical exposures (force exertion, frequent bending and kneeling), which, unexpectedly, were not correlated with SES among jobs specific to healthcare, but only among generic jobs.
Figure 1 Mean O*NET quintile of exposure by socioeconomic status (SES), 114 jobs in two private hospitals, Massachusetts, 2002.
Among job titles with at least five injuries recorded, all those with yearly injury rates >10 per 100 full‐time workers belonged to the two lowest SES categories, except for “miscellaneous health technologists and technicians” (table 3).
Table 3 Yearly injury rates by Census 2000 job titles: hospital jobs with at least five recorded injuries per 100 full‐time employees.
| Census 2000 job title | Injuries, n (5 years) | Injury rate per 100 FTEs |
|---|---|---|
| Janitors and building cleaners | 34 | 21.3 |
| Electrical and electronics repairers, industrial and utility | 11 | 20.1 |
| Cooks | 13 | 17.5 |
| Dining room and cafeteria attendants and bartender helpers | 30 | 13.4 |
| Miscellaneous health technologists and technicians | 60 | 13.2 |
| Maids and housekeeping cleaners | 18 | 11.6 |
| Nursing, psychiatric and home health aides | 95 | 10.1 |
| Emergency medical technicians and paramedics | 10 | 9.8 |
| Health diagnosing and treating practitioner support technicians | 23 | 9.5 |
| Registered nurses | 290 | 9.2 |
| Respiratory therapists | 9 | 9.2 |
| Licensed practical and licensed vocational nurses | 18 | 9.0 |
| Security guards and gaming surveillance officers | 12 | 8.8 |
| Medical assistants and other healthcare support occupations | 17 | 7.2 |
| Grounds maintenance workers | 8 | 7.0 |
| Clinical laboratory technologists and technicians | 19 | 6.5 |
| Diagnostic‐related technologists and technicians | 27 | 5.6 |
| Medical scientists | 7 | 4.5 |
| Office clerks, general | 19 | 3.9 |
| First‐line supervisors/managers of office and administrative support workers | 11 | 3.7 |
| Secretaries and administrative assistants | 11 | 2.9 |
FTEs, full‐time employees.
Injury rates were lowest and similar between hospitals for the SES categories of administrators and professionals (table 4). The risk of injury was highest in the lowest SES class, with a RR of >5, followed by nurses, whose risk was almost four times higher. Skilled labourers and semiprofessionals had rates almost three times higher than in the highest SES stratum. The inverse trend in the risk of injury by SES was significant (p = 0.04) only after exclusion of the nurses.
Table 4 Average work days lost, injury rates and RRs of injury by socioeconomic status category, stratified by number of work days lost (0 vs ⩾1).
| Occupational class (number of injuries) | Average yearly work days lost per 100 FTEs | Yearly injury rates per 100 FTEs | RR of injury by SES | RR for injuries with no lost work days | RR for injuries with ⩾1 lost work days |
|---|---|---|---|---|---|
| n | Rate (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Administrators (7) | 0.7 | 2.5 (1.0 to 5.1) | 1.00 | 1.00 | 1.00 |
| Professionals (32) | 43.1 | 2.3 (1.6 to 3.2) | 0.93 (0.41 to 2.11) | 0.71 (0.29 to 1.77) | 2.24 (0.29 to 17.4) |
| Nurses (107) | 59.6 | 9.2 (8.2 to 10.3) | 3.73 (1.76 to 7.90) | 3.29 (1.46 to 7.40) | 6.40 (0.89 to 46.1) |
| Semiprofessionals (156) | 69.8 | 7.1 (6.0 to 8.3) | 2.87 (1.34 to 6.11) | 2.19 (0.96 to 4.98) | 7.15 (0.99 to 51.6) |
| Skilled workers (218) | 28.6 | 6.4 (5.6 to 7.3) | 2.61 (1.23 to 5.53) | 1.88 (0.83 to 4.25) | 7.19 (1.00 to 51.6) |
| Semiskilled workers (290) | 148.4 | 13.0 (10.6 to 15.7) | 5.26 (2.45 to 11.3) | 2.64 (1.13 to 6.18) | 21.2 (2.91 to 151.5) |
FTE, full‐time employee; SES, socioeconomic status.
