After diabetic retinopathy, retinal venous occlusion (RVO) is the most common cause of retinopathy leading to severe visual loss in all age groups. Generally, RVO is associated with systemic diseases with significant morbidity and mortality. The risk of RVO is increased in patients older than 65 years of age with systemic hypertension, cardiovascular disease, diabetes and obesity.1 Patients younger than 50 years of age may have other underlying conditions requiring appropriate investigation and treatment.2,3 We describe the development of central retinal venous occlusion (CRVO) and the efficacy of intravitreal triamcinolone acetonide injection (IVTA) for associated cystoid macular oedema (CME) in a young healthy woman after she was started on systemic multiple anti‐androgen therapy for treatment of hirsutism.
Case report
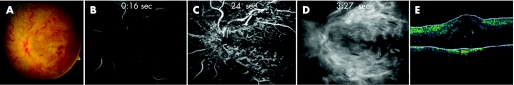
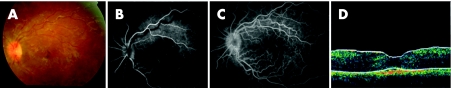
A 24‐year‐old woman with a 4‐month history of painless loss of vision and a diagnosis of CRVO in her left eye (OS) was referred for further evaluation and management. Her ocular history revealed squint surgery and amblyopia in her right eye (OD) since childhood. Since puberty she had had acne and hirsutism that were unsatisfactorily treated conservatively. Seven months earlier she had sought treatment for the hirsutism and was started on systemic multiple anti‐androgen therapy that included Noractone (spironlactone) 25 mg three times daily, Androcur (cyproterone acetate) 25 mg twice daily and Diane‐35 (cyproterone acetate 2 mg and ethinyl oestradiol 35 μg) once daily. These medications were discontinued by a local ophthalmologist after the discovery of CRVO. The patient reported no other systemic disorder and family history was non‐contributory. Her visual acuity (VA) was 20/300 in OD and 20/200 in OS with normal intraocular pressures. Slit‐lamp examination was unremarkable with no evidence of rubiosis iridis in OS. Dilated fundus examination of OD was within normal limits; however, OS showed flame‐shaped haemorrhages with tortuous dilated retinal veins (fig 1A). There was evidence of significant CME but no evidence of retinal neovascularisation on the disc or elsewhere. Intravenous fluorescein angiography of OS fundus showed delayed fillings and diffuse CME without any evidence of capillary non‐perfusion or abnormal neovascularisation (fig 1B–D). Central macular thickness by optical coherence tomography was 736 μm (fig 1E). A diagnosis of non‐ischaemic CRVO with extensive CME in OS was established. Her medical evaluation revealed normal blood pressure and physical examination. Mild microcytic hypochromic anaemia was noted in her laboratory work‐up. Her erythrocyte sedimentation rate, protein electrophoresis, plasma viscosity, lipid profile, plasma homocysteine, sickling test, anti‐phospholipid antibodies (cardiolipin antibodies IgG, IgM), plasma fibrinogen, lipoprotein A, abnormal factor V Leiden, factors VII, VIII, XII, anti‐thrombin III, protein S, and protein C were normal. She had negative anti‐nuclear antibody with non‐reactive TPHA. Application of grid laser therapy to the macular area did not resolve her CME. However, a single injection of IVTA (4 mg/0.1 ml) resulted in a dramatic decrease in CME (fig 2A) and improvement of her VA to 20/50. The improvement in CME was verified by intravenous fluorescein angiography (IVFA; fig 2B,C) and optical coherence tomography (OCT; fig 2D), and was sustained over a 3‐year follow‐up period.
Figure 1 A baseline fundus photograph prior to treatment of OS (A) and intravenous fluorescein angiography of OS fundus, early phase (B), mid phase (C) and late phase (D); optical coherence tomography of macular area of OS (E).
Figure 2 Fundus photograph of the OS after a single intravitreal triamcinolone acetonide injection showing resolution of cystoid macular oedema (A), which was evident on intravenous fluorescein angiography (B, C) as well as on optical coherence tomography of the macular area (D).
Discussion
Hirsutism (excessive hair growth), acne and seborrhea are distressing and common endocrine problems in women which may be difficult to manage conservatively. One cause of hirsutism is excessive androgen production by the ovaries. Anti‐androgen regimes effective for hirsutism include spironolactone, cyproterone acetate and cyproterone acetate with ethinyl oestradiol (Diane‐35).4 These medications suppress the release of gonadotrophin hormone, which reduces androgen production. Cyproterone used alone has a minor effect on blood clotting factors, however in combination with ethinyl oestradiol it enhances coagulation. Numerous reports have described vascular complications due to drugs after use of the oral contraceptive pill (OCP). Use of the OCP is known to be a risk factor for cardiovascular and cerebrovascular diseases and, as this report suggests, CRVO.5 Other serious ocular complications include branch RVO, artery occlusion and acute ischaemic optic neuropathy.5,6 Investigation in a 28‐year‐old CRVO patient treated with an anti‐androgen drug revealed an abnormality of the haemostatic system; however, 1 month after the primary episode CRVO resolved and the fundus became normal without macular oedema.7 Our case suggests that anti‐androgen therapy in young patients may result in CRVO. A single injection of IVTA (4 mg/0.1 ml) may be effective to resolve CRVO‐associated CME and improve VA. To the best of our knowledge this is the first report of a case of CRVO due to multiple anti‐androgen therapy in a young female with hirsutism. Patients should be informed of the potential side effects of such medications and warned that anti‐androgen therapy may result in CRVO in addition to other possible thromboembolic disorders; the use of these drugs should be discouraged, especially in patients with monocular vision. These medications should be discontinued at the first sign of any visual disturbance and the patient should be carefully monitored for any signs of significant CME which can be treated with IVTA.
Footnotes
Competing interests: None declared.
Informed consent was obtained for publication of the person's details in this report.
References
- 1.The Eye Disease Case‐Control Study Group Risk factors for central retinal vein occlusion. Arch Ophthalmol 1996114545–554. [PubMed] [Google Scholar]
- 2.Dodson P M, Kritzinger E E. Underlying medical conditions in young patients and ethnic differences in retinal vein occlusion. Trans Ophthalmol Soc UK 1985104114–119. [PubMed] [Google Scholar]
- 3.Fong A C O, Shatz H. Central retinal vein occlusion in young adults. Surv Ophthalmol 199337393–417. [DOI] [PubMed] [Google Scholar]
- 4. Diane‐35 [product monograph]. In: Compendium of pharmaceuticals and specialties. Ottawa: Canadian Pharmacists Association, 2002493–495.
- 5.Stowe G C I I I, Zakov Z N, Albert D M. Central retinal vascular occlusion associated with oral contraceptives. Am J Ophthalmol 197886798–801. [DOI] [PubMed] [Google Scholar]
- 6.Glacet‐Bernard A, Kuhn D, Soubrane G. Ocular complications of hormonal treatments: oral contraception and menopausal hormonal replacement therapy. Contracept Fertil Sex 199927285–290. [PubMed] [Google Scholar]
- 7.Zaoui M, Cordebar B, Naoun‐Hubert I.et al Central retinal vein occlusion in a patient treated with antiandrogenic drug. J Fr Ophthalmol 20002342–44. [PubMed] [Google Scholar]