Abstract
Objective
To assess the contribution of work-organisational and personal factors to the prevalence of work-related musculoskeletal disorders (WMSDs) among garment workers in Los Angeles.
Methods
This is a cross-sectional study of self-reported musculoskeletal symptoms among 520 sewing machine operators from 13 garment industry sewing shops. Detailed information on work-organisational factors, personal factors, and musculoskeletal symptoms were obtained in face-to-face interviews. The outcome of interest, upper body WMSD, was defined as a worker experiencing moderate or severe musculoskeletal pain. Unconditional logistic regression models were adopted to assess the association between both work-organisational factors and personal factors and the prevalence of musculoskeletal pain.
Results
The prevalence of moderate or severe musculoskeletal pain in the neck/shoulder region was 24% and for distal upper extremity it was 16%. Elevated prevalence of upper body pain was associated with age less than 30 years, female gender, Hispanic ethnicity, being single, having a diagnosis of a MSD or a systemic illness, working more than 10 years as a sewing machine operator, using a single sewing machine, work in large shops, higher work–rest ratios, high physical exertion, high physical isometric loads, high job demand, and low job satisfaction.
Conclusion
Work-organisational and personal factors were associated with increased prevalence of moderate or severe upper body musculoskeletal pain among garment workers. Owners of sewing companies may be able to reduce or prevent WMSDs among employees by adopting rotations between different types of workstations thus increasing task variety; by either shortening work periods or increasing rest periods to reduce the work–rest ratio; and by improving the work-organisation to control psychosocial stressors. The findings may guide prevention efforts in the garment sector and have important public health implications for this workforce of largely immigrant labourers.
Keywords: work organisation, musculoskeletal disorder, ergonomic, psychosocial, sewing machine
Employment in the garment industry rose worldwide in the late 1990s to approximately 11 million workers in 1998.1 In the United States, over 300 000 garment workers were employed in 2005 to sew apparel.2
California is home to the largest garment production centre in the United States, with the majority of the garment shops located in the Los Angeles basin. Altogether these shops employ over 144 000 sewing machine operators, the majority of whom are minimum wage, unrepresented, immigrant women.3
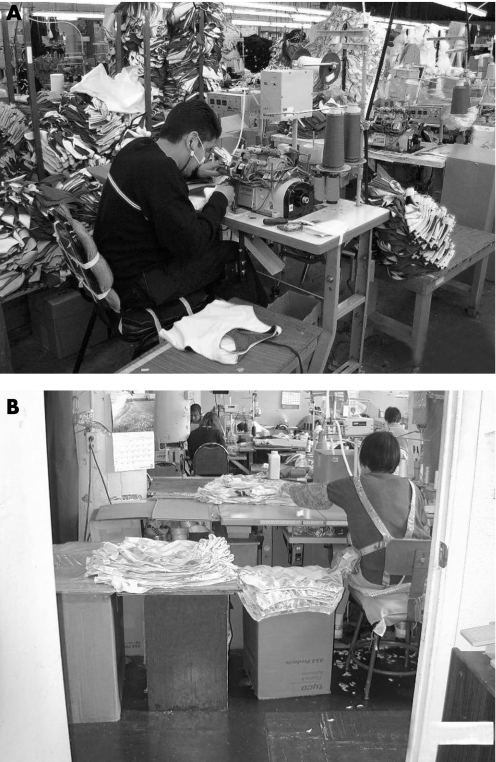
A typical sewing workstation consists of a sewing table with a built-in electric sewing machine, a non-adjustable household chair, and cardboard boxes/cart to hold incoming fabrics and sewn products. Production sewing is a highly repetitive, high-precision task that requires the worker to lean forward to see the point of operation, while simultaneously using the hands to control fabric feed to the needle, and continuously operate foot and knee pedals (fig 1).4,5,6 In the United States, sewing machine operators are in the top 20 occupations (out of 821) with the highest rate of lost time due to over-use injuries.7 In spite of this high injury rate, few studies have focused on this occupation.
Figure 1 Typical sewing machine workstations; (A) operator leaning forward in a cramped space, (B) operator using non-adjustable household chair and cardboard boxes to support incoming fabric.
Generally, sewing machine operators have little control over their workload, work pace and work schedule. Employment is unstable and often involves a tight delivery schedule so that the work pace is fast, time for rest breaks is limited and working hours may be long. Thus, in this population, work-organisation might be an important contributor to musculoskeletal disorders.8,9 Work-organisation may contribute to work-related musculoskeletal disorders (WMSDs) via the nature of the work activities, the extent, duration and frequency of workloads, and psychosocial factors.10,11,12 In this study, we assessed the contribution of work-organisational factors to the prevalence of self-reported moderate or severe neck–shoulder and distal upper extremity pain among sewing machine operators.
Methods
Study design and subjects
This paper evaluates the baseline data collected from a prospective ergonomics intervention study.13 The study population consisted of sewing machine operators in Los Angeles, California. Subjects were recruited based on the following eligibility criteria: they performed sewing machine operations for more than 20 h per week including work on single/double needle straight-stitch, overlock and cover-stitch machines, were not in a probationary period (the probationary period ranged from 1 to 6 months), did not have an active worker's compensation claim, had worked for at least 3 months, and were not planning to quit their jobs within 6 months. These criteria were not mutually exclusive, and were employed to ensure that subjects were selected from a stable garment worker population.
Between October 2003 and March 2005, 13 out of 29 garment shops contacted agreed to participate in the study. Thus, these 13 shops represent a convenience sample from the garment industry in Los Angeles. The types of garments sewn in these 13 shops included men's and women's clothes such as shirts, T-shirts, jackets, gowns, lingerie, blouses, skirts, pants and jeans. Within these shops, we had contact with 555 subjects, and 520 (93.7%) were eligible and agreed to participate in this study [14 (2.5%) subjects refused to participate, and 21 (3.8%) subjects did not meet the eligibility criteria]. The number of participants from each shop varied between 11 and 148. In accordance with National Institutes of Health (NIH) policy, approval for all study procedures was obtained from the Offices for the Protection of Research Subjects at the University of California, Los Angeles (UCLA). All participants provided written informed consent.
Data collection
All information was collected in face-to-face interviews conducted in the language of the employee (including Spanish, Cantonese and Mandarin Chinese, and English). The standardised interview elicited information on: (1) musculoskeletal pain symptoms; (2) personal factors; and (3) work-organisational factors, including physical and psychosocial stressors.