On average, administrators had lost <1 day due to injury per 100 full‐time workers per year (table 4); in the other SES categories the number of days lost increased with SES (except for skilled workers) to a high of about 150 per 100 workers (p = 0.45). For injuries without lost work days, the risk was approximately doubled in all groups except professionals and there was no linear trend with SES. For injuries with at least one work day lost there was a RR of 6–7 in nurses, semiprofessionals and skilled workers, marginally significant for semiprofessionals and skilled workers, whereas the increase in risk was markedly higher for the lowest SES category.
Among the 114 jobs matched to the O*NET job–exposure matrix, the injury rate was significantly associated with each exposure considered except pause frequency (table 5). Healthcare‐specific and non‐specific jobs did not show a significant difference in the coefficients of the risk of injury associated with O*NET exposures, except for coworkers' support and pause frequency. The exclusion of 29 jobs not in the matrix resulted in the exclusion of 13.1% of the population being studied and 19.8% of the injuries; it also resulted in a stronger gradient in risk by SES categories, compared with the analysis including all jobs (table 5, first row, vs table 4, RR column). The population linkable to the O*NET matrix showed a risk of injury higher than the unlinked one and a lower proportion of subjects in lower SES strata (data not shown).
Table 5 RRs of injury by socioeconomic category, unadjusted and adjusted by quintiles of O*NET exposure scores: 114 hospital jobs in 6 strata (reference category = administrators).
| O*NET exposure | RR per quintile of exposure (95% CI) | RR per quintile of exposure adjusted by SES (95% CI) | SES‐specific RR, adjusted for O*NET exposures (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| Professionals (29)* | Nurses (41)* | Semiprofessionals (111)* | Skilled (176)* | Semiskilled (290)* | |||
| No adjustment | 1.62 (0.49 to 5.32) | 6.80 (2.18 to 21.2) | 4.81 (1.53 to 15.1) | 4.47 (1.43 to 14.0) | 6.71 (2.08 to 21.7) | ||
| Psychological demand | 1.10 (1.04 to 1.17) | 1.01 (0.94 to 1.09) | 1.61 (0.49 to 5.30) | 6.69 (2.13 to 21.0) | 4.84 (1.54 to 15.3) | 4.47 (1.43 to 14.0) | 6.71 (2.08 to 21.7) |
| Decision latitude | 0.81 (0.75 to 0.87) | 0.70 (0.61 to 0.80) | 1.58 (0.48 to 5.19) | 4.55 (1.44 to 14.3) | 2.53 (0.78 to 8.20) | 1.86 (0.56 to 6.11) | 2.35 (0.68 to 8.11) |
| Job strain ratio | 1.31 (1.22 to 1.41) | 1.14 (1.04 to 1.26) | 1.50 (0.46 to 4.93) | 4.36 (1.34 to 14.2) | 3.95 (1.24 to 12.6) | 3.15 (0.98 to 10.1) | 4.49 (1.34 to 15.0) |
| Rewards | 0.70 (0.65 to 0.76) | 0.76 (0.67 to 0.86) | 1.50 (0.46 to 4.92) | 3.68 (1.15 to 11.8) | 2.89 (0.90 to 9.33) | 2.25 (0.69 to 7.34) | 2.84 (0.83 to 9.72) |
| Coworkers' support | 1.20 (1.13 to 1.28) | 1.18 (1.08 to 1.29) | 1.62 (0.49 to 5.32) | 5.40 (1.72 to 16.9) | 4.96 (1.57 to 15.6) | 5.16 (1.65 to 16.2) | 7.60 (2.35 to 24.6) |
| Supervisors' support | 0.91 (0.86 to 0.96) | 0.90 (0.82 to1.00) | 1.67 (0.51 to 5.49) | 6.46 (2.07 to 20.2) | 5.51 (1.74 to 17.5) | 5.71 (1.78 to 18.3) | 7.99 (2.45 to 26.1) |
| Noise | 1.24 (1.17 to 1.31) | 1.14 (1.05 to 1.24) | 1.76 (0.54 to 5.79) | 5.26 (1.67 to 16.6) | 5.12 (1.63 to 16.1) | 4.47 (1.43 to 14.0) | 6.14 (1.90 to 19.9) |
| Temperature too high or too low | 1.20 (1.14 to 1.27) | 1.08 (1.00 to 1.17) | 1.57 (0.48 to 5.15) | 5.47 (1.72 to 17.4) | 4.72 (1.50 to 14.9) | 4.10 (1.30 to 12.9) | 5.94 (1.83 to 19.3) |
| Hazardous equipment | 1.21 (1.14 to 1.28) | 1.09 (1.02 to 1.17) | 1.47 (0.45 to 4.84) | 5.01 (1.56 to 16.1) | 4.33 (1.37 to 16.7) | 3.83 (1.21 to 12.1) | 5.71 (1.75 to 18.6) |
| Bending | 1.36 (1.27 to 1.45) | 1.29 (1.18 to 1.40) | 1.08 (0.33 to 3.57) | 2.92 (0.91 to 9.41) | 3.33 (1.05 to 10.6) | 2.66 (0.84 to 8.44) | 3.46 (1.05 to 11.4) |
| Kneeling | 1.40 (1.29 to 1.52) | 1.27 (1.16 to 1.39) | 1.25 (0.38 to 4.14) | 3.90 (1.23 to 12.4) | 3.38 (1.06 to 10.7) | 2.93 (0.93 to 9.28) | 3.99 (1.22 to 13.1) |
| Force exertion | 1.37 (1.28 to 1.47) | 1.29 (1.18 to 1.40) | 1.14 (0.34 to 3.76) | 2.91 (0.90 to 9.41) | 3.23 (1.02 to 10.3) | 2.66 (0.84 to 8.45) | 3.46 (1.05 to 11.4) |
