ABSTRACT
Objective: The infratemporal fossa (ITF) is a continuation of the temporal fossa between the internal surface of the zygoma and the external surface of the temporal bone and greater wing of the sphenoid bone that is sitting deep to the ramus of the mandible. The principal structure to understanding its relationships is the lateral pterygoid muscle. Other important structures are the medial pterygoid muscle, the maxillary artery, the pterygoid venous plexus, the otic ganglion, the chorda tympani nerve and the mandibular nerve. In this study, we describe the microsurgical anatomy of the ITF, as viewed by step-by-step anatomical dissection and also through the perspective of three lateral approaches and one anterior surgical approach. Methods: Eight cadaver specimens were dissected. In one side of all specimens, an anatomical dissection was done in which a wide preauricular incision from the neck on the anterior border of the sternoclidomastoid muscle at the level of the cricoid cartilage to the superior temporal line was made. The flap was displaced anteriorly and the structures of the neck were dissected followed by a zygomatic osteotomy and dissection of the ITF structures. On the other side were the surgical approaches to the ITF. The combined infratemporal and posterior fossa approach was done in two specimens, the subtemporal preauricular infratemporal fossa approach in two, the zygomatic approach in two, and the lateral transantral maxillotomy in two. The anatomical dissections were documented on the three-dimensional (3D) anaglyphic method to produce stereoscopic prints. Results: The lateral pterygoid muscle is one of the principal structures to enable understanding of the relationships into the ITF. The tendon of the temporal muscle inserts in the coronoid process at the ITF. The maxillary artery is the terminal branch of the external carotid artery that originates at the neck of the mandible and runs into the parotid gland. In our dissections the maxillary artery was lateral to the buccal, lingual, and inferior alveolar nerves. We found the second part of the maxillary artery superficial to the lateral pterygoid muscle in all specimens The anterior and posterior branches of the deep temporal artery supply the temporal muscle. In two cases we found a middle deep temporal artery. The different approaches that we used provided different views of the same anatomical landmarks and this provides not only safer surgery but also the best choice to approach the ITF according with the pathology extension. Conclusions: The ITF is a complex region on the skull base that is affected by benign and malignant tumors. The study through different routes is helpful to disclose the relationship among the anatomical structures. Although the authors have shown four approaches, there are a variety of approaches and even a combination of these can be used. This type of anatomical knowledge is essential to choosing the best approach to treat lesions in this area.
Keywords: Infratemporal fossa, surgical anatomy, approaches, paraganglioma, mandibular nerve
The infratemporal fossa (ITF) is a continuation of the temporal fossa between the internal surface of the zygoma and the external surface of the temporal bone and greater wing of the sphenoid bone. It is sitting deep to the ramus of the mandible. The principal structure to enable understanding of these relationships is the lateral pterygoid muscle. Other important structures include the medial pterygoid muscle, the maxillary artery, the pterygoid venous plexus, the otic ganglion, the chorda tympani nerve, and the mandibular nerve.1,2,3,4
The purpose of this article is to show our anatomical dissections regarding the ITF and its variations and analyze different skull base approaches to this complex region.
MATERIAL AND METHODS
The dissections were performed on eight cadaveric heads at the Dianne and M. Gazi Yasargil Educational Center Microsurgical Laboratory. The heads were fixed in Carolina's Perfect Solution® (Carolina Biological Supply Company, Burlington, NC). Arteries and veins were perfused with colored latex to enhance their visibility. On one side of all specimens, an anatomical dissection was done via a wide preauricular incision from the neck on the anterior border of the sternoclidomastoid muscle at the level of the cricoid cartilage to the superior temporal line. The flap was displaced anteriorly. The next steps are summarized as follows. The branches of the facial nerve and the parotid duct were dissected. The parotid fascia and parotid gland were removed preserving the facial nerve. The masseter muscle was cleaned and resected. The temporoparietalis fascia (superficial temporal fascia) and the fat pad were removed along the zygomatic arch. The zygomatic arch was cut and taken out. The superficial temporal artery (STA) and the auriculotemporal nerve were identified over the deep temporal fascia. The coronoid process of the mandible was cut and reflected upward with the temporal muscle tendon, while the insertion of the deep layer of the masseter muscle was resected. The neck of the mandible was cut and another cut was made at the level of the angle. This part of the mandible was resected and the structures of the ITF identified.
On the other side surgical approaches to the ITF were performed. The combined infratemporal and posterior fossa approach was used in two specimens, the subtemporal preauricular ITF approach in another two, the zygomatic approach in two others, and the lateral transantral maxillotomy in the final two. The steps of these approaches are detailed in the results.
The anatomical dissections were documented on the three-dimensional (3D) anaglyphic method to produce stereoscopic prints, in which the same object is photographed from two different positions. The first corresponds to a view of the left eye and the second to the right eye. The images were superimposed with previously defined software coordinates and printed. To see the printed pictures, 3D glasses with colored lenses are required. The technique used by the authors was the same as previously described.5 To document our dissections we used a digital camera (Nikon D70).
RESULTS
Microanatomy
LIMITS
The zygomatic process of the temporal bone divides the temporal from the ITF. There is no anatomical floor located in the ITF. The roof is the greater wing of the sphenoid bone, the medial wall is the lateral pterygoid plate, the lateral wall is the ramus of the mandible, the posterior wall is the articular tubercle of the temporal bone and the spine of the sphenoid bone. This anatomical region has communication through the pterygomaxillary fissure with the pterygopalatine fossa.1 The medial pterygoid fascial layer and the medial pterygoid muscle are the boundaries between the ITF and the parapharyngeal space.6
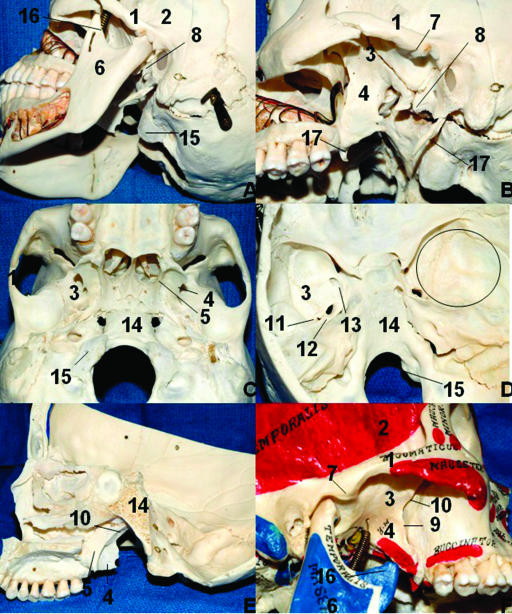
The limits and osseous relationships of the ITF are shown in Fig. 1. The steps of the anatomical dissections are shown in Figs. 2 through 9.
Figure 1.
