Abstract
We developed chimeric Sindbis (SINV)/Eastern equine encephalitis (EEEV) viruses and investigated their potential for use as live virus vaccines against EEEV. One vaccine candidate contained structural protein genes from a typical North American EEEV strain, while the other had structural proteins from a naturally attenuated Brazilian isolate. Both chimeric viruses replicated efficiently in mammalian and mosquito cell cultures and were highly attenuated in mice. Vaccinated mice did not develop detectable disease or viremia, but developed high titers of neutralizing antibodies. Upon challenge with EEEV, mice vaccinated with >104PFU of the chimeric viruses were completely protected from disease. These findings support the potential use of these SIN/EEEV chimeras as safe and effective vaccines.
Keywords: Encephalitis, vaccine, alphavirus
Introduction
Eastern equine encephalitis virus (EEEV), a member of the family Togaviridae, genus Alphavirus, is an important mosquito-borne human and veterinary pathogen in the Americas [1–3]. The virus contains a single strand, positive-sense RNA genome of approximately 11.7 kb. Four nonstructural proteins (nsP1-4), encoded in the 5’ two-thirds of the genome, are required for viral replication and polyprotein processing. A structural protein gene polyprotein is translated from the subgenomic (26S) RNA and cleaved into the 3 major structural proteins (capsid, and envelope glycoproteins E2 and E1) that are involved in receptor recognition, virus attachment and penetration, membrane fusion and virion assembly [4].
Using antigenic and genetic analyses, EEEV virus has been classified into one North American (NA) and 3 South American (SA) subtypes [5]. The NA subtype consists of isolates from the eastern United States, Canada, northern Mexico and islands of the Caribbean, while the 3 SA subtypes include isolates from South and Central America, ranging from Guatemala to northern Argentina. The NA strains are genetically conserved, uniformly virulent and cause severe encephalitis in both human and equines, with mortality rates of 30–80% in apparent human and 90–95% in equine cases [1, 2, 6]. Human EEE exhibits nonspecific clinical signs and symptoms that usually begin with high fever, headache, dizziness, and vomiting, which can sometimes progress to severe encephalitis by the second day of disease with coma and paralysis. Up to 30% of patients, especially children who survive the infection, have life-threatening neurologic sequelae and often require costly, permanent institutional care [7]. Similar to NA strains of EEEV, SA strains regularly cause fatal equine infections. However, human EEE is rare in Latin America despite evidence of widespread virus circulation. Epidemiologic studies suggest that SA strains are less virulent and/or infectious for humans [8], possibly due to greater sensitivity to human interferons [9]. Most NA and SA EEEV strains are lethal to mice, which develop disease pattern similar to those in humans and horses. However, strain BeAr436087 isolated from Brazil in 1985, is completely attenuated in adult mice by either subcutaneous (SC) or intracranial (IC) inoculation, and protects mice against subsequent challenge by virulent NA strains (PVA, SCW, unpublished).
Eastern equine encephalitis virus is a zoonotic, mosquito-borne virus that circulates among passerine birds in swamp habitats of NA. Aside from avoidance of enzootic foci, there is no way to prevent infection or to treat EEE. No antiviral drug is available to treat EEEV infections, and no licensed human vaccine is available. Formalin-inactivated vaccines have been produced from wild-type, NA strains of EEEV [10], and used to vaccinate humans [11], equids, and other domestic and wild animals affected by the virus such as pheasants, whooping cranes, pigs, and emus [12–17]. However, immunity is weak and short-lived, and residual live virus can cause severe disease, as exemplified in a vaccinated horse in California [18]. Two doses of the formalin-inactivated vaccine are typically recommended each year in locations with year-round enzootic circulation.
The rationale for the development of chimeric alphavirus vaccines included: 1) the consistently attenuated phenotype of all chimeric alphaviruses described to date, including recombinants between 2 highly virulent viruses [19–22], suggesting that their recombinant nature confers an attenuation phenotype, rather than point mutations that are subject to high rates of reversion. The latter may be explain the residual reactogenicity of alphavirus vaccines that rely on point mutations that accumulate during cell passages, including attenuated strains of Chikungunya virus [23] and VEEV [24]; 2) the success of the chimeric flavivirus vaccines also argues for this approach [25]; 3) live-attenuated vaccines have advantages over other approaches (e.g. subunit and inactivated vaccines) of rapid and long-lasting immunity, including both cellular and humoral. In the present study, two recombinant SIN/EEEV strains were developed and investigated as live vaccine candidates for protection against EEE. The nonstructural protein genes and cis-acting RNA genome elements were derived from wild-type SINV strain AR339 [26], and the structural protein genes were derived from either north American EEEV strain FL93-939, or from the naturally murine-attenuated SA strain BeAr436087. These recombinant vaccine candidates were evaluated in mice to assess immunogenicity, protection against EEEV challenge, and attenuation. Our findings suggest that both recombinant SINV/EEEV strains are safe and efficacious.
Materials and Methods
Cells
Baby hamster kidney (BHK-21) and African green monkey (Vero) cells were purchased from the American Type Culture Collection (Bethesda, MD) and grown at 37°C in Eagles minimal essential medium (MEM) with 10% fetal bovine serum (FBS) and 0.05 mg/ml of gentamycin sulfate (Invitrogen, Carlsbad, CA). The Aedes albopictus mosquito cell line C7/10 was maintained in MEM at 32°C with 10% FBS and 10% tryptose phosphate broth.
Construction of recombinant SIN/EEEV plasmids
Chimeric alphavirus infectious cDNA clones were derived SINV strain AR339 [26], and EEEV strain FL93-939 (NA), a 1993 Florida mosquito isolate passed once in Vero cells, or BeAr436087 (SA), a 1985 Brazilian mosquito isolate passed once in C6/36 mosquito cells and once in newborn mice [9]. The nonstructural protein genes as well as the cis-acting RNA elements were derived from SINV, and the structural protein genes were derived from EEEV. The 3’ untranslated region contained 335 nucleotide sequences derived from SINV as well as the poly (A) tail, followed by either a Pvu I restriction site for SIN/NAEEEV, or an Xho I site for SIN/SAEEEV. Because the EEEV promoter functions less efficiently with SINV replication proteins [27], the SINV subgenomic promoter was included, followed immediately downstream by the 5’ untranslated sequence of the EEEV subgenomic region. Maps and sequences of the plasmids are available from the authors upon request.