Musculoskeletal pain symptoms
Musculoskeletal symptoms experienced in the past 4 weeks were assessed by asking each subject to self-report pain frequency (1 or 2 days in the last month, 1 day per week, several days per week, or every day) and pain intensity (0- to 5-point scale with verbal anchors of ‘a little painful' for 1 and ‘very painful' for 5) for three body regions: neck/shoulders, arms/elbows, and hands/wrists.14 We used self-reports of pain as a surrogate for musculoskeletal disorders, and we defined a case as a worker who reported moderate or severe musculoskeletal pain. That is, upper body musculoskeletal pain experienced during the past 4 weeks at least 1 day per week, with pain intensity of 3 or more on a scale of 0 to 5. We combined the outcomes for the regions arms/elbows and hands/wrists into distal upper extremities because pain reports for these regions were strongly correlated. Thus, WMSDs are presented for two upper body regions: neck/shoulders and distal upper extremities.
Personal factors
Information was collected on gender, age, ethnicity, education, health-related factors [i.e., body mass index (BMI), non-work physical activity, smoking behaviour, and medical history of systemic illnesses and musculoskeletal disorders (MSDs)], and family-related factors (i.e. marital status, living with children, and whether workers supported other family members outside their own household). The number of years the workers had lived in the United States, and their ability to speak English, and years of employment in the garment industry were also recorded.
Work-organisational factors
Work-organisational factors included task, pay, shop, time, physical exertion and psychosocial measures. The measures included variety of machines operated (number of different sewing machines operated in the past 4 weeks), variety of tasks performed (number of different types of sewing tasks performed in the past 4 weeks), pay method (piece rate vs. hourly rate), shop size (small shop vs. large shop), work–time management factors and perceived physical job demands including physical exertion and physical isometric loads. Generally, the large shops had established work organisational structures including non-flexible work schedules, in contrast to small shops that had more flexible work schedules but employment was more tenuous than in large shops. The owners of all the nine small shops were members of the Chinese Garment Contractor Association.
The chronological diary of work periods and rest periods self-reported by each subject recorded information such as time of starting and stopping work, time until they took a rest break or returned to work after a break. This data allowed computing several work–time management related factors including hours and days worked per week, maximum continuous work period (defined as the time from start of work to a break, or the work duration between two breaks), total rest period in a day, number of rests in a day, and work–rest ratio (total work minutes divided by the total recovery minutes in a day; the recovery minutes included rest and lunch period). Both perceived physical exertion and physical isometric workload were constituted by five items from the full recommended version (49 items) of the Karasek Job Content Questionnaire (JCQ).15 The three items for physical exertion represent physical efforts including heavy physical effort, lifting heavy loads and rapid physical activity (Cronbach's alpha = 0.47), and the two items for physical isometric load include awkward body and arm positions (Cronbach's alpha = 0.81).
Five psychosocial stressors were constituted from 28 items of the JCQ. The six items for skill discretion reflect aspects of learning new tasks, amount of repetitive work, required creative skills, and task variety (Cronbach's alpha = 0.43), and the three items for decision authority reflect influence over planning of work tasks and ability to make decisions at work (Cronbach's alpha = 0.18). Both skill discretion and decision authority together constituted job control (Cronbach's alpha = 0.48). The five items for job demands encompass fast work, hard work, excessive work, insufficient time to complete work, and conflicting demands (Cronbach's alpha = 0.15). The three items for job insecurity include work stability, job security, and the possibility of future lay-off (Cronbach's alpha = 0.40). The five items for supervisor support reflect the supervisor's control over a worker's job and the positive nature of interactions with the supervisor (Cronbach's alpha = 0.64), and the six items for co-worker support reflect the positive nature of interactions with co-workers (Cronbach's alpha = 0.52). Both supervisor and co-worker support together constitute social support (Cronbach's alpha = 0.65).
For some scales we calculated much lower Cronbach's alpha values for our population than reported in other studies,15 indicating low internal consistency among items used to generate the scale. Removing items that received small weights for job control, job demand, social support and physical exertion did not improve internal consistency considerably except for job demands [Cronbach's alpha after exclusions were 0.60 vs. 0.48 (job control), 0.54 vs. 0.15 (job demands), 0.66 vs. 0.40 (job insecurity), 0.66 vs. 0.65 (social support)]. More importantly, however, deleting or adjusting items would jeopardise comparability with other published studies that employed these scales as recommended by Karsek.16 Thus, we decided to retain the original formulas for creating these scales. In addition, we defined job strain based on the factors ‘job demand' and ‘job control' according to Karasek's demand–control model.17
Data analysis
Some researchers have suggested that the relation between work organisational factors and musculoskeletal pains is not linear.18,19,20 Therefore, we categorised most continuous variables into quartiles of the observed distribution to examine linear and non-linear associations. Four continuous variables were categorised differently: ‘number of rests' was split into three categories (one, two, and more than two breaks); ‘work–rest ratio' was split into three categories: 0–9.2, 9.2–11.6, and 11.6+ [Note: the California law requires a total 20 min rest period and 30 min lunch break when working 6 or more hours per day; thus, the ratio of 9.2 and 11.6 are the legally required work–rest ratios for 8-h and 10-h shifts and were used to represent appropriate (according to the law) versus non-appropriate work schedules in our population]. Some variables were better categorised as tertiles: ‘job insecurity' (0–24, 25–74 and 75+ percentile), ‘physical isometric loads' (0–49, 50–74 and 75+ percentile), and ‘job satisfaction' (‘not satisfied', ‘satisfied' and ‘very satisfied').
We estimated the associations [odds ratios (OR) and 95% confidence intervals] between risk and exposure factors and the prevalence of moderate or severe musculoskeletal pain in crude and adjusted unconditional logistic regression models. We mutually adjusted our odds ratios (OR) for all 12 presumed risk factors including age, gender, ethnicity, BMI, medical history of MSD, smoking behaviour, shop size, years of employment in the garment industry, number of sewing machines operated, number of rest breaks, job strain and social support.3,10,21 Furthermore, we assessed whether each variable is likely to be an independent risk factor for the outcome of interest and also unlikely to be an intermediate in the causal pathway. Finally, we considered the potential for collinearity among risk factors.
Results
All 520 participants were immigrant workers; the majority were female (64.4%), Hispanic or Asian (67.1% and 28.3% respectively), with a mean age of 38 years (range, 18–65). More than half (54.0%) were overweight or obese with a BMI above 24.9 kg/m2, but few had ever smoked (10.4%) or were currently smoking (4.8%), or reported a physician-diagnosed systemic illness (14.8%) or musculoskeletal disorder (10.0%). Almost half (45.2%) did not complete high school, 21.0% had lived in the United States for fewer than 5 years, and a majority (91.2%) spoke little or no English (Table 1).
Table 1. Demographic characteristics for all subjects working as sewing machine operators in Los Angeles, California (n = 520).
| Variable | Category | Number | %* |
|---|---|---|---|
| Gender | Female | 335 | 64.4 |
| Male | 185 | 35.6 | |
| Age group | Mean (SD) | 37.7 | (9.9) |
| <30 | 121 | 23.3 | |
| 30–39 | 176 | 33.8 | |
| 40–49 | 153 | 29.4 | |
| ⩾50 | 70 | 13.5 | |
| Ethnicity | Asian/Pacific Islander | 147 | 28.3 |
| Hispanic | 349 | 67.1 | |
| Caucasian | 24 | 4.6 | |
| Educational level | Primary | 235 | 45.2 |
| High school | 261 | 50.2 | |
| University or more | 23 | 4.4 | |
| Marital status | Living alone | 110 | 21.2 |
| Cohabitating but not married | 110 | 21.2 | |
| Married but separated | 75 | 14.4 | |
| Married and living with spouse | 166 | 31.9 | |
| Living with children | No children | 120 | 23.1 |
| Equal or less than 5 years of age | 157 | 30.2 | |
| More than 5 years of age | 243 | 46.7 | |
| Supporting other family members | No | 235 | 45.2 |
| outside of their own household | Yes | 285 | 54.8 |
| Body mass index (BMI) | Mean (SD) | 26.2 | (4.8) |
| Underweight (<18.5 kg/m2) | 6 | 1.2 | |
| Normal (18.6–24.9 kg/m2) | 195 | 37.5 | |
| Overweight (25–29.9 kg/m2) | 203 | 39.0 | |
| Obese (>29.9 kg/m2) | 83 | 16.0 | |
| Non-work-related physical activity | None | 194 | 37.3 |
| Less than once per week | 34 | 6.5 | |
| Once or twice per week | 171 | 32.9 | |
| Three or more times per week | 121 | 23.3 | |
| Smoking behaviour | Non-smoker | 441 | 84.8 |
| Past smoker | 54 | 10.4 | |
| Current smoker | 25 | 4.8 | |
| Medical history of systemic illness† | None | 443 | 85.2 |
| Any | 77 | 14.8 | |
| Medical history of musculoskeletal disorders | None | 468 | 90.0 |
| Any | 52 | 10.0 | |
| Years lived in the United States | Mean (SD) | 12.0 | (7.2) |
| <5 years | 109 | 21.0 | |
| 5–10 years | 103 | 19.8 | |
| 10–20 years | 148 | 28.5 | |
| >20 years | 160 | 30.8 | |
| English-speaking ability | None at all | 117 | 22.5 |
| Only a few words | 357 | 68.7 | |
| Enough to get by or very well | 46 | 8.8 | |
| Years of employment in garment industry | Mean (SD) | 11.1 | (7.3) |
| <7 | 154 | 29.6 | |
| 7–10 | 106 | 20.4 | |
| 11–15 | 152 | 29.2 | |
| >15 | 108 | 20.8 |
* Some percentages do not total 100 because of rounding; † the list of systemic illnesses or diseases included: diabetes (excluding diabetes solely related to pregnancy), rheumatoid arthritis, lupus erythematodes, degenerative arthritis (osteoarthritis), low thyroid or overactive thyroid, chronic renal failure, and gout.
Upper body pain during more than 1 day per week in the past month was reported by 58% of study participants. The prevalence of moderate or severe pain in the neck/shoulder region (referred from here on as ‘pain') was 24% and for distal upper extremity it was 16%. The overall prevalence of upper body WMSDs was 32% (165) (Table 2).
Table 2. Intensity and frequency of upper body musculoskeletal pain for the 30 days prior to the interview (n = 520).
| Pain | Symptoms by anatomical site | ||
|---|---|---|---|
| Neck/shoulders | Arms/elbows | Hands/wrists | |
| n (%*) | n (%*) | n (%*) | |
| Frequency | |||
| No pain | 218 (41.9) | 434 (83.5) | 374 (71.9) |
| One or 2 days/month | 58 (11.2) | 14 (2.7) | 25 (4.8) |
| One day/week | 73 (14.0) | 26 (5.0) | 34 (6.5) |
| Several days/week | 108 (20.8) | 28 (5.4) | 53 (10.2) |
| Every day | 63 (12.1) | 18 (3.5) | 34 (6.5) |
| Intensity (0–5 scale) | |||
| Mean score (SD) | 1.4 (1.4) | 0.4 (1.1) | 0.7 (1.3) |
| 0 | 218 (41.9) | 434 (83.5) | 374 (71.9) |
| 1–2 | 156 (30.0) | 46 (8.8) | 73 (14.0) |
| 3–5 | 146 (28.1) | 40 (7.7) | 73 (14.0) |
| Prevalence by anatomical regions | ||
|---|---|---|
| Prevalence of moderate or severe pain† | Neck/shoulders | Distal upper extremities‡ |
| n (%) | n (%) | |
| 125 (24.0) | 82 (15.8) | |
*Some percentages do not total 100 because of rounding or some missing value; † defined as subjects experiencing pain at least 1 day per week, with pain intensity of 3 or more out of a maximum score of 5; ‡ subjects who experience musculoskeletal pain in any part of the arms/elbows, and hands/wrists.
The odds ratios for personal factors estimated in multivariate fully adjusted models are shown in Table 3. Male compared to female garment workers reported experiencing less pain in both upper body regions (approximately half). Less pain (again approximately half) in the neck and should region alone, was reported by Asian compared to Hispanic workers, workers married and living with a spouse compared to singles and also non-smokers, while age showed a somewhat u-shaped relation with neck/shoulder pains. The prevalence of neck/shoulder or a distal upper extremity pain was also higher among sewing machine operators who reported an ever physician diagnosis of a musculoskeletal disorder or systemic illness. We observed an increase (and positively increasing trend ptrend = 0.02) with years of employment in the garment industry for the prevalence of hand/wrist but not for neck/shoulder pain, mostly attributable to employees who had worked in the garment industry for 10 years or more.
Table 3. Generated odds ratio estimates (95% CIs) for selected personal factors on neck/shoulder and distal upper extremity pain.
| Variable | Category | Neck/shoulder pain | Distal upper extremity pain | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Number | Crude | Adjusted* | Number | Crude | Adjusted* | ||||
| No pain | With pain | OR (95% CI) | OR (95% CI) | No | Yes | OR (95% CI) | OR (95% CI) | ||
| Gender | Female | 250 | 85 | 1.00 | 1.00 | 272 | 63 | 1.00 | 1.00 |
| Male | 145 | 40 | 0.81 (0.53 to 1.24) | 0.50 (0.28 to 0.90) | 166 | 19 | 0.49 (0.29 to 0.85) | 0.55 (0.28 to 1.09) | |
| Age group | <30 | 84 | 37 | 1.00 | 1.00 | 105 | 16 | 1.00 | 1.00 |
| 30–39 | 140 | 36 | 0.58 (0.34 to 0.99) | 0.50 (0.27 to 0.94) | 154 | 22 | 0.94 (0.47 to 1.87) | 1.03 (0.46 to 2.28) | |
| 40–49 | 119 | 34 | 0.65 (0.38 to 1.12) | 0.61 (0.3 to 1.27) | 123 | 30 | 1.60 (0.83 to 3.1) | 1.64 (0.69 to 3.92) | |
| >49 | 52 | 18 | 0.79 (0.41 to 1.52) | 0.79 (0.31 to 2.06) | 56 | 14 | 1.64 (0.75 to 3.6) | 1.61 (0.53 to 4.93) | |
| ptrend† | 0.38 | 0.55 | 0.07 | 0.24 | |||||
| Ethnicity | Asian/Pacific Islander | 123 | 24 | 1.00 | 1.00 | 129 | 18 | 1.00 | 1.00 |
| Hispanic | 253 | 96 | 1.94 (1.18 to 3.19) | 2.00 (0.94 to 4.25) | 289 | 60 | 1.49 (0.84 to 2.62) | 1.47 (0.63 to 3.46) | |
| Caucasian | 19 | 5 | 1.35 (0.46 to 3.96) | 1.37 (0.43 to 4.34) | 20 | 4 | 1.43 (0.44 to 4.67) | 1.51 (0.43 to 5.31) | |
| Educational level | Primary | 179 | 56 | 1.00 | 1.00 | 197 | 38 | 1.00 | 1.00 |
| High school | 196 | 65 | 1.06 (0.70 to 1.60) | 1.12 (0.69 to 1.81) | 222 | 39 | 0.91 (0.56 to 1.48) | 0.94 (0.54 to 1.64) | |
| University or above | 19 | 4 | 0.67 (0.22 to 2.06) | 0.54 (0.15 to 1.93) | 18 | 5 | 1.44 (0.5 to 4.11) | 1.35 (0.40 to 4.52) | |
| Marital status | Living alone | 78 | 32 | 1.00 | 1.00 | 92 | 18 | 1.00 | 1.00 |
| Cohabitating but not married | 77 | 33 | 1.04 (0.59 to 1.86) | 0.99 (0.52 to 1.91) | 93 | 17 | 0.93 (0.45 to 1.92) | 0.93 (0.42 to 2.06) | |
| Married but separated | 56 | 19 | 0.83 (0.43 to 1.61) | 0.68 (0.32 to 1.44) | 58 | 17 | 1.50 (0.71 to 3.14) | 1.26 (0.55 to 2.89) | |
| Married and live with spouse | 141 | 25 | 0.43 (0.24 to 0.78) | 0.51 (0.24 to 1.08) | 143 | 23 | 0.82 (0.42 to 1.61) | 1.16 (0.50 to 2.69) | |
| Living with children | No children | 89 | 31 | 1.00 | 1.00 | 104 | 16 | 1.00 | 1.00 |
| ⩽5 years | 115 | 42 | 1.05 (0.61 to 1.80) | 1.01 (0.55 to 1.87) | 134 | 23 | 1.12 (0.56 to 2.22) | 1.07 (0.49 to 2.32) | |
| >5 years old | 191 | 52 | 0.78 (0.47 to 1.30) | 0.79 (0.44 to 1.42) | 200 | 43 | 1.40 (0.75 to 2.60) | 1.32 (0.66 to 2.64) | |
| Supporting families outside of household | No | 199 | 36 | 1.00 | 1.00 | 186 | 49 | 1.00 | 1.00 |
| Yes | 239 | 46 | 1.38 (0.92 to 2.08) | 1.34 (0.82 to 2.20) | 209 | 76 | 1.06 (0.66 to 1.71) | 1.26 (0.71 to 2.21) | |
| BMI | Underweight (<18.5 kg/m2) | 6 | 0 | – | – | 6 | 0 | – | – |
| Healthy (18.6–24.9 kg/m2) | 150 | 53 | 1.00 | 1.00 | 167 | 38 | 1.00 | 1.00 | |
| Overweight (25–29.9 kg/m2) | 150 | 45 | 1.18 (0.75 to 1.86) | 0.94 (0.56 to 1.57) | 165 | 28 | 1.37 (0.81 to 2.34) | 1.15 (0.64 to 2.07) | |
| Obese (>29.9 kg/m2) | 67 | 16 | 0.80 (0.42 to 1.51) | 0.60 (0.30 to 1.21) | 72 | 11 | 0.91 (0.43 to 1.93) | 0.71 (0.31 to 1.61) | |
| Physical activity | None | 149 | 45 | 1.00 | 1.00 | 159 | 35 | 1.00 | 1.00 |
| <once per week | 27 | 7 | 0.86 (0.35 to 2.10) | 0.74 (0.27 to 2.05) | 31 | 3 | 0.44 (0.13 to 1.52) | 0.37 (0.08 to 1.71) | |
| Once or twice per week | 126 | 45 | 1.18 (0.73 to 1.90) | 1.07 (0.61 to 1.89) | 151 | 20 | 0.60 (0.33 to 1.09) | 0.72 (0.37 to 1.41) | |
| ⩾times per week | 93 | 28 | 1.00 (0.58 to 1.71) | 0.87 (0.48 to 1.58) | 97 | 24 | 1.12 (0.63 to 2.00) | 0.93 (0.49 to 1.76) | |
| ptrend† | 0.78 | 0.82 | 0.88 | 0.73 | |||||
| Smoking behaviour | None | 339 | 102 | 1.00 | 1.00 | 368 | 73 | 1.00 | 1.00 |
| Past smoker | 40 | 14 | 1.16 (0.61 to 2.22) | 1.77 (0.81 to 3.89) | 47 | 7 | 0.75 (0.33 to 1.73) | 1.17 (0.45 to 3.04) | |
| Current smoker | 16 | 9 | 1.87 (0.80 to 4.36) | 2.20 (0.82 to 5.89) | 23 | 2 | 0.44 (0.10 to 1.90) | 0.57 (0.12 to 2.69) | |
| Physician diagnosed MSDs | No | 352 | 91 | 1.00 | 1.00 | 387 | 56 | 1.00 | 1.00 |
| Yes | 43 | 34 | 2.60 (1.44 to 4.70) | 3.08 (1.59 to 5.95) | 51 | 26 | 2.17 (1.12 to 4.21) | 2.37 (1.13 to 5.00) | |
| Physician diagnosed systemic illness‡ | No | 365 | 103 | 1.00 | 1.00 | 400 | 68 | 1.00 | 1.00 |
| Yes | 30 | 22 | 3.06 (1.85 to 5.07) | 3.45 (1.88 to 6.30) | 38 | 14 | 3.52 (2.03 to 6.10) | 3.43 (1.81 to 6.51) | |
| Years of employment in garment industry | Quartile 1 (<7) | 101 | 16 | 1.00 | 1.00 | 138 | 16 | 1.00 | 1.00 |
| Quartile 2 (7–10) | 262 | 95 | 1.00 (0.55 to 1.80) | 0.93 (0.48 to 1.82) | 94 | 12 | 1.10 (0.50 to 2.43) | 1.32 (0.56 to 3.13) | |
| Quartile 3 (11–15) | 31 | 13 | 1.13 (0.67 to 1.92) | 1.12 (0.60 to 2.07) | 121 | 31 | 2.21 (1.15 to 4.24) | 2.69 (1.26 to 5.73) | |
| Quartile 4 (>15) | 31 | 13 | 1.19 (0.67 to 2.11) | 1.21 (0.58 to 2.53) | 85 | 23 | 2.33 (1.17 to 4.67) | 2.22 (0.93 to 5.33) | |
| ptrend† | 0.49 | 0.55 | 0.004 | 0.02 | |||||
* Adjusted models included: age, gender, ethnicity, BMI, medical history of MSD, smoking behaviour, shop size, years of employment in garment industry, number of sewing machines operated, number of rest breaks, job strain, and social support; † p value for trend across categories (Pearson's chi-squared test) ;‡ the list of systemic illnesses or diseases included: diabetes (excluding pregnancy-related diabetes), rheumatoid arthritis, lupus erythematodes, degenerative arthritis (osteoarthritis), Hyper- or hypo-thyroidism, chronic renal failure, and gout.