Limits of the ITF and bone relationships. (A) Oblique lateral view of the ITF. (B) Same view after removal of the mandible. (C) Inferior aspect of the cranium. (D) Interior view of the cranial base. The circle on the right middle fossa represents approximately the correspondence of the ITF in the middle fossa. (E) Lateral view of the ITF after sagittal paramedian section. (F) Note that the depression of the mandible (open mouth) gives more access to the ITF laterally. 1, zygomatic process of the temporal bone; 2, temporal fossa; 3, greater wing of the sphenoid; 4, lateral pterygoid plate; 5, medial pterygoid plate; 6, mandibular ramus; 7, articular tubercle of the temporal bone; 8, spine of the sphenoid bone; 9, pterygomaxillary fissure; 10, pterygopalatine fossa; 11, foramen spinosum; 12, foramen ovale; 13, foramen rotundum; 14, clivus; 15, occipital condyle; 16, coronoid process; 17, styloid process. ITF, infratemporal fossa.
Figure 2.
Lateral view of the superficial dissection of the left face. 1, orbicularis oculi (palpebral part); 2, orbicularis oculi (orbital part); 3, zygomaticus minor and major; 4, buccal fat pad; 5, parotid duct; 6, accessory parotid gland; 7, masseter muscle; 8, parotid fascia over the parotid gland; 9, superficial temporal artery; 10, temporal fascia (deep temporal fascia); 11, temporoparietal fascia (superficial temporal fascia); 12, great auricular nerve; 13, sternocleidomastoid muscle; 14, internal jugular vein; 15, common carotid artery; 16, facial artery; 17, nasalis (more medially) and levator labii superioris alaeque nasi.
Figure 3.
Lateral view of the superficial dissection of the left face. The majority of the parotid tissue was removed to expose the facial nerve branches. A blue field was put under the nerves to enhance them. The distal ramification as well as the parotid plexus are not shown. 1, facial nerve (superior trunk); 2, facial nerve (inferior trunk); 3, cervical branch; 4, mandibular branch; 5, buccal branch; 6, zygomatic branch; 7, temporal branches; 8, superficial temporal artery; 9, superficial temporal vein; 10, auriculotemporal nerve; 11, great auricular nerve; 12, masseter muscle.
Figure 4.
(A) Lateral view of the deep dissection of the left face. The masseter muscle was removed. Note the insertion of the temporal tendon into the coronoid process and anterior aspect of the mandible. 1, mentalis muscle; 2, depressor labii inferioris; 3, depressor anguli oris; 4, fibers of the platisma muscle; 5, orbicularis oris muscle; 6, risorius muscle; 7, zygomatic major muscle; 8, facial artery; 9, angle of the mandible; 10, retromandibular vein; 11, coronoid process; 12, condylar process; 13, coronoid process; 14, zygomatic bone; 15, superficial temporal artery; 16, buccal fat pad; 17, medial pterygoid muscle. (B) The figure shows the stereoscopic view.
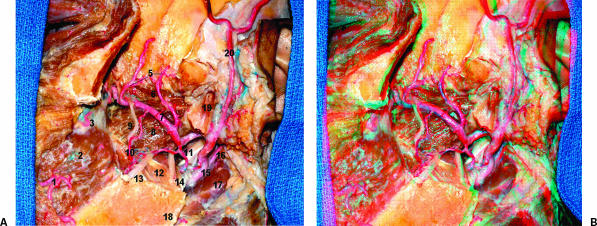
Figure 5.
(A) Lateral view of the ITF. The zygoma and part of the mandible were removed. The condylar process was left to show the insertion of the lateral pterygoid muscle in the pterygoid fovea in the neck of the mandible. 1, facial artery; 2, buccinator muscle; 3, posterior superior alveolar artery; 4, sphenopalatine artery; 5, anterior and posterior deep temporal arteries; 6, lateral pterygoid muscle (upper head); 7, maxillary artery; 8, lateral pterygoid muscle (lower head); 9, buccal nerve; 10, buccal artery; 11, styloid process; 12, medial pterygoid muscle; 13, lingual nerve; 14, inferior alveolar nerve; 15, external carotid artery; 16, posterior auricular artery; 17, digastric muscle (posterior belly); 18, angle of the mandible; 19, condylar process; 20, superficial temporal artery.(B) The figure shows the stereoscopic view. ITF, infratemporal fossa.
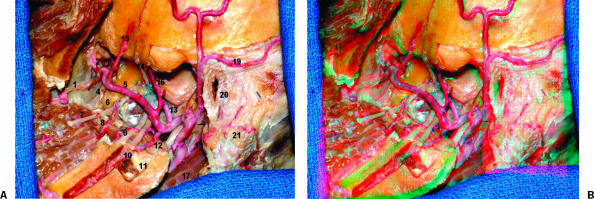
Figure 6.
(A) Lateral view of the ITF. The lateral pterygoid process and the condylar process were removed. 1, posterior superior alveolar artery; 2, infraorbital artery; 3, sphenopalatine artery; 4, descending palatine artery (not injected); 5, maxillary artery; 6, lateral pterygoid plate; 7, buccal nerve; 8, buccal artery; 9, lingual nerve; 10, inferior alveolar nerve; 11, medial pterygoid muscle; 12, inferior alveolar artery; 13, middle meningeal artery; 14, deep temporal nerve; 15, anterior deep temporal artery; 16, posterior deep temporal artery; 17, digastric muscle (posterior belly); 18, posterior auricular artery; 19, posterior auricular artery; 20, external acoustic meatus; 21, mastoid. (B) The figure shows the stereoscopic view. ITF, infratemporal fossa.
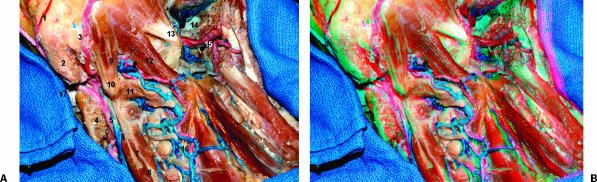
Figure 7.
Posterior oblique view of the neck and part of the left ITF. 1, posterior auricular artery; 2, mastoid; 3, occipital artery; 4, middle pterygoid muscle; 5, external carotid artery; 6, internal jugular vein; 7, accessory nerve; 8, levator scapula muscle; 9, superior oblique muscle; 10, transverse process of atlas; 11, inferior oblique; 12, rectus capitis posterior major muscle; 13, rectus capitis posterior minor; 14, right jugular bulb; 15, right vertebral artery; 16, deep cervical vein and artery. (B) The figure shows the stereoscopic view. ITF, infratemporal fossa.
Figure 8.
Lateral view of the ITF and neck, emphasizing the branches of the external carotid artery. 1, superior thyroid artery; 2, inferior pharyngeal constrictor muscle; 3, thyroid cartilage; 4, submandibular gland; 5, lingual artery; 6, hypoglossal nerve; 7, facial artery; 8, ascending palatine artery; 9, stylohyoid muscle; 10, styloglossus muscle; 11, ascending pharyngeal artery; 12, internal jugular vein sectioned; 13, vertebral artery; 14, suboccipital triangle with venous plexus and muscular branches from the vertebral artery; 15, styloid process and posterior auricular artery; 16, maxillary artery; 17, infraorbital nerve; 18, buccinator muscle. ITF, infratemporal fossa.