In vitro transcription, transfection and production of infectious virus
Plasmid DNAs of the SIN/NAEEEV and SIN/SAEEEV chimeras were linearized by restriction endonuclease digestion with Pvu I or XhoI, respectively, and purified by phenol-chloroform extraction and ethanol precipitation. RNAs were synthesized in vitro using the mMESSAGE mMACHINE SP6 kit (Ambion, Austin, Texas) and examined on an ethidium bromide-containing agarose gel to determine yield and integrity of the transcripts. The RNAs were transfected into BHK-21 cells by electroporation. The V3526 VEEV strain was rescued from an infectious cDNA clone as described previously . The rescued viruses were collected following the development of cytopathic effects (CPE) at approximately 24 h post-transfection. Virus titers were determined by plaque assay on Vero cells.
Virus replication in cell culture
Replication kinetics of SINV and the chimeric viruses were compared in Vero and C7/10 cells. Confluent monolayers grown in 12-well plates were infected at a multiplicity of infection (MOI) of 1 PFU/cell and incubated at 37°C for Vero cells and 32°C for C7/10 cells. Infections were done in triplicate for statistical analysis. After 1 h of incubation, the plates were washed with phosphate buffer saline (PBS) and 2 ml of EMEM with 2% FBS were added. At selected times postinfection, cell culture medium was collected and replaced with fresh medium. Virus titers in the harvested media were determined by plaque assay on Vero cells [28].
Mouse infections
Six- to 8-week-old female and older pregnant NIH Swiss mice were purchased from Harlan (Indianapolis, IN) and maintained under specific-pathogen-free conditions. Newborn mice were held for 6 days after birth prior to intracerebral infection.
Adult mice were vaccinated SC in the medial thigh in a total volume of 100 μl of PBS. Blood samples were collected from the retroorbital sinus and virus titers were determined by plaque assay. To monitor body temperature, some adult mice were anaesthetized before infection with isofluorane and implanted SC with a pre-programmed telemetry chip (IPTT-300; Bio Medical Data Systems, Inc., Seaford, DE) according manufacturer’s instructions. Mice were monitored for 7–10 days to ensure that trauma, infection, or other reactions to the implanted chips did not affect the infection results. Temperatures and body weights were recorded daily without anesthetization.
As an extremely stringent measurement that can distinguish vaccine strains with differences in virulence, parental viruses [SINV, or EEEV (NA or SA strain)] and the SIN/EEEV chimeras were also inoculated into 6-day-old NIH Swiss mice at a dose of 5.3 log10 PFU by the intracerebral (IC) route. Animals were monitored daily for 28 days for signs of paralysis or ataxia associated with EEE. Two animals per group were sacrificed on days 1 and 2 and virus content in the brains was determined by plaque assay. Intranasal infection of adult mice was done following light anesthetization with isofluorane, followed by instillation of a 10 μl volume per nostril.
Serological assays
Neutralizing antibodies were assayed using 80% plaque reduction neutralization tests (PRNT), and IgG responses were detected using enzyme-linked immunosorbent assays (ELISAs) [28]. For ELISAs, mouse brain antigens of a North American strain of EEEV, provided from the Centers for Disease Control and Prevention in Fort Collins, Colorado, were resuspended in 0.25 ml of water and then diluted 1:2000 in PBS. Then, 100 μl of diluted antigens were added to each well of a NUNC Immuno plate PolySorp 96-well plate (Nalge Nunc International, Rochester, NY) and incubated at 4°C overnight. Plates were washed with wash buffer [phosphate-buffered saline with 0.1% Tween 20 (Sigma)] and blocked with blocking buffer (phosphate-buffered saline, 0.1% Tween 20, 5% nonfat dry milk). Following the addition of experimental mouse sera at a 1:100 dilution, IgG was detected with horseradish peroxidase-conjugated goat anti-mouse IgG (Kirkegaard & Perry Laboratories Inc., Gaithersburg, MD). Sera yielding absorbance values that exceeded the mean values of negative control sera by more than 2 standard deviations (0.1 ± 0.02) were considered IgG positive for EEEV.
Results
Replication of chimeric viruses in cell cultures
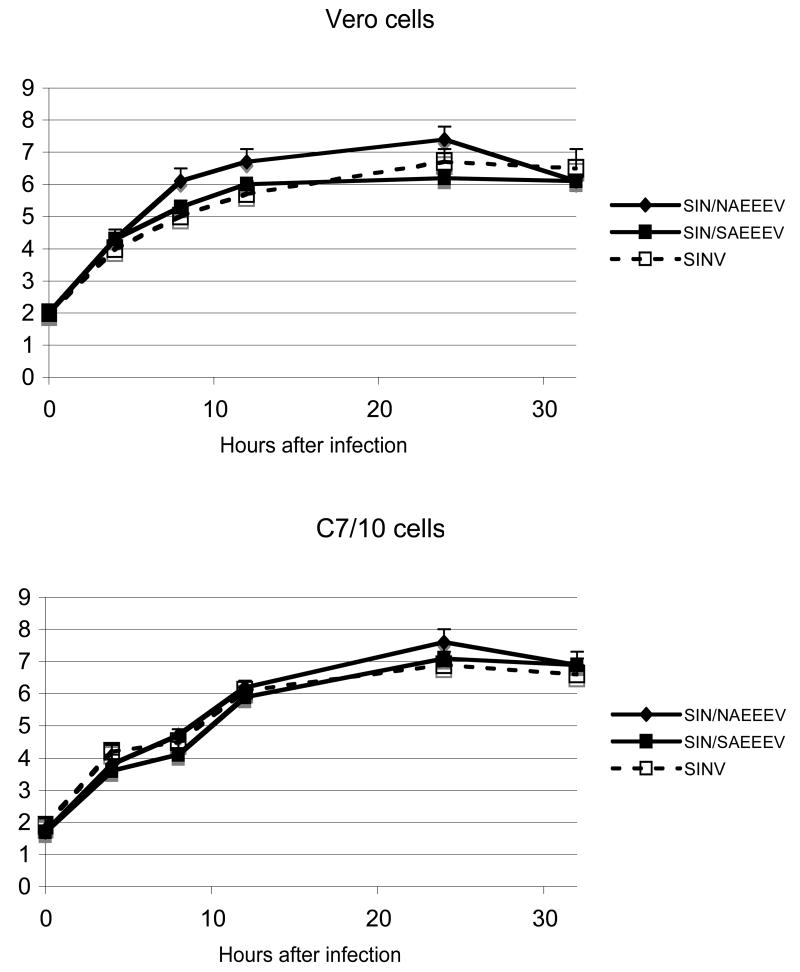
The overall design of chimeric SIN/EEEV cDNA infectious clones was essentially the same as that described previously for SIN/Venezuelan equine encephalitis virus (VEEV) chimeras [19, 20]. The chimera including the NA EEEV structural protein genes was designated SIN/NAEEEV, while that containing the SA EEEV structural protein genes was designated SIN/SAEEEV. Specific activities of the transcribed RNAs determined by infectious center assays were similar to those of other alphavirus chimeric clones (data not shown)[19]. Parental and chimeric viruses recovered from BHK cells after RNA electroporation were tested for replication in Vero (an approved mammalian vaccine production substrate) and C7/10 mosquito cells at a MOI of 1. High yields of both chimeric viruses were produced in both cell types, similar to those of the parental SINV (Fig. 1); unlike the SIN/VEEV chimeras described previously [19, 20], SIN/EEEV derived from electroporated cells produced large plaques on BHK and Vero cells and did not require further passages to replicate efficiently. The SIN/NAEEEV chimeric virus replicated to slightly higher titers than SIN/SAEEEV in Vero cells, with peak titers about 10-fold higher (Fig. 1); however, these differences were not significant (p>0.05, ANOVA). No cytopathic effects (CPE) were observed after infection of C7/10 cells, while all Vero cells exhibited CPE with all viruses by 24 h postinfection.
