Abstract
Aim
To describe the phenotype and to analyse the peripherin/RDS gene in 10 unrelated families with multifocal pattern dystrophy simulating Stargardt disease (STGD1).
Methods
The probands of 10 families and 20 affected family members underwent an ophthalmic examination including dilated fundus examination, fundus autofluorescence imaging and optical coherence tomography (OCT). In all probands and in selected family members, fluorescein angiography, electrophysiological testing and visual field analysis were performed. Blood samples were obtained from affected and unaffected family members for analysis of the peripherin/RDS gene.
Results
All 10 probands carried mutations in the peripherin/RDS gene. Nine different mutations were identified, including six mutations that were not described previously. All probands showed a pattern dystrophy with yellow–white flecks in the posterior pole that strongly resembled the flecks seen in STGD1, on ophthalmoscopy as well as on autofluorescence and OCT. Clinical findings in the family members carrying the same mutation as the proband were highly variable, ranging from no visible abnormalities to retinitis pigmentosa.
Conclusions
Mutations in the peripherin/RDS gene are the major cause of multifocal pattern dystrophy simulating STGD1/fundus flavimaculatus. This autosomal dominant disorder should be distinguished from autosomal recessive STGD1, in view of the different inheritance pattern and the overall better visual prognosis.
Autosomal dominant pattern dystrophies constitute a group of disorders characterised by deposits of yellow, orange or grey pigment, predominantly in the macular area. In general, these disorders are relatively benign, manifesting usually in midlife with mild‐to‐moderate disturbance of central vision.1,2,3,4 Nevertheless, severe vision loss may occur in up to 50% of the affected individuals after the age of 70, due to atrophy of the retinal pigment epithelium (RPE)‐photoreceptor complex and/or the development of choroidal neovascularisation.5,6,7,8,9 In addition, progression to a more widespread retinal dystrophy with characteristics of retinitis pigmentosa may develop depending on the underlying genotype.10,11 In the classification according to Gass, five main categories of pattern dystrophy are discriminated, based on the pattern of pigment distribution: adult‐onset foveomacular vitelliform dystrophy, butterfly‐shaped pigment dystrophy, reticular dystrophy of the retinal pigment epithelium, multifocal pattern dystrophy simulating fundus flavimaculatus and fundus pulverulentus.2 A striking interfamilial and intrafamilial phenotypic variability has been described by several authors and different subtypes of pattern dystrophy have even been reported in the individual patient.4,5,6,7,10,12,13,14,15,16,17,18,19,20,21,22,23,24 Pattern dystrophy is genetically heterogeneous, but mutations in the peripherin/RDS gene are frequently encountered.5,11,23,25,26,27,28 Weleber and co‐workers reported pattern dystrophy, retinitis pigmentosa and fundus flavimaculatus in a single family with family members carrying the same peripherin/RDS mutation.29 Besides pattern dystrophy and autosomal dominant retinitis pigmentosa, peripherin/RDS mutations have been associated with a wide range of other retinal dystrophies, such as central areolar choroidal dystrophy, autosomal dominant cone‐rod dystrophy and digenic retinitis pigmentosa.11,25,26,27 The gene product of peripherin/RDS is the integral membrane protein peripherin/rds, which plays an important role in photoreceptor outer segment morphogenesis.30,31,32 In this study, we describe the clinical findings and the underlying genetic defects of patients in 10 unrelated families with multifocal pattern dystrophy resembling Stargardt disease (STGD1)/fundus flavimaculatus.
Patients and methods
The research described in this study conformed to the tenets of the Declaration of Helsinki and was approved by the committee on research involving human subjects at the Radboud University Nijmegen Medical Centre (Nijmegen). Informed consent was obtained from all participants before enrolling them in the clinical and molecular genetic studies.
