Abstract
BACKGROUND:
A large foodborne outbreak of cyclosporiasis occurred in North America in 1996. An index cluster of cases associated with a catered event on May 11, 1996, in Ontario sparked the recognition of this outbreak in Canada.
OBJECTIVES:
To describe the Ontario experience with the North American outbreak of cyclosporiasis in 1996.
PATIENTS AND METHODS:
Public health units investigated the index and subsequent event-associated clusters. Investigations included retrospective cohort studies of clusters, traceback of suspect foods and a case-control study of sporadic cases. These activities, coordinated with those in the United States, were part of an international investigation.
RESULTS:
In Ontario, 232 cases of cyclosporiasis (20 laboratory-confirmed and 72 clinically defined cases associated with seven events plus 140 additional laboratory-confirmed sporadic cases) were identified between May 1 and July 30, 1996. For the index cluster, a strawberry flan with raspberries and blueberries was the only significant exposure (relative risk 2.16, P=0.02). Fresh berries were served at all seven events associated with clusters of cases. Raspberries were definitely served at three events, possibly served at three events, and not served at one event. Only imported berries were available in Ontario in May 1996, when initial clusters and sporadic cases were identified. The raspberries served at the two events with well documented traceback data came from Guatemala. Univariate analyses of the matched case-control study demonstrated that illness was associated with consumption of raspberries (matched odds ratio 21.0, 95% CI 3.48 to 448) and strawberries (matched odds ratio 28.5, 95% CI 4.02 to 478). Further evidence amassed by the international investigation compellingly implicated Guatemalan raspberries as the vehicle of the outbreak.
CONCLUSION:
Cyclosporiasis may be acquired domestically from the consumption of contaminated produce. The scope and vehicle of this international foodborne outbreak were recognized through a coordinated public health response.
Key Words: Canada, Cyclosporiasis, Cyclospora cayetanensis, Foodborne outbreak
Cyclosporiasis is caused by ingestion of oocysts of Cyclospora cayetanensis, a parasite which was first recognized in the late 1970s (1). The clinical picture of cyclosporiasis can be indistinguishable from that of giardiasis, cryptosporidiosis and isosporiasis. The main symptom is watery diarrhea that occurs in a relapsing, cyclical pattern, lasting for several days to weeks; it is often associated with weight loss and fatigue. In immunocompromised hosts, especially those with AIDS, the duration and severity of illness may be increased (2). The recommended treatment for cyclosporiasis is a seven-day course of trimethoprim/sulphamethoxazole, but patients with AIDS may require both longer courses of therapy and maintenance therapy (2,3).
Cyclospora oocysts, measuring 8 to 10 μm in diameter, are recognized as nonrefractile spheres (containing refractile globules) on light microscopic examination of wet preparations of stool. With modified acid-fast staining, some oocysts may stain deep red, others may stain pink and still others may remain unstained as glassy, membranous oocysts (4).
Foodborne and waterborne transmission are now well established (5-7). Before 1995, outbreaks were infrequent and usually associated with waterborne transmission (5,6). In Canada before 1996, case reports were associated with travellers returning from developing countries (8). In Ontario, Brennan et al (9) reported an estimated prevalence of 0.5 cases/1000 stool examinations based on a survey examining 80,000 stool samples submitted to three parasitology laboratories from June 1993 through June 1995 (9).
In May 1996, the North York Public Health Department in Ontario was notified by a local primary care physician of several cases of cyclosporiasis among guests who had attended a wedding reception on May 11, 1996. Simultaneously, another cluster of cases was being investigated in Houston, Texas; and several state health departments in the United States reported an increased number of cases of cyclosporiasis to the Centers for Disease Control and Prevention, Atlanta, Georgia (CDC). These clusters and sporadic cases were ultimately recognized as part of a North American outbreak of cyclosporiasis for which preliminary investigations implicated both strawberries and raspberries. This paper describes the Ontario experience with the North American outbreak of cyclosporiasis in 1996.