Fig. 1.
Replication of chimeric SIN/EEEV strains and Sindbis virus parent in Vero (37°C) and C7/10 mosquito cells (32°C). SIN/NAEEEV - chimera including the North American EEEV structural protein genes; SIN/SAEEEV - chimera containing the South American structural genes. Cells were infected at a MOI of 1 PFU/cell for one h, washed three times with PBS, then viral titers in the culture medium were determined by plaque assay at selected times after infection. Bars indicate standard deviations for triplicate infections.
Attenuation and immunogenicity
To assess attenuation and safety of the SIN/EEEV chimeras, 8-week-old, female NIH Swiss mice were inoculated SC with either SIN/NAEEEV or SIN/SAEEEV at doses of 3.7–5.8 log10 PFU (Tables 1–2). Controls were sham-infected with PFU were determined on days 1 and 2 PBS. Viremia levels in mice that received ca. 4.7–5.8 log10 post-inoculation, and no infectious virus was detected in the serum by plaque assay, where the limit of detection was 8 PFU/ml. None of the animals infected at any dose exhibited any signs of disease. Four weeks after immunization, animal sera were collected to measure antibody responses. Antibody titers measured by PRNT and ELISA showed a dose response to SIN/NAEEEV, with the highest mean titers following immunization with 5.7 log10 PFU. At this dose, 80% mean PRNT titers were 1:320-1:1028; (Table 1) when tested against the NA EEEV strain. In addition, 8 of 10 mice immunized with the highest SIN/NAEEEV dose had cross-reactive neutralizing antibodies against the SA EEEV strain (mean PRNT titers 1:20-1:60). After the lowest SIN/NAEEEV dose (3.7 log10 PFU), 3 of 10 mice had undetectable homologous neutralizing antibody titers (<1:20), but 1 of these 3 had a positive IgG titer (OD of 0.20) by ELISA (Table 1).
Table 1.
Neutralizing antibodies and IgG in female NIH Swiss mice four weeks after SIN/NAEEEV or SIN/SAEEEV immunization
| Vaccine strain | Vaccine dose (log10PFU) | Mean PRNT titer against NAEEEV±SD* | Number Positive /total | Mean PRNT titer against SAEEEV±SD* | Number Positive /total | OD of IgG ELISA±SD** |
|---|---|---|---|---|---|---|
| SIN/NAEEEV | 3.7 | 125±39 | 7/10 | 20±0 | 4/10 | 0.9±0.7 |
| 4.7 | 226±168 | 10/10 | 20±0 | 4/10 | 1.2±0.3 | |
| 5.7 | 660±289 | 10/10 | 50 ±48 | 8/10 | 1.5±0.4 | |
| SIN/SAEEEV | 3.8 | 20±0 | 5/10 | 28±19 | 10/10 | 1.2±0.3 |
| 4.8 | 28±10 | 8/10 | 56±20 | 10/10 | 1.3±0.3 | |
| 5.8 | 36±17 | 10/10 | 308±210 | 10/10 | 1.3±0.2 |
Reciprocal of highest positive (80% plaque reduction) serum dilution
Negative control sera generated a mean absorbance of 0.18±0.02
Table 2.
Viremia and viral titers in organs in vaccinated mice after challenge with EEEV
| Organ | Virus titer day 3 after intranasal challenge (log10 PFU/ml or g)
|
Virus titer day 3 after intraperitoneal challenge (log10 PFU/ml or g)
|
||
|---|---|---|---|---|
| Vaccine | PBS | SIN/EEEV | PBS | SIN/EEEV |
| Serum | 3.6±0.1 | <0.9 | ND* | <0.9 |
| Brain | 9.3±0.0 | <0.9 | 9.0±0.5 | <0.9 |
| Lung | 3.2±0.1 | <0.9 | 5.0±1.0 | <0.9 |
| Heart | 3.1±0.1 | <0.9 | 5.6±0.2 | <0.9 |
| Liver | 2.9±0.5 | <0.9 | 3.7±0.7 | <0.9 |
| Spleen | 4.3±0.0 | <0.9 | 4.8±0.1 | <0.9 |
| Kidney | 2.0±0.2 | <0.9 | 3.9±0.1 | <0.9 |
All mice immunized with SIN/SAEEEV developed neutralizing antibodies, with the highest mean titer again found in the cohort that received the highest vaccine dose of 5.8 log10 PFU (Table 2). At this vaccine dose, 80% PRNT titers against SA EEEV were 40-640. The SIN/SAEEEV vaccine appeared to be less immunogenic than SIN/NAEEEV chimera, with mean PRNT titers consistently lower against homologous SA EEEV. However, SIN/SAEEEV appeared to be more cross-immunogenic, with 50% of the low-dose cohort (3.8 log10 PFU), 80% of the medium-dose cohort (4.8 log10 PFU), and all of the high dose animals (5.8 log10 PFU) producing anti-NA EEEV antibodies (Table 2).
