Abstract
Objective
The authors sought to empirically derive Alcohol Dependence (AD) subtypes based on clinical characteristics using data from a nationally representative epidemiological survey.
Method
A sample of 1,484 respondents to the National Epidemiological Survey on Alcohol and Related Conditions (NESARC) with past-year AD was subjected to latent class analysis in order to identify homogeneous subtypes.
Results
The best fitting model was a five-cluster solution. The largest cluster (Cluster 1: ~31%) was comprised of young adults, who rarely sought help for drinking, had moderately high levels of periodic heavy drinking, relatively low rates of comorbidity, and the lowest rate of multigenerational AD (~ 22%). In contrast, Clusters 4 and 5 (~21% and 9%, respectively) had substantial rates of multigenerational AD (53% and 77%, respectively), had the most severe AD criteria profile, were associated with both comorbid psychiatric and other drug use disorders, lower levels of psychosocial functioning, and had engaged in significant help-seeking. Clusters 2 and 3 (~19% each) had the latest onset, the lowest rates of periodic heavy drinking, medium/low levels of comorbidity, moderate levels of help-seeking, and higher psychosocial functioning.
Conclusion
Five distinct subtypes of AD were derived, distinguishable on the basis of family history, age of AD onset, endorsement of DSM-IV AUD criteria, and the presence of comorbid psychiatric and substance use disorders. These clinically relevant subtypes, derived from the general population, may enhance our understanding of the etiology, treatment, natural history, and prevention of AD and inform the DSM-V research agenda.
1. Introduction
Alcohol Dependence (AD) is a complex, common disorder that arises as the consequence of biological, behavioral, and environmental factors. For more than 60 years, the heterogeneity of individuals with AD has been recognized by both clinicians and researchers. Efforts to classify individuals with AD into subtypes have been motivated by the pragmatics of clinical management (Jellinek, 1960; Lesch et al., 1988), recognition of the influences of family history and comorbidity on manifestations of AD (Babor et al., 1992; Cloninger et al., 1981; Schuckit, 1985), a life-course perspective that emphasizes long-term prognostic outcomes (Jacob et al., 2005; Lesch et al., 1988; Vailant, 1983; Zucker, 1987), and attempts to elucidate the complexity of genetic and environmental influences on the biopsychosocial etiology of the disorder (Bucholz et al., 1996; Cloninger et al., 1981; McGue, 1999).
These extant approaches to AD subtyping have employed either empirical or clinical/observational strategies using data derived primarily from treatment-seeking samples. This is a significant limitation, since sample size and attributes influence typological solutions. Recent data from the National Epidemiological Survey on Alcohol and Related Conditions (NESARC) suggest that, among those with prior-to-past year AD, only 25.5% have ever received treatment (Dawson et al., 2005). Thus, there is a substantial proportion of the AD population that is not represented in the clinical samples previously used for typology development. Consistent with Berkson’s bias (Peritz, 1984), sole reliance on hospitalized or treatment AD cases for subtype development may introduce a form of selection bias wherein only those cases that manifest greater severity or have clinical features associated with treatment program admission are accounted for in the typology. The resultant subtypes may not generalize well to the broad spectrum of community-dwelling AD individuals, thereby diminishing the utility of the typology for public health initiatives involving screening, early identification, treatment planning, or prevention.
Consequently, the purpose of this study is to empirically subtype those with current AD based upon a multivariate panel of dichotomous and dimensional clinical indicators, and using a nationally representative epidemiological sample obtained through the NESARC survey. We know of no other existing AD typology that is based upon nationally representative data, and that includes individuals both in and not seeking treatment who meet DSM-IV criteria for AD. This subtyping effort expands on prior research not only by using the DSM-IV criteria for Alcohol Use Disorders (AUD), but also by including age of drinking onset, age of onset of AD, family history of AD in various configurations, the lifetime presence or absence of specific externalizing and internalizing psychiatric disorders, and other substance use disorders that are salient features of extant typologies.
This study is timely because the research agenda for DSM-V is currently being mapped out (Kupfer et al., 2002). By describing the clinical characteristics of disparate subgroups of individuals in the general population with AD, we hope to generate hypotheses that may stimulate changes in the diagnostic criteria for the next version of the psychiatric classification system. However, the clinical utility of any diagnostic typology relates not only to its capacity to aggregate clinical features into relatively homogeneous subgroupings as we report here, but also to guide treatment modality selection, predict treatment outcome, and prognosis. This report focuses on the initial objective of clinical categorization and its description; the latter therapeutic and prognostic objectives are beyond the scope of this current investigation, but will be addressed when data from the NESARC follow-up are available.
2. Methods
2.1. Sample
This analysis utilizes data from the 2001–2002 National Epidemiological Survey on Alcohol and Related Conditions (NESARC), conducted by the National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health. As described elsewhere (Grant et al., 2004b), the NESARC sample represents the civilian, non-institutionalized adult population of the United States, including all 50 states and the District of Columbia. It includes persons living in households, military personnel living off-base, and persons residing in boarding or rooming houses, non-transient hotels and motels, shelters, college quarters, and group homes. The U.S. Census Supplementary Survey, in combination with the Census 2000 Group Quarters Inventory, comprised the sampling frame for the NESARC. The NESARC over-sampled African-Americans, Hispanics, and adults 18–24 years of age, to ensure an adequate sample size for subgroup comparisons within these high-risk populations. A single sample adult 18 or older was randomly selected for interview from each sample household. Personal interviews were conducted in respondents’ homes. The overall response rate was 81% (n= 43,093). Weights are available in NESARC for making population estimates based on the sample data. The analyses herein are based on the 1,484 respondents who met at least three DSM-IV diagnostic criteria for AD in the past year, weighted to represent about 7.9 million individuals in the U.S. adult population. Of these, 68% were men, 71% were Caucasian, 49% were never married, and their average age was 32 years.
2.2. Measures
2.2.1. DSM-IV Alcohol Dependence Diagnoses and Alcohol Use Disorder Criteria
The presence of AD was defined in accordance with the criteria established by DSM-IV, employing the items from Alcohol Use Disorders and Associated Disabilities Interview Schedule-DSM-IV version (AUDADIS-IV) (Grant et al., 2003). The AUDADIS-IV is a fully structured diagnostic interview that includes modules to assess major mood and anxiety disorders, antisocial personality disorder (ASPD), substance related medical conditions, family history of alcohol and drug use disorders, alcohol and drug diagnoses, and modules that measure the frequency and quantity of substance use. For alcohol, a comprehensive set of questions also measures the respondent’s specific beverage consumption during usual and heaviest drinking periods. DSM-IV diagnostic criteria for alcohol abuse and dependence are derived from multiple AUDADIS-IV indicators. We employed the seven AD criteria with a cut-off of three of the seven in accordance with DSM-IV. We also used the four criteria for Alcohol Abuse (AA) from the DSM-IV. Test-retest reliabilities for past year DSM-IV AA and AD diagnoses have a Kappa = 0.76 and an intra-class correlation = 0.75 (Grant et al., 1995).