No clear patterns emerged for education, living with children, BMI and physical activity, and we observed no associations with pain reports for having to support members of the family outside the household.
We also found some work-organisational factors to be associated with differences in reported prevalence of neck/shoulder and distal upper extremity pain (Table 4). Operating three or more machines was associated with a reduced prevalence of both upper body pain (88% reduction for neck/shoulder disorders and 58% reduction for distal upper extremity disorders) but our estimates for distal upper extremity disorders were rather imprecise. Subjects working in large garment shops were more than twice more likely to report upper body pain than those from small shops. Interestingly, payment method (piece vs. hourly) affected symptom reporting in opposite directions for employees from small and large shops. Stratification on shop size showed that subjects in large shops paid via piece rate were less likely to report upper body disorders, while the opposite was observed in small shops, where piece rate payment seemed to contribute to pain reports although our estimates were imprecise due to small sample sizes.
Table 4. Generated odds ratio estimates (95% CIs) for work-organisational factors on neck/shoulder and distal upper extremity pains.
| Variable | Category | Neck/shoulder pain | Distal upper extremity pain | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Number | Univariate | Multivariate * | Number | Univariate | Multivariate * | ||||
| No pain | With pain | OR (95% CI) | OR (95% CI) | No | Yes | OR (95% CI) | OR (95% CI) | ||
| Number of machines operated in the past month | 1 | 323 | 108 | 1.00 | 1.00 | 359 | 72 | 1.00 | 1.00 |
| 2 | 37 | 14 | 1.13 (0.59 to 2.17) | 1.11 (0.53 to 2.31) | 44 | 7 | 0.79 (0.34 to 1.83) | 0.87 (0.35 to 2.14) | |
| 3 and more | 35 | 3 | 0.26 (0.08 to 0.85) | 0.11 (0.01 to 0.89) | 35 | 3 | 0.43 (0.13 to 1.43) | 0.37 (0.08 to 1.73) | |
| ptrend† | 0.06 | 0.07 | 0.15 | 0.22 | |||||
| Shop size | Small shops | 135 | 27 | 1.00 | 1.00 | 144 | 18 | 1.00 | 1.00 |
| Large shops | 260 | 98 | 1.88 (1.17 to 3.03) | 2.42 (1.13 to 5.17) | 294 | 64 | 1.74 (1 to 3.05) | 2.60 (1.1 to 6.17) | |
| Pay method | Small shops | ||||||||
| Hourly rate | 59 | 7 | 1.00 | 1.00 | 62 | 4 | 1.00 | 1.00 | |
| Piece rate | 76 | 20 | 2.22(0.88 to 5.60) | 2.35 (0.66 to 8.30) | 82 | 14 | 2.65 (0.83 to 8.43) | 1.75 (0.45 to 6.73) | |
| Large shops | |||||||||
| Hourly rate | 71 | 36 | 1.00 | 1.00 | 81 | 26 | 1.00 | 1.00 | |
| Piece rate | 189 | 62 | 0.65 (0.40 to 1.06) | 0.54 (0.29 to 1.00) | 213 | 38 | 0.56 (0.32 to 0.97) | 0.63 (0.31 to 1.27) | |
| Work–rest ratio | <9.2 | 160 | 40 | 1.00 | 1.00 | 174 | 26 | 1.00 | 1.00 |
| 9.2–11.6 | 116 | 52 | 1.79 (1.11 to 2.89) | 1.87 (1.05 to 3.36) | 133 | 35 | 1.76 (1.01 to 3.07) | 1.27 (0.63 to 2.55) | |
| >11.6 | 67 | 25 | 1.49 (0.84 to 2.65) | 2.10 (0.84 to 5.28) | 79 | 13 | 1.10 (0.54 to 2.26) | 1.04 (0.33 to 3.27) | |
| ptrend† | 0.08 | 0.05 | 0.47 | 0.77 | |||||
| Physical exertion | Quartile 1 (<7) | 124 | 18 | 1.00 | 1.00 | 128 | 14 | 1.00 | 1.00 |
| Quartile 2 (7–7.9) | 102 | 31 | 2.09 (1.11 to 3.96) | 1.95 (0.98 to 3.86) | 115 | 18 | 1.43 (0.68 to 3.01) | 1.38 (0.62 to 3.09) | |
| Quartile 3 (8–8.9) | 95 | 37 | 2.68 (1.44 to 5.00) | 2.15 (1.09 to 4.23) | 106 | 26 | 2.24 (1.11 to 4.51) | 2.08 (0.97 to 4.46) | |
| Quartile 4 (>8.9) | 74 | 39 | 3.63 (1.94 to 6.81) | 3.30 (1.63 to 6.71) | 89 | 24 | 2.47 (1.21 to 5.03) | 2.92 (1.31 to 6.52) | |
| ptrend† | <0.0001 | 0.001 | |||||||
| Physical isometric loads | Quartile 1&2 (<5) | 258 | 63 | 1.00 | 1.00 | 274 | 47 | 1.00 | 1.00 |
| Quartile 3 (5–5.9) | 113 | 46 | 1.67 (1.07 to 2.59) | 1.82 (1.07 to 3.1) | 132 | 27 | 1.19 (0.71 to 2.00) | 1.45 (0.79 to 2.68) | |
| Quartile 4 (>5.9) | 23 | 16 | 2.85 (1.42 to 5.71) | 3.60 (1.6 to 8.06) | 31 | 8 | 1.51 (0.65 to 3.47) | 1.72 (0.68 to 4.36) | |
| ptrend† | <0.001 | <0.001 | |||||||
| Job demands | Quartile 1 (<30) | 111 | 29 | 1.00 | 1.00 | 123 | 17 | 1.00 | 1.00 |
| Quartile 2 (30–32) | 118 | 30 | 0.97 (0.55 to 1.72) | 1.18 (0.58 to 2.39) | 123 | 25 | 1.47 (0.76 to 2.86) | 1.62 (0.73 to 3.58) | |
| Quartile 3 (32–35) | 83 | 27 | 1.25 (0.69 to 2.26) | 1.64 (0.72 to 3.73) | 96 | 14 | 1.06 (0.50 to 2.25) | 1.15 (0.43 to 3.04) | |
| Quartile 4 (>35) | 83 | 39 | 1.80 (1.03 to 3.14) | 2.77 (1.06 to 7.28) | 96 | 26 | 1.96 (1.01 to 3.82) | 2.67 (0.88 to 8.13) | |
| ptrend† | 0.02 | 0.03 | |||||||
| Job satisfaction | Not satisfied | 10 | 7 | 1.00 | 1.00 | 12 | 5 | 1.00 | 1.00 |
| Somewhat satisfied | 180 | 54 | 0.43 (0.16 to 1.18) | 0.33 (0.11 to 1.01) | 198 | 36 | 0.44 (0.14 to 1.31) | 0.44 (0.13 to 1.42) | |
| Very satisfied | 205 | 64 | 0.45 (0.16 to 1.22) | 0.34 (0.11 to 1.05) | 228 | 41 | 0.43 (0.14 to 1.29) | 0.31 (0.09 to 1.08) | |
| ptrend† | 0.51 | 0.35 | 0.42 | 0.08 | |||||
* Full model controlled: age, gender, ethnicity, BMI, medical history of MSD, smoking behaviour, shop size, years of employment in garment industry, number of sewing machine operated, number of rest break, job strain, and social support; † p value for trend across categories (Pearson chi-squared test).