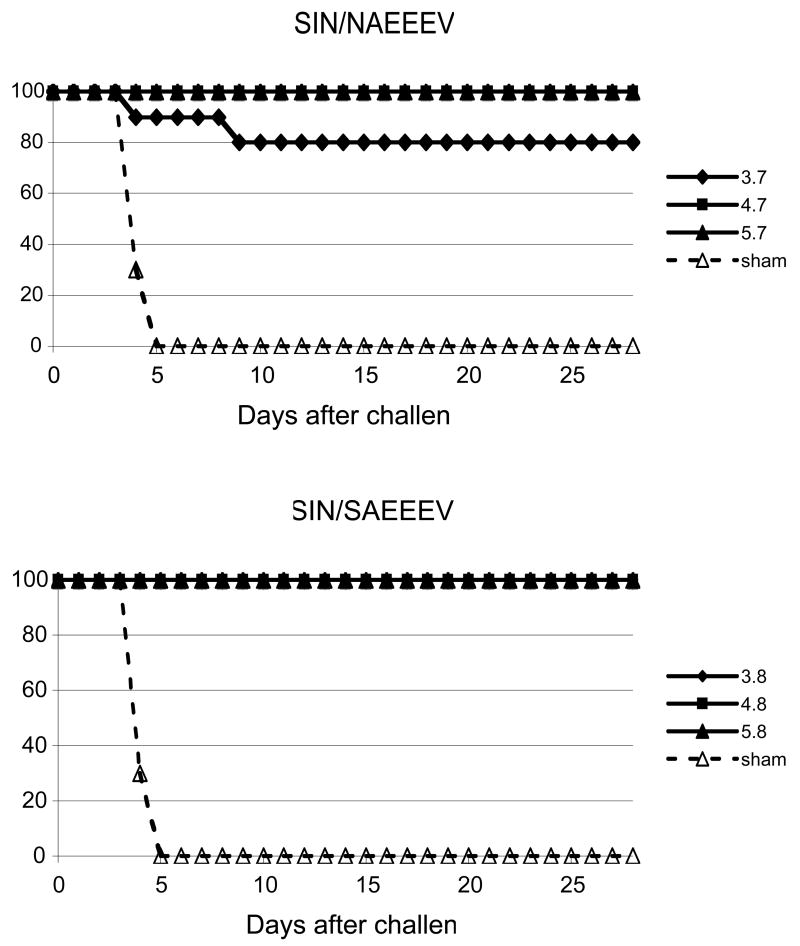
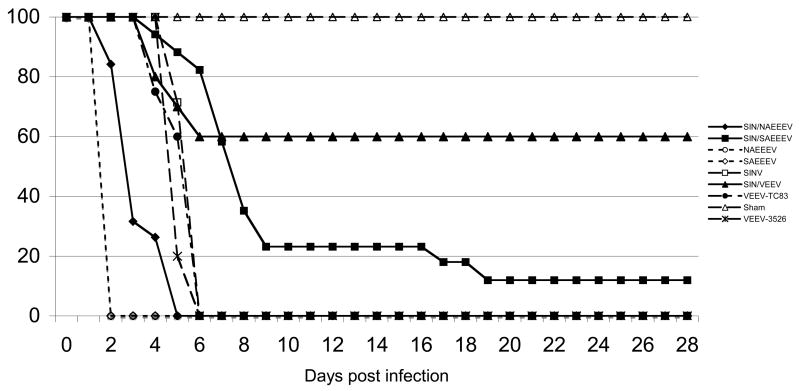
Protection against EEEV challenge
Because the SA EEEV strain is avirulent for mice (PVA, SCW, unpublished), efficacy challenges were conducted only with the NA strain FL93-939, at 28 days after vaccination. With the exception of 2 mice vaccinated with 3.7 log10 PFU of SIN/NAEEEV that died 4 and 9 days after intraperitoneal (IP) challenge with 6 log10 PFU, all other immunized mice survived (Fig. 2); in contrast, all sham-vaccinated mice developed clinical signs of encephalitis by day 3 or 4 after challenge, and then died by day 4 or 5. Consistent with these clinical outcomes, all vaccinated mice with detectable IgG antibodies survived (Table 2), while the 2 animals that were vaccinated with low-dose SIN/NAEEEV and did not develop detectable IgG antibodies succumbed to EEEV challenge.
Fig. 2.
Survival following vaccination and challenge. Eight-week-old, female NIH Swiss mice were immunized SC by SIN/NAEEEV or SIN/SAEEEV with the indicated doses (expressed as log10 PFU). Four weeks after immunization, mice were challenged IP with 106 PFU of EEEV strain FL-93-939, and mortality was recorded.