2.2.2. Ages of Onset
Ages of onset are employed as developmental indicators of life course in these analyses. Such drinking and problem-onset data are important components of the subtype constructs developed by Cloninger (Cloninger et al., 1981), Schuckit (Schuckit, 1985), Zucker (Zucker, 1987), Babor (Babor et al., 1992), and Hauser and Rybakowski (Hauser and Rybakowski, 1997). The AUDADIS-IV collects “age when started drinking, not counting small tastes or sips;” “age of onset of AD;” and, the presence or absence of “major depression prior to age 15 years.” The inclusion of early depression onset is based upon recent evidence linking childhood depression to early onset of alcohol use (Wu et al., 2006).
2.2.3. Family History of AD
Familial transmission of alcohol problems is an inherent component of the Cloninger (Cloninger et al., 1981), Hauser and Rybakowski (Hauser and Rybakowski, 1997), and Windle and Scheidt (Windle and Scheidt, 2004) typologies. The AUDADIS-IV collects extensive data on family history of AD. We recoded family history as “first degree relatives only,” “second degree relatives only,” and “both first and second degree relatives.” We refer to this latter pattern of affected first and second degree relatives as multigenerational AD.
2.2.4. Lifetime Psychiatric Diagnoses
2.2.4.1. Internalizing Psychopathology
The presence of internalizing forms of psychopathology figure prominently in the typologies of Schuckit (Schuckit, 1985), Zucker (Zucker, 1987), Hauser and Rybakowski (Hauser and Rybakowski, 1997), and Windle and Scheidt (Windle and Scheidt, 2004). We utilized AUDADIS-IV to determine the lifetime presence of DSM-IV Major Depression, Dysthymia, Bipolar Disorder, Generalized Anxiety Disorder, Panic Disorder without Agoraphobia, and Social Phobia. In addition, we added the presence or absence of Obsessive-Compulsive Personality Disorder on theoretical grounds since “addiction” is a manifestation of the compulsion to use a given drug.
2.2.4.2. Externalizing Psychopathology
The Cloninger (Cloninger et al., 1981), Schuckit (Schuckit, 1985), Zucker (Zucker, 1987), Babor (Babor et al., 1992), Hauser and Rybakowski (Hauser and Rybakowski, 1997), and Windle and Scheidt (Windle and Scheidt, 2004) typologies all utilize ASPD or adult antisocial behavior as externalizing characteristics discriminating subtypes of AD individuals. In this analysis, we used both the presence of DSM-IV ASPD (with Conduct Disorder), and the quantification of the lifetime number of adult antisocial behaviors from the AUDADIS-IV checklist.
2.2.4.3. Other Substa nce Use Disorders and Behaviors
The Schuckit (Schuckit, 1985), and Windle and Scheidt (Windle and Scheidt, 2004) typologies include other substance use behavior in their criteria. In our model, we employed the AUDADIS-IV DSM-IV lifetime diagnoses to include any Cannabis Use Disorders, any Cocaine Use Disorders, any Opioid Use Disorders, and any Amphetamine Use Disorders. In addition, we included a daily cigarette smoking variable to measure regular smoking behavior.
2.3. Analysis
Subtypes of AD were identified by latent class analysis (LCA), based on the 26 categorical indicators (including the seven DSM-IV AD criteria and the four DSM-IV AA criteria) and the three continuous indicators described above (age when started drinking, age of onset of AD, and lifetime number of adult antisocial behaviors). The purpose of LCA is the same as that of traditional cluster analysis, viz., to classify similar objects into groups, where the numbers of groups, as well as their forms, are unknown (Kaufman, 1990). However, using model-based LCA for AD subtyping is more likely to yield better classifications than previous AD typology studies using traditional clustering procedures (e.g., K-Means, hierarchical clustering), which rely on an ad-hoc distance measure for classification, and thus, are limited to interval scale variables and require standardization of variables to equal variance (Magidson, 2002). Until recently, LCA was limited to the analysis of categorical variables; however, advances now permit LCA with a mixed scale of both categorical and continuous variables (Vermunt, 2005). The objective of LCA is to find the smallest number of groups (i.e., latent classes) that best describe the associations among a set of observed indicators, such that individuals in one class are similar to one another but are distinct from individuals in other classes. The resulting classes were characterized by the differentials in the observed indicators (means for the continuous indicators and proportions for the categorical indicators). In contrast to the observed indicators, the number of classes is latent and determined by the model. The best-fit model is the one with the lowest Bayesian Information Criterion (BIC). Generally, the lower the BIC is, the better the model fits. Initially, we fitted one- to 10-class standard latent class models and compared their BICs. However, standard LCA assumes local independence among all indicators within a class, and its strategy to counter the violation of this assumption is to increase the number of latent classes until a model with an acceptable fit is obtained (Vermunt, 2005). Since many of our indicators are highly correlated (e.g., lifetime major depression, and age at onset of major depression before 15), the initial better-fitted models yielded too many latent classes to be clinically useful. In order to reduce the number of latent classes, we relaxed the local independence assumption by allowing for associations between some pairs of indicators based on bivariate residuals.1 These selected pairs also appeared to mirror clinical reality. We then fit one to 7 latent classes under this relaxed constraint.
We conducted the LCA using Latent GOLD 4.0 (Statistical Innovations, Belmont, Massachusetts), which takes into account the effect of complex sampling design and allows for local dependence between indicators. The parameters were estimated by the posterior mode (PM) method with weak priors to prevent boundary solutions or the problem of non-existence of maximum likelihood estimates. Statistical tests were obtained using the linearization variance estimator. To fully utilize the study sample, respondents with missing data (mostly on age at drinking onset) were included in the analysis using the full information PM estimation assuming missing at random or the missing data mechanism being ignorable (Vermunt, 2005).
Based on the classes identified by our best-fit model, each respondent was assigned to a class according to their most likely class membership (i.e., the highest posterior class probabilities). We then calculated the proportions/means for each of the classes for a number of important covariates. These covariates included sex, age, race/ethnicity, marital status, education, family income, alcohol treatment, and drinking measures (i.e., frequency, quantity, volume, frequency of binge drinking, and the largest number of drinks at one occasion). These descriptive measures were compared across classes to provide criterion validity checks for the latent class memberships. Overall comparisons across classes were made by log-likelihood Chi-square tests for categorical indicators and by Wald F-tests for continuous indicators using SUDAAN 9 (Research Triangle Institute, Research Triangle Park, North Carolina).