We did not observe consistent patterns or more than moderate increases in symptom reporting with some measures such as the number of tasks performed in the past month, the number of days or hours worked per week, the maximum continuous work period, the total period of rest time in a day, or the number of rests taken in a day (data not presented). However, for our compound measure work–rest ratio we observed an association with reporting of symptoms in the neck/shoulder region; i.e. working on a schedule with a work–rest ratio between 9.2 and 11.6 was associated with a 87% increase in the prevalence of reporting neck/shoulder pain in the past month, and a twofold increases was suggested for a ratio above 11.6, yet the later estimate was imprecise. A positive trend with an increase in this ratio was suggested (ptrend = 0.05).
The strongest and most consistent association and a strong trend for increasing pain in both upper body regions was observed for the compound scale of physical exertion derived from the JCQ. Another scale, high physical isometric load was also strongly associated with the prevalence of neck/shoulder but not distal upper extremity pain. There was no significant relationship between job control, social support and job insecurity and prevalence of neck/shoulder or distal upper extremity MSD (data not shown).
The prevalence of a neck/shoulder pain was higher among subjects who perceived high job demands, and low job satisfaction. We observed a positive increasing trend for job demands and the prevalence of neck/shoulder pain (ptrend = 0.03) and a similar size association with highest level of demands for distal upper extremity pain, but this estimate was less precisely estimated. However, low job satisfaction was strongly associated with the prevalence of distal upper extremity pain.
Discussion
This is one of the largest studies evaluating upper body musculoskeletal symptoms among garment workers. Garment workers are a vulnerable working population, since they are primarily immigrants of low socio-economic status, low educational level, and without union representation. We hypothesised that work-organisational factors may be particularly important risk factors for this population due to the lack of control over job tasks, work schedules and work–rest patterns. Our findings suggest that a number of work-organisational factors as well as some personal factors are associated with increased prevalence of upper body disorders even after mutual adjustment for each other, underscoring the multifactorial nature of WMSDs in these workers.
There were several notable findings regarding the relation of personal factors to upper body disorders. First, the lack of an association between elevated BMI and upper body WMSDs. While elevated BMI has been related to entrapment neuropathies and low back pain among workers,22 the relation to other upper body disorders seems less consistent and a lack of association with BMI is supported by our data.23 Second, the literature suggests that living with children is associated with neck and shoulder pain in sewing machine operators.24 We observed an increased risk for neck/shoulder pain among workers who were single and lived alone compared to workers who were married and lived with a spouse, but no relation between pain and having children at home. Third, we observed that the reported pain prevalence for both upper body regions was lower for males compared with females and the prevalence of neck/shoulder disorders was higher for Hispanics compared with Asians.
A longitudinal study of apparel manufacturing employees conducted in the south-eastern United States in the early 1990s25 found that older age was associated with WMSD rates especially among those above 45 years of age. We did not observe a trend of increasing pain with increasing age. Operators less than 30 years of age reported a higher prevalence of neck–shoulder pain than their older co-workers. This finding may be explained by a healthy-worker selection effect such that healthier garment workers remain employed longer even in physically demanding jobs. Another possible explanation for this apparent inconsistency is that neck–shoulder pain is more prevalent among sewing machine operators and may develop earlier than distal upper extremity pain. The neck–shoulder pain may stop workers from remaining in sewing jobs, while distal upper extremity pain may take longer to develop and therefore have less impact on removing workers from sewing jobs. There is evidence from workers who do computer intensive work that neck–shoulder pain is of more rapid onset among new employees than distal upper extremity pain.26
Previous studies suggested that the prevalence of upper body WMSDs increases with years of employment as sewing machine operators.4,5 Blader et al. reported that years working as a sewing machine operator predicted risk of neck/shoulder problems.6 We confirmed an association with years of employment for distal upper extremity pain but not for neck/shoulder pain, the later possibly attributable to the above mentioned healthier worker survival selection effect in our cross-sectional survey.