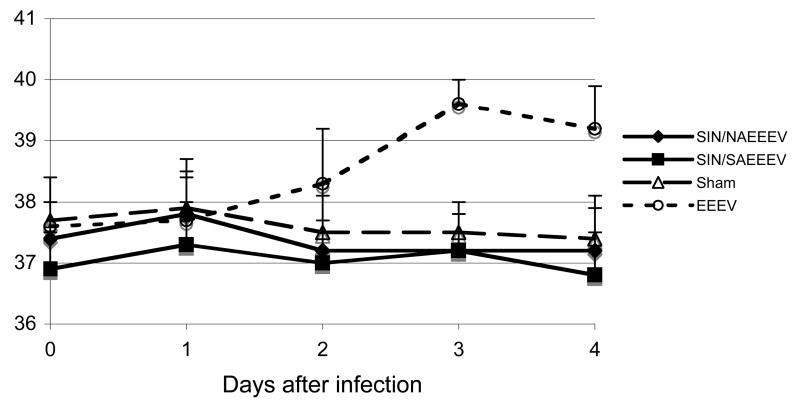
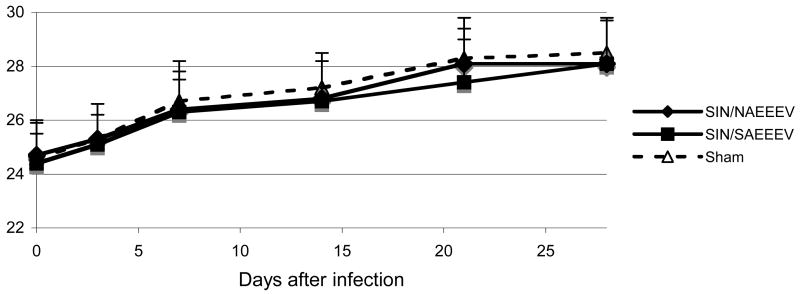
Body temperature and weight changes associated with vaccination and challenge
To monitor with greater sensitivity the potential clinical signs related to vaccination or challenge, randomly assigned cohorts of weight-matched, seven to 8-week-old mice were implanted with pre-programmed telemetry chips to measure body temperature before and after SC vaccination with 5.3 log10 PFU of SIN/NAEEEV or 5.0 log10 PFU of SIN/SAEEEV. No febrile response was detected after vaccination or sham-vaccination (PBS), and all body temperatures remained within the normal range (35.5–38°C). However, following infection with NA EEEV strain FL93-939 (positive control), mice exhibited a significant increase in mean body temperature beginning on day 3 post-infection (39.6°C±0.4, P<0.05, ANOVA with Tukey-Kramer multiple comparisons test) with a continued rise in temperature on day 4 (Fig. 3). Body weight was also recorded on days 0, 3 and weekly thereafter to day 28 after vaccination (Fig. 4). All mice gained weight throughout the period, and there were no significant differences (P>0.05) between SIN/EEEV-vaccinated cohorts compared to the sham-vaccinated animals (Fig. 4).
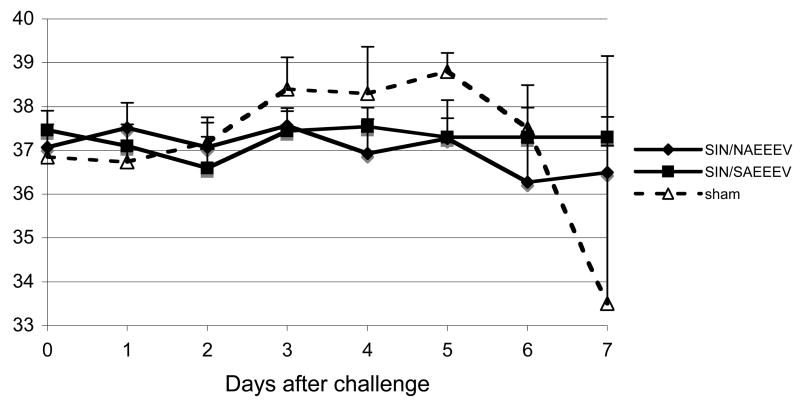
Fig. 3.
Body temperatures of 8-week-old, female NIH Swiss mice after vaccination with SIN/NAEEEV, SIN/SAEEEV or after sham-vaccination with PBS. Infection with North American EEEV was included as a positive control.
Fig. 4.
Body weights of 8-week-old, female NIH Swiss mice after vaccination with SIN/NAEEEV, SIN/SAEEEV or after sham-vaccination with PBS.
We next challenged the immunized mice described above with virulent NA EEEV strain FL93-939 at day 28 after vaccination. Mice were inoculated IP with 5.0 log10 PFU and monitored for 28 days. As in the first study, sham-vaccinated mice developed clinical signs of encephalitis by day 3–4, and all died by day 4 or 5 post-challenge. All of the sham-vaccinated mice showed a febrile response by day 3–4, and exhibited hypothermia 1–2 days before death by day 8 (Fig. 5). In contrast, mice vaccinated with either SIN/NAEEEV or SIN/SAEEEV and then challenged with NA EEEV showed no signs of disease, and none of the chimera-vaccinated mice exhibited a body temperature outside of the normal range (35.5–38°C). All mice that were not sacrificed for virus content studies survived for at least 14 days after challenge, when the experiment was terminated.
Fig. 5.
Body temperatures of vaccinated (SIN/NAEEEV or SIN/SAEEEV) or sham-vaccinated (PBS) female NIH Swiss mice following intraperitoneal challenge with North American EEEV.
Levels of virus replication in immunized mice after challenge
We further examined viremia and virus replication levels in organs of 12-week-old mice previously immunized with SIN/NAEEEV (5.3 log10 PFU) or SIN/SAEEEV (5.0 log10 PFU) and challenged with the NA EEEV strain, either IP (6 log10 PFU) or IN (5.3 log10 PFU). On days 3, 7 and 28 post-challenge, two animals per group were bled, perfused with PBS, sacrificed and their brains, hearts, lungs, livers, spleens, and kidneys were collected for virus titration. As described previously, all body temperatures remained normal, no abnormal clinical signs were observed, and all mice in the SINV/EEEV vaccinated groups survived (data not shown). Regardless of route, all sham-vaccinated mice developed fevers ≥38.3°C beginning on day 3 after challenge, and quickly progressed to encephalitis as indicated by hind limb paralysis. All sham-vaccinated mice died within 5 days of IN challenge, while some survived slightly longer (7–9 days) after IP challenge.
Regardless of route, EEEV replication was not detected in the tissues of SINV/EEEV chimera-vaccinated mice on days 3 (Table 3), 7 or 28 (data not shown) post-challenge. The limit of detection for the plaque assay was 0.9 log10 PFU/ml serum or gram of tissue. In contrast, sham-vaccinated mice developed high virus concentrations in all organs collected on day 3 post-challenge (Table 3) with the highest titers in the brain (≥9 log10 PFU/g). Viremia was detected on day 3 after IN challenge, but not after IP challenge of sham-vaccinated mice. High levels (8.7 log10 PFU/g) of EEEV were also found in the brains of 2 sham-vaccinated mice at 7 days after challenge, with lower virus titers in other organs (data not shown).