3. Results
3.1. Five-Cluster Solution for AD
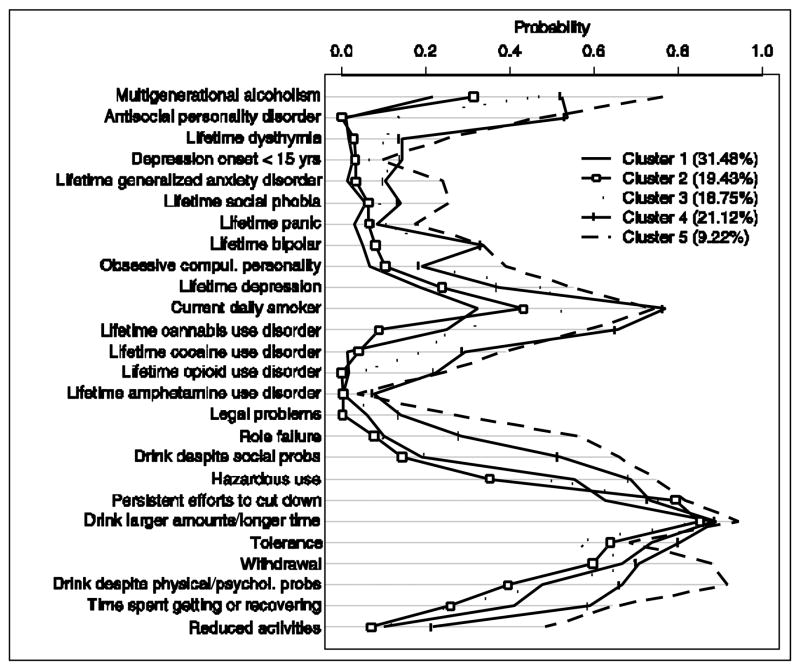
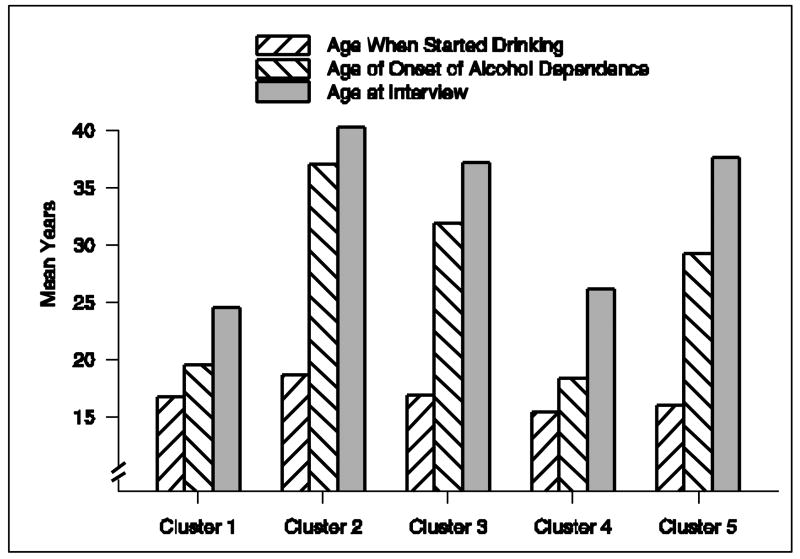
As may be seen in Table 1, significant improvements in model fit (reductions in BIC) were obtained as we increased the number of clusters from one to five, and then fit indices began to worsen as the five-cluster model was exceeded. Thus, the best model fit was a five-cluster solution. The prevalence of cluster membership ranged from 31.48% (Cluster 1) to 9.22% (Cluster 5). The conditional probabilities according to cluster membership for only the 26 categorical variables are graphically displayed in Figure 1. Among the three continuous indicator variables, mean values within each cluster for age when started drinking and age at onset of AD are presented, along with age at time of interview (not an indicator variable), in Figure 2. The mean number of lifetime adult antisocial behaviors for the five clusters were 3.6, 1.7, 7.2, 12.0, and 11.5, respectively. Cluster classification quality, based upon most likely class membership, ranged from 0.85–0.88. Descriptions of the sociodemographic characteristics of individuals assigned to each cluster are displayed in Table 2. DSM-IV AA and AD symptom counts and measures of the drinking behavior of subjects assigned to each cluster are displayed in Table 3. The treatment-seeking behaviors of AD individuals, according to their cluster membership, are displayed in Table 4.
Table 1.
Model Fitting: 5-Cluster solution (in bold italic) most parsimonious for having the smallest Bayesian Information Criterion.
| Solution | Log Likelihood (LL) | Bayesian Information Criterion | Number of Parameters |
|---|---|---|---|
| 1-Cluster | −32302.8151 | 65021.8724 | 57 |
| 2-Cluster | −31216.2770 | 63111.6861 | 93 |
| 3-Cluster | −30508.4477 | 61958.9174 | 104 |
| 4-Cluster | −30235.3242 | 61675.5603 | 139 |
| 5-Cluster | −30063.3921 | 61594.5860 | 201 |
| 6-Cluster | −29950.5259 | 61631.7435 | 237 |
| 7-Cluster | −29888.2992 | 61770.1800 | 273 |
Fig 1.
Conditional probabilities of the 26 categorical variables according to resultant five-cluster model derived from latent class analysis (Displayed separately in Figure 2 are two of the three continuous variables in the analysis [i.e., age of drinking onset, and age of onset of AD]). Large differences between clusters were determined by the presence/absence of multigenerational familial Alcohol Dependence (AD), the presence/absence of antisocial personality disorder, the presence/absence of lifetime major depression, the presence of daily smoking, cannabis, cocaine, and opioid use disorders, hazardous use of alcohol, and alcohol tolerance and withdrawal. Clusters converged around two of the DSM-IV AD criteria (i.e., drinking larger amounts of alcohol for a longer time, and persistent efforts to cut down on drinking).
Fig 2.
Mean ages of respondents at time of interview, ages at initiation of alcohol use, and ages of onset of Alcohol Dependence (AD) according to derived clusters. The ages of initiation are comparable across the clusters. Younger AD individuals (Clusters 1 and 4) reported younger age of onset for AD with shortened course. Older AD individuals (Clusters 2, 3, and 5) reported a longer course between initiation and development of AD.
Table 2.
Sociodemographic characteristics of subjects assigned to AD clusters. Clusters 4 and 5 demonstrate lowest indicators of functional status. Cluster 2 displays the high level of functional status. Cluster 1 has over a third of its members in school on a full- or part-time basis.
