Extranodal marginal zone B‐cell lymphoma of the mucosa‐associated lymphoid tissue (MALT lymphoma) of the lacrimal gland is a rare condition. Treatment options chiefly include radiation of the tumour, chemotherapy, surgical removal or a combination of these strategies.1 Radiation therapy is associated with a high risk of ocular morbidity, especially dry eye.1 Here, we report a case of a biopsy‐proven extranodal MALT lymphoma of the lacrimal gland treated with two courses of four weekly cycles of rituximab.
Case report
A 64‐year‐old woman presented with unilateral ptosis and swelling of her right lacrimal gland. Best‐corrected visual acuity was 20/25. Slit‐lamp examination showed severe punctate superficial keratopathy (basal secretion 0 mm OU). MRI scan detected a tumour of the lacrimal gland (fig 1A). Histopathological and immunohistochemical studies of a lacrimal gland biopsy specimen disclosed an extranodal MALT lymphoma (fig 2); typical extraorbital manifestations were excluded. Treatment was started with four weekly cycles of rituximab (each dose 375 mg/m2).
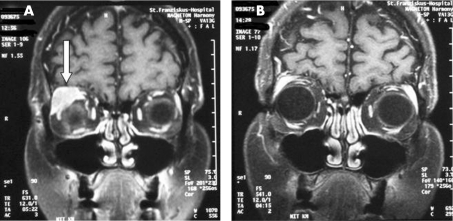
Figure 1 Coronal contrast‐enhanced T1‐weighted MR image shows MALT lymphoma (arrow) before therapy (A) and 12 months later (B).
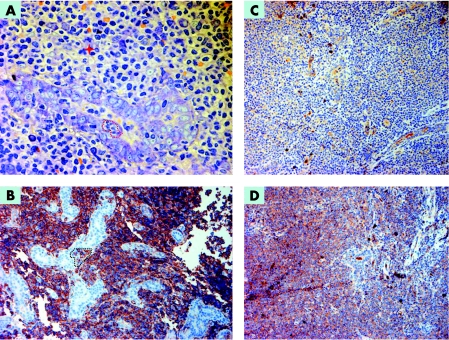
Figure 2 (A) Orbital soft tissue with destruction of the lacrimal gland by an atypical lymphoid infiltrate. Remnants of the glandular structures surrounded by atypical centrocytoid or monocytoid lymphatic cells with an increase in blasts (one atypical mitotic figure is highlighted with a cross) and scattered plasma cells can be seen. A typical intra‐acinar lymphoepithelial lesion is shown surrounded by a dotted line. Giemsa 630×. (B) The neoplastic lymphoid infiltrate is mainly composed of strongly CD20‐positive cells. Several destructive intraglandular lymphoepithelial lesions are clearly visible, one of which is highlighted by a surrounding dotted line. The complete phenotype of the lymphoma was CD20+, CD5−, CD23−, cyclinD1−, kappa+, lambda–; 200×. (C, D) Lambda and kappa light chain stainings show monoclonal light chain restriction of the neoplastic lymphoid cells, with a polyclonal background of plasma cells; 200×.
The MRI scan at 2 months showed a subtotal involution of the tumour. Schirmer values were 2 mm OU. Exophthalmus, which according to Hertel readings was 3 mm before treatment, had resolved 3 months after initiating therapy. Another four cycles of rituximab therapy were given 4 months after the first course to treat the residual lacrimal gland tumour. After 12 months the lacrimal gland tumour was no longer visible on MRI (fig 1B) and the Schirmer test score was 7 mm. Vision was unchanged and the corneal slit‐lamp appearance was normal. In addition to topical lubricants, the patient underwent temporary punctual occlusion with resorbable collagen plugs as therapy. No extraorbital manifestation of the MALT lymphoma occurred during the subsequent follow‐up period.
Comment
Patients treated with radiation for orbital MALT lymphomas often suffer from eye‐related side effects. In a recent paper, four of nine patients who received additional radiotherapy for orbital and/or conjunctival lymphoma suffered from dry eye, conjunctivitis and cataract. One of the patients eventually lost his sight due to radiation‐induced retinopathy.1 Particularly when lymphoma develops in the lacrimal gland, the therapeutic approach should aim to prevent further damage to the that gland.
Treatment with the anti‐CD20 monoclonal antibody rituximab for ocular adnexal MALT lymphomas has been reported primarily in recurring conjunctival lymphomas.2 Only a few studies also report on the treatment of lacrimal gland involvement.1,3,4 In a recent report, two patients with lacrimal gland lymphomas had a relapse after a median time of 5 months following primary rituximab therapy with one cycle of four weekly infusions.3 Rituximab therapy also had a beneficial effect on the salivary and lacrimal gland function in patients with primary Sjögren syndrome associated with MALT lymphoma of the parotid gland.5 Our patient presented with severe dry eye and a very low Schirmer test score. Notably, rituximab treatment led to significant relief of the patient's complaints and increased tear secretion. Rituximab may be considered as a first‐line therapy for lacrimal MALT lymphoma when radiation therapy is expected to aggravate the dry eye symptoms or when a reduction in the tumour size is anticipated before radiation therapy. In our patient two courses of four weekly cycles of rituximab therapy led to a prolonged remission period.
Footnotes
Competing interests: None.
Informed consent was obtained for publication of the person's details in this report.
References
- 1.Charlotte F, Doghmi K, Cassoux N.et al Ocular adnexal marginal zone B cell lymphoma: a clinical and pathologic study of 23 cases. Virchows Arch 2006448506–516. [DOI] [PubMed] [Google Scholar]
- 2.Nuckel H, Meller D, Steuhl K P.et al Anti‐CD20 monoclonal antibody therapy in relapsed MALT lymphoma of the conjunctiva. Eur J Haematol 200473258–262. [DOI] [PubMed] [Google Scholar]
- 3.Ferreri A J, Ponzoni M, Martinelli G.et al Rituximab in patients with mucosal‐associated lymphoid tissue‐type lymphoma of the ocular adnexa. Haematologica 2005901578–1579. [PubMed] [Google Scholar]
- 4.Asproudis I, Gorezis S, Charonis G C.et al Mucosa‐associated lymphoid tissue lymphoma of the lacrimal gland—a case report. In Vivo 2005191105–1109. [PubMed] [Google Scholar]
- 5.Pijpe J, van Imhoff G W, Vissink A.et al Changes in salivary gland immunohistology and function after rituximab monotherapy in a patient with Sjogren's syndrome and associated MALT lymphoma. Ann Rheum Dis 200564958–960. [DOI] [PMC free article] [PubMed] [Google Scholar]