Neurovirulence and replication of chimeric vaccine candidates in 6 day-old mice
To use a highly stringent model for neurovirulence, cohorts of twelve 6 day-old NIH Swiss mice were inoculated IC (5 log10 PFU) with either SINV/EEEV chimeras, parental NA EEEV, SA EEEV, or SINV strains, the previously described chimeric SIN/VEEV [20], or the TC-83 [24, 29] or V3526 [30] attenuated VEEV vaccine strain, and monitored for signs of neurologic disease (Fig. 6). Both NA and SA EEEVs were highly neurovirulent, and all animals died within 4 days of infection. The SINV/NAEEEV strain was less virulent compared to the wild-type EEEV parents, and caused death between 2 and 4 days after infection. SINV/SAEEEV was even less virulent, with the majority of mice dying between days 4 and 9 after infection. After day 9, some SINV/SAEEEV survivors developed hind limb paralysis and 2 of these mice died on days 17 and 19 post-infection. The remaining 2 mice also developed signs of disease but recovered and survived until the experiment was terminated on day 28 after infection.
Fig. 6.
Survival of six-day-old mice after intracranial inoculation with 20 μl of PBS containing 5 log10 PFU the EEEV or SINV/EEEV indicated in the legend. The TC-83 attenuated VEEV strain and SIN/VEEV chimeric vaccine candidate strain are included for comparison.
Both the TC-83 and V3526 attenuated VEEV strains killed all mice by day 6, suggesting a virulence intermediate between the SINV/NAEEEV and SINV/SAEEEV strain. The parental SINV strain was also intermediate between SINV/NAEEEV and SINV/SAEEEV, killing all the mice within 5–6 days of infection.
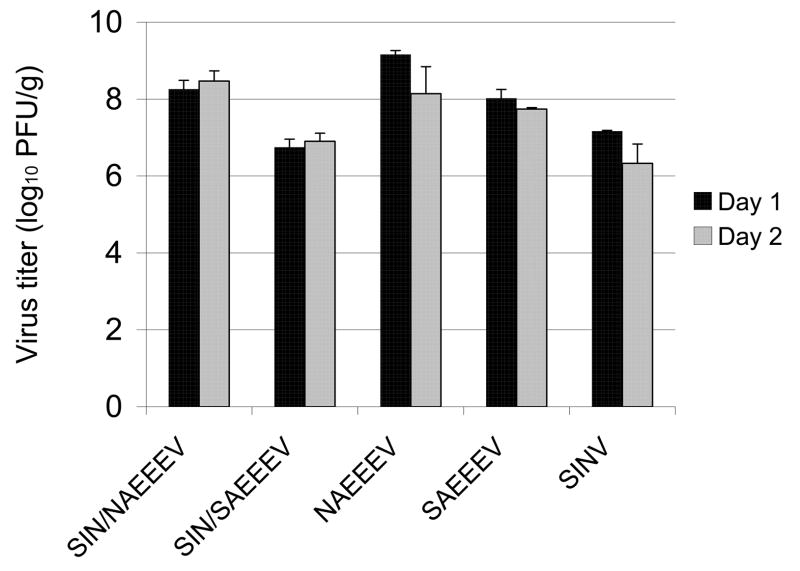
Levels of viral replication in the brains of the 6-day-old mice were quantified by plaque assay on days 1 and 2 after infection (Fig. 7). On day 1, the parental NAEEEV strain replicated to the highest mean titer of 9.2 log10 PFU/g and the mean levels of virus replication of the SIN/EEEV chimeras were 1–1.3 log10 PFU/g lower than their respective parental EEEVs. Wild-type SINV had levels of replication similar to those of SIN/SAEEEV.
Fig. 7.
Mean virus titers in brains of 6 day-old mice, one and 2 days after intracerebral infection with 5 log10 PFU the virus indicated. Two animals were sampled at each time point. Bars indicate the standard deviations.
Discussion
To fill the need for an effective human vaccine against EEEV as well as to develop an improved veterinary vaccine, we developed and evaluated 2 chimeric strains of SIN/EEEV. The rationale for the chimeric approach was based on the previously described SIN/VEEV strains that are highly attenuated and immunogenic for mice [19, 20] as well as a chimeric Western equine encephalitis/EEEV vaccine candidate [22]. Several chimeric flavivirus vaccines have a similar combination of structural proteins of the vaccine target and the nonstructural protein genes of the 17D attenuated Yellow fever vaccine strain [31]. In the present study, both SIN/EEEV strains replicated efficiently in mammalian and mosquito cell cultures without any adaptation to cell cultures. Therefore, commercial scale production should be adequate to generate a large numbers of doses at even the highest vaccination doses tested (5.8 log10 PFU per animal).
Attenuation and Safety
Our initial data indicate that both of the SIN/EEEV vaccine candidate strains are highly attenuated in mice. None of the adult or subadult mice we infected exhibited any signs of neurologic disease, febrile responses, or growth delays as indicated by weight gain. Although the SINV parent virus used to make the chimeras is not pathogenic in adult mice, most strains of EEEV kill 70–100% of mice infected SC, IP, IN or IC [9, 32]. Our data with the highly stringent baby mouse IC model indicate that both chimeric SIN/EEEV vaccines are more attenuated than most wild-type EEEV (although the SA BeAr436087 strain is an exception to this pattern). Based on mean time of survival of IC infected 6-day-old mice, the virulence order of the alphavirus strains we tested, was: NAEEEV > SAEEEV > SIN/NAEEEV > V3526 > TC-83 > SINV > SIN/SAEEEV > SIN/VEEV. Considering the natural attenuation of the SA EEEV strain BeAr436087, the epidemiological evidence that other SA strains are also attenuated for humans [8], and that the SIN/SAEEEV chimera protects mice as well as SIN/NAEEEV against NAEEEV challenge yet is more attenuated, SIN/SAEEEV may be the most promising of the 2 vaccine candidates. Additional studies to determine if strain BeAr436087 is attenuated in other rodent models and equids would be useful to support the rationale for further development of this vaccine candidate.
The NA and SA strains of EEEV used to generate our chimeric vaccine candidates differ overall by ca. 23% in their nucleotide sequences and by ca. 10% in amino acids within the structural protein genes. Therefore, the differences we detected in virulence between the SIN/NAEEEV and SIN/SAEEEV chimeras could be due to any or all of the structural EEEV proteins. Additional genetic manipulations to create chimeras that differ only in individual EEEV structural protein genes or domains would be useful to map these virulence differences. This approach might be helpful for designing additional SIN/EEEV chimeras that express most of the critical antigenic determinants of the NA strain while exhibiting the reduced virulence of the SA strain.