| Pause frequency | 1.03 (0.98 to 1.09) | 1.17 (1.09 to 1.26) | 1.49 (0.45 to 4.91) | 7.74 (2.48 to 24.2) | 4.10 (1.30 to 13.0) | 3.98 (1.27 to 12.5) | 5.30 (1.63 to 17.2) |
| Decision latitude+force exertion+supervisor support+temperature extremes | 1.16 (0.35 to 3.84) | 2.39 (0.73 to 7.82) | 2.42 (0.74 to 7.91) | 2.02 (0.60 to 6.82) | 2.23 (0.64 to 7.80) | ||
*Number of injuries.
When single exposure variables were included in the model with SES, five of them, in particular, had a strong decrease in the RR of injury for the three lowest SES strata: decision latitude, rewards (both protective), bending, kneeling and forceful exertion. Jobs including only female workers were significantly protected (p<0.001), although adjustment for this variable did not substantially change the risk related to SES. Hospital was not included in these analyses as a control variable, because, although it retained a significant effect, there were no important changes in coefficients of other variables, while producing more unstable models. All exposure variables, except psychological demand, were still significantly associated with the risk of injury after adjusting for SES, although their coefficients were smaller; the only exception was decision latitude, for which the relative protection for the highest versus the lowest quintile increased from 0.81 to 0.70.
The strongest decrease in risk by SES was reported by including decision latitude and force exertion in the regression model simultaneously. The effect of SES dropped to about one‐third among nurses, skilled and semiskilled workers and to one‐half in semiprofessionals after adjusting for these factors. An alternative model including “frequent bending” instead of “force exertion” displayed an equivalent fit and produced similar RRs by SES (data not shown). The variable “temperature extremes” was also added to the model, despite it being only marginally associated with the risk of injury (p = 0.08), because it increased the estimated coefficient for force exertion by almost 30%; however, it did not have an effect on the risk by SES. The model with the highest fit also included supervisor support, whose inclusion produced a slight increase in the RR by SES, compared with the previous model; this increase was owing to the fact that supervisor support, as expected, presented a protective effect on the risk of injury (table 5), although, according to O*NET it was higher in lower SES strata.
Discussion
In these two medium‐size hospitals, there was a strong SES gradient in the risk of injury, the RR for the lowest category versus the highest being 5.3 for all injuries and 21.2 for injuries with at least one work day lost. Similarly, the number of work days lost was two orders of magnitude higher in semiskilled workers than in administrators. The steeper SES gradient in risk reported for injuries with work days lost and the longer mean prognosis of injuries among low SES subjects both indicate that work injuries are on average more severe in these workers.
A strong decrease in the SES gradient was reported after adjustment for physical and psychosocial exposures at work. This demonstrated that a great proportion of the differences in injury rates between social strata could be explained by differences in workplace exposures. Only a few variables could be fitted in this model, because of collinearity among the exposures, so the selection of a final model is slightly arbitrary. However, it is worth noting that the retained predictors represent three main workplace dimensions known to influence the risk of injury—namely psychosocial (decision latitude and supervisor support), physical (force exertion) and environmental (temperature extremes). Of particular interest is the observation that the physical exposures such as trunk bending and forceful exertions seemed to explain the greatest proportion of excess risk for the professional employees (table 5), whereas the psychosocial dimensions of decision latitude and rewards had the greatest impact for the lower status jobs.
In the two hospitals there was a yearly reported injury rate of 7.2 per 100 full‐time workers and a rate of 2.5 per 100 full‐time employees (FTEs) for injuries with lost work days. The first figure is lower than the corresponding rate of occupational injuries and illnesses reported by Bureau of Labor Statistics29 for hospital workers, whereas the second one is quite consistent (9.7 and 2.3 per 100 full‐time workers for total injuries and injuries with lost work days, respectively).
Although there may have been some under‐reporting in the facilities examined, it is also likely that these community hospitals had lower rates than those in other types of hospitals, especially large teaching and referral facilities. Differences in injury rates among facilities seem to be largely unexplained to date. Wilkinson et al36 reported 5.9 occupational injuries per 100 full‐time workers in a US health science centre and teaching hospital. A large teaching hospital in Massachusetts had a back injury rate of 1.4 per 100 FTEs, also using OSHA logs as a source of cases of injury.37 This value appears similar to or lower than our data, in which back injuries were 25% of total injury records (rate = 1.8 per 100 FTEs). Injuries involving days away from work in a large teaching hospital in the Midwest had almost double the rate we observed. At this facility, African‐American workers represented half of the working population and had a threefold RR of any injury.38 Thus, our study population might not be completely representative of the US healthcare workforce. There is no obvious reason why this should interfere with the generalisability of these results although, certainly, similar analyses should be carried out in other populations.
OSHA logs of occupational injuries are affected by under‐reporting: a comparison of occupational injuries reported in the National Health Interview Survey in 1994 with those from Bureau of Labor Statistics suggested that more than one‐fourth of injuries were not reported to or recorded by the employer.39 Under‐reporting in healthcare workers has been mainly investigated regarding percutaneous injuries, with estimates ranging from 18% in the US40 to about 2/3 of the total cases in Spain41 and Costa Rica.19 Nevertheless, there is no obvious reason that the two hospitals we studied should have dramatically more under‐reporting than US hospitals in general. In addition, the difference observed between administrators and other SES strata appears too big to be explained by factors different from injury severity, such as differential injury reporting.
The risk of injury in hospital 2 was significantly higher than in hospital 1 (RR 1.33, p = 0.01), and the RR was not modified by adjusting for SES or for exposure to occupational factors. A possible explanation is that workers in hospital 2 were younger and included a higher proportion of minority workers, which are both known risk factors for injuries at work. However, adjustment for job median age or proportion of non‐white workers reduced but did not cancel the excess risk. From data of the American Hospital Association, during 1997–2001, the two hospitals differed in the ratio between inpatient and outpatient activity:42 hospital 2 had a higher number of admissions per FTE (9.3 vs 7.2), whereas hospital 1 was characterised by almost twice as many outpatient visits per worker (157 vs 87). The higher proportion of organisational and technical procedures involved in inpatient care may explain the higher injury rate in hospital 2.
To our knowledge, no other study has investigated the overall risk of injury by socioeconomic or educational level in healthcare workers, although the differential risk reported in other industries seems consistent with our results. For example, increased risk of work injury (RR 3.8) was found among male blue‐collar employees in six industrial sectors in Israel, compared with white‐collar workers.10 Consistent with our results, the risk of injury related to low education (<12 vs ⩾12 years) decreased from 1.6 to 0.98 when adjusted for an ergonomic stress index, although the RR for blue‐collar status did not change substantially (all variables in the same model). In a Swedish population‐based study,12 a 2.7 RR of injury was reported in manual workers compared with non‐manual workers. Similarly, excess risk of work injury (RR 2.7) was shown by Oh and Shin11 in subjects with <12 years of education, compared with those with >15 years of education. The higher excess risks we reported were probably a result of including administrators and using a six‐level classification of SES, more articulated than the dichotomised variables used by these studies, whose risks resemble those in our central SES strata.
Although the gradient reported here could in theory be attributable to selective injury under‐reporting among workers in higher SES strata, this hypothesis seems to be contradicted by observations indicating that reporting barriers are more prevalent among low‐wage or temporary workers, who are at a higher risk of being fired because of filing injury claims43,44 and have more difficulties in affording lost work days45 and in accessing workers' compensation medical care.46,47 A study of 12 hospital environmental service departments, composed mainly of workers from low SES, found that 39% of injuries were not reported to the supervisor.48 This figure appears comparable to or higher than total under‐reporting in the healthcare industry in the US—for example, an Iowa survey of healthcare workers found that an overall 31% of percutaneous injuries or blood exposures were not reported, which decreased to 27% among registered nurses and 21% among medical technologists, both in higher SES levels.49
One strength of this study is that exposures were attributed through a job–exposure matrix from O*NET and injuries were obtained from OSHA logs. This use of two independent data sources should protect against distortions of the risk estimates owing to differential misclassification of exposures. However, the use of a job–exposure matrix to assign exposures is likely, in general, to cause non‐differential exposure misclassification.50 These analyses would therefore be expected to underestimate the effects of exposure on the risk of injury, with a consequent overestimate of the RR by SES adjusted by occupational exposures, owing to increased residual confounding.
The comparison between subjects linked or unlinked to the O*NET matrix indicates that the job titles linked had, on average, higher risks of injury and higher SES than the unlinked ones. Such a selection is not expected to have caused a distortion of the risk of injury associated with exposures or to SES, but it possibly reduced the generalisability of our results, although the proportion of injuries and workforce excluded was small.
O*NET has some drawbacks as a job–exposure matrix. The ratings are based on either expert assessments, without explicit reference values or on “incumbent” (worker) ratings by a relatively small number of subjects. In neither case is there an explicit consideration of potential sources of within‐job variability in exposure. In particular, O*NET is a one‐dimensional matrix because it only has job title as the key entrance to the job description, and not industrial sector. There are many jobs in the study population that are not specific to healthcare (eg, cook, dishwasher, janitor, secretary and so on). In addition, some healthcare‐specific jobs may have different exposures depending on where they are located (eg, nurse in hospital, nursing home, school, outpatient clinic, community/visiting service and so on). However, except for a few physical exposures, the correlation between SES and most O*NET exposures was similar among jobs specific and non‐specific to healthcare, as was the relationship between exposures and the risk of injury.
In all, 11 of 13 workplace exposures selected from the O*NET database were significantly associated with the risk of injury, demonstrating that the predictive validity of this job–exposure matrix is satisfactory, despite its limitations. All exposures examined were selected because they were found to be associated with the risk of injury in previous studies, either among healthcare workers or in other industries. For example, Hemingway and Smith51 found an increased risk of reported injuries in Canadian nurses associated with high workload, low peer cohesion, low autonomy and high role ambiguity. In a study on Finnish hospital personnel, low decision latitude, low skill discretion and monotonous work were significant predictors of work injuries.16 In two studies of workplace safety climate, support from management for safety programmes and safety‐related training were the two most important factors related to the incidence of workplace exposure to blood and other body fluids52 and to overall injury incidence.19 Results from different industries and from population‐based studies support an excess risk of injury for exposure to high physical workload and lifting,11,13 use of machinery,11 climate discomfort10 and work pressure.17
An effect on the risk of injury was reported for almost all occupational exposures examined, even after adjusting for SES. This finding would confirm the results of previous studies showing an association with these risk factors, although there is the possibility that such an independent effect would instead be attributable to SES residual confounding, owing to low accuracy of SES attribution, which could have reduced the correlation between occupational exposures and SES. However, we believe that the SES classification adopted in this study was quite accurate, as it was articulated in several classes, it included both power and prestige social features of a certain job and was developed by insiders of the healthcare industry with a long work experience. Especially for low‐decision latitude, it seems that at least part of its effect on the risk of injury would be independent of SES, given that its risk was not attenuated but rather increased after adjustment for this variable. Support for this view also comes from studies of SES, psychosocial factors at work and the risk of coronary heart disease, in which a significant effect associated with decision latitude, independent of SES, was reported even after further adjustment for the main behavioural/biological risk factors for coronary heart disease, which should have limited the extent of possible SES residual confounding.53,54
Since workforce rosters were not available before 2002, it was not possible to analyse occurrences of injury at the individual level—that is, by merging workforce data and OSHA logs of injury by name or employee code number. Thus, we could not evaluate potential confounding by work‐related individual characteristics such as worker's age, gender, physical activity, seniority or day–night shifts. We tried to include in the model indicator variables for jobs including only women, men, white or non‐white workers. The female‐only jobs came out as a significant protective factor, although it did not modify the SES gradient much, nor did it change the inclusion of significant O*NET exposures. Also, the fit of the model was slightly but significantly increased. The other variables were not significant and did not change substantially other variable coefficients. Ethnicity as recorded in the workforce was determined to contain many errors in comparison with self‐reported survey information (unpublished).