PATIENTS AND METHODS
The index Ontario cluster was investigated by the North York Public Health Department, Toronto, Ontario (10). Initially, cases were ascertained and an environmental inspection of the implicated venue was conducted. Thereafter, a retrospective cohort study examined food and water consumption by attendees. For this first cluster, a case was defined as having three or more unexplained loose or watery bowel movements/day for three consecutive days, or a stool specimen positive for cyclospora oocysts.
Further case finding and cluster identification:
Laboratories do not routinely look for cyclospora oocysts in stools submitted for 'ova and parasite' testing. To facilitate the diagnosis of cases and to enhance surveillance, the Ontario Ministry of Health, Toronto, Ontario requested that laboratories in Ontario report when cyclospora oocysts were identified in stool specimens and that public health units interview all laboratory-confirmed cases with a structured questionnaire. The sporadic case questionnaire gathered information about demographics, travel history outside Ontario and North America, and consumption of strawberries, raspberries, blackberries, blueberries and other fresh produce during the two weeks before the onset of symptoms.
A sporadic case was defined as a person with a stool specimen positive for cyclospora oocysts during May 1 through July 30, 1996 who did not travel overnight outside North America in the four weeks before illness and who was not associated with a cluster. Clinical cases associated with clusters were defined in a similar manner as for the index cluster. Clusters were defined as two or more cases associated with a common event, with at least one case being laboratory-confirmed by a reference laboratory (Ontario Provincial Laboratory, Toronto, Ontario or CDC). The local public health unit(s) performed cluster investigations. Provincial and territorial epidemiologists across Canada were notified about the investigations in Ontario and the United States.
Traceback investigations:
The Canadian Food Inspection Agency, Ottawa, Ontario, Health Canada and the public health inspectors of the specific health units carried out traceback investigations with assistance from the Ontario Ministry of Health. Only imported berries were available for sale in Ontario when the initial events occurred. Airway bill numbers of imported berries likely served at the implicated events were provided to the CDC and United States Food and Drug Administration (FDA) to trace the sources of the berries to the exporters and farms that contributed to specific shipments. Traceback activities in Canada were coordinated with the extensive activities in the United States. A well documented traceback of produce was considered one that confirmed verbally and in writing (eg, through copies of invoices) all steps from consumers back to farms (7).
Case-control study:
A matched case-control study was conducted to determine further whether consumption of berries was associated with cyclospora infection in Ontario. Sporadic cases were included if they were Ontario residents at least age 18 years and had an onset of symptoms by July 1, 1996. Sporadic cases were excluded if other enteric pathogens were identified on stool examination.
Potential neighbourhood and age-matched controls were interviewed by telephone. Inclusion criteria for controls were no gastrointestinal illness on or after May 1, 1996, no foreign travel during the four weeks before onset of illness of the matched case and no more than three nights spent outside of Ontario during the two weeks before onset of illness of the matched case.
A structured questionnaire gathered information about consumption of fresh berries and other fresh fruits and vegetables, domestic water supply and water consumption, and exposures to domestic animals and soil. Cases and their matched controls were questioned about exposures during the two weeks before the relevant case's onset of illness. Cases and controls were interviewed from July 4 to July 27, 1996.
Statistical analysis:
For analyses of the clusters of cases, univariate relative risks were calculated for exposure variables, and two-tailed P values were computed with $#x03C7;2 test or, if appropriate, Fisher's exact test. For the case-control study univariate analyses were performed in EPI INFO 6.04 (CDC, Atlanta, Georgia). Continuous variables were dichotomized into high and low categories by the median. Mantel-Haenszel matched odds ratios and confidence intervals determined by the exact 95% percent mid-P limits. Conditional logistic regression was performed in LogXact (Cytel Corp, Cambridge, Massachusetts).
RESULTS
Event-associated clusters:
In the index cluster, 35 of the 49 guests became ill (attack rate 71%). The median incubation period was eight days (range six to 13 days). Only symptomatic persons submitted stool specimens for laboratory testing, of whom 13 (59%) of the 22 were positive for cyclospora oocysts. The epidemic curve (Figure 1) was consistent with a point-source outbreak. No secondary cases were identified. Analyses of food exposures (Table 1) showed that the strawberry flan with raspberries and blueberries was the only food item significantly associated with illness (relative risk 2.16, P=0.02).