| Sociodemographic Characteristics | Cluster 1 | Cluster 2 | Cluster 3 | Cluster 4 | Cluster 5 | p-valuea |
|---|---|---|---|---|---|---|
| Cluster size (proportion of total) | 31.48% | 19.43% | 18.75% | 21.12% | 9.22% | |
| Age (years) | 24.52 | 40.66 | 37.91 | 26.47 | 37.82 | <0.0001 |
| Sex | 0.0018 | |||||
| Male | 71.58% | 59.77% | 63.59% | 75.83% | 64.48% | 0.0018 |
| Female | 28.42% | 40.23% | 36.41% | 24.17% | 35.52% | 0.0018 |
| Race/Ethnicity | 0.0003 | |||||
| White | 76.65% | 63.75% | 74.77% | 71.33% | 61.41% | 0.0074 |
| Black | 7.29% | 16.66% | 10.43% | 8.99% | 11.30% | 0.0126 |
| American Indian/Alaska Native | 1.21% | 0.91% | 2.99% | 5.98% | 13.55% | 0.0002 |
| Asian/Native Hawaiian/Pacific Islander | 3.06% | 2.60% | 2.51% | 2.95% | 1.99% | 0.9805 |
| Hispanic or Latino | 11.79% | 16.08% | 9.31% | 10.75% | 11.75% | 0.1058 |
| Marital status | <0.0001 | |||||
| Married | 15.47% | 49.47% | 37.92% | 15.28% | 28.70% | <0.0001 |
| Living with someone as if married | 4.38% | 5.03% | 9.11% | 9.36% | 5.82% | 0.1060 |
| Widowed | 0.00% | 4.44% | 2.51% | 0.00% | 6.05% | 0.3163 |
| Divorced | 3.79% | 11.91% | 20.89% | 7.16% | 25.11% | <0.0001 |
| Separated | 1.29% | 5.58% | 7.83% | 4.25% | 8.56% | 0.0129 |
| Never Married | 75.08% | 23.56% | 21.74% | 63.95% | 25.75% | <0.0001 |
| Education | <0.0001 | |||||
| Less than HS | 9.01% | 16.50% | 14.58% | 25.57% | 25.21% | <0.0001 |
| HS or GED | 27.80% | 25.11% | 26.69% | 35.02% | 29.17% | 0.2241 |
| Some college | 44.07% | 32.76% | 39.49% | 31.80% | 36.63% | 0.0280 |
| College degree or higher | 19.12% | 25.63% | 19.24% | 7.61% | 9.00% | 0.0003 |
| Working full-time (35+ hours a week) | 54.17% | 62.27% | 68.34% | 47.61% | 42.95% | <0.0001 |
| Working part-time (<35 hours a week) | 18.06% | 13.13% | 9.45% | 17.67% | 11.89% | 0.0379 |
| Unemp loyed or laid off and looking for work | 5.45% | 7.07% | 8.02% | 15.45% | 16.96% | 0.0028 |
| Unemployed or laid off and not looking for work | 1.35% | 1.07% | 1.55% | 3.48% | 3.22% | 0.4550 |
| Unemployed and permanently disabled | 0.23% | 2.82% | 3.41% | 2.75% | 7.59% | 0.0003 |
| Retired | 0.97% | 4.98% | 3.17% | 0.58% | 1.20% | 0.0049 |
| In school full-time | 31.25% | 3.59% | 3.09% | 13.41% | 2.82% | <0.0001 |
| In school part-time | 5.21% | 2.42% | 3.67% | 1.98% | 3.22% | 0.2771 |
| Full-time homemaker | 0.66% | 5.48% | 4.52% | 4.63% | 2.79% | 0.0265 |
| Total family income in last 12 months | $41,854 | $59,576 | $49,687 | $31,989 | $31,932 | <0.0001 |
Based on log-likelihood Chi-square test for overall differences across the clusters.
Table 3.
DSM-IV Alcohol Use Disorder symptom counts and alcohol consumption measures of subjects assigned to Alcohol Dependence clusters. Clusters 4 and 5 demonstrate the highest levels of symptom endorsements and alcohol consumption behavior.
| DSM-IV Diagnostic Criteria and Alcohol Consumption | Cluster 1 | Cluster 2 | Cluster 3 | Cluster 4 | Cluster 5 | p-valuea |
|---|---|---|---|---|---|---|
| DSM-IV diagnostic criteria met | ||||||
| # Alcohol abuse criteria | 0.92 | 0.59 | 0.82 | 1.65 | 2.28 | <.0001 |
| # Alcohol dependence criteria | 3.90 | 3.61 | 3.67 | 4.67 | 5.38 | <.0001 |
| Alcohol consumption measures | ||||||
| # Days drank any alcohol in last 12 months | 142.98 | 181.39 | 172.16 | 201.36 | 247.46 | <0.0001 |
| # Days drank 5+ drinks of any alcohol in last 12 months | 103.89 | 97.76 | 93.57 | 161.40 | 172.11 | <0.0001 |
| Binge drinking rate (Percentage of last- year drinking days that consumption exceeded 5 drinks) | 73% | 54% | 54% | 80% | 69% | |
| Number of drinks of any alcohol usually consumed on days when drank alcohol | 6.21 | 5.14 | 4.81 | 8.28 | 8.15 | <0.0001 |
| Largest number of drinks of any alcohol consumed on days when drank alcohol | 13.79 | 10.03 | 9.79 | 17.13 | 15.43 | <0.0001 |
| Average daily volume of ethanol (fluid ounces) consumed in past year | 2.48 | 2.66 | 2.16 | 4.69 | 6.38 | <0.0001 |
Based on Wald F-test for overall differences across the clusters.
Table 4.
Treatment-Seeking among Alcohol Dependent Individuals according to Subtype. Clusters 3, 4 and 5 have the highest rate of treatment-seeking. Cluster 1, the most prevalent subtype, has the lowest rate of treatment-seeking. Overall, Cluster 5 has the highest rates of attendance across a wide variety of treatment venues.
| Alcoholism Treatment | Cluster 1 | Cluster 2 | Cluster 3 | Cluster 4 | Cluster 5 | p-valu ea |
|---|---|---|---|---|---|---|
| Ever sought help because of drinking | 8.70% | 17.03% | 26.87% | 34.36% | 65.95% | <0.0001 |
| Among those with AD who sought help for drinking: | ||||||
| Ever went to alcoholics/narcotics/cocaine anonymous, or 12-step meeting | 71.09% | 63.45% | 74.23% | 65.95% | 90.40% | 0.0074 |
| Ever went to family services or other social service agency | 21.88% | 15.45% | 24.03% | 26.43% | 40.07% | 0.2019 |
| Ever went to alcohol/drug detoxification ward/clinic | 25.61% | 25.33% | 42.74% | 40.54% | 63.89% | 0.0044 |
| Ever went to inpatient ward of psychiatric/general hospital or community mental health program | 6.86% | 16.84% | 24.10% | 34.51% | 48.14% | 0.0003 |
| Ever went to outpatient clinic, including outreach and day/partial patient program | 19.12% | 11.36% | 33.00% | 32.48% | 55.39% | 0.0016 |
| Ever went to alcohol/drug rehabilitation program | 37.10% | 29.72% | 53.76% | 50.21% | 74.50% | 0.0006 |
| Ever went to emergency room because of drinking | 17.68% | 12.57% | 30.03% | 37.90% | 51.57% | 0.0028 |
| When went to halfway house/therapeutic community | 3.08% | 4.86% | 11.02% | 10.89% | 15.43% | 0.0780 |
| Ever went to crisis center because of drinking | 2.94% | 0.00% | 3.91% | 5.83% | 8.85% | 0.0306 |
| Ever went to employee assistance program (EAP) | 8.93% | 5.07% | 14.28% | 4.88% | 10.67% | 0.3498 |
| Ever went to clergyman, priest, or rabbi because of drinking | 17.54% | 14.67% | 15.68% | 26.46% | 25.64% | 0.4256 |
| Ever went to private physician, psychiatrist, psychologist, social worker, or any other professional | 20.49% | 30.99% | 41.56% | 58.17% | 51.51% | 0.0005 |
| Ever went to any other agency or professional | 7.45% | 6.48% | 16.95% | 18.89% | 11.49% | 0.1231 |
Based on log-likelihood Chi-square test for overall differences across the clusters.