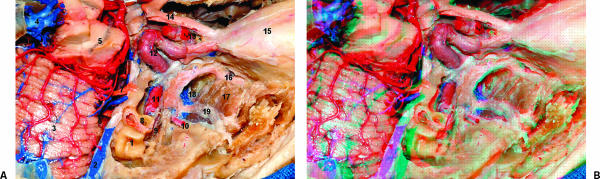
Figure 9.
(A) Lateral superior view of the ITF. Part of the middle fossa floor was removed to expose the ITF. The gasserion ganglion was resected to expose the intrapetrous portion of the ICA. The floor of the anterior fossa was resected also. 1, semicircular canals; 2, superior petrosal sinus; 3, superior surface of the cerebellum; 4, great cerebral vein (Galen); 5, substantia nigra; 6, cranial nerves VII and VIII; 7, cranial nerve V; 8, cochlea; 9, geniculate ganglion; 10, middle meningeal artery; 11, ICA (intrapetrous portion); 12, ICA (intracavernous portions); 13, ICA (subclinoidal portion); 14, cranial nerve II; 15, orbit; 16, maxillary nerve; 17, lateral pterygoid muscle (upper head); 18, part of the pterygoid plexus; 19, V3. (B) The figure shows the stereoscopic view. ITF, infratemporal fossa; ICA, internal carotid artery.
MUSCULAR RELATIONSHIPS
To understand the surgical approaches to the ITF, it is necessary to have knowledge not only of the pterygoid muscles but also of the masseter and temporalis muscles. The tendon of the temporalis muscle is sitting in this space.
The masseter muscle is covered by the masseteric fascia7 and is formed by three muscular layers (superficial, middle, and deep). The superficial layer has tendineous septum between muscular fibers and is a continuation of an aponeurosis that arises from the zygomatic bone at the maxillary process and the anterior part of the inferior border of the zygomatic arch. This layer then inserts into the lateral surface of the mandibular ramus and angle. The middle layer arises from the medial portion of the anterior part of the zygomatic arch and from the inferior border of the posterior part and then inserts into the central part of the mandibular ramus. The deep layer originates from the zygomatic arch more deeply, and inserts into the coronoid process and upper part of the mandibular ramus. The masseter muscle is supplied by the masseteric branch that has its origin in the second part of the maxillary artery which is deep to the muscle, and by two other arteries that run superficial to the muscle: the facial and transverse facial arteries. The masseter is innervated by the masseteric branch of the mandibular nerve.
The temporal muscle is a fan-shaped muscle that lies in the temporal fossa. This muscle has a main portion, along with the anteromedial, anterolateral, and middle lateral bundles. It also arises in the temporal fossa and its fibers insert as two separate tendinous heads (superficial and deep) that run deep to the zygomatic arch and insert in the coronoid process and the anterior border of the ramus of the mandible. Although it is difficult to individualize the tendons separately at its insertion, the superficial part is more related to the lateral surface of the coronoid process. One important consideration that has implications for the surgical approaches is the anatomical study of the fascia related to the temporal muscle. We identified the temporoparietal fascia (superficial temporal fascia) that blends superiorly in the galea aponeurotica and the temporal fascia (deep temporal fascia). Between this was fat tissue and loose areolar tissue (temporparietal fat pad). There was fat tissue always between the deep temporal fascia and the temporal muscle fibers and fat tissue superficial to the superficial temporal fascia, although with a variable amount in the different specimens. In our dissections the temporal branch of the facial nerve was found inside the temporoparietal fat pad but superficially, meaning that it was related to the internal surface of the superficial temporal fascia. The fascial nerve fibers were also identified on the superficial temporal fascia, inside the fat tissue. The deep temporal fascia split into superficial and deep laminae that attached to the lateral and medial surfaces of the zygomatic bone. These aspects are detailed in a previous article.8
The lateral pterygoid muscle has an upper head that originates in the roof of the ITF and in the infratemporal crest (inferior portion of the greater wing of the temporal bone) and a lower head that originates in the lateral surface of the lateral pterygoid plate (Fig. 5). The insertion is the same for both parts; in the pterygoid fovea that is a convex space in the neck of the mandible. The vascular supply is from the pterygoid branches of the maxillary artery and the ascending palatine branch of the facial artery. The innervation is from the anterior trunk of the mandibular nerve (Fig. 6).
The medial pterygoid muscle lies in the medial aspect of the ramus of the mandible (Fig. 6). It has a deep large head and a minor superficial head. The origin of the deep head is the medial surface of the lateral pterygoid plate and the pyramidal process of the palatine bone. The superficial head is from the maxillary tuberosity and the pyramidal process of the palatine bone. The two heads embrace the lower head of the lateral pterygoid and unite to insert on the medial surface of the ramus of the mandible near its angle. The arterial supply is from the pterygoid ramus of the maxillary artery and the innervation by the medial pterygoid branch of the mandibular nerve.
ARTERIAL RELATIONSHIPS
The maxillary artery is the terminal branch of the external carotid artery that originates at the neck of the mandible and runs in its beginning into the parotid gland (Fig. 8). It is divided into three parts, mandibular (or retromandibular), pterygoid, and pterygopalatine. The division of the maxillary artery is in relation to the lateral pterygoid muscle. The first part is before, the second at the level of, and the third after this muscle (Fig. 5). In our dissections the maxillary artery was lateral to the buccal, lingual, and the inferior alveolar nerves (Fig. 6).
The branches of the first part characteristically pass through foramina or canals. It passes between the neck of the mandible and the sphenomandibular ligament, running adjacent to the auriculotemporal nerve. This is the deep auricular artery that pierces the wall of the external acoustic meatus. The anterior tympanic artery runs parallel to the chorda tympani nerve and enters into the petrotympanic fissure. The middle meningeal artery (MMA) is the first branch of the maxillary artery which runs superficial to the lateral pterygoid muscle. The MMA can originate as a common trunk with the inferior alveolar artery, but we did not observe this pattern. The MMA ascends to pass through the foramen spinosum. The accessory meningeal artery can have its origin in the MMA and ascends adjacent to the tensor and levator veli palatine to reach the foramen ovale. The mandibular artery enters into the mandibular foramen in the medial surface of the mandible to supply the mandible and inferior teeth.
We found the second part of the maxillary artery superficial to the pterygoid muscle in all the specimens. The anterior and posterior branches of the deep temporal artery supply the temporal muscle. In two cases we found a middle deep temporal artery. The masseteric artery runs into the mandibular notch to reach the masseter muscle. The pterygoid arteries are variable in number and supply the pterygoid muscles. The buccal artery runs parallel to the buccal branch of the nerve and supplies the skin over the buccinator (Fig. 5).
