Abstract
BACKGROUND:
While several studies have reported on sexual risk behaviours and the prevalence of sexually transmitted infections (STIs) among injection drug users (IDUs), there are fewer prospective studies that have been able to examine populations of IDUs with no history of STIs. Therefore, the authors examined prevalence, correlates and factors associated with time to first STI infection in a prospective cohort of IDUs in Vancouver, British Columbia.
METHODS:
The authors examined the prevalence and correlates of STIs among IDUs at the time of recruitment into a prospective cohort study. The authors also evaluated the cumulative rate of time to first STI among IDUs with no history of STIs at baseline using the Kaplan-Meier method, and modelled factors independently associated with first STI using Cox regression.
RESULTS:
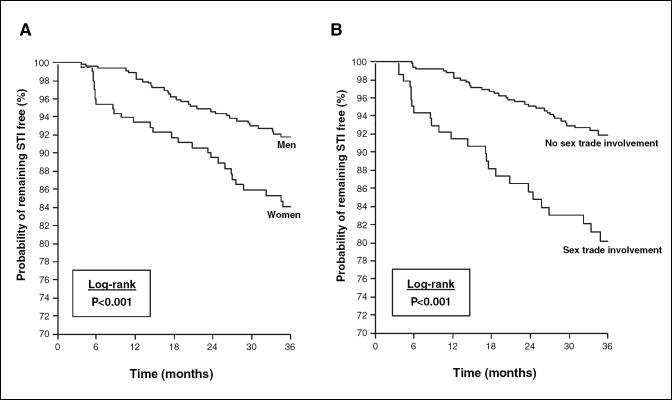
Between May 1996 and November 2003, 1560 individuals were recruited into the cohort; of these individuals, 745 reported a history of STI at baseline. Among the 815 who did not report an STI at baseline, 671 (82%) had at least one follow-up visit and were eligible for the analysis of time to first STI. After 36 months of follow-up, the cumulative rate of first STI was 8.2% for men and 15.9% for women (log-rank P<0.001), whereas the cumulative rate of first STI was 8.0% for IDUs who did not report sex trade involvement versus 19.8% for IDUs who reported sex trade involvement (log-rank P<0.001). In multivariate analyses, the risk of first STI remained independently associated with unprotected sex with regular partners (relative hazard=2.04, 95% CI 1.29 to 3.23; P=0.001) and unprotected sex with sex trade clients (relative hazard=2.36, 95% CI 1.46 to 3.82; P=0.005).
CONCLUSIONS:
In the present study, the authors found that STIs were associated with both regular sex partnerships and sex trade involvement. These findings are of particular concern because both unprotected sex with regular partners and sex trade involvement is common among IDUs. Interventions to encourage condom use among IDUs, particularly those with regular sex partners and those involved in the sex trade, should be further developed.
Key Words: IDU, Prospective cohort, STI
The high prevalence of sexually transmitted infections (STIs) among injection drug users (IDUs) has been documented previously (1-5). As well, STIs may be more prevalent in IDUs than in the general population (1). The elevated prevalence of STIs among IDUs may largely be due to the high number of IDUs involved in the sex trade (2). Furthermore, sexual risk behaviours with noncommercial sexual partners are common among IDUs, which places IDUs at additional risk of STIs (2,6,7). A recent study of IDUs from Vancouver, British Columbia, reported extremely high numbers of sexual partners among IDUs and relatively low rates of condom use with casual partners (2).
While several studies have reported on sexual risk behaviours and the prevalence of STIs among IDUs (2,3,5), there are fewer prospective studies that have examined populations of IDUs with no history of STIs to determine the factors associated with time to first STI. This may be of particular concern in Vancouver due to the widespread use of injected cocaine and crack cocaine (2,8,9); the use of these drugs has been associated with a higher incidence of risky sexual behaviours than other illicit drugs, including heroin (7,10). We have recently demonstrated (11) that there may be an elevated risk of HIV infection among drug-using women in Vancouver as a result of elevated sexual risk behaviour, suggesting that substantial risky sexual behaviours occur in this population. We therefore examined prevalence, correlates and factors associated with time to first STI infection in a prospective cohort of IDUs.