3.2. Cluster Descriptions
Cluster 1(“Young Adult Subtype”) is the most prevalent cluster (31.5 %), and is characterized by a younger age (mean age 24.5 years), a relatively early onset of AD (mean age 19.6 years), a low probability of ASPD (<1%), and a moderate probability of AD in both first and second degree family members (~22%). Relative to other clusters, cluster members manifest lower probabilities of comorbid psychiatric disorders and legal problems, and a moderate probability of being cigarette smokers (~32%) and cannabis abusers (~25%). Cluster 1 AD individuals have an elevated probability of engaging in hazardous use of alcohol and experiencing alcohol withdrawal. Examination of demographic data suggests that Cluster 1 AD males are 2.5 times more common than Cluster 1 AD females. Given the relative youth of cluster members, it is not surprising that ~75% have never been married. Only 54% work full-time, while 36.5% are in school either full-time or part-time. They tend to drink alcohol less frequently than other cluster members (~143 drinking days in last year); however, they drink 5+ drinks on an average of 104 (73%) of these drinking days. They report drinking an average maximum of 13.8 (standard) drinks on drinking days. Only 8.7% of Cluster 1 individuals have ever sought help because of drinking. When they do seek help, it is more frequently through 12-step groups rather than through private professional or specialty treatment.
Cluster 2 (“Functional Subtype”) (19.4%) is characterized by older respondents (age ~41 years), a slightly older age of initiation to drinking (mean age 18.5 years), a later onset of AD (mean age 37 years), a low probability of ASPD (<1%), and a moderate probability of AD in both first and second degree family members (~31%). Cluster members manifest a moderate probability of major depression (~24%), and low rates of anxiety disorders. Members have a moderate probability of being regular smokers (~43%), low probabilities of other substance use disorders, and the least probability of having legal problems (<1%). Cluster 2 individuals have a moderately elevated probability of endorsing engagement in hazardous use of alcohol (~35%), and the lowest cluster probability for using alcohol despite problems (~14%). They also have the lowest probability for endorsing a reduction in activities due to alcohol (~7%), and drinking despite problems (~40%). In terms of external covariates, there is a modest over-representation of males (~60%) relative to females (~40%). Nearly 50% of Cluster 2 individuals are married, 62% work full-time, and only 3.6% are in school full-time. Nearly 26% have a college degree or higher. This cluster has the highest proportion of retired individuals (~5%). Cluster 2 mean total family income ($59,576) is the highest among the AD clusters. Cluster 2 individuals tend to drink alcohol every other day (~181 drinking days in last year), and they consume 5+ drinks on an average of almost 98 (54%) of these drinking days. They report an average of 10 drinks as being the maximum number consumed on drinking days. Seventeen percent of Cluster 2 individuals have ever sought help for their drinking. Help-seeking Cluster 2 individuals more typically participate in 12-step groups or are treated for AD by private health care professionals.
Cluster 3 (“Intermediate Familial Subtype”) (18.8%) is also characterized by an older mean respondent age (~38 years), an onset of drinking at almost age 17, and an onset of AD at age 32 years. They have a modestly elevated probability of meeting criteria for ASPD (~12.5%), and an elevated probability for having both first and second degree family members with AD (~47%). There is a heightened probability that Cluster 3 members smoke cigarettes (57%), suffer from major depression (47%), bipolar disorder (~22%), obsessive-compulsive personality disorder (~19%), and/or generalized anxiety disorder (~15%) at some time in their lives. They also have elevated probabilities of cannabis (~25%) and/or cocaine use disorder (~20%). In terms of external covariates, 64% of cluster members are male and 36% female. About 38% are married, and 21% are divorced. Nearly 20% of Cluster 3 members have a college degree or higher and 68% work full-time, giving this cluster the highest level of employment among the AD clusters. Total family income is nearly $50,000/year. Cluster 3 members report drinking on an average of 172 days in the last year, 93 on which they drank 5+ drinks (54%). The maximum number of drinks consumed on drinking days is about 9.8 standard drinks. Of those in Cluster 3, almost 27% have ever sought help for their drinking. When treatment is sought by Cluster 3 individuals, they tend to go to self-help groups, specialty treatment programs, detoxification programs, and individual private health care providers.
Cluster 4 (“Young Antisocial Subtype”) (21.1%) is comprised of individuals who are relatively young (mean age 26.4 years), have the earliest onset of drinking (mean age 15.5 years), and the earliest onset of AD (mean age 18.4 years). They have the highest probability of ASPD among the clusters (~54%), and an elevated probability of multigenerational AD (52.5%). The number of reported antisocial behaviors is highest among members of this cluster (average of 12 antisocial behaviors endorsed). Cluster 4 is also characterized by an elevated probability of major depression (~37%), bipolar disorder (33%), social phobia (~14%), and obsessive compulsive personality disorder (19%). As a group, they have the highest probability for a major depressive episode prior to age 15 years (~14%). Cluster 4 members also have a high probability for other forms of substance abuse. They have the highest probability among the clusters of being regular smokers (~77%), meeting criteria for cannabis abuse/dependence (~66%) and/or amphetamine abuse/dependence (7.8%). They also have a high probability for cocaine use disorder (~29%) and opioid use disorder (22%). They have higher endorsement probabilities for all four of the AA criteria. They have the highest probability for endorsement of tolerance. In terms of external covariates, Cluster 4 is comprised of 76% males and 24% females. Only 15.3% are married, and 64% are never married. This cluster has the lowest proportion receiving a college degree or higher (7.6%). Among Cluster 4 individuals, 47% are employed full-time, while 13.4% are in school full-time. Total family income in the last 12 months averaged $31,988, along with Cluster 5, one of the two lowest of the AD clusters. Cluster 4 individuals have an average of ~201 drinking days in the last 12 months, consuming 5+ drinks on an average of 161 of those drinking days (80%). They report consuming a maximum number of 17.1 drinks on drinking days, which is the largest reported amount among any of the AD clusters. Almost 35% of Cluster 4 individuals report having sought help for their drinking. Cluster 4 individuals tend to go to self-help groups, specialty treatment programs, and detoxification programs, and they have the highest rate of participation in treatment with individual private health care providers.
Cluster 5 (“Chronic Severe Subtype”) is the least prevalent of the clusters (9.2%). Respondents average 37.8 years of age, with an early onset of drinking (mean age 15.9 years), and a later onset of AD (mean age ~29 years). The probability of meeting the ASPD diagnosis is about 47%. Members of the cluster have, on average, the second highest number of antisocial behaviors endorsed (11.5). Cluster 5 has the highest probability of both first and second degree family members affected with AD (~77%) among the AD clusters. The probabilities for Cluster 5 exceed all other AD clusters for lifetime major depression (~55%), dysthymia (~25%), bipolar disorder (~34%), generalized anxiety disorder (~24%), social phobia (~26%), and panic disorder (~17%). Cluster 5 members have elevated probabilities for regular smoking (~75%), cannabis use disorders (58%), cocaine use disorders (39%), and opioid use disorders (24%). Cluster 5 individuals have the highest probabilities for endorsing all four of the AA criteria. For AD criteria, they have the highest probability for endorsement of withdrawal (88%), persistent efforts to cut down (~83%), drinking larger/longer amounts than intended (94%), time spent recovering from alcohol (~64%), reduced activities due to drinking (~48%), and drinking despite problems (~92%). Examination of the external sociodemographic covariates reveals that this cluster is comprised of ~65% males and ~35% females. Among these, 28.7% are married. This cluster has the highest divorce rate among the AD clusters, with 25.1% divorced and ~8.6% separated. Only 9% are educated through college or beyond. Cluster 5 has the lowest employment rate with ~43% employed full-time, and ~7.6% unemployed and permanently disabled. Members of Cluster 5 have the greatest number of past year drinking days of any of the AD clusters (247.5 days), and they drank 5+ drinks on 172 of them (69%). They report that, on average, they drink a maximum number of 15.4 drinks on any drinking day. Nearly 66% of Cluster 5 individuals have sought help for their drinking problem, making them the most prevalent AD help-seekers. Cluster 5 members have the highest rates of attendance at self-help groups, specialty rehabilitation programs, and detoxification programs, as well as the highest rate of receiving treatment in an inpatient program. They tend to select private physicians, psychiatrists, psychologists, social workers for treatment, and the highest rate of emergency room visits for help with their drinking.