VENOUS RELATIONSHIPS
The pterygoid venous plexus has a superficial portion between the temporal muscle and the lateral pterygoid muscle and a deep portion between the pterygoid muscles. We observed a more developed deep part, principally in the medial surface of the lateral pterygoid muscle, around the superior head (Fig. 9).
The pterygoid venous plexus receives venous drainage from the orbit and adjacent areas of the ITF and communicates with the cavernous sinus by the sphenoidal emissary foramen, the foramen ovale, and the foramen lacerum and with the facial vein through the deep facial vein. The maxillary vein runs parallel to the first part of the maxillary artery and joins inside the parotid gland with the superficial temporal vein to form the retromandibular vein.
NEURAL RELATIONSHIPS
The ITF is the locus of the otic ganglion, chorda tympani nerve, and major divisions of the mandibular branch of the trigeminal nerve. The mandibular nerve is a mixed nerve that emerges from the skull base through the foramen ovale and runs between the tensor veli palatine muscle and the lateral pterygoid muscle. It then divides into two trunks, anterior and a larger posterior. Before this division into two principal trunks, the mandibular nerve gives origin to a meningeal branch that re-enters the skull base passing the foramen spinosum to innervate the middle fossa dura and a nerve to the medial pterygoid muscle.1
The anterior trunk gives rise the buccal nerve, a sensory branch of the buccal mucous membrane, which innervates the skin over the anterior part of the buccinator muscle. The other three branches are motor. The nerve to the masseter innervates the masseter muscle and the temporomandibular joint and crosses between the tendon of the temporal muscle and the lateral pterygoid muscle. The deep temporal nerves are two or three branches that innervate the temporal muscle, the anterior branch that arises from the buccal nerve. The nerve to the lateral pterygoid also can also have its origin in the buccal nerve.
The posterior trunk carries principally sensory fibers. The first branch is the auriculotemporal nerve that travels between the lateral pterygoid muscle and the tensor veli palatine muscle and between the sphenomandibular ligament and the neck of the mandible. It has two roots that encircle the MMA and join each other later to ascend. It communicates with the facial nerve and the otic ganglion and innervates the tragus, the auricle, and the posterior part of the temple. The lingual nerve is joined by the chorda tympani branch of the facial nerve and runs downwards closer to the medial surface of the mandibular ramus, passing medial to the mylohyoid muscle to innervate the anterior two thirds of the tongue and the floor of the mouth. The inferior alveolar descends to enter the mandibular canal with the inferior alveolar artery and related veins.
The otic ganglion is separated from the pharyngotympanic tube by the tensor veli palatine muscle and is in front of the MMA. The lesser petrosal nerve passes through the foramen ovale. The chorda tympani nerve enters the ITF passing by the petrotympanic fissure, crosses posterolateral to the tensor veli palatine, and joins to the lingual nerve.
LIGAMENTS RELATIONSHIPS
There are three ligaments that must be recognized. The stylomandibular ligament joins the styloid process to the angle of the mandible and is a thickened part of the parotid sheath. The sphenomandibular ligament is a strong ligament that suspends the mandible and descends from near the spine of the sphenoid bone to the lingula of the mandible. The pterygospinous ligament descends from the spine of the sphenoid bone to the posterior border of the lateral pterygoid plate. Sometimes it is replaced by muscle fibers and sometimes it is ossified, creating a true foramen through which branches of the mandibular nerve travel.
Approaches
The authors have chosen three lateral approaches that use different incisions in relation to the ear or different displacements of the temporal muscle, and one anterior approach, to exemplify the anatomical exposition that can be reached by different anatomical corridors. In the combined infratemporal and posterior fossa approach (Fig. 10),9 which is a variation of the Fisch approach,10,11,12 the incision is retroauricular. The subtemporal-preauricular ITF approach (Fig. 11)14 incision is preauricular and the temporal muscle is displaced down. In the zygomatic approach (Fig. 12),14 the incision is preauricular and the muscle is displaced up. The lateral transantral maxillotomy (Fig. 13)15 is a more conservative anterior approach to the ITF and pterygopalatine fossa. In all approaches the patient is in the supine position.
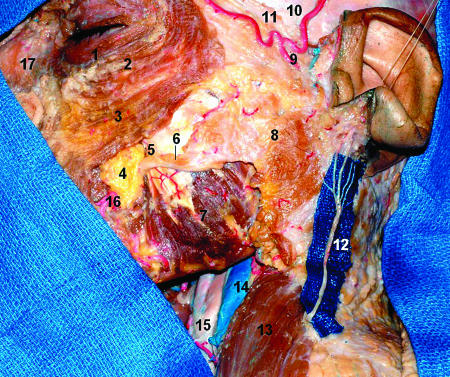
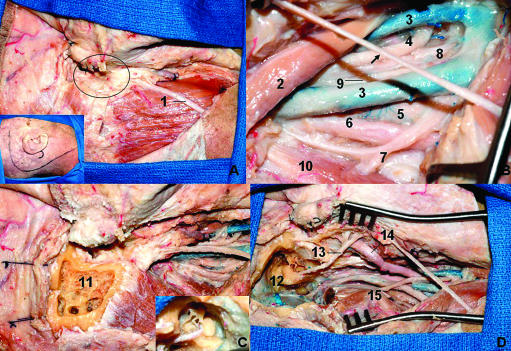
Figure 10.
Combined infratemporal and posterior fossa approach. (A) After the incision (inset) the flap is reflected anteriorly and the external meatus is sectioned and closed in a blind sac as described by Ugo Fisch (oval). (B) The neurovascular structures are exposed in the neck to proximal control. The arrow indicates the greater auricular nerve. (C) The petrosectomy is performed. The inset shows the facial nerve, the ossicles, and semicircular canals. (D) Final anatomical view of the neurovascular structures in the neck and the presigmoid and temporal fossa dura after petrosectomy. The semicircular canals are preserved and the facial nerve is transposed anteriorly. 1, great auricular nerve; 2, digastric muscle (posterior belly); 3, duplicated internal jugular vein; 4, glossopharyngeal nerve; 5, internal carotid artery; 6, sympathetic trunk; 7, accessory nerve; 8, hypoglossal nerve; 9, vagus nerve; 10, inferior oblique nerve; 11, mastoid drilled; 12, facial nerve; 13, semicircular canals; 14, superficial temporal artery; 15, transverse process of C1.
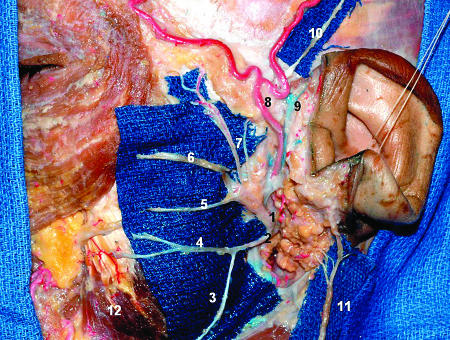
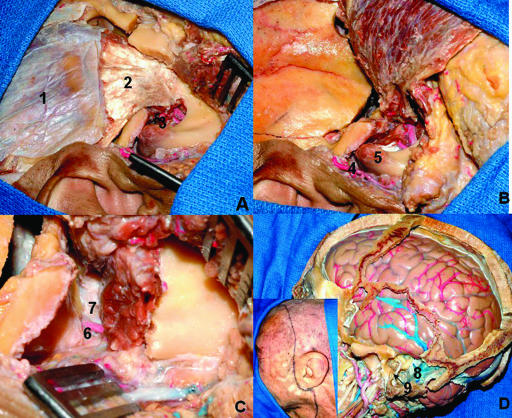
Figure 11.
Subtemporal preauricular ITF approach. (A) The preauricular incision on the right side was performed, the flap is displaced anteriorly, and the zygomatic process was removed. (B) The temporal muscle is displaced all the way down. (C) Exposition of the middle meningeal artery and V3 in the ITF. (D) Relationship among ITF, mastoid, and temporal lobe; the inset shows the incision. 1, temporal superficial fascia; 2, tendon of the temporal muscle; 3, mandibular incisura and maxillary artery; 4, superficial temporal artery; 5, mandibular condyle; 6, middle meningeal artery entering in the foramen spinosum; 7, V3; 8, sigmoid sinus exposed after mastoidectomy; 9, mastoid portion of the facial nerve.
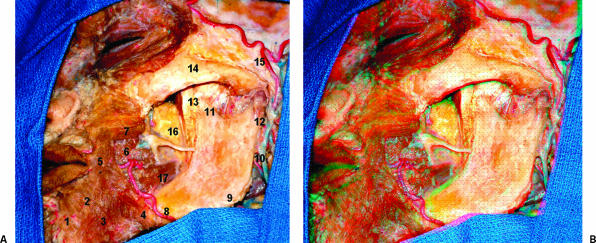
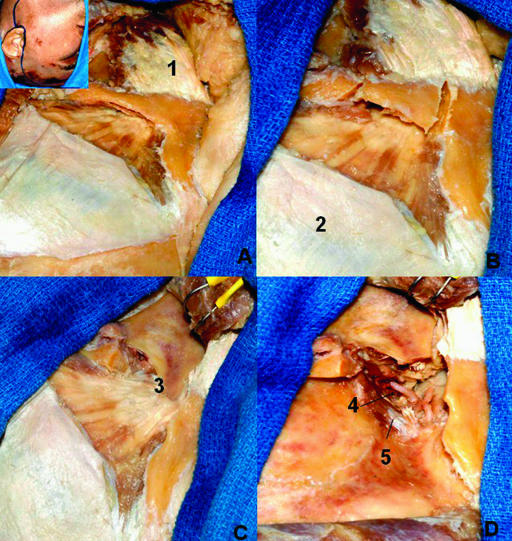
Figure 12.
Zygomatic approach. Part of the deep temporal fascia was removed to show the muscular fibers. (A) Preauricular incision and anterior displacement of the flap. (B) Section of the zygomatic arch. (C) The masseter and the zygomatic arch are displaced inferiorly. (D) The coronoid process is sectioned and displaced upward with the temporal muscle. 1, masseter muscle; 2, deep temporal fascia; 3, coronoid process; 4, maxillary artery; 5, lateral pterygoid muscle (upper head).
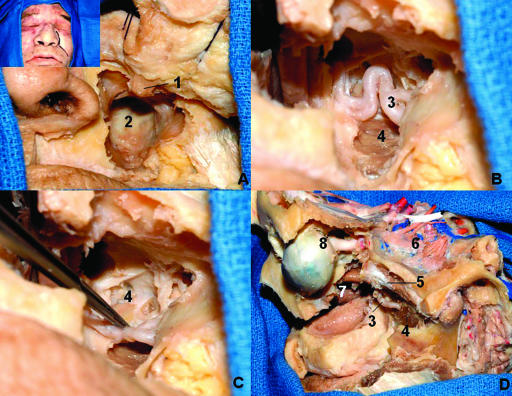
Figure 13.
Lateral transantral maxillotomy. (A) The anterior and lateral walls of the maxilla are resected. (B) After removal of the sinus mucosa, the posterior wall is drilled out, exposing the ITF. (C) The maxillary is displaced to show the lateral pterygoid plate. (D) This dissection exposes the ITF via an anterior and lateral view. The maxilla was totally removed. 1, infraorbital nerve; 2, posterior wall of the maxilla; 3, maxillary artery; 4, lateral pterygoid plate; 5, lateral pterygoid muscle (upper head); 6, lateral pterygoid muscle (lower head); 7, nasal cavity; 8, eyeball and optic nerve. ITF, inferior temporal fossa.
The dissection of each of the approaches is briefly described below.
COMBINED INFRATEMPORAL AND POSTERIOR FOSSA APPROACH
The head is fixed in the Mayfield headrest and turned away from the side to be approached. A C-shaped incision is made from behind the ear to the neck. The external ear is transected, everted, and closed as a blind sac according to Fisch's description.10,11,12,16 The sternoclidomastoid is detached from the mastoid. The following structures are identified and dissected: common carotid artery; internal carotid artery (ICA); external carotid artery; internal jugular vein; cranial nerves IX, X, XI, and XII; ascending pharyngeal; and posterior auricular and occipital arteries, which can be ligated during the surgery. The mastoid is drilled to skeletonize the mastoid portion of the facial nerve with its subsequent anterior transposition. A posterior fossa craniotomy and exposition of the sigmoid sinus is the next step. Dissect and remove the posterior belly of the digastric muscle, the stylohyoid muscle, and the styloid process. During the surgery the sigmoid sinus is ligated between the mastoid emissary vein proximally (there is an anterior and posterior, but the posterior is bigger) and the sigmoid sinus distally to the tumoral extension. The skin of the external ear canal and the tympanic membrane are removed. The intrapetrous segment of the ICA is exposed by drilling the carotid canal. The Eustachian tube is identified and during the surgery will be obliterated with wax and fascia.
The surgeon must identify the lower cranial nerves leaving the jugular foramen by opening the dura of the posterior fossa and finding the fifth and twelfth nerves and the structures of the cerebellopontine angle, as well as the posterior inferior cerebellar artery (PICA) and the superior cerebellar artery.
SUBTEMPORAL PREAURICULAR INFRATEMPORAL FOSSA APPROACH
Begin with extension of the neck and turn the head 45 degrees to the contralateral side. The beginning of the incision is made on the frontal skin, descending in front of the external auditory canal and with anterior extension in the neck. The skin flap is reflected anteriorly. The facial nerve is identified and dissected between the stylomastoid foramen and the parotid gland. This last structure is separated from the masseteric fascia to facilitate the anterior displacement of the mandible without traction of the facial nerve. The temporal muscle is displaced all the way down and the zygomatic arc is resected. Cut the attachment of the stylomandibular and sphenomandibular ligaments to displace anteroinferiorly the mandibular condyle. To gain more space, sometimes the condyle of the mandible must be resected. The next step is identification and dissection of the neurovascular structures in the neck. The digastric muscle is divided and the styloid process resected. A pterional craniotomy is performed with the posteroinferior limit just above the glenoid fossa. The next step is the peeling of the middle fossa with identification of the arcuate eminence, MMA, greater and lesser superficial petrosal nerves, V3, V2, and V1 entering into the superior orbital fissure. The part of the greater wing of the sphenoid bone in the floor of the middle fossa is drilled around the foramen rotundum and foramen ovale to expose, respectively, the V2 entering into the pterygopalatine fossa and the V3 entering into the ITF. The Eustachian tube and the tensor tympani muscle are resected. The intrapetrous portion of the ICA is identified. The cervical ICA is displaced forward. An anterior petrosectomy (by drilling the Kawase triangle) can be done to expose the clivus.
ZYGOMATIC APPROACH
The head is turned to the side contralateral to the lesion. A preauricular incision similar to the subtemporal preauricular ITF approach is performed. Following the original description, an intrafacial dissection is performed to preserve the facial nerve. The STA is identified and must be preserved. The ICA is dissected in the neck. The facial nerve is identified entering into the parotid gland. The superficial temporal fascia is incised over the zygomatic arch, which is sectioned through anterior and posterior cuts, both in an oblique trajectory for reattachment of the arch, being displaced downward. The insertion of the temporal tendon in the coronoid process into the ITF is sectioned at its base and is displaced upward with the temporal muscle until before it reaches the insertion of the muscle in the temporal squama. A temporal craniotomy is performed, but depending on the tumor extension a large single orbitocranial flap can also be made. The dura is open if there is intradural or cavernous sinus (CS) tumor. The same middle fossa peeling described in the subtemporal preauricular ITF approach section can be done.
LATERAL TRANSANTRAL MAXILLOTOMY
The head is extended 15 degrees and rotated 20 degrees contralateral from the side approached. An incision is performed that extends from inferiorly to the site of the lacrimal canaliculi through the nasolabial fold to the level of the upper lip. The anterior and lateral walls of the maxilla are exposed by retraction of the skin and are resected en bloc with the anterior limit superior to the infraorbital foramen to allow the infraorbital nerve to be displaced laterally to gain more lateral access to the ITF. The next step is to remove the mucosa of the sinus and drill the lateral and posterior walls of the maxillary sinus, which permits the dissection and identification of the ITF structures. In the beginning the temporal muscle fibers, the maxillary artery, and the maxillary nerve (V2) and its superior alveolar branch are identified. So both heads of the lateral pterygoid muscle are transected medially and the muscle displaced laterally. The lateral pterygoid plate is drilled permitting visualization of the medial part of the ITF and the pterygopalatine fossa. The pterygoid venous plexus is dissected and the V3 and foramen rotundum and MMA and foramen spinosum are identified. The branches of V3 are identified. The muscles of the palate are exposed when the medial pterygoid plate is drilled. The levator veli palatine muscle courses parallel and inferior to the Eustachian tube and is medial to the tensor veli palatine muscle. The bone around V3 is drilled and this nerve is displaced laterally to allow a view of the Eustachian tube. Drilling superior to it exposes the intrapetrous portion of the ICA. The sella turcica and the clivus can be reached with this approach.
DISCUSSION
There is some discord among authors regarding the exact limits of the ITF.1,2,7,17 Some authors3,17 include, in addition to the temporal and pterygoid muscles, branches of the V3, the pterygoid venous plexus, and the maxillary artery; also the lower cranial nerves, sympathetic plexus, ICA, and internal jugular vein (IJV). Our limits in this study do not include the jugular fossa and the ICA. In a more inclusive concept, the ITF can be subdivided by the interpterygoid fascia superiorly and the medial pterygoid muscle inferiorly in the pterygomandibular and maxillopharyngeal regions. The styloid diaphragm divides this second region into the prestyloid and retrostyloid region, which contain the ICA, IJV, and the proximal part of cranial nerves IX to XII. The styloid diaphragm is formed by the posterior belly of the digastric muscle, stylohyoid, styloglossus, and stylopharyngeal muscles, stylohyoid and stylomandibular ligaments, stylopharyngeal fascia, and the fascia between the sternoclidomastoid to the digastric muscle.3
The ITF approaches are categorized as anterior (transfacial, transmaxillary, transoral, and transpalatal), lateral (transzygomatic and lateral infratemporal), or inferior (transmandibular and transcervical).18
The pioneers of the ITF were Conley and Barbosa. Before the 1960s the ITF was considered surgically inaccessible.4 Barbosa indicated the ITF approach for advanced tumors into the maxillary sinus. The deep 3D microanatomical knowledge and a multidisciplinary team, as well as advances in neurointensive care, made it possible to perform surgery with an acceptable rate of morbidity on tumors situated in this region.
In 1969, Terez et al19 used a craniofacial approach for tumors invading the pterygoid fossa but residual tumor could not be avoided.
In 1976, House and Hitselberger20 described a transcochlear approach for tumors that originated medially to the internal auditory canal or from the clivus. This approach is a forward extension of the translabyrintine approach where the cochlea is removed and the facial nerve posteriorly rerouted.
In 1977, Fisch and coworkers reported the posterolateral ITF approach. Fisch was revolutionary because his innovation permitted the treatment of lesions involving the temporal bone and skull base.10,11,12 The ITF approach of Fisch was divided into types A, B, C, and D.
In 1981, Friedman and associates21 described a stylomandibular dissection for tumors in the ITF but vascular complications occurred in 25% of the patients.
In 1987, Al-Mefty and colleagues9 described a combined infratemporal and posterior fossa approach that was a modification of the infratemporal approach popularized by Fisch, which permitted tumors with large intracranial extensions to be resected in one procedure and not in another separate procedure as had been advocated by Fisch.10,11,12 The anterior transposition of the facial nerve was emphasized as being crucial to adequate tumor exposure and preservation of the facial nerve. The detailed closure was essential to avoid cerebrospinal fluid leak and also included, in addition to the repair of the dura mater and tight skin closure, obliteration of the cavity and the Eustachian tube and closure of the external ear canal.
Sekhar et al13 described the subtemporal-preauricular ITF approach that was used in 22 patients. This approach provides an extensive exposure but the authors emphasized some limitations, such as when the facial recess and hypotympanic areas are invaded by tumor, with loss of conductive hearing. In these cases a Fisch type A approach is necessary. For extensive clival lesions a combination with an anterior approach (transbasal or transethmoidal) can be necessary. This approach has good exposition, especially if the tumor extends into the ITF and the orbit, maxillary and ethmoidal sinus, and retro and parapharyngeal space. Special attention must be given to the reconstruction, principally if the paranasal sinus and nasopharynx were opened.
Hakuba et al22 used the orbitozygomatic infratemporal approach in 4 vascular lesions and 10 tumors into the CS. The authors noted that this approach provides exposure of the ITF that is accessed obliquely upward through the lateral wall of the CS.
Al-Mefty and Anand14 described the zygomatic approach, a preauricular approach that displaced the muscle upward by cutting the coronoid process of the mandible and maintaining the attachment in the temporal squama, providing an excellent exposure of the ITF and keeping intact the adequate vascularity of the muscle due to the preservation of the middle temporal artery, a branch from the STA, and the deep temporal arteries. The temporal muscle is supplied also by the occipital, supraorbital, and supratrochlear arteries. In addition, there are intradiploic anastomoses between the MMA and the deep temporal arteries, and in this fact resides the importance of leaving the muscle attached to the temporal bone. In our dissection it was possible to keep the deep temporal arteries intact when the displacement upward of the temporal muscle was slight, permitting a low temporal craniotomy. However, if a larger craniotomy with more displacement of the muscle were necessary, the deep temporal arteries could not be left intact.
In general, the ITF approaches that use a preauricular incision are not adequate to expose the mastoid portion of the facial nerve and the jugular bulb. When the lesion involves the temporal bone and invades the ITF, the postauricular incision is indicated. Until proven otherwise, tumors located anterior to the vertical portion of the carotid artery can be resected through a preauricular incision.23
Pieper and Al-Mefty24 used the middle fossa/zygomatic approach to resect intracranial meningiomas extending into the ITF, showing that this approach can reach the intra- and extracranial parts of a tumor, as well as the cavernous sinus, paranasal sinus, and nasopharynx.
Guinto and colleagues6 described the zygomatic-transmandibular approach in the treatment of 10 patients with giant tumors localized in the ITF and parapharyngeal space and studied 10 cadaveric specimens. In 3 cases in which both the prestyloid and retrostyloid were invaded, the styloid process was removed. The authors note that the masticator space is a physiological concept that is different from the anatomic concept of the ITF and also that the profuse bleeding around V3 when the middle fossa is drilled is due to the large number of veins of the pterygoid plexus around the superior head of the lateral pterygoid muscle. In this approach the posterior half of the ascending ramus of the mandible is only rotated, preserving the joint capsule and providing adequate exposure with minimal morbidity.
Although complete exposition of the ITF can be achieved principally with Fisch B and C approaches, the subtemporal-preauricular,13 zygomatic approach,14 or these approaches combined with the anterior subfrontal approach, Le Fort I, and transmaxillary approaches can also be performed. Sabit et al15 proposed a microsurgical model to approach the ITF via a lateral transantral maxillotomy that would be a less invasive anterior route to the region. A nasolabial incision and an en bloc osteotomy of the anterolateral wall of the maxilla, plus removal the posterior wall of the maxilla, exposed the ITF from the sphenomandibular ligament laterally to the sphenopalatine fossa medially. The risk of facial deformity and lesion of the frontalis branch of the facial nerve and infraorbital nerve that can occur in the facial translocation approach, as well as violation of the nasal and oral cavities that can occur in the extended maxillotomy/subtotal maxillectomy, can be avoided. The complications related to the lateral approaches to the ITF also would be avoided. However, this approach would be limited to tumors restricted to the anteromedial part of the ITF, and could result in vascular complications from the pterygoid venous plexus and the maxillary artery. The transantral maxillotomy performed by the authors can also be done with a sublabial incision for small lesions, avoiding facial scars.25 In our dissections we preferred the first approach because of the more rigid characteristics of the soft tissue preserved with formalin. In general, transfacial approaches are indicated for sinunasal or nasopharynx tumors invading the ITF.
Mansour and colleagues26 studied the variables of tumoral extensions that necessitated modifications in the ITF preauricular approach according to the individual characteristics of the tumor in 44 malignant tumors and 21 benign tumors. In the malignant group, the numbers were statistically significant to necessitate additional osteotomies (supraorbital and Le Fort I) for tumors with medial and intracranial extensions; subtemporal craniectomy for tumors with superior extension; craniotomy for tumors with medial, superior, or intracranial extension; parotidectomy and mandibulectomy for tumors with lateral extension; and maxillectomy for tumors with medial and superior extension. In the benign group, only zygomatic osteotomy was necessary in the majority of cases and additional procedures were less necessary. In this study the authors advocate the versatility of the preauricular ITF approach.
Massive tumors of the ITF can also be reached by a combined Fisch type D approach with a transmaxillary approach, avoiding the risks of loss of hearing and facial paralysis.27
The lateral transmandibular approach reaches the ITF, but is limited to access the skull base.28
Kassam and coworkers29 proposed the fully endoscopic expanded endonasal approach for selected cases of tumors into the ITF, but the lesion must be medial and inferior to the principal neurovascular structures. They maintain that tumor size, vascularity, fibrosity, or calcification do not represent contraindications.
One important topic is management of the mandibular condyle. The anterior displacement of the mandible without resection can be necessary to gain a sufficiently large field to resect benign tumors limited to the more superior part of the ITF. On the other hand, malignancies in a great number of cases necessitate the resection of the mandibular condyle, which can cause lateral deviation of the mandible and pain in the contralateral side, but this is a more acceptable morbidity than severe trismus that can develop after resection of the masticator muscles.3 Some authors prefer the mandibular condylectomy because the same lateral sway on full opening of the jaw is better than the pain and temporomandibular joint (TMJ) dysfunction that results if only incision of the TMJ and inferior retraction of the condyle are performed.16 To avoid the lesion of the maxillary artery deep to the mandibular condyle, subperiosteal dissection must be performed.16
CONCLUSION
The ITF is a complex region in the skull base that is affected by benign and malignant tumors. The study of different routes and the reproduction of the images in an anaglyphic 3D stereoscopic printing are helpful to disclose the relationships among the anatomical structures. Although the authors have shown four approaches, there are a variety of approaches and even combinations of them that can be used. This type of anatomical knowledge is essential to choosing the best approach to treat lesions in this area, not only for skull base surgeons but also for the vascular surgeons who perform carotid endarterectomies with high bifurcation.
REFERENCES
- Gray H. Anatomy of the Human Body. New York: Bartley.com; 2000.
- Vrionis F D, Cano W G, Heilman C B. Microsurgical anatomy of the infratemporal fossa as viewed laterally and superiorly. Neurosurgery. 1996;39:777–786. doi: 10.1097/00006123-199610000-00027. [DOI] [PubMed] [Google Scholar]
- Bejjani G K, Sullivan B, Salas-Lopez E, et al. Surgical anatomy of the infratemporal fossa: the styloid diaphragm revisited. Neurosurgery. 1998;43:842–852. doi: 10.1097/00006123-199810000-00072. [DOI] [PubMed] [Google Scholar]
- Schramm V L., Jr In: Sekhar LN, Schramm VL, editor. Tumors of the Cranial Base: Diagnosis and Treatment. Mount Kisco, NY: Futura Publishing Co; 1987. Infratemporal fossa surgery. pp. 421–437.