Figure 1.
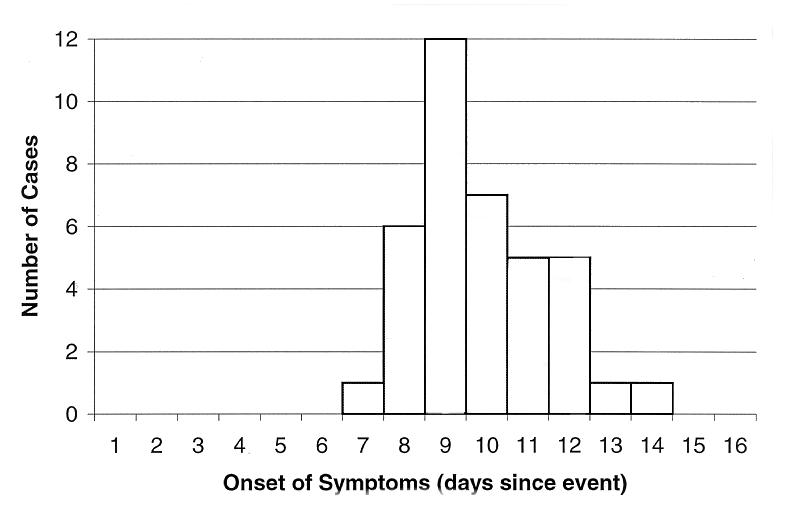
Epidemic curbe for the index Ontario cylosporiasis cluster, event data, May 11, 1996 (n=35 cases)
TABLE 1.
Food exposures and risk of developing illness in the index cluster in an outbreak of cyclosporiasis in Ontario in 1996
| Food item* | Attack rate in the exposed† | Attack rate in unexposed | Relative risk | P |
|---|---|---|---|---|
| Strawberry flan with raspberries and blueberries | 0.81 (30/37) | 0.38(3/8) | 2.16 | 0.02‡ |
| Caesar salad | 0.71 (24/34) | 0.5 (5/10) | 1.42 | 0.27‡ |
| Chulent (booked beef) | 0.77 (20/26) | 0.64 (14/22) | 1.20 | 0.31 |
| Corned beef | 0.77 (17/22) | 0.65 (17/26) | 1.18 | 0.37 |
| Chicken | 0.83 (15/18) | 0.67 (20/30) | 1.25 | 0.32‡ |
| Egg salad | 0.71 (15/21) | 0.71 (20/28) | 1.00 | 1.00 |
| Water | 0.78 (14/18) | 0.62 (16/26) | 1.26 | 0.26 |
| Tea | 0.71 (12/17) | 0.70 (21/30) | 1.01 | 0.97 |
| Tomato salad | 0.67 (4/6) | 0.73 (29/40) | 0.92 | 1.00‡ |
Food items shown include all the fresh produce and the cooked items with highest relative risk and statistical significance;
People who recalled eating the food item. The food items are ranked by frequency of exposure in cases.
Fisher's exact p-value
By the end of July 1996, enhanced cluster surveillance identified six additional event-associated clusters of cases. All seven clusters are summarized in Table 2. The events occurred from May 11 through June 14, 1996. Of the 213 persons attending these seven events, 164 (77%) were interviewed. Among these, 20 laboratory-confirmed and 72 additional clinically defined cases of cyclosporiasis were identified. The overall attack rate was 56% (94 of 168). Cluster-specific attack rates ranged from 30% to 71%, and the median of the cluster-specific incubation periods was eight days. The incubation period for all 94 individual cases varied from two to 14 days.
TABLE 2.
Summary of the seven clusters of cyclosporiasis in Ontario, 1996 (by event date)
| Event # | Date of event | Description | Attendees | Attack rate (cases/attendees interviewed) | Number of laboratory-confirmed cases | Berry consumption | Raspberries served at event | Well documented rapberry (blackberry) traceback | Relative risk and P |
|---|---|---|---|---|---|---|---|---|---|
| 1 | May 11 | Wedding (North York) | 49 | 71% (35/49) | 13 | Strawberry flan with rapberries and blueberries | Definitely served | Yes, Guatemalan farms | 2.16 P=0.02 |
| 2 | May 11 | Dinner party (Toronto) | 20 | 75% (12/16) | 1 | Fresh raspberries and blueberries | Definitely served | No | NA |
| 3 | May 15 | Soccer team meal (Ottawa) | 14 | 50% (6/12) | 1 | Fruit salad with strawberries and blackberries | Not served | Yes, Guatemalan farm (blackberries) | RR=undefinted P=0.002 |
| 4 | May 17-19 | Private parties (North York) | 50 | 31% (8/26) | 1 | Chocolate dipped and plain strawberries, likely other berries | Probably served | No | No |
| 5 | May 28 | Business luncheon (Toronto) | 32 | 52% (11/21) | 1 | Fresh fruit flan (with various berries) | Probably served | No | NA |
| 6 | June 1 | Bridal shower (Toronto) | 22 | 55% (12/22) | 2 | Cake garnished with strawberries, rapberries and blueberries | Definitely served | Yes, Guatemalan farms | 4.2 P=0.02 |
| 7 | June 9-14 | Business seminar (Caledon) | 26 | 56% (10/18) | 1 | Fruit salad with various berries | Probably served | No | NA |
NA Not applicable, food exposure data were not obtained from the attendees
For all events, food recall histories indicated that various mixtures of raspberries, strawberries, blackberries and blueberries were served. Raspberries were definitely not served at only one event (#3), an event at which blackberries from Guatemala were served. The tracebacks that were well documented demonstrated that raspberries served at events #1 and #6 originated from the same Guatemalan exporter and the blackberries from event #3 originated from another Guatemalan exporter. Although tracebacks for the other events did not fulfill the criteria of being well documented, only berries from outside Canada were available during the outbreak period.
Sporadic cases:
From May 1, 1996, through July 30, 1996, 140 sporadic cases were reported to the Ontario Ministry of Health. For the 131 cases for whom sex and age information was available, the median age was 46 years (range 12 to 85 years) and 47% (n=62) were male. Public health unit personnel completed questionnaires for 74 sporadic cases. No cases were hospitalized, nor were there any reported deaths. The proportion of sporadic cases who, during the two weeks before illness onset, reportedly ate raspberries was 42% (30 of 72), strawberries 78% (56 of 72), blueberries 24% (17 of 70) and blackberries 7% (five of 69).
Case-control study:
Twenty-six of the 140 sporadic cases and 52 controls were interviewed for the case-control study. Thirty-eight per cent (n=10) of the cases and 33% (n=17) of controls were men. The median ages of the cases and controls were 42 years (range 19 to 76 years) and 41 years (range 18 to 87 years), respectively. Cases were significantly more likely than their matched controls to have completed postsecondary education (matched odds ratio [MOR]=7.33; 95% CI 1.89 to 28.0).
For cases, the predominant symptoms were diarrhea (96%), fatigue (96%), weight loss (96%), increased gas or bloating (88%), abdominal pain (77%), nausea (61%), head ache (54%) and fever (38%). The median weight loss was 3 kg (maximum 8.0 kg). The onsets of illness were from May 16 to June 26, 1996. All 26 cases consulted physicians for their illness; none were hospitalized. Trimethoprim/sulphamethoxazole was prescribed to 81% of the cases. The median duration of diarrhea was 13 days (range zero to 28 days), not accounting for whether the cases had been treated. Three cases reported having a medical condition affecting their immune system, but none reported having HIV infection, organ transplantation, diabetes or inflammatory bowel disease, or taking oral steroid medication. Five cases reported taking antacids, and two reported taking ulcer medication. Six patients had made overnight trips outside Ontario but within North America.
All cases and 96% (n=50) of the controls reported eating fresh fruit during the two-week exposure period. All cases and 98% (n=51) of the controls reported that they usually washed fruit before they ate it. There were no differences between cases and their matched controls in the number of servings of fresh fruit or raw vegetables consumed daily. In the univariate analyses, illness was associated with consumption of strawberries (MOR=28.5, 95% CI 4.02 to 478), raspberries (MOR=21.0, 95% CI 3.48 to 448), blackberries (MOR=undefined, 95% CI 0.82 to infinity) and blueberries (MOR=6.5, 95% CI 1.38 to 44.8). Illness was not associated with consumption of other fruits, place of fruit purchase, consumption of tap water or exposure to untreated water or animals. Analyses are summarized in Table 3.