4. Discussion
We identified five empirical subtypes of AD in this representative general U.S. population sample. This classification effort may help guide phenotypic categorization for AD gene-hunting efforts, assist in the characterization of human molecular targets for pharmacotherapy, or guide ascertainment criteria for clinical trials of behavioral and pharmacotherapy interventions. We believe the results are heuristic for the DSM-V, and provide a useful and clinically meaningful classification of AD individuals that may be further examined in a variety of clinical and research settings. As may be seen in Figure 5, the major discriminating features that differentiated the subtypes were age of onset of AD, multigenerational familial AD (but not first degree-only affected family members with AD), ASPD, endorsement of specific AA criteria, comorbid substance use disorders, comorbid mood, comorbid anxiety disorders, and consumption patterns. The resulting subtypes share elements in common with prior typologies, as well as identifying distinct AD subtypes not previously described. The sharing of common features with prior typologies is not surprising since we have selected model variables that are, in part, based upon extant typologies. Furthermore, others have identified overlap among the extant AD typologies, and have also demonstrated a significant degree of heterogeneity within these established AD subtypes (Anthenelli et al., 1994; Epstein et al., 2002). Importantly, in the current analyses, we were able to assign each respondent to an individual class according to their most likely class membership (i.e., the highest posterior class probabilities). In order to address the question of the clinical ramifications of these latent classes, we conducted two additional analyses (Data not shown). In the first analysis, we selected only those subjects where ever sought treatment for their drinking. Latent class analysis revealed three clusters of treatment seekers (n=367). The treatment subtypes consisted of one cluster of individuals mainly from the original Clusters 1–3, one subtype from the original Cluster 4, and one from the original Cluster 5. The conditional probabilities profiles for the second and third clusters were consistent with our original Clusters 4 and 5. The profile of treatment cluster 1, appeared to be an averaged profile from original Clusters 1–3. Thus, the newly formed 3 AD subtypes of ever treated AD individuals were consistent with the original typology generated by the full AD sample. Then, we examined the conditional probability profiles of those cluster members who have ever sought treatment versus those who never sought treatment on a cluster by cluster basis; the profiles did not differ much for any of the five clusters regardless of treatment status. Nevertheless, within each cluster, compared with their non-treated counterparts, those who ever sought help with drinking problems tend to be older and have experienced a longer duration of AD from AD onset. In addition, they were more likely to exhibit multigenerational alcoholism and have higher probabilities endorsing both DSM-IV AA and AD criteria as well as daily smoking and other substance use disorders.
Cluster 1, the most prevalent subtype (~31.5%), is an early onset subtype of AD found primarily among young adults. There are low rates of multigenerational familial AD, ASPD, comorbid psychiatric, and substance use disorders. A substantial proportion of Cluster 1 individuals are still in school (~36% full- or part-time), suggesting that they may be an unrecognized part of the college drinking problem. None of the extant typologies capture this subtype with any degree of specificity. The relative youth of this highly prevalent group suggests that they may be a “developmentally limited” subtype, as hypothesized by Zucker (Zucker, 1987). Data from the NESARC follow-up will be able to examine this hypothesis directly. This cluster also shares some common features with the Young Adult Alcoholics subtype described by Jacob and colleagues (Jacob et al., 2005). Members of this cluster tend to drink less frequently, but when they do drink, they tend to binge.
Cluster 2 (~19%) is characterized by a later initiation to drinking, a later onset of AD, and low rates of multigenerational AD, ASPD, mood disorders, anxiety disorders, and had almost no other substance use disorders, aside from regular smoking. They have minimal legal problems, and tend not to endorse other AA criteria. They are, on average, older than other cluster members, and tend to drink in an excessive, although less severe, manner. They have the highest family income, are college educated, and are most likely to be married. From a psychosocial perspective, they represent the highest functioning subtype of AD. They share commonalities with those subtypes described by Schuckit (Schuckit, 1985), Hauser and Rybakowski (Hauser and Rybakowski, 1997), and Windle and Scheidt (Windle and Scheidt, 2004), characterized by later onset of dependence, low prevalence of familial alcoholism, low levels of antisociality, and a lower rate of binge drinking. Despite their high level of functioning, this subgroup may still ultimately be at significant risk for the biomedical consequences of AD.
Cluster 3 (~19%) is comprised of middle-aged individuals with a longer time course from drinking initiation to AD. They appear to have only a modest rate (~13%) of ASPD. A significant proportion of Cluster 3 individuals (~47%) come from families with affected first- and second-degree relatives. Nearly half (~47%) of cluster members have manifested a major depressive disorder sometime in their lives. Fifteen percent have generalized anxiety disorder. More than half are regular smokers, and significant numbers meet criteria for other substance use disorders. Despite the presence of other substance abuse, Cluster 3 has a lower quantity of alcohol consumption and a lower binge rate similar to Cluster 2 individuals. The group resembles aspects of the “negative affect” type of Zucker (Zucker, 1987), the “primary” alcoholic described by Schuckit (Schuckit, 1985), and the “negative affect type” of Windle and Scheidt (Windle and Scheidt, 2004).
Cluster 4 (~21%) is a young adult, early-onset group with the highest proportion of individuals with comorbid AD and ASPD (~54%). Nearly half endorse having affected first- and second-degree family members at a level similar to Cluster 3. They have the highest severity of alcohol consumption of any of the AD subtypes in terms of both quantity consumed and rate of binge drinking. They have high rates of smoking (~77%), and other forms of substance abuse. Over a third of the cluster members have a lifetime history of major depression, and bipolar disorder. About 15% had an episode of major depression during childhood. Anxiety disorders are prevalent at a moderate level. This subgroup is the least educated and, along with Cluster 5, is at the lower end of the socioeconomic continuum. As a group, they resemble aspects of the Cloninger Type 2 (Cloninger et al., 1981), the Babor Type B (Babor et al., 1992), and the heavy drinking antisocial subtype of Windle and Scheidt (Windle and Scheidt, 2004).