- Ribas G C, Bento R F, Rodrigues A J. Anaglyphic three-dimensional stereoscopic printing: revival of an old method for anatomical and surgical teaching and reporting. J Neurosurg. 2001;95:1057–1066. doi: 10.3171/jns.2001.95.6.1057. [DOI] [PubMed] [Google Scholar]
- Guinto G, Abello J, Molina A, et al. Zygomatic-transmandibular approach for giant tumors of the infratemporal fossa and parapharyngeal space. Neurosurgery. 1999;45:1385–1398. doi: 10.1097/00006123-199912000-00025. [DOI] [PubMed] [Google Scholar]
- Gardner E. Anatomia Humana. São Paulo, Brazil: Guanabara; 1993.
- Krayenbuhl N, Isolan G R, Hafez A, Yasargil M G. The relationship of the fronto-temporal branches of the facial nerve to the fascias of the temporal region: a literature review applied to practical anatomical dissection. Neurosurg Rev. 2007;30:8–15. doi: 10.1007/s10143-006-0053-5. [DOI] [PubMed] [Google Scholar]
- Al-Mefty O, Fox J L, Rifai A, Smith R R. A combined infratemporal and posterior fossa approach for the removal of giant glomus tumors and chondrosarcomas. Surg Neurol. 1987;28:423–431. doi: 10.1016/0090-3019(87)90224-2. [DOI] [PubMed] [Google Scholar]
- Fisch U, Pilsbury H C. Infratemporal fossa approach to lesions in the temporal bone and base of skull. Arch Otolaryngol. 1979;105:99–107. doi: 10.1001/archotol.1979.00790140045008. [DOI] [PubMed] [Google Scholar]
- Fisch U, Fagan P, Valvanavis A. The infratemporal fossa approach for the lateral skull base. Otolaryngol Clin North Am. 1984;17:513–552. [PubMed] [Google Scholar]
- Fisch U. The infratemporal fossa approach for nasopharyngeal tumors. Laryngoscope. 1983;93:36–44. doi: 10.1288/00005537-198301000-00007. [DOI] [PubMed] [Google Scholar]
- Sekhar L N, Schramm V L, Jones N F. Subtemporal-preauricular infratemporal fossa approach to large lateral and posterior cranial base neoplasms. J Neurosurg. 1987;67:488–499. doi: 10.3171/jns.1987.67.4.0488. [DOI] [PubMed] [Google Scholar]
- Al-Mefty O, Anand V K. Zygomatic approach to skull-base lesions. J Neurosurg. 1990;73:668–673. doi: 10.3171/jns.1990.73.5.0668. [DOI] [PubMed] [Google Scholar]
- Sabit I, Schaefer S D, Coldwell W T. Modified infratemporal fossa approach via lateral transantral maxillotomy: a microsurgical model. Surg Neurol. 2002;58:21–31. doi: 10.1016/s0090-3019(02)00764-4. [DOI] [PubMed] [Google Scholar]
- Donald P J. In: Donald PJ, editor. Surgery of the Skull Base. Philadelphia: Lippincott-Raven Publishers; 1998. Infratemporal fossa: middle cranial fossa approach. pp. 309–339.
- Tedeschi H, Rhoton A L., Jr Lateral approaches to the petroclival region. Surg Neurol. 1994;41:180–216. doi: 10.1016/0090-3019(94)90123-6. [DOI] [PubMed] [Google Scholar]
- Tiwari R, Quak J, Egeler S, et al. Tumors of the infratemporal fossa. Skull Base Surg. 2000;10:1–9. doi: 10.1055/s-2000-6789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terez J J, Alksne F J, Lawrence W. Craniofacial resection for tumors invading the pterygoid fossa. Am J Surg. 1969;118:732–740. doi: 10.1016/0002-9610(69)90220-7. [DOI] [PubMed] [Google Scholar]
- House W F, Hitselberger W E. The transcochlear approach to the skull base. Arch Otolaryngol. 1976;102:334–342. doi: 10.1001/archotol.1976.00780110046004. [DOI] [PubMed] [Google Scholar]
- Friedman W H, Katsantonis G P, Cooper M H, Lee J M, Strelzow V V. Stylohamular dissection: a new method for en bloc reaction of malignancies of the infratemporal fossa. Laryngoscope. 1981;91:1869–1879. doi: 10.1288/00005537-198111000-00012. [DOI] [PubMed] [Google Scholar]
- Hakuba A, Tanaka K, Suzuki T, Nishimura S. A combined orbitozygomatic infratemporal epidural and subdural approach for lesions involving the entire cavernous sinus. J Neurosurg. 1989;71:699–704. doi: 10.3171/jns.1989.71.5.0699. [DOI] [PubMed] [Google Scholar]
- Anand V. Infratemporal approaches for skull base lesions. Oper Tech Neurosurg. 1999;2:87–104. [Google Scholar]
- Pieper D R, Al-Mefty O. Management of intracranial meningiomas secondarily involving the infratemporal fossa: radiographic characteristics pattern of tumor invasion, and surgical implications. Neurosurgery. 1999;45:231–237. doi: 10.1097/00006123-199908000-00005. [DOI] [PubMed] [Google Scholar]
- Kantas I, Tzindros G, Papadopoulou A, Marangos N. Midfacial degloving: the best alternative for treatment of trans-sphenoidal meningocele of the pterygopalatine fossa. Skull Base. 2006;16:117–122. doi: 10.1055/s-2006-934110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansour O I, Carrau R L, Snyderman C H, Kassam A. Preauricular infratemporal fossa surgical approach: modifications of the technique and surgical indications. Skull Base. 2004;14:143–151. doi: 10.1055/s-2004-832256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahinian H K, Suh R H, Jarrahy R. Combined infratemporal fossa and transfacial approach to excising massive tumors. Ear Nose Throat J. 1999;78:350–356. [PubMed] [Google Scholar]
- Carrillo J F, Rivas Leon B, Celis M A, Ponce-de-Leon S, Ochoa-Carrillo F J. Anterolateral and lateral skull-base approaches for treatment of neoplastic diseases. Am J Otolaryngol. 2004;25:58–67. doi: 10.1016/s0196-0709(03)00094-2. [DOI] [PubMed] [Google Scholar]
- Prades J M, Timoshenko A, Merzougui N, Martin C. A cadaveric study of a combined trans-mandibular and trans-zygomatic approach to the infratemporal fossa. Surg Radiol Anat. 2003;25:180–187. doi: 10.1007/s00276-003-0126-x. [DOI] [PubMed] [Google Scholar]