Work-organisational factors
Sewing machine operators have previously been identified as one of the groups at highest risk for developing distal upper extremity disorders, likely due to mono-task, repetitive pinching activities.27,28,29 In our study we found that increased variety of work was associated with a decreased prevalence of upper body pain. Working with multiple machines may introduce a form of job rotation and task diversity that distributes the load to multiple muscle groups rather than continuously loading a limited set of muscles. This finding is supported by Schibye et al. who reported that for many sewing machine operators, neck and shoulder symptoms are reversible and may be influenced by reallocation to more varied work tasks.30
The less-flexible work schedules typical of large shops may be contributing to the observed elevated prevalence of WMSDs. On the other hand, the pay method seemed to affect the prevalence of upper body pain in opposite ways in large and small shops: piece rate work – usually interpreted as an incentive for increasing physical stress by increasing speed – was associated with higher risk in small shops but not in large shops. Generally, in the garment industry, employees are paid via piece rate and this was also the case for workers in our population (60–70% piece rate workers). While our estimates for payment method in small shops are tentative and imprecise due to a smaller sample size, we would like to provide a qualitative explanation for these differences. The small shops participating in our study are mostly family owned businesses and hourly rate workers tended to be relatives or family members of the shop owners. These workers may have less incentive, compared to other workers who are paid at piece rate to work faster and harder to increase their pay. In contrast, in our large shops, it was common policy to ‘promote' piece rate workers to hourly rate jobs if they showed high performance and skill. Yet, once promoted, these workers must maintain a high work rate in order to retain their hourly rate status. Thus, the differences we observed might be due to the differences between the hourly workers in each shop type, i.e. the reference group.
Interestingly, the number of hours or number of days worked per week as singular measures were not strongly associated with upper body disorders, and we did not observe a consistent pattern in symptom reporting with singular measures of work–time management.
Yet, a chronological diary of work periods and rest periods allowed us to compute the ratio of work time to recovery time, and we observed a strong association between this ratio and neck–shoulder disorders. Thus, this compound measure was a better predictive measure than any singular measure, such as work duration or number of rests, possibly because longer work duration may not affect WMSDs as long as rest periods are increased accordingly as well. It has also been observed previously that the higher the work–rest ratio the greater the chance for fatigue, error, and accidents.31
Although the aetiological mechanisms are still poorly understood, there is evidence that psychosocial factors related to the work environment play a role in the development or reporting of WMSD. While previous study findings are not entirely consistent, most studies suggest that perceptions of intensified workload,32 monotonous work,33,34 limited job control,32,33,35 job dissatisfaction,36 and low social support33 are risk factors for WMSD of the neck, shoulders or distal upper extremity region. We confirmed some of these associations in our study. A perception of low job satisfaction, high physical exertion and high physical isometric loads was strongly associated with an elevated prevalence of a neck/shoulder disorders. Likewise, job dissatisfaction and high physical exertion were strongly associated with an elevated prevalence of distal upper extremity disorders.
Limitations and strengths of study
Some researchers have suggested that subjective self-reported data regarding workload may limit the predictive value for adverse health effects due to recall bias.37 Bias due to self-reporting is a potential problem in many job strain studies, since exposures and outcomes are usually assessed simultaneously in study participants. The data presented here came from a convenience sample of 13 shops located in the Los Angeles basin. Convenience sampling may result in estimates non-representative of garment workers in general, to the extent that the shops and employees are different from the non-participating shops. Due to rigorous eligibility criteria, our population most likely represented a stable garment worker population. We obtained no information for non-participants and there is little reliable information published regarding the characteristics of the immigrant workforce employed in the garment industry in Los Angeles.
Furthermore, low internal consistency for measures of psychosocial stress obtained with the JCQ may reduce the reliability of our results. One possible reason for the low internal consistency of some composite measures may be the unimportance or irrelevance of certain items collected in the JCQ for this immigrant worker population. Sensitivity analyses, however, indicated that – except for the job demand estimates – our analyses based on the original format of the JCQ was unlikely to have resulted in strong bias, but may have reduced precision of the estimates. We observed associations of similar strength and direction as reported in previous studies performed in other working populations.11
This study has two methodological strengths. One is that our case criteria for WMSDs relied on a two-dimensional factor combining both pain frequency and pain intensity instead of using a single measure of pain. The other is that measures of physical and psychosocial stress were constructed as compound measures, such as the work rest ratio or the JCO factors. Results based on a complex combination of single items into composite measures are likely less prone to recall related bias.
In conclusion, our study results indicate that both personal and work-organisational factors are associated with increased prevalence of upper body WMSDs in sewing machine operators. Owners of sewing companies may be able to reduce WMSDs among employees by adopting rotations between different types of workstations thus, increasing task variety; by either shortening work periods or increasing rest periods to reduce the work–rest ratio; and by improving the work-organisational management to control psychosocial stressors. These findings can be used to guide prevention efforts for garment workers and may have important public health implications for this workforce of immigrant labourers.
Main messages
Upper body WMSD is a common adverse health effect among garment workers.
Work-organisational and personal factors were associated with increased prevalence of moderate or severe upper body musculoskeletal pain among garment workers.
Policy implication
Owners of sewing companies may be able to reduce or prevent WMSDs among employees by adopting rotations between different types of workstations thus increasing task variety; by either shortening work periods or increasing rest periods to reduce the work–rest ratio; and improving the work-organisation to control psychosocial stressors.
Acknowledgements
This study was supported in part by a grant (1 R01 OH007779) from the Centers for Disease Control/National Institutes for Occupational Safety and Health. The authors wish to thank the Los Angeles Garment Worker Center and participating garment shops located in the Los Angeles basin for their cooperation and support of this study.