Cluster 5 (~9.0%) is an older, later onset subtype, with a high proportion having comorbid AD and ASPD. Drinking severity is high, and at about the same level as Cluster 4. This group has the highest rate of lifetime major depression, dysthymia, and bipolar disorder. They also have the highest rates of generalized anxiety disorder, panic disorder, and social phobias. Cluster 5 is also remarkable in that nearly 40% also met diagnostic criteria for obsessive-compulsive personality disorder. There are also high rates of other substance abuse with three-quarters being regular smokers, and nearly 40% endorsed criteria for cocaine use disorder. This cluster has the highest rate of endorsement for AA items that are indicators of alcohol-related psychosocial dysfunction (e.g., role obligations failure, hazardous use, use despite problems, and legal problems), and the lowest socioeconomic indicators suggesting that members of this subgroup manifest the highest levels of alcohol consequences. As a group, Cluster 5 individuals drink with the greatest frequency, and have a high rate of binge consumption. This cluster resembles a trajectory-defined subgroup described by Jacob and colleagues (Jacob et al., 2005) as “Severe Chronic Alcoholics.”
As noted by Hasin and Grant (Hasin and Grant, 2004) in the DSM-IV, an AA diagnosis is preempted by AD, yet many individuals with AD also endorse AA symptoms. The highest endorsement probabilities for AA symptoms are found among Clusters 4 and 5. Hasin and Grant have suggested that AD individuals with and without AA may represent heterogeneous phenotypes for genetic research. Our data both confirm and extend that observation. High AA endorsement rates are associated with the more antisocial, familial, and psychiatrically comorbid variants of AD.
The over-representation of AD among males is a well-established observation. The aggregate 12-month AD prevalence ratio of males to females is reported to be about 2.3 in the NESARC (Grant et al., 2004a). Unlike the “male-limited” characterization of the Cloninger Type 2 grouping, this study revealed that empirically-derived AD clusters were not “limited” only to males. Females represented ~28%, ~40%, ~36%, 24%, and ~36% of Clusters 1 through 5, respectively. Cluster 4 individuals, whose early-onset features resemble the antisocial Cloninger Type 2 grouping, contained the highest male to female ratio (~3.14), but still had a substantial representation of females (~24%). The next highest ratio was found among individuals in the early-onset, young adult Cluster 1 (~2.5). Middle-aged Cluster 2 individuals had the lowest male to female ratio (~1.5). Middle-aged Clusters 3 and 5 also had relatively low ratios (~1.8 and ~1.8, respectively) when compared with the aggregate male to female ratio for AD. Thus, it appears from the data that those AD subgroups, comprised predominantly of earlier-onset young adults, tend to have a greater degree of male over-representation. Antisociality and multigenerational familial AD appear to have limited influence on the gender ratio, suggesting that the typical etiological course in AD development for females may take longer than in males, and reflecting an onset occurring later in life. That being said, it is also clear that there are exceptions to this “typical course,” suggesting gender-specific heterogeneity. Future gender-specific analyses may clarify these gender differences, and identify opportunities for intervention.
Greater identification and treatment efforts may be required to intervene successfully with those individuals who have the multigenerational familial forms of AD, have increased liability to psychiatric comorbidity, and have experienced AD for a relatively longer period of time (Clusters 3, 4, and 5). While an analysis of the recovery process among individuals comprising these subtypes is beyond the scope of this report, such individuals might be refractory to low-intensity interventions, require longer-term disease management approaches, and benefit from pharmacotherapy for both AD and their comorbid conditions. The observation that 34% of Cluster 5 individuals have sought help for their drinking in emergency room settings suggests that some of the perceived “health care system burden” of AD might be a consequence of provider interactions with these complex and severe Cluster 5 patients in emergent care facilities.
This is not the first effort to utilize LCA in order to find mutually exclusive classes of individuals with alcohol use disorders. Lynskey and colleagues (2005) used a general population sample of male and female twins, treated separately as singletons, and classified with LCA on the basis of DSM-IV AA and AD criteria. They arrived at a four-class solution for women and a five-class solution for men. Kendler et al., (1998) used LCA to find subtypes of male Swedish twins registered with their Temperance Board. They reported five qualitatively distinct subtypes of alcoholism using a set of predictors specific to Temperance Board registrants. Bucholz et al. (1996) used LCA to study high-risk family members of probands with AD. They found a four-class, severity-based solution. As previously noted, our study is distinct in that it utilizes a general population sample of both males and females with AD, weighted to be nationally representative of the U.S.
As with all research, there are limitations to this study, probably the largest being the cross-sectional nature of the dataset and its subsequent cluster structure. Both Zucker’s (Zucker, 1987) and Lesch’s (Lesch et al., 1988) typologies emphasize longitudinal perspectives as the bases for their constructs. Individuals may move in and out of classes over time. For example, over time some of the younger Cluster 4 individuals could become middle-aged Cluster 5 members. In future research we hope to examine prospectively the outcomes of these subtypes; however, we must wait until the next wave of NESARC results before examining longitudinal outcomes and trajectories.
In summary, we have used latent class analysis on general population psychiatric and substance abuse survey data to reduce the heterogeneity of AD through empirical subtyping. Our results suggest five separate clusters based upon age of onset of AD, multigenerational familial AD, ASPD, endorsement of specific AA criteria, comorbid substance use disorders, comorbid mood, and comorbid anxiety disorders. The resultant AD subtypes share common features with extant typologies, but extend prior subtyping efforts through the identification of subgroups that are not typically found in clinical treatment samples. We believe the results are heuristic and provide a useful classification of AD individuals that may be applied in a variety of clinical and research settings.
Table 5.
Summary characteristics of five empirically-derived AD subtypes in the general U.S. population. Population prevalence of each cluster grouping is in parentheses. Checkmarks indicate proportionally elevated rates for a given characteristic.
| Characteristics | Cluster 1 (31.48%) | Cluster 2 (19.43%) | Cluster 3 (18.75%) | Cluster 4 (21.12%) | Cluster 5 (9.22%) |
|---|---|---|---|---|---|
| Age group | Young adult | Middle aged | Middle aged | Young adult | Middle aged |
| Mean onset of AD from drinking initiation | 2.8 years | 18.4 years | 15.0 years | 2.9 years | 13.2 years |
| Multigenerational familial alcohol dependence | ✓ | ✓ | ✓ | ||
| Antisocial personality disorder | ✓ | ✓ | |||
| DSM-IV alcohol abuse criteria (i.e., hazardous use, use despite social problems and legal problems) | ✓ | ✓ | |||
| Mood disorders | ✓ | ✓ | ✓ | ||
| Anxiety disorders | ✓ | ✓ | ✓ | ||
| Regular smoking | ✓ | ✓ | ✓ | ||
| Other substance use disorders | ✓ | ✓ | ✓ | ||
| Recent alcohol consumption severity (percentage of last year drinking days that consumption exceeded 5 drinks) | 73% | 54% | 54% | 80% | 69% |
Footnotes
These data were presented in part at the 29th Annual Scientific Meeting of the Research Society on Alcoholism, June 23–28, 2006.