TABLE 3.
Results of the matched case-control study (casees 26; controls 52) in an outbreak of cyclosporiasis in Ontario in 1996
| Variable | Cases n (%) | Controls n (%) | Matched odds ratio | 95% CI |
|---|---|---|---|---|
| Univariate analysis | ||||
| Completed postsecondary education | 21 (81) | 23 (44) | 7.3 | 1.89-28.0 |
| Strawberries | 24 (92) | 19 (36) | 28.5 | 4.02-478 |
| Cantaloupes | 17 (65) | 21 (40) | 3.8 | 1.21-13.6 |
| Raspberries | 11 (42) | 2 (4) | 21.0 | 3.48-448 |
| Blueberries | 8 (31) | 4 (8) | 6.5 | 1.38-44.8 |
| Peaches | 5 (19) | 13 (25) | 0.7 | 0.18-2.31 |
| Blackberries | 3 (12) | 0 | Undefined | 0.82-infinity |
| Fruit consumption more than one serving/day | 12 (46) | 16 (31) | 0.9 | 0.34-2.69 |
| Place of fruit purchase | ||||
| Supermarket | 20 (77) | 40 (77) | 1.0 | 0.33-3.36 |
| Street vendor | 3 (12) | 2 (4) | 3.0 | 0.45-25.2 |
| Farmer's market | 3 (12) | 5 (10) | 1.2 | 0.22-6.21 |
| Green grocer | 10 (38) | 13 (25) | 2.4 | 0.66-5.55 |
| Any raw vegetables | 23 (88) | 46 (88) | 1.2 | 0.25-9.30 |
| Raw vegetable consumption more than one serving/day | 5 (21) | 18 (35) | 0.5 | 0.12-1.84 |
| Tap water more than two glasses/day | 9 (36) | 29 (55) | 0.5 | 0.17-1.21 |
| Any untreated drinking water | 2 (8) | 6 (12) | 0.6 | 0.08-3.38 |
| Pets at home | 13 (50) | 21 (40) | 1.4 | 0.56-3.81 |
| Multivariate analysis | ||||
| Strawberries | 13.8 | 2.35-infinity% | ||
| Raspberries | 6.3 | 0.86-277* | ||
| Completed postsecondary education | 5.3 | 0.77-infinity* |
Exact CI
Consumption of strawberries was the only statisically significant risk factor in a conditional logistics regression model that included all types of berry consumption and education. The final model excluded blueberries and blackberries, in part, because of the infrequent consumption of these berries.
DISCUSSION
By the end of August 1996, 1465 cases of cyclosporiasis were reported in North America (740 sporadic and 725 cases related to 55 clusters) (7). Preliminary investigations suggested a possible common source for this outbreak. Although several berries including strawberries were initially suspect, Guatemalan raspberries were ultimately implicated. This conclusion was based on the strength of the cumulative evidence gathered in many jurisdictions, thus highlighting the importance of the coordinated multiagency response led by the CDC.
Several key factors were crucial to the initial identification and investigation of this outbreak. A family physician was responsible for reporting the first cluster of cases of cyclosporiasis in Ontario. Subsequently, the municipal public health unit notified provincial public health authorities when local investigations raised concerns of a widespread and ongoing outbreak. The additional event-associated clusters and sporadic cases in Ontario were recognized in part because Ontario laboratories and health units received specific directions to facilitate diagnosis and enhance surveillance. The initial responses from the local primary and public health systems are testimony to their important role in surveillance and control of communicable diseases, including emerging infectious diseases.
The different components of the outbreak investigation in Canada (cohort cluster investigations, a case-control study of sporadic cases, and the traceback of berries to a common source) and the necessity of combining evidence from investigations in other jurisdictions, each have potential strengths and limitations. An important limitation of the Ontario case-control study was potential recall bias from media attention on strawberries. Patients with cyclosporiasis may have been more likely to recall eating strawberries than other produce, thereby increasing the likelihood of an observed association. In several American case-control studies that were performed earlier than the Ontario study, consumption of fresh raspberries was most strongly associated with illness (7). The potential for recall bias was less likely in the cluster investigations compared with the case-control study because persons were interviewed earlier and specifically about food eaten at a single event. At these events, however, the berry items included mixtures of berries and only three of seven clusters had well documented food histories. Tracing food to a contaminated common source can potentially provide strong direct evidence of causal association. However, tracebacks of fresh produce in general, and berries in particular, are often difficult to perform. Only two of the six cluster-associated events (events £1 and £6) in Ontario at which raspberries were definitely or probably served had well documented traceback data.
Raspberry exports from Guatemala to Canada are routed via the United States and occur primarily in the spring and fall. From March 23 to July 7, 1996, Guatemalan raspberries represented approximately 10% of the 88,565 kg of raspberries imported into Canada (personal communication, Horticulture Section, Agriculture and Agri-Food Canada, 1996). Of the Guatemalan raspberries imported during this period, 86% were imported from May 1 to June 22 when the cluster-associated events occurred. During this period, Guatemalan raspberries were not imported into British Columbia, Manitoba, Saskatchewan or the Atlantic Provinces and no increase in cases of cyclosporiasis was identified in these provinces. From May 1 to June 22, 1996, 79% of the Guatemalan raspberries were imported into Quebec, where only one cluster and a few sporadic cases of cyclosporiasis were reported, whereas only 20% were imported into Ontario. Enhanced surveillance, availability of laboratory diagnostic testing and uneven distribution of contaminated raspberries could have contributed to the burden of disease identified in Ontario.
After the outbreak in 1996, Guatemalan berry growers voluntarily introduced control measures that focused on improving sanitary conditions and water quality on individual farms (11). Even so, in the spring of 1997, a cyclosporiasis outbreak in North America was associated with Guatemalan raspberries (11); during this time, raspberries were imported from only those farms classified by the Guatemalans as low risk. In 1997, outbreaks of cyclosporiasis in the United States were also associated with consumption of mesclun lettuce and fresh basil (12). In the spring of 1998, a cyclosporiasis outbreak associated with Guatemalan raspberries was identified in the Toronto area but not elsewhere (13,14). Until June 9, 1998, raspberries from low risk farms continued to be imported into Canada; no Guatemalan raspberries were imported into the United States in the spring of 1998. The mode of raspberry contamination has not been identified for any of these outbreaks. As of December 1999, the fall and winter crop (November and December) of Guatemalan raspberries, that was harvested and packed under a new and more stringent system, was allowed to be imported into Canada. Health Canada and the Canadian Food Inspection Agency are currently reviewing the importation policy for the spring crop (April and June) of Guatemalan raspberries and blackberries (personal communication, René Cardinal, Canadian Food Inspection Agency, 2000). Cyclosporiasis was made a nationally notifiable disease in Canada on January 1, 2000.
These outbreaks of cyclosporiasis in North America have established cyclospora as a foodborne pathogen and cyclosporiasis as a disease that is not restricted to travelers returning from developing countries. Laboratory diagnosis of cyclosporiasis is necessary to detect outbreaks and to differentiate the clinical presentation from that seen with other enteric pathogens. In addition, specific medical treatment (ie, with trimethoprim/sulphamethoxazole [3]) is available once cyclosporiasis is diagnosed.
In the past, foodborne outbreaks were often thought of as local events, affecting a group of people eating at a restaurant or attending a social event (15). With globalization of food products, the impact of foodborne outbreaks is also globalized. Local, national and international organizations and agencies need to work closely together to strengthen global surveillance and the capacity to control, and prevent, future outbreaks (15). The investigation of this international outbreak of cyclosporiasis in 1996 demonstrated the importance of a coordinated, multijurisdictional public health response.