Moreover, no information was available on extra‐occupational risk factors for work injuries, such as leisure physical activity,24,25 family conflicts18 and stressful life events.27 These factors seem to have a rather small influence on the risk of work injury, although their confounding role cannot be ruled out. In fact, because they are probably correlated with the occupational exposures on the basis of social class, both groups of risk factors may be mutually confounding.
Another potential limitation derives from the attribution of SES based on job title because no information could be obtained on household income or other individual socioeconomic indicators. This could lead especially to misclassification of women workers, who are a very large proportion of this study population, to the extent that SES of the family varies among individuals in similar jobs. Nonetheless, it seems questionable that an SES classification based on family characteristics could represent a better predictor of the risk of events occurring at work than one based on the position held by individuals within the workplace hierarchy.
Lastly, possible errors in job denominators cannot be excluded. Although the number of employees per job title could have changed during the years for which no information was available (1997–2001 and 1998–2001 for fospitals 1 and 2, respectively), interviews with human resource personnel indicated that no such large changes had occurred. Thus, it was necessary to assume that the relative proportions of workers by job title and SES had remained relatively constant. In addition, the workforce rosters lacked the weekly hours worked by per diem workers. We assigned them the average number of hours reported by questionnaire in a sample of per diem workers at hospital 2. However, this information was only provided by 20% of the per diem workers at hospital 2; assigning it to all per diem workers in both hospitals necessitated the assumption that this mean value was representative of all of them and did not vary by SES. Since the proportion of per diem workers was less than one‐fourth of the total workforce, the overall bias in the risk estimate owing to incorrect assignment of work time to these subjects is not expected to be important. However, we could not evaluate whether there was likely to be differential error by SES.
Conclusions
A strong gradient in the risk of reported injury was observed by SES in a population of hospital workers, which was even stronger for injuries involving lost work days. Selected workplace exposures were assigned to job titles through a job–exposure matrix; most of them were found to be significantly associated with injury rates. Controlling for psychosocial and ergonomic workplace exposures, the SES gradient in the risk of injury was greatly attenuated, indicating that a large proportion of that gradient can be explained by differences in working conditions.
Acknowledgements
We thank Jody Lally for facility liaison and assistance with data collection Joan Handstad and Mary Ellen Davis for facilitation of data collection Maggie Y Hood for Standard Occupational Classification coding of job titles and Gustavo Perez‐Reyes for coding of OSHA logs.
Abbreviations
FTE - full‐time employee
OSHA - Occupational Safety and Health Administration
SES - socioeconomic status
Footnotes
Funding: This research was supported by Grant Number R01‐OH07381 from the National Institute for Occupational Safety and Health. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH.
Competing interests: None.
References
- 1.Krieger N, Williams D R, Moss N E. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health 199718341–378. [DOI] [PubMed] [Google Scholar]
- 2.Davey Smith G, Hart C, Hole D.et al Education and occupational social class: which is the more important indicator of mortality risk? J Epidemiol Community Health 199852153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oakes J M, Rossi P H. The measurement of SES in health research: current practice and steps toward a new approach. Soc Sci Med 200356769–784. [DOI] [PubMed] [Google Scholar]
- 4.Wright E O, Hachen D, Costello C.et al The American class structure. Am Sociol Rev 198247709–726. [Google Scholar]