The pairs are: use despite problems & reduced activities; panic disorder without agoraphobia-lifetime & cocaine abuse/dependence -lifetime; larger amount than intended & drink despite problems ; use despite problems & drink despite problems ; role obligations failure & use despite problems ; cocaine abuse/dependence-lifetime & opioid abuse/dependence-lifetime ; cannabis abuse/dependence -lifetime & cocaine abuse/dependence-lifetime; obsessive-compulsive personality disorder & bipolar-lifetime ; major depression-lifetime & generalized anxiety-lifetime; obsessive-compulsive personality disorder & social phobia-lifetime; role obligations failure & reduced activities; tolerance & drink despite problems ; time spent getting or recovering from alcohol & reduced activities ; unsuccessful to cut down & time spent getting or recovering from alcohol; tolerance & unsuccessful to cut down; major depression-lifetime & social phobia-lifetime ; major depression-lifetime & panic disorder without agoraphobia-lifetime; dysthymia-lifetime & generalized anxiety-lifetime ; major depression-lifetime & bipolar-lifetime ; major depression-lifetime & dysthymia-lifetime; age at onset of major depression<15 & major depression-lifetime ; obsessive-compulsive personality disorder & major depression-lifetime ; and, age when started drinking & age at onset of alcohol dependence.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anthenelli RM, Smith TL, Irwin MR, Schuckit MA. A comparative study of criteria for subgrouping alcoholics: the primary/secondary diagnostic scheme versus variations of the type 1/type 2 criteria. Am J Psychiatry. 1994;151:1468–1474. doi: 10.1176/ajp.151.10.1468. [DOI] [PubMed] [Google Scholar]
- Babor TF, Hofmann M, DelBoca FK, Hesselbrock V, Meyer RE, Dolinsky ZS, Rounsaville B. Types of alcoholics, I. Evidence for an empirically derived typology based on indicators of vulnerability and severity. Arch Gen Psychiatry. 1992;49:599–608. doi: 10.1001/archpsyc.1992.01820080007002. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Heath AC, Reich T, Hesselbrock VM, Kramer JR, Nurnberger JI, Jr, Schuckit MA. Can we subtype alcoholism? A latent class analysis of data from relatives of alcoholics in a multicenter family study of alcoholism. Alcohol Clin Exp Res. 1996;20:1462–1471. doi: 10.1111/j.1530-0277.1996.tb01150.x. [DOI] [PubMed] [Google Scholar]
- Cloninger CR, Bohman M, Sigvardsson S. Inheritance of alcohol abuse. Cross-fostering analysis of adopted men. Arch Gen Psychiatry. 1981;38:861–868. doi: 10.1001/archpsyc.1981.01780330019001. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100:281–292. doi: 10.1111/j.1360-0443.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- Epstein EE, Labouvie E, McCrady BS, Jensen NK, Hayaki J. A multi-site study of alcohol subtypes: classification and overlap of unidimensional and multi-dimensional typologies. Addiction. 2002;97:1041–1053. doi: 10.1046/j.1360-0443.2002.00164.x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend. 2004a;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004b;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Grant BF. The co-occurrence of DSM-IV alcohol abuse in DSM-IV alcohol dependence: results of the National Epidemiologic Survey on Alcohol and Related Conditions on heterogeneity that differ by population subgroup. Arch Gen Psychiatry. 2004;61:891–896. doi: 10.1001/archpsyc.61.9.891. [DOI] [PubMed] [Google Scholar]
- Hauser J, Rybakowski J. Three clusters of male alcoholics. Drug Alcohol Depend. 1997;48:243–250. doi: 10.1016/s0376-8716(97)00130-0. [DOI] [PubMed] [Google Scholar]
- Jacob T, Bucholz KK, Sartor CE, Howell DN, Wood PK. Drinking trajectories from adolescence to the mid-forties among alcohol dependent males. J Stud Alcohol. 2005;66:745–755. doi: 10.15288/jsa.2005.66.745. [DOI] [PubMed] [Google Scholar]
- Jellinek EM. The Disease Concept of Alcoholism. Hillhouse Press; New Brunswick: 1960. [Google Scholar]
- Kaufman LRP. Finding Groups in Data: An Introduction to Cluster Analysis. John Wiley & Sons; New York: 1990. [Google Scholar]
- Kendler KS, Karkowski LM, Prescott CA, Pedersen NL. Latent class analysis of temperance board registrations in Swedish male-male twin pairs born 1902 to 1949: searching for subtypes of alcoholism. Psychol Med. 1998;28:803–813. doi: 10.1017/s003329179800676x. [DOI] [PubMed] [Google Scholar]
- Kupfer D, First M, Regier D. A research agenda for DSM-IV. American Psychiatric Association; Washington, DC: 2002. [Google Scholar]
- Lesch OM, Dietzel M, Musalek M, Walter H, Zeiler K. The course of alcoholism. Long-term prognosis in different types. Forensic Sci Int. 1988;36:121–138. doi: 10.1016/0379-0738(88)90225-3. [DOI] [PubMed] [Google Scholar]
- Lynskey MT, Nelson EC, Neuman RJ, Bucholz KK, Madden PAF, Knopik VS, Slutske W, Whitfield JB, Martin NG, Heath AC. Limitations of DSM-IV Operationalizations of Alcohol Abuse and Dependence in a Sample of Australian Twins. Twin Research and Human Genetics. 2005;8:574–584. doi: 10.1375/183242705774860178. [DOI] [PubMed] [Google Scholar]
- Magidson J, Vermunt JK. Latent class models for clustering; A comparison with K-means. Canadian Journal of Marketing. 2002;20:37–44. [Google Scholar]
- McGue M. Behavioral genetic models of alcoholism and drinking. In: Leonard KEBHT, editor. Psychological Theories of Drinking and Alcoholism. Guilford Publications; New York, New York: 1999. pp. 372–421. [Google Scholar]
- Peritz E. Berkson's bias revisited. J Chronic Dis. 1984;37:909–916. doi: 10.1016/0021-9681(84)90067-5. [DOI] [PubMed] [Google Scholar]
- Schuckit MA. The clinical implications of primary diagnostic groups among alcoholics. Arch Gen Psychiatry. 1985;42:1043–1049. doi: 10.1001/archpsyc.1985.01790340021003. [DOI] [PubMed] [Google Scholar]
- Vailant G. Natural History of Alcoholism. Harvard University Press Publishing; Cambridge, Mass: 1983. [Google Scholar]
- Vermunt J, Magidson J. Technical Guide for Latent GOLD 4.0: Basic and Advanced. Statistical Innovations, Inc; Belmont, Mass: 2005. [Google Scholar]
- Windle M, Scheidt DM. Alcoholic subtypes: are two sufficient? Addiction. 2004;99:1508–1519. doi: 10.1111/j.1360-0443.2004.00878.x. [DOI] [PubMed] [Google Scholar]
- Wu P, Bird HR, Liu X, Fan B, Fuller C, Shen S, Duarte CS, Canino GJ. Childhood depressive symptoms and early onset of alcohol use. Pediatrics. 2006;118:1907–1915. doi: 10.1542/peds.2006-1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker RA. The four alcoholisms: A developmental account of the etiological process. In: Rivers PC, editor. Nebraska Symposium on Motivation, Alcohol and Addictive Behaviors. University of Nebraska Press; Lincoln, NE: 1987. pp. 27–83. [PubMed] [Google Scholar]