Although our vaccine candidates did not produce detectable viremia in mice, the potential for viremia in other mammalian species needs to be assessed, as well as the ability of the chimeras to infect and be transmitted by potential mosquito vectors. Additional studies are also needed to assess the genetic and phenotypic stability of the chimeric viruses.
Immunogenicity
With vaccination doses greater than 4 log10 PFU of either SIN/EEEV chimeric strain, all mice developed neutralizing antibody titers and were protected against a highly virulent EEEV strain, with no evidence of viremia or disease. Antibody responses to the vaccines appeared to be dose-dependent. Cross-neutralization titers between the 2 vaccines and their parent NA and SA EEEV strains generally differed by ≥ 4-fold, consistent with previous antigenic data indicating these 2 isolates represent EEEV subtypes [5]. However, despite the lower neutralization titers against the NA EEEV strain that were induced by the SIN/SAEEEV compared to the SIN/NAEEEV chimeric strain, the former exhibited complete protection against NA EEEV challenge, even at the lowest vaccination dose of (3.8 log10 PFU per mouse). Additional studies are eventually needed using longer-lived nonhuman primate models to determine the duration of immunity and to assess the possible role of interference in sequential immunizations with SINV-based chimeric vaccines (e.g. SIN/VEEV followed by SIN/EEEV). Experiments to test for interference are not possible with short-lived rodents because VEEV and EEEV on their own induce cross-protective immunity for at least several months [8] and the structural proteins are probably responsible for most of this immunity. However, studies of vaccinees who receive the TC-83 attenuated strain of VEEV [29] as well as seroprevalence data from VEEV-endemic locations [33] suggest that homologous immunity induced by live alphaviruses is very long-lived.
In summary, we have developed 2 chimeric SIN/EEEV vaccine candidates that show in mice promise as effective human and veterinary vaccines against EEEV. Further studies will need to address the safety and efficacy in other animal species, mosquito transmissibility and stability of attenuation. Because of the existing market in the U.S. and the larger number of natural equine than human EEE cases, these new vaccine candidates may have their greatest potential impact on veterinary health.
Acknowledgments
We thank Anna Grund and Melinda Kelley for assistance with the implantation of telemetry chips and transferring temperature data from mice, and Eric Fokam for help with serological assays. Nancy Davis and Robert Johnston kindly provided the V3526 cDNA clone. This work was supported by a grant from NIAID through the Western Regional Center of Excellence for Biodefense and Emerging Infectious Diseases Research, NIH grant number U54 AI057156. PVA and APA were supported by the James W. McLaughlin fellowship fund. SP was supported by NIH K08 grant no. AI059491.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Weaver SC. Eastern equine encephalitis. In: Service MW, editor. The Encyclopedia of Arthropod-transmitted Infections. Wallingford, UK: CAB International; 2001. pp. 151–59. [Google Scholar]
- 2.Weaver SC, Tesh RB, Shope RE. Alphavirus infections. In: Guerrant RI, Walker DH, Weller PF, editors. Tropical Infectious Diseases Principles, Pathogens and Practice. Philadelphia: Churchill Livingstone; 1999. pp. 1281–87. [Google Scholar]
- 3.Griffin DE. Alphaviruses. In: Knipe DM, Howley PM, editors. Fields' Virology. 4. New York: Lippincott, Williams and Wilkins; 2001. pp. 917–62. [Google Scholar]
- 4.Schlesinger S, Schlesinger MJ. Togaviridae: The viruses and their replication. In: Knipe DM, Howley PM, editors. Fields' Virology. 4. New York: Lippincott, Williams and Wilkins; 2001. pp. 895–916. [Google Scholar]
- 5.Brault AC, Powers AM, Chavez CL, Lopez RN, Cachon MF, Gutierrez LF, et al. Genetic and antigenic diversity among eastern equine encephalitis viruses from North, Central, and South America. Am J Trop Med Hyg. 1999;61(4):579–86. doi: 10.4269/ajtmh.1999.61.579. [DOI] [PubMed] [Google Scholar]
- 6.Tsai TF, Weaver SC, Monath TP. Alphaviruses. In: Richman DD, Whitley RJ, Hayden FG, editors. Clinical Virology. Washington, D.C.: ASM Press; 2002. pp. 1177–210. [Google Scholar]
- 7.Villari P, Spielman A, Komar N, McDowell M, Timperi RJ. The economic burden imposed by a residual case of eastern encephalitis. Am J Trop Med Hyg. 1995;52(1):8–13. doi: 10.4269/ajtmh.1995.52.8. [DOI] [PubMed] [Google Scholar]
- 8.Aguilar PV, Robich RM, Turell MJ, O'Guinn ML, Klein TA, Huaman A, et al. Endemic eastern equine encephalitis in the Amazon region of Peru. Am J Trop Med Hyg. 2007;76(2):293–8. [PubMed] [Google Scholar]
- 9.Aguilar PV, Paessler S, Carrara AS, Baron S, Poast J, Wang E, et al. Variation in interferon sensitivity and induction among strains of eastern equine encephalitis virus. J Virol. 2005;79(17):11300–10. doi: 10.1128/JVI.79.17.11300-11310.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maire LF, 3rd, McKinney RW, Cole FE., Jr An inactivated eastern equine encephalomyelitis vaccine propagated in chick-embryo cell culture. I. Production and testing. Am J Trop Med Hyg. 1970;19(1):119–22. doi: 10.4269/ajtmh.1970.19.119. [DOI] [PubMed] [Google Scholar]
- 11.Bartelloni PJ, McKinney RW, Duffy TP, Cole FE., Jr An inactivated eastern equine encephalomyelitis vaccine propagated in chick-embryo cell culture. II. Clinical and serologic responses in man. Am J Trop Med Hyg. 1970;19(1):123–6. doi: 10.4269/ajtmh.1970.19.123. [DOI] [PubMed] [Google Scholar]