Methods
In May 1996, the Vancouver Injection Drug User Study (VIDUS) began to enroll IDUs into an ongoing prospective cohort study (12,13). As of November 2003, 1560 study subjects had been recruited through self-referral and street outreach. Data collection for the project was conducted in a storefront office in the downtown of eastside Vancouver, an area of about 10 city blocks, where approximately 5000 IDUs resided (14). Persons were eligible for VIDUS if they had injected illicit drugs at least once during the previous month, resided in the greater Vancouver region and provided written, informed consent. Evidence of recent injection drug use was required in the form of needle tracks. At baseline and at six-month intervals, subjects provided blood samples for HIV and hepatitis C virus serology and completed an interviewer-administered questionnaire. The questionnaire collected sociodemographic data, including housing, illicit drug use, HIV risk behaviours and attendance at syringe exchange programs. Participants were provided with a nominal monetary stipend ($20) at each study visit. Pre- and post-test counselling was also available throughout the study. Ethical approval for the project was provided by the University of British Columbia's Ethics Committee on Human Experimentation. All participants who were HIV-negative at enrollment and had at least one follow-up visit were eligible for inclusion in the present analyses.
As a preliminary analysis, the authors examined the prevalence and correlates of ever having had an STI at the time of recruitment into the cohort. In all analyses, STIs were based on self-report to the nurse's questionnaire that dealt with health-related issues. Those individuals who reported ever having had an STI were compared with those who reported never having had an STI. Among participants who reported never having had an STI at baseline, the authors evaluated the incidence rate of first STI. Cumulative STI rates were calculated using the Kaplan-Meier method, and STI incidence rates were compared using the log-rank test.
Variables of interest in these analyses included age, sex, housing, place of residence, incarceration, sex trade involvement, frequency of heroin and cocaine injection, participation in methadone maintenance therapy, and condom use with regular, casual partners or sex trade clients (11,15). Sex trade involvement was defined as exchanging sex for money, goods, drugs, shelter or anything else (16). All of the behavioural variables referred to the six-month period before the interview, with the exception of housing status, which referred to the current housing situation at the time of the interview. Sociodemographic variables such as age and sex were treated as fixed covariates, whereas behavioural variables, such as frequency of drug use and sex trade involvement, were treated as time-updated covariates in the univariate Cox regression analyses. The authors prepared adjusted analyses by using an a priori-defined model-building protocol that adjusted for all variables that were statistically significant at the P<0.1 level in bivariate analyses. Because the authors were aware of the potential for significant collinearity between activities (ie, sex and sex trade involvement), in instances where significant collinearity was observed, covariates were excluded if they were assumed to be a risk marker for causal activities. All statistical analyses were performed using SAS software (version 8.0, SAS, USA).
Results
Between May 1996 and November 2003, 1560 individuals were recruited into the cohort; of these individuals, 745 reported a history of STI at baseline. These STIs included gonorrhea (n=372), nongonococcal urethritis (n=37), chlamydia (n=214), herpes (n=105), genital warts (n=124), syphilis (n=66), cervicitis (n=5), pelvic inflammatory disease (n=61), unknown STI (n=68) and 'other' (n=45). The baseline characteristics of the overall population of participants, stratified by a history of STI at baseline, are shown in Table 1. Persons reporting an STI at baseline, in comparison with persons that did not report an STI, were more likely to be older, female, cocaine users, living in the downtown eastside of Vancouver (the HIV epicentre), involved in the sex trade, and enrolled in methadone maintenance therapy. These persons were also more likely to have had protected sex with casual partners and unprotected sex with sex trade clients (Table 1). Persons with and without an STI at baseline did not differ with respect to housing stability, incarceration, heroin use or unprotected sex with regular partners.
TABLE 1.
Baseline characteristics of Vancouver Injection Drug User Study (VIDUS) participants enrolled between May 1996 and November 2003 (n=1560)
| Characteristic | Has STI, n (%) (n=745) | No STI, n (%) (n=815) | OR (95% CI) | P |
|---|---|---|---|---|
| Age, years | ||||
| Median (IQR) | 35 (28-41) | 32 (25-39) | 2.07 (1.65-2.59) | <0.001 |
| Sex | ||||
| Men | 415 (56) | 580 (71) | ||
| Women | 330 (44) | 235 (29) | 1.96 (1.59-2.42) | <0.001 |
| Unstable housing* | ||||
| Yes | 460 (62) | 507 (62) | 0.98 (0.80-1.20) | 0.851 |
| No | 285 (38) | 308 (38) | ||
| Reside in an HIV epicentre* | ||||
| Yes | 450 (60) | 448 (55) | 1.25 (1.02-1.53) | 0.030 |
| No | 295 (40) | 367 (45) | ||
| Incarceration† | ||||
| Yes | 237 (32) | 283 (35) | 0.88 (0.71-1.08) | 0.223 |
| No | 508 (68) | 532 (65) | ||
| Sex trade work† | ||||
| Yes | 269 (36) | 175 (21) | 2.07 (1.65-2.59) | <0.001 |
| No | 476 (64) | 640 (79) | ||
| Daily heroin injection† | ||||
| Yes | 324 (43) | 341 (42) | 1.07 (0.88-1.31) | 0.511 |
| No | 421 (57) | 474 (58) | ||
| Daily cocaine injection† | ||||
| Yes | 342 (46) | 328 (40) | 1.26 (1.03-1.54) | 0.024 |
| No | 403 (54) | 487 (60) | ||
| Enrolled in MMT* | ||||
| Yes | 104 (14) | 65 (8) | 1.87 (1.35-2.60) | <0.001 |
| No | 641 (86) | 750 (92) | ||
| Unprotected sex with regular partners† | ||||
| Yes | 126 (17) | 130 (16) | 1.07 (0.82-1.40) | 0.608 |
| No | 619 (83) | 685 (84) | ||
| Unprotected sex with casual partners† | ||||
| Yes | 108 (15) | 173 (21) | 0.63 (0.48-0.82) | <0.001 |
| No | 637 (86) | 642 (79) | ||
| Unprotected sex with sex trade clients† | ||||
| Yes | 219 (29) | 165 (20) | 1.64 (1.30-2.07) | <0.001 |
| No | 526 (71) | 650 (80) |
Indicates current activities;
Indicates activities during previous six months. IQR Interquartile range; MMT Methadone maintenance therapy; STI Sexually transmitted infection
Time to first STI
Among the 815 individuals who did not report an STI at baseline, 671 (82%) had at least one follow-up visit and were eligible for the analysis of time to first STI. Of the 671 participants who did not have any STIs at baseline, 93 individuals became infected with an STI during the follow-up period, yielding a cumulative incidence rate of 3.24/100 person-years (95% CI 2.62 to 3.97). These STIs included gonorrhea (n=20), chlamydia (n=12), herpes (n=24), genital warts (n=10), trichomonas (n=4), syphilis (n=15), unknown STI (n=5) and 'other' (n=6).
The Kaplan-Meier analysis of time to first STI, stratified by sex and sex trade involvement, is shown in Figure 1. After 36 months of follow-up, the cumulative rate of first STI was 8.2% among men versus 15.9% among women (log-rank P<0.001). The cumulative rate of first STI was 8.0% for IDUs who did not report sex trade involvement versus 19.8% for IDUs who reported sex trade involvement (log-rank P<0.001) after 36 months of follow-up. The univariate Cox regression analyses of factors associated with time to first STI are shown in Table 2. The factors associated with time to first STI in the univariate analysis included younger age, female sex, sex trade involvement and unprotected intercourse with regular partners or sex trade clients. The authors observed that there was a statistically significant correlation between sex trade involvement and female sex, and also between sex trade involvement and unprotected intercourse with sex trade clients. In the final models, the authors sought to examine whether there was an independent association between unprotected intercourse with regular partners and incident STIs, and between unprotected sex with sex trade clients and incident STIs. Here, when the authors adjusted for age (relative hazard [RH]=0.95, 95% CI 0.92 to 0.97; P<0.001 per year older), the risk of first STI remained independently associated with unprotected sex with regular partners (RH=2.04, 95% CI 1.29 to 3.23; P=0.001) and unprotected sex with sex trade clients (RH=2.36, 95% CI 1.46 to 3.82; P=0.005).