- 5.Bosma H, Appels A, Sturmans F.et al Differences in mortality and coronary heart disease between Lithuania and The Netherlands: results from the WHO Kaunas‐Rotterdam Intervention Study (KRIS). Int J Epidemiol 19942312–19. [DOI] [PubMed] [Google Scholar]
- 6.Wohlfarth T. Socioeconomic inequality and psychopathology: are socioeconomic status and social class interchangeable? Soc Sci Med 199745399–410. [DOI] [PubMed] [Google Scholar]
- 7.Coleman J S.The foundations of social theory. Cambridge: Belknap, 1990
- 8.Liberatos P, Link B G, Kelsey J L. The measurement of social class in epidemiology. Epidemiol Rev 19881087–121. [DOI] [PubMed] [Google Scholar]
- 9.French M T, Zarkin G A. Racial differences in exposure to on‐the‐job hazards. Am J Public Health 19908089–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Melamed S, Yekutieli D, Froom P.et al Adverse work and environmental conditions predict occupational injuries. The Israeli Cardiovascular Occupational Risk Factors Determination in Israel (CORDIS) Study. Am J Epidemiol 199915018–26. [DOI] [PubMed] [Google Scholar]
- 11.Oh J H, Shin E H. Inequalities in nonfatal work injury: the significance of race, human capital, and occupations. Soc Sci Med 2003572173–2182. [DOI] [PubMed] [Google Scholar]
- 12.Laflamme L, Eilert‐Petersson E. Injury risks and socioeconomic groups in different settings. Differences in morbidity between men and between women at working ages. Eur J Public Health 200111309–313. [DOI] [PubMed] [Google Scholar]
- 13.Craig B N, Congleton J J, Kerk C J.et al A prospective field study of the relationship of potential occupational risk factors with occupational injury/illness. AIHA J 200364376–387. [DOI] [PubMed] [Google Scholar]
- 14.Bureau of Labor Statistics Characteristics of injuries and illnesses resulting in absence from work. Washington, DC: US Government Printing Office, 1996
- 15.Bureau of Labor Statistics Lost‐working injuries: characteristics and resulting time away from work, 1995. Washington, DC: US Government Printing Office, 1997
- 16.Salminen S, Kivimaki M, Elovainio M.et al Stress factors predicting injuries of hospital personnel. Am J Ind Med 20034432–36. [DOI] [PubMed] [Google Scholar]
- 17.Hofmann D A, Stetzer A. A cross‐level investigation of factors influencing unsafe behaviors and accident. Pers Psychol 199649307–339. [Google Scholar]
- 18.Kirschenbaum A, Oigenblick L, Goldberg A I. Well being, work environment and work accidents. Soc Sci Med 200050631–639. [DOI] [PubMed] [Google Scholar]
- 19.Felknor S A, Aday L A, Burau K D.et al Safety climate and its association with injuries and safety practices in public hospitals in Costa Rica. Int J Occup Environ Health 2000618–25. [DOI] [PubMed] [Google Scholar]
- 20.Horwitz I B, McCall B P. The impact of shift work on the risk and severity of injuries for hospital employees: an analysis using Oregon workers' compensation data. Occup Med (Lond) 200454556–563. [DOI] [PubMed] [Google Scholar]
- 21.Hoyos C G, Ruppert F. Safety diagnosis in industrial work settings: the safety diagnosis questionnaire. J Safety Res 199526107–117. [Google Scholar]
- 22.Garavan T N, O'Brien F. An investigation into the relationship between safety climate and safety behaviors in Irish organizations. Ir J Manage 200122141–170. [Google Scholar]
- 23.Leigh J P. Education, working conditions, and workers' health. Soc Sci J 19832099–107. [PubMed] [Google Scholar]
- 24.McSweeney K P, Congleton J J, Kerk C J.et al Correlation of recorded injury and illness data with smoking, exercise, and absolute aerobic capacity. Int J Ind Ergon 199924193–200. [Google Scholar]
- 25.Andersson G. Factors important in the genesis and prevention of occupational back pain and disability. J Manipulative Physiol Ther 19921543–46. [PubMed] [Google Scholar]
- 26.Ryan J, Zwerling C, Orav E. Occupational risks associated with cigarette smoking: a prospective study. Am J Public Health 19928229–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jones J, Murphy L R, Steffy B D. Impact of organizational stress management on accident rates and insurance losses: two quasi‐experiments. In: Opatz JP, ed. Health promotion evaluation: measuring the organizational impacts Stevens Point, WI: National Wellness Association, 198765–81.