- 12.Tengelsen LA, Bowen RA, Royals MA, Campbell GL, Komar N, Craven RB. Response to and efficacy of vaccination against eastern equine encephalomyelitis virus in emus. J Am Vet Med Assoc. 2001;218(9):1469–73. doi: 10.2460/javma.2001.218.1469. [DOI] [PubMed] [Google Scholar]
- 13.Jochim MM, Barber TL. Immune response of horses after simultaneous or sequential vaccination against eastern, western, and Venezuelan equine encephalomyelitis. J Am Vet Med Assoc. 1974;165(7):621–5. [PubMed] [Google Scholar]
- 14.Snoeyenbos GH, Weinack OM, Rosenau BJ. Immunization of pheasants for Eastern encephalitis. Avian Dis. 1978;22(3):386–90. [PubMed] [Google Scholar]
- 15.Clark GG, Dein FJ, Crabbs CL, Carpenter JW, Watts DM. Antibody response of sandhill and whooping cranes to an eastern equine encephalitis virus vaccine. J Wildl Dis. 1987;23(4):539–44. doi: 10.7589/0090-3558-23.4.539. [DOI] [PubMed] [Google Scholar]
- 16.Elvinger F, Baldwin CA, Liggett AD, Tang KN, Dove CR. Protection of pigs by vaccination of pregnant sows against eastern equine encephalomyelitis virus. Vet Microbiol. 1996;51(3–4):229–39. doi: 10.1016/0378-1135(96)00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Olsen GH, Turell MJ, Pagac BB. Efficacy of eastern equine encephalitis immunization in whooping cranes. J Wildl Dis. 1997;33(2):312–5. doi: 10.7589/0090-3558-33.2.312. [DOI] [PubMed] [Google Scholar]
- 18.Franklin RP, Kinde H, Jay MT, Kramer LD, Green EG, Chiles RE, et al. Eastern equine encephalomyelitis virus infection in a horse from California. Emerg Infect Dis. 2002;8(3):283–8. doi: 10.3201/eid0803.010199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paessler S, Fayzulin RZ, Anishchenko M, Greene IP, Weaver SC, Frolov I. Recombinant Sindbis/Venezuelan equine encephalitis virus is highly attenuated and immunogenic. J Virol. 2003;77(17):9278–86. doi: 10.1128/JVI.77.17.9278-9286.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Paessler S, Ni H, Petrakova O, Fayzulin RZ, Yun N, Anishchenko M, et al. Replication and clearance of Venezuelan equine encephalitis virus from the brains of animals vaccinated with chimeric SIN/VEE viruses. J Virol. 2006;80(6):2784–96. doi: 10.1128/JVI.80.6.2784-2796.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kuhn RJ, Griffin DE, Owen KE, Niesters HG, Strauss JH. Chimeric Sindbis-Ross River viruses to study interactions between alphavirus nonstructural and structural regions. Journal of Virology. 1996;70(11):7900–9. doi: 10.1128/jvi.70.11.7900-7909.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schoepp RJ, Smith JF, Parker MD. Recombinant chimeric western and eastern equine encephalitis viruses as potential vaccine candidates. Virology. 2002;302(2):299–309. doi: 10.1006/viro.2002.1677. [DOI] [PubMed] [Google Scholar]
- 23.Edelman R, Tacket CO, Wasserman SS, Bodison SA, Perry JG, Mangiafico JA. Phase II safety and immunogenicity study of live chikungunya virus vaccine TSI-GSD-218. Am J Trop Med Hyg. 2000;62(6):681–5. doi: 10.4269/ajtmh.2000.62.681. [DOI] [PubMed] [Google Scholar]
- 24.Berge TO, Banks IS, Tigertt WD. Attenuation of Venezuelan equine encephalomyelitis virus by in vitro cultivation in guinea pig heart cells. Am J Hyg. 1961;73:209–18. [Google Scholar]
- 25.Monath TP, McCarthy K, Bedford P, Johnson CT, Nichols R, Yoksan S, et al. Clinical proof of principle for ChimeriVax: recombinant live, attenuated vaccines against flavivirus infections. Vaccine. 2002;20(7–8):1004–18. doi: 10.1016/s0264-410x(01)00457-1. [DOI] [PubMed] [Google Scholar]
- 26.McKnight KL, Simpson DA, Lin SC, Knott TA, Polo JM, Pence DF, et al. Deduced consensus sequence of Sindbis virus strain AR339: mutations contained in laboratory strains which affect cell culture and in vivo phenotypes. J Virol. 1996;70(3):1981–9. doi: 10.1128/jvi.70.3.1981-1989.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hertz JM, Huang HV. Utilization of heterologous alphavirus junction sequences as promoters by Sindbis virus. J Virol. 1992;66(2):857–64. doi: 10.1128/jvi.66.2.857-864.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beaty BJ, Calisher CH, Shope RE. Arboviruses. In: Schmidt NJ, Emmons RW, editors. Diagnostic procedures for viral, rickettsial and chlamydial infections. 6. Washington, D. C.: American Public Health Association; 1989. pp. 797–855. [Google Scholar]
- 29.Pittman PR, Makuch RS, Mangiafico JA, Cannon TL, Gibbs PH, Peters CJ. Long-term duration of detectable neutralizing antibodies after administration of live-attenuated VEE vaccine and following booster vaccination with inactivated VEE vaccine. Vaccine. 1996;14(4):337–43. doi: 10.1016/0264-410x(95)00168-z. [DOI] [PubMed] [Google Scholar]
- 30.Davis NL, Brown KW, Greenwald GF, Zajac AJ, Zacny VL, Smith JF, et al. Attenuated mutants of Venezuelan equine encephalitis virus containing lethal mutations in the PE2 cleavage signal combined with a second-site suppressor mutation in E1. Virology. 1995;212(1):102–10. doi: 10.1006/viro.1995.1458. [DOI] [PubMed] [Google Scholar]
- 31.Lai CJ, Monath TP. Chimeric flaviviruses: novel vaccines against dengue fever, tick-borne encephalitis, and Japanese encephalitis. Adv Virus Res. 2003;61:469–509. doi: 10.1016/s0065-3527(03)61013-4. [DOI] [PubMed] [Google Scholar]
- 32.Vogel P, Kell WM, Fritz DL, Parker MD, Schoepp RJ. Early events in the pathogenesis of eastern equine encephalitis virus in mice. Am J Pathol. 2005;166(1):159–71. doi: 10.1016/S0002-9440(10)62241-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Estrada-Franco JG, Navarro-Lopez R, Freier JE, Cordova D, Clements T, Moncayo A, et al. Venezuelan equine encephalitis virus, southern Mexico. Emerg Infect Dis. 2004;10(12):2113–21. doi: 10.3201/eid1012.040393. [DOI] [PMC free article] [PubMed] [Google Scholar]