Figure 1.
Kaplan-Meier analysis of the cumulative rate of time to first sexually transmitted infection (STI) among injection drug users stratified by sex (A) and sex trade involvement (B)
TABLE 2.
Univariate Cox regression analysis of factors associated with time to first sexually transmitted infection among participants between May 1996 and November 2003 (n=671)
| Variable | Unadjusted relative hazard | 95% CI | P |
|---|---|---|---|
| Age | |||
| (per year older) | 0.94 | (0.91-0.96) | <0.001 |
| Sex | |||
| (women versus men) | 2.18 | (1.45-3.27) | <0.001 |
| Unstable housing | |||
| (yes versus no) | 1.16 | (0.77-1.75) | 0.483 |
| Reside in an HIV epicentre* | |||
| (yes versus no) | 1.48 | (0.98-2.24) | 0.063 |
| Incarceration† | |||
| (yes versus no) | 1.09 | (0.70-1.70) | 0.689 |
| Sex trade involvement† | |||
| (yes versus no) | 2.98 | (1.87-4.73) | <0.001 |
| Daily cocaine injection† | |||
| (yes versus no) | 1.27 | (0.80-2.01) | 0.317 |
| Daily heroin injection† | |||
| (yes versus no) | 1.01 | (0.65-1.56) | 0.981 |
| Enrolled in MMT* | |||
| (yes versus no) | 0.79 | (0.48-1.31) | 0.360 |
| Unprotected intercourse with regular partners† | |||
| (yes versus no) | 2.18 | (1.38-3.44) | <0.001 |
| Unprotected intercourse with casual partners† | |||
| (yes versus no) | 1.40 | (0.84-2.36) | 0.200 |
| Unprotected intercourse with sex trade clients† | |||
| (yes versus no) | 2.95 | (1.84-4.71) | <0.001 |
Indicates current activities;
Indicates activities occurring during the previous six months. MMT Methadone maintenance therapy
Conclusions and Discussion
In the present study, we found that persons diagnosed with an STI at baseline were more likely than individuals who were not diagnosed with an STI to be older, female, daily cocaine users, living in the downtown eastside of Vancouver (the HIV epicentre), involved in the sex trade, and enrolled in methadone maintenance therapy. These persons were also more likely to have had protected sex with casual partners and unprotected sex with sex trade clients. We found that first incident STI was associated with younger age, female sex, sex trade involvement, and unprotected sex with regular partners or sex trade clients.
While harm reduction efforts targeting IDUs have typically focused on reducing injection risk practices, much less attention has been directed toward reducing sexual risk behaviours in this population (7), although efforts to control further STI outbreaks have increased since a recent outbreak of syphilis occurred in Vancouver (17). It is clear from the present study that risky sexual behaviours are common in this population and that such behaviours have led to a much higher prevalence and incidence of STIs among specific populations of IDUs. In particular, IDUs engaged in unprotected sex with regular partners and IDUs involved in the sex trade may be at particular risk of STIs. Previous studies have shown that a high number of IDUs do not use condoms with their regular partners (2,6). As such, the high rate of STIs among these individuals is not surprising. Nevertheless, previous studies from Vancouver only documented high rates of sexual risk behaviour (2,11). The present study demonstrates infectious disease transmission that is likely occurring in this context, and reinforces the need for targeted interventions in this area. We also found that sex trade involvement was associated with a shorter time to first STI. This finding indicates a high risk of STI transmission, particularly for women, because more women are involved in the sex trade than men (15). The poor health and social conditions facing female IDUs involved in the sex trade in Vancouver has recently received international attention (9,11,18-20). In Vancouver, it has been demonstrated that sex trade workers are commonly offered higher rates if they engage in sex without condoms, a factor which may be relevant to the present study (21). In any event, the present study supports the large and growing literature indicating a need for interventions to reduce the health and social harms experienced by individuals involved in the sex trade (9,11).
The present study has several limitations. Although we have previously demonstrated that the study cohort appears to be highly representative of IDUs in the downtown eastside of Vancouver, the subjects participating in VIDUS do not constitute a random sample (22). In addition, while some studies have suggested that self reports of IDUs are valid (23), STI contraction is likely to be underreported, and it is possible that we have significantly underestimated the rates of incident STIs because this variable was based on self report in our study (24). However, we are not aware of any reason why reporting STIs would be differentially reported across populations engaging in different behaviours, such as having or not having a regular sex partner. Nevertheless, it is likely that the rate of STIs was underestimated in the present study. The specific etiology of the STI was collected but this was also based on self report and would be prone to misclassification. Furthermore, it is important to note that STIs were not systematically measured in the cohort; as such, asymptomatic infections would have been unreported. With regard to the above limitations, we should note that misclassification would only serve to lead to underestimates of the actual rate of STIs in this population. Furthermore, because misclassification is unlikely to have been systematic, our findings would have been biased toward the null; despite this, strong associations persisted.
In the present study, we found that STIs are largely transmitted through regular partnerships and through sex trade involvement. Our findings should raise concern given that both unprotected sex with regular partners and sex trade involvement is common among IDUs. Moreover, carrying an STI increases the likelihood of becoming infected with HIV; as a result, the high prevalence of STIs in this population with an already high HIV prevalence may lead to further increases in HIV transmission. Strategies to encourage condom use among IDUs, particularly those involved in the sex trade, should be further developed.
Acknowledgments
The authors would particularly like to thank the VIDUS participants for their willingness to participate in the study. We also thank Drs Kevin Craib, Richard Harrigan, David Patrick, Martin Schechter, Patty Spittal, Will Small and Steffanie Strathdee for their research assistance, and Bonnie Devlin, John Charette, Caitlin Johnston, Vanessa Volkommer, Steve Kain, Dave Isham and Peter Vann for their administrative assistance. The study was supported by the United States National Institutes of Health (R01 DA011591-04A1) and a Canadian Institutes of Health Research grant (MOP-67262).
References
- 1.Siegal HA, Falck RS, Wang J, Carlson RG. History of sexually transmitted diseases infection, drug-sex behaviors, and the use of condoms among midwestern users of injection drugs and crack cocaine. Sex Transm Dis 1996;23:277-82. [DOI] [PubMed] [Google Scholar]
- 2.Tyndall MW, Patrick D, Spittal P, Li K, O'Shaughnessy MV, Schechter MT. Risky sexual behaviours among injection drugs users with high HIV prevalence: Implications for STD control. Sex Transm Infect 2002;78(Suppl 1):i170-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nelson KE, Vlahov D, Cohn S, et al. Sexually transmitted diseases in a population of intravenous drug users: association with seropositivity to the human immunodeficiency virus (HIV). J Infect Dis 1991;164:457-63. [DOI] [PubMed] [Google Scholar]
- 4.Latka M, Ahern J, Garfein RS, et al; Collaborative Injection Drug User Study Group. Prevalence, incidence, and correlates of chlamydia and gonorrhea among young adult injection drug users. J Subst Abuse 2001;13:73-88. [DOI] [PubMed] [Google Scholar]