- 28.Savery L K, Wooden M. The relative influence of life events and hassles on work‐related injuries: some Australian evidence. Hum Relat 199447283–305. [Google Scholar]
- 29.Bureau of Labor Statistics Incidence rates of nonfatal occupational injuries and illnesses by industry and case types. 2002. http://www.bls.gov (accessed 23 Feb 2007)
- 30.Bureau of Labor Statistics Employed persons by detailed industry, sex, race, and Hispanic or Latino ethnicity, 2003. http://www.bls.gov (accessed 23 Feb 2007)
- 31.Slatin C, Galizzi M, Melillo K D.et al Conducting interdisciplinary research to promote healthy and safe employment in health care: promises and pitfalls. Public Health Rep 200411960–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Research Council The changing nature of work: implications for occupational analysis. Washington, DC: National Academy Press, 1999
- 33.National O*NET Consortium, North Carolina Employment Security Commission O*NET 98 Data Dictionary, Release 1.0. Raleigh, NC
- 34.Karasek R A.Job Content Questionnaire and user's guide. Los Angeles: University of Southern California, 1985
- 35.Siegrist J. Adverse health effects of high‐effort/low‐reward conditions. J Occup Health Psychol 1996127–41. [DOI] [PubMed] [Google Scholar]
- 36.Wilkinson W E, Salazar M K, Uhl J E.et al Occupational injuries: a study of health care workers at a northwestern health science center and teaching hospital. AAOHN J 199240287–293. [PubMed] [Google Scholar]
- 37.Goldman R H, Jarrard M R, Kim R.et al Prioritizing back injury risk in hospital employees: application and comparison of different injury rates. J Occup Environ Med 200042645–652. [DOI] [PubMed] [Google Scholar]
- 38.Simpson C L, Severson R K. Risk of injury in African American hospital workers J Occup Environ Med 2000421035–1040. [DOI] [PubMed] [Google Scholar]
- 39.Warner M, Barnes P M, Fingergut L A.et al Injury and poisoning episodes and conditions; National Health Interview Survey, 1997. Vital Health Stat 10 20002021–38. [PubMed] [Google Scholar]
- 40.Henry K, Campbell S. Needlestick/sharps injuries and HIV exposure among health care workers. National estimates based on a survey of U.S. hospitals. Minn Med 19957841–44. [PubMed] [Google Scholar]
- 41.Benitez Rodriguez E, Ruiz Moruno A J, Cordoba Dona J A.et al Underreporting of percutaneous exposure accidents in a teaching hospital in Spain. Clin Perform Qual Health Care 1999788–91. [PubMed] [Google Scholar]
- 42.Health Forum, LLC The AHA annual surveys: 1993 to 2002. Chicago: American Hospital Association, 2002
- 43.Azaroff L, Levenstein C, Wegman D H. Occupational injury and illness surveillance: conceptual filters explain underreporting. Am J Public Health 2002921421–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stephenson J. Good workers may get bad breaks on health. JAMA 19952731643–1646. [PubMed] [Google Scholar]
- 45.Fricker M. California workers try to secure benefits: debilitating delays. Insults to injury: workers' comp series, http://www.pressdemo.com/workerscomp (accessed 22 Feb 2007)
- 46.Herbert R, Janeway K, Schecter C. Carpal tunnel syndrome and workers' compensation in New York State. Am J Ind Med 19991967–74. [DOI] [PubMed] [Google Scholar]
- 47.Meister J S. The health of migrant farm workers. Occup Med 19916503–518. [PubMed] [Google Scholar]
- 48.Weddle M G. Reporting occupational injuries: the first step. J Safety Res 199627217–223. [Google Scholar]
- 49.Doebbeling B N, Vaughn T E, McCoy K D.et al Percutaneous injury, blood exposure, and adherence to standard precautions: are hospital‐based health care providers still at risk? Clin Infect Dis 2003371006–1013. [DOI] [PubMed] [Google Scholar]
- 50.Kauppinen T P, Mutanen P O, Seitsamo J T. Magnitude of misclassification bias when using a job‐exposure matrix. Scand J Work Environ Health 199218105–112. [DOI] [PubMed] [Google Scholar]
- 51.Hemingway M A, Smith C S. Organizational climate and occupational stressors as predictors of withdrawal behaviours and injuries in nurses. J Occup Organ Psychol 199972285–299. [Google Scholar]
- 52.Gershon R R, Karkashian C D, Grosch J W.et al Hospital safety climate and its relationship with safe work practices and workplace exposure incidents. Am J Infect Control 200028211–221. [DOI] [PubMed] [Google Scholar]
- 53.Marmot M G, Bosma H, Hemingway H.et al Contribution of job control and other risk factors to social variations in coronary heart disease incidence. Lancet 1997350235–239. [DOI] [PubMed] [Google Scholar]
- 54.Bobak M, Hertzman C, Skodova Z.et al Association between psychosocial factors at work and nonfatal myocardial infarction in a population‐based case‐control study in Czech men. Epidemiology 1998943–47. [PubMed] [Google Scholar]