Acknowledgments
The authors thank Mariana Grmusa and Wayne Lee, Public Health Inspectors, North York Health Department, Toronto, Ontario; Doug Morrison, Mary Anne Rose and Jeff Wilson, Health Canada, Ottawa, Ontario; Maria Arrieta, Montreal Children's Hospital, Montreal, Quebec; Michael Brodsky and T Scholten, Ontario Ministry of Health, Toronto, Ontario; Brian Ward, Montreal General Hospital, Montreal, Quebec; John Carsley, Montreal Public Health Department, Montreal, Quebec; Idera Rusen, Community Medicine Resident, University of Toronto, Toronto, Ontario; Michael Arrowood and Susanne Wahlquist, Division of Parasitic Diseases, National Center for Infectious Diseases, Centers for Disease Control and Prevention, Atlanta, Georgia, for their invaluable support during the cyclosporiasis investigations.
References
- 1.Ashford RW. Occurrence of an undescribed coccidian in man in Papua New Guinea.Ann Trop Med Parasitol 1979;73:497-500. [DOI] [PubMed] [Google Scholar]
- 2.Pape WJ, Verdier RI, Boncy M, Boncy J, Johnson WD Jr. Cyclospora infection in adults infected with HIV. Clinical manifestations, treatment and prophylaxis.Ann Intern Med 1994;121:654-7. [DOI] [PubMed] [Google Scholar]
- 3.Hoge CW, Shlim DR, Ghimire M, et al. Placebo-controlled trial of cotrimoxazole for cyclospora infections among travelers and foreign residents in Nepal.Lancet 1995;345:691-3. [Erratum, Lancet 1995;345:1060] [DOI] [PubMed] [Google Scholar]
- 4.Garcia LS, Bruckner DA. Diagnostic Medical Parasitology, 3rd edn.Washington: American Society for Microbiology, 1997:66-9. [Google Scholar]
- 5.Huang P, Weber JT, Sosin DM, et al. The first reported outbreak of diarrheal illness associated with cyclospora in the United States.Ann Intern Med 1995;123:409-14. [DOI] [PubMed] [Google Scholar]
- 6.Rabold JG, Hoge CW, Shlim DR, Kefford C, Rajah R, Echeverria P. Cyclospora outbreak associated with chlorinated drinking water.Lancet 1994;344:1360-1. [DOI] [PubMed] [Google Scholar]
- 7.Herwaldt BL, Ackers ML,. An outbreak in 1996 of cyclosporiasis associated with imported raspberries. The Cyclospora Working Group.N Engl J Med 1997;336:1548-56. [DOI] [PubMed] [Google Scholar]
- 8.Purych DB, Perry IL, Bulawka D, Kowalewska-Grochowska KT, Oldale BL. A case of cyclospora infection in an Albertan traveller.Can Commun Dis Rep 1995;21:88-91. [PubMed] [Google Scholar]
- 9. Brennan MK, MacPherson DW, Palmer J, Keystone JS. Cyclosporiasis: a new cause of diarrhea.CMAJ 1996;155:1293-6. [PMC free article] [PubMed] [Google Scholar]
- 10.Manuel DG, Shahin R, Lee W, Grmusa M. The first reported cluster of food-borne cyclosporiasis in Canada.Can J Pub Health 1999;90:399-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Herwaldt BL, Beach MJ. The return of cyclospora in 1997: Another outbreak of cyclosporiasis in North America. Cyclospora Working Group.Ann Intern Med 1999;130:210-20. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Outbreak of cyclosporiasis - Northern Virginia-Washington, DC-Baltimore, Maryland, metropolitan area, 1997.MMWR Morb Mortal Wkly Rep 1997;46:689-91. [PubMed] [Google Scholar]
- 13.Outbreak of cyclosporiasis - Ontario, May 1998.Can Commun Dis Rep 1998;24:153-6. [PubMed] [Google Scholar]
- 14.Buck P, Huang S, Pichette S, et al. Raspberries and cyclospora: not a berry healthy combination! International Clinical Epidemiology Network (INCLEN) XVI Global Meeting. March 1999, Bangkok, Thailand. [Google Scholar]
- 15.Tauxe RV, Hughes JM. International investigation of outbreaks of foodborne disease.BMJ 1996;313:1093-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