- 5.Ross MW, Gold J, Wodak A, Miller ME. Sexually transmissible diseases in injecting drug users. Genitourin Med 1991;67:32-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rhodes T, Donoghoe M, Hunter G, Soteri A, Stimson GV. Sexual behaviour of drug injectors in London: Implications for HIV transmission and HIV prevention. Addiction 1994;89:1085-96. [DOI] [PubMed] [Google Scholar]
- 7.Somlai AM, Kelly JA, McAuliffe TL, Ksobiech K, Hackl KL. Predictors of HIV sexual risk behaviors in a community sample of injection drug-using men and women. AIDS Behav 2003;7:383-93. [DOI] [PubMed] [Google Scholar]
- 8.Tyndall MW, Currie S, Spittal P, et al. Intensive injection cocaine use as the primary risk factor in the Vancouver HIV-1 epidemic. AIDS 2003;17:887-93. [DOI] [PubMed] [Google Scholar]
- 9.Spittal PM, Bruneau J, Craib KJ, et al. Surviving the sex trade: A comparison of HIV risk behaviours among street-involved women in two Canadian cities who inject drugs. AIDS Care 2003;15:187-95. [DOI] [PubMed] [Google Scholar]
- 10.Hudgins R, McCusker J, Stoddard A. Cocaine use and risky injection and sexual behaviors. Drug Alcohol Depend 1995;37:7-14. [DOI] [PubMed] [Google Scholar]
- 11.Spittal PM, Craib KJ, Wood E, et al. Risk factors for elevated HIV incidence rates among female injection drug users in Vancouver. CMAJ 2002;166:894-9. [PMC free article] [PubMed] [Google Scholar]
- 12.Strathdee SA, Patrick DM, Currie SL, et al. Needle exchange is not enough: Lessons from the Vancouver injecting drug use study. AIDS 1997;11:F59-65. [DOI] [PubMed] [Google Scholar]
- 13.Strathdee SA, Patrick DM, Archibald CP, et al. Social determinants predict needle-sharing behaviour among injection drug users in Vancouver, Canada. Addiction 1997;92:1339-47. [PubMed] [Google Scholar]
- 14.Buxton JA. Vancouver Drug Use Epidemiology. Site report for the Canadian Community Epidemiology Network on Drug Use, July 2003. [Google Scholar]
- 15.Craib KJ, Spittal PM, Wood E, et al. Risk factors for elevated HIV incidence among Aboriginal injection drug users in Vancouver. CMAJ 2003;168:19-24. [PMC free article] [PubMed] [Google Scholar]
- 16.Miller CL, Johnston C, Spittal PM, et al. Opportunities for prevention: Hepatitis C prevalence and incidence in a cohort of young injection drug users. Hepatology 2002;36:737-42. [DOI] [PubMed] [Google Scholar]
- 17.Patrick DM, Rekart ML, Jolly A, et al. Heterosexual outbreak of infectious syphilis: Epidemiological and ethnographic analysis and implications for control. Sex Transm Infect 2002;78(Suppl 1):i164-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Culbert L. Pickton to stand trial for murder in deaths of 15 sex-trade workers: Crown prepares seven additional counts based on new evidence. The Vancouver Sun, July 24, 2003. [Google Scholar]
- 19.McIlroy A. Macabre lead in mass killing. The Guardian, February 11, 2002. <www.guardian.co.uk/elsewhere/journalist/story/0,7792,648523,00.html> (Version current at May 17, 2005).
- 20.Lowman J, Fraser L. Violence against Persons who Prostitute: The Experience in British Columbia. Technical Report No TR1996 – 14th edn. Ottawa: Department of Justice Canada, 1996.
- 21.Sex Work Subcommittee. Voices for dignity: A call to end the harms caused by Canada's sex trade laws. Vancouver: PIVOT Legal Society, 2003. [Google Scholar]
- 22.Wood E, Schechter MT, Tyndall MW, Montaner JS, O'Shaughnessy MV, Hogg RS. Antiretroviral medication use among injection drug users: Two potential futures. AIDS 2000;14:1229-35. [DOI] [PubMed] [Google Scholar]
- 23.Darke S. Self-report among injecting drug users: A review. Drug Alcohol Depend 1998;51:253-63. [DOI] [PubMed] [Google Scholar]
- 24.Des Jarlais DC, Paone D, Milliken J, et al. Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: A quasi-randomised trial. Lancet 1999;353:1657-61. [DOI] [PubMed] [Google Scholar]