References
- 1.International Labour Office Geneva Labour practices in the footwear, leather, textiles, and clothing industries. 10-16-2000. Geneva: International Labour Organization (ILO), TMLFI/2000. 8-1- 2004
- 2.Bureau of Labor Statistics Current population survey (CPS) – Employed persons by detailed industry, sex, race, and Hispanic or Latino ethnicity. March 25 2004
- 3.Chan J, Janowitz I, Lashuay N.et al Preventing musculoskeletal disorders in garment workers: preliminary results regarding ergonomics risk factors and proposed interventions among sewing machine operators in the San Francisco Bay Area. Appl Occup Environ Hyg 200217247–253. [DOI] [PubMed] [Google Scholar]
- 4.Andersen J H, Gaardboe O. Musculoskeletal disorders of the neck and upper limb among sewing machine operators: a clinical investigation. Am J Ind Med 199324689–700. [DOI] [PubMed] [Google Scholar]
- 5.Andersen J H, Gaardboe O. Prevalence of persistent neck and upper limb pain in a historical cohort of sewing machine operators. Am J Ind Med 199324677–687. [DOI] [PubMed] [Google Scholar]
- 6.Blader S, Barck-Holst U, Danielsson S.et al Neck and shoulder complaints among sewing-machine operators: A study concerning frequency, symptomatology and dysfunction. Appl Ergonom 199122251–257. [DOI] [PubMed] [Google Scholar]
- 7.Bureau of Labor Statistics Case and demographic characteristics for work-related injuries and illnesses involving days away from work. March 25, 2004. Bureau of Labor Statistics, U. S. Department of Labor. 8-9- 2004
- 8.Smith M J, Sainfort P C. A balance theory of job design for stress reduction. Int J Ind Ergonom 1989467–79. [Google Scholar]
- 9.Cox T, Ferguson E. Measurement of the subjective work environment. Work Stress 1994898–109. [Google Scholar]
- 10.Carayon P, Smith M J, Haims M C. Work organization, job stress, and work-related musculoskeletal disorders. Hum Factors 199941644–663. [DOI] [PubMed] [Google Scholar]
- 11.Ariens G A, van Mechelen W, Bongers P M.et al Psychosocial risk factors for neck pain: a systematic review. Am J Ind Med 200139180–193. [DOI] [PubMed] [Google Scholar]
- 12.Houtman I L, Bongers P M, Smulders P G.et al Psychosocial stressors at work and musculoskeletal problems. Scand J Work Environ Health 199420139–145. [DOI] [PubMed] [Google Scholar]
- 13.Rempel D, Wang P C, Janowitz I.et al A randomized control trial evaluating the effects of new task chairs on shoulder and neck pain among sewing operators: the Log Angeles Garment Study. Spine 200732931–938. [DOI] [PubMed] [Google Scholar]
- 14.Dickinson C E, Campion K, Foster A F.et al Questionnaire development: an examination of the Nordic Musculoskeletal questionnaire. Appl Ergonom 199223197–201. [DOI] [PubMed] [Google Scholar]
- 15.Karasek, R The job content questionnaire and user's guide. 10-1-1997. Lowell, University of Massachusetts Lowell
- 16.Greenland S. A semi-Bayes approach to the analysis of correlated multiple associations, with an application to an occupational cancer-mortality study. Stat Med 199211219–230. [DOI] [PubMed] [Google Scholar]
- 17.Landsbergis P A, Schnall P L, Warren K.et al Association between ambulatory blood pressure and alternative formulations of job strain. Scand J Work Environ Health 199420349–363. [DOI] [PubMed] [Google Scholar]
- 18.Hagberg M, Silverstein B, Wells R.et alWork-related musculoskeletal disorders (WMSDs): A reference book for prevention. London: Taylor & Francis, 1995
- 19.Jansen J P, Morgenstern H, Burdorf A. Dose–response relations between occupational exposures to physical and psychosocial factors and the risk of low back pain. Occup Environ Med 200461972–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Winkel J, Mathiassen S E. Assessment of physical work load in epidemiologic studies: concepts, issues and operational considerations. Ergonomics 199437979–988. [DOI] [PubMed] [Google Scholar]
- 21.Malchaire J, Cock N, Vergracht S. Review of the factors associated with musculoskeletal problems in epidemiological studies. Int Arch Occup Environ Health 20017479–90. [DOI] [PubMed] [Google Scholar]
- 22.Nathan P A, Istvan J A, Meadows K D. A longitudinal study of predictors of research-defined carpal tunnel syndrome in industrial workers: findings at 17 years. J Hand Surg [Br] 200530593–598. [DOI] [PubMed] [Google Scholar]
- 23.Werner R A, Franzblau A, Gell N.et al A longitudinal study of industrial and clerical workers: predictors of upper extremity tendonitis. J Occup Rehabil 20051537–46. [DOI] [PubMed] [Google Scholar]
- 24.Kaergaard A, Andersen J H. Musculoskeletal disorders of the neck and shoulders in female sewing machine operators: prevalence, incidence, and prognosis. Occup Environ Med 200057528–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dignan M, Hayes D, Main H.et al Cumulative trauma disorders among apparel manufacturing employees in the southeastern United States. South Med J 1996891057–1062. [DOI] [PubMed] [Google Scholar]
- 26.Gerr F, Marcus M, Ensor C.et al A prospective study of computer users: I. Study design and incidence of musculoskeletal symptoms and disorders. Am J Ind Med 200241221–235. [DOI] [PubMed] [Google Scholar]
- 27.Punnett L, Robins J M, Wegman D H.et al Soft tissue disorders in the upper limbs of female garment workers. Scand J Work Environ Health 198511417–425. [DOI] [PubMed] [Google Scholar]
- 28.Leigh J P, Miller T R. Occupational illnesses within two national data sets. Int J Occup Environ Health 1998499–113. [DOI] [PubMed] [Google Scholar]
- 29.Evans T H, Mayer T G, Gatchel R J. Recurrent disabling work-related spinal disorders after prior injury claims in a chronic low back pain population. Spine J 20011183–189. [DOI] [PubMed] [Google Scholar]
- 30.Schibye B, Skov T, Ekner D.et al Musculoskeletal symptoms among sewing machine operators. Scand J Work Environ Health 199521427–434. [DOI] [PubMed] [Google Scholar]
- 31.Hedge A. DEA 325 Human factors: ergonomics, anthropometrics and biomechanics CLASS NOTES. Cornell University Ergonomics Web. 8-19- 0003
- 32.Hales T R, Sauter S L, Peterson M R.et al Musculoskeletal disorders among visual display terminal users in a telecommunications company. Ergonomics 1994371603–1621. [DOI] [PubMed] [Google Scholar]
- 33.Ryan G A, Bampton M. Comparison of data process operators with and without upper limb symptoms. Community Health Stud 19881263–68. [DOI] [PubMed] [Google Scholar]
- 34.Ekberg K, Bjorkqvist B, Malm P.et al Case–control study of risk factors for disease in the neck and shoulder area. Occup Environ Med 199451262–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Theorell T, Harms-Ringdahl K, Ahlberg-Hulten G.et al Psychosocial job factors and symptoms from the locomotor system – a multicausal analysis. Scand J Rehabil Med 199123165–173. [PubMed] [Google Scholar]
- 36.Viikari-Juntura E, Riihimaki H, Tola S.et al Neck trouble in machine operating, dynamic physical work and sedentary work: a prospective study on occupational and individual risk factors. J Clin Epidemiol 1994471411–1422. [DOI] [PubMed] [Google Scholar]
- 37.Tsang P S, Velazquez V L. Diagnosticity and multidimensional subjective workload ratings. Ergonomics 199639358–381. [DOI] [PubMed] [Google Scholar]