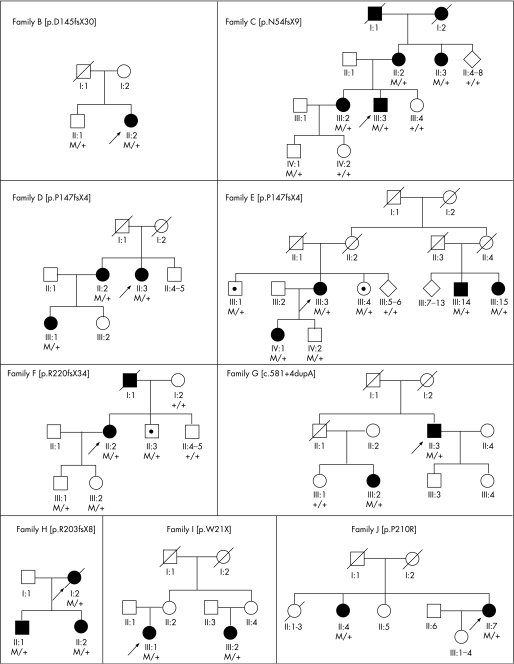
Figure 1 Pedigrees of the examined families. The probands with multifocal pattern dystrophy are indicated with an arrow. The specific mutations have been put between brackets and are indicated by an M within the pedigree. Mutation carriers who showed only mild foveal abnormalities, without signs of multifocal pattern dystrophy, are indicated with a black dot. The pedigree of proband A (p.D157N) is not shown, as he was the only person of his family who was clinically affected and who was examined.
Molecular genetic studies
Peripheral venous blood samples were obtained from the 10 probands and from 39 family members. Their genomic DNA was isolated as described elsewhere.33 The three coding exons and splice junctions of the peripherin/RDS gene were amplified by the polymerase chain reaction, and these fragments were then subjected to sequence analysis to detect mutations.23
Clinical studies
We examined 10 probands with multifocal pattern dystrophy simulating fundus flavimaculatus. Seven of these patients had received the diagnosis multifocal pattern dystrophy in the past. Three of the 10 probands (E, G and H) were identified retrospectively when a group of 15 presumed STGD1 patients without ABCA4 mutations were analysed for peripherin/RDS mutations. The medical histories of the 10 probands were obtained; subsequent clinical examination included best‐corrected Snellen visual acuity, indirect ophthalmoscopy and fundus photography. In addition, fundus autofluorescence (AF) imaging (Heidelberg Retina Angiograph (HRA) 2, Heidelberg Engineering, Dossenheim, Germany) was performed in all probands using a previously described protocol,34 as well as optical coherence tomography (OCT) (Stratus OCT, Carl Zeiss Meditech, Inc., Dublin, California, USA), using the Macular Thickness Map protocol. The probands also underwent fluorescein angiography and visual field analysis, by means of Goldmann perimetry (stimuli V4e‐III4e‐I4e‐I3e‐I2e‐I1e) and Humphrey 10‐2 Swedish Interactive Thresholding Algorithm (SITA)‐Fast visual field analysis of the central 10° of the visual field, except for patients 8 and 10 who were unavailable for visual field analysis. A full‐field electroretinography (ERG) and an electro‐oculography (EOG) were performed in all probands according to the guidelines of the International Society for Clinical Electrophysiology of Vision (ISCEV), except for proband H in whom the ERG and EOG were recorded according to an older protocol.35 Additionally, we examined the 20 family members who carried the same mutation as the proband of that family. The medical history was obtained in all of these 20 family members and a clinical examination was performed including fundus photography, fundus AF imaging and OCT. Six affected family members underwent full‐field ERG and EOG according to the ISCEV standards, whereas one patient underwent these examinations according to the protocol by Thijssen et al.35
Results
Molecular genetic findings
All 10 probands carried mutations in the peripherin/RDS gene. Nine different mutations were identified, including five different frameshift mutations, two missense mutations and one nonsense mutation (table 1). Six of these mutations (p.D145fsX30, p.N54fsX9, p.R220fsX34, c.581+4dupA, p.R203fsX8 and p.W21X) have not been described previously. The splice site mutation c.581+4dupA was detected in proband G. This mutation is predicted to completely abolish splicing.36 The six novel mutations were not found in 92 control individuals. The frameshift mutation p.P147fsX4 was identified in two unrelated probands (probands D and E). Of the 39 additional family members that were screened for the peripherin/RDS mutation that was found in the proband, 20 family members were shown to also carry the same mutation as the proband (table 2).
Table 1 Summary of clinical findings in the probands with multifocal pattern dystrophy.
| Proband number | Sex | Age at onset (y) | Age (y) | Visual acuity | ERG photopic* | ERG scotopic* | EOG† | Macula | Peripheral retina | Mutation | Effect | Previously described | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OD | OS | OD | OS | OD | OS | OD | OS | |||||||||
| A | M | 34 | 43 | 1.2 | 1.2 | SA | A | A | N | 2.6 | 2.1 | Pattern of multiple yellow lesions (fig 3) | No abnormalities | c.469G>A | p.D157N | Yes38 |
| B | F | 35 | 41 | 0.9 | 0.8 | A | SA | N | N | 1.5 | 2.4 | OD: multiple pigmented round lesions. OS: butterfly‐shaped pattern dystrophy (fig 2) | No abnormalities | c.433_434delGA | p.D145fsX30 | No |
| C | M | 47 | 56 | 1.2 | 1.0 | SA | SA | SA | SA | 1.7 | 1.6 | Atrophic confluence of yellow‐white lesions, surrounded by STGD1‐like lesions | Discrete mid‐peripheral granular pigmentary changes | c.163delT | p.N54fsX9 | No |
| D | F | 50 | 61 | 0.8 | 0.025 | SA | SA | SA | SA | 1.0 | 1.0 | Extensive chorioretinal atrophy | (Mid‐)peripheral atrophy, bone spicule and paravenous pigmentation, narrow vasculature, temporal paleness of optic disc | c.441delT | p.P147fsX4 | Yes39 |
| E | F | 48 | 57 | 1.0 | 0.9 | N | N | N | A | 2.0 | 2.0 | Confluent atrophic yellow‐white lesions, surrounded by STGD1‐like flecks | Peripheral atrophy, reticular pigmentary pattern | c.441delT | p.P147fsX4 | Yes39 |
| F | F | 45 | 51 | 0.5 | 1.0 | N | N | N | A | 2.0 | 1.7 | Round area of chorioretinal atrophy, surrounded by STGD1‐like flecks (fig 3) | No abnormalities | c.658delC | p.R220fsX34 | No |
| G | M | 45 | 73 | 0.05 | 0.05 | NR | NR | NR | NR | 2.8 | 2.6 | Extensive chorioretinal atrophy (fig 4) | Peripheral atrophy, OD perivascular pigmentation | c.581+4dupA | splice defect | No |
| H | F | 48 | 65 | 0.017 | 0.4 | N‡ | N‡ | N‡ | N‡ | 1.7‡ | 1.9‡ | Central atrophy, surrounded by STGD1‐like yellowish lesions | No abnormalities | c. 607_620delCGGTACCTGGTGGA | p.R203fsX8 | No |
| I | F | 44 | 55 | 0.6 | 0.8 | SA | SA | N | N | 1.5 | 1.4 | Atrophic confluence of yellow‐white lesions, surrounded by STGD1‐like lesions | No abnormalities | c.63G>A | p.W21X | No |
| J | F | 55 | 81 | 0.017 | 0.5 | SA | SA | A | A | 1.6 | 1.7 | OD: chorioretinal atrophy, OS: atrophic confluence of yellow‐white lesions, with small areas of profound atrophy | No abnormalities | c.629C>G | p.P210R | Yes27,40 |
*ERG results are expressed in abbreviations that reflect the amplitude: N, normal (equal to or above the lower 5% of the range for a normal population: photopic ⩾78 μV, scotopic ⩾263 μV); A, abnormal (1–5% of normal range: photopic: ⩾69 μV and <78 μV, scotopic: ⩾195 μV and <263 μV); SA, severely abnormal (below 1% of normal range: photopic <69 μV, scotopic <195 μV); NR, non‐recordable. †Values are Arden ratios: ISCEV: normal if ⩾2.0, non‐ISCEV: normal if ⩾1.8. ‡Recorded prior to ISCEV regulations according to the protocol described by Thijssen et al.35
Table 2 Summary of clinical findings in family members with identical peripherin/RDS mutation as the probands.
| Family | Pedigree number | Mutation | Age at onset (y) | Age (y) | Visual acuity | Retinal phenotype | ERG photopic* | ERG scotopic* | EOG† | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OD | OS | OD | OS | OD | OS | OD | OS | ||||||
| B | II:1 | p.D145fsX30 | – | 39 | 1.2 | 1.0 | ODS: normal | – | – | – | – | – | – |
| C | II:2 | p.N54fsX9 | 70 | 85 | 0.017 | 0.0033 | ODS: extensive atrophy of posterior pole, mid‐peripheral yellowish flecks | – | – | – | – | – | – |
| II:3 | p.N54fsX9 | – | 80 | 0.9 | 1.0 | ODS: macular pattern dystrophy changes, non‐confluent STGD1‐like flecks around vascular arcades | – | – | – | – | – | – | |
| III:2 | p.N54fsX9 | 56 | 57 | 1.2 | 1.2 | ODS: macular pattern dystrophy changes, STGD1‐like flecks around vascular arcades with incipient confluence | N | N | N | N | 2.1 | 2.9 | |
| IV:1 | p.N54fsX9 | – | 34 | 1.2 | 1.0 | OS: normal, OD: discrete spot of parafoveal pigmentary changes | – | – | – | – | – | – | |
| D | II:2 | p.P147fsX4 | 60 | 67 | 0.8 | 0.9 | ODS: confluence of STGD1‐like lesions and patches of atrophy in posterior pole, OD slight peripheral pigmentary changes | N | N | N | N | – | – |
| III:1 | p.P147fsX4 | – | 41 | 0.9 | 0.9 | ODS: macular pattern dystrophy changes, STGD1‐like flecks around vascular arcades | N | N | N | N | 1.8 | 1.6 | |
| E | III:1 | p.P147fsX4 | – | 59 | 0.017 (amblyopia) | 0.8 | ODS: mild foveal pigmentary changes, reticular pattern of pigmentary changes in peripheral retina | – | – | – | – | – | – |
| III:4 | p.P147fsX4 | – | 50 | 1.2 | 1.2 | ODS: mild foveal pigmentary changes | – | – | – | – | – | – | |
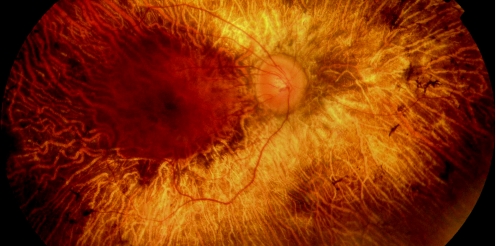
| III:14 | p.P147fsX4 | 12 | 60 | 0.2 | 0.2 | ODS: extensive chorioretinal atrophy outside macular area, bone spicule pigmentation, narrow retinal vessels, waxy pale optic disc | SA | SA | SA | SA | 1.0 | 1.0 | |
| III:15 | p.P147fsX4 | 35 | 65 | 0.6 | 0.6 | ODS: multifocal pattern dystrophy, yellow‐white flecks throughout posterior pole | – | – | – | – | – | – | |
| IV:1 | p.P147fsX4 | – | 37 | 1.2 | 1.0 | ODS: discrete foveal pigmentary changes, small yellow–white dots around retinal vascular arcades | – | – | – | – | – | – | |
| IV:2 | p.P147fsX4 | – | 32 | 1.6 | 0.0033 (trauma) | ODS: normal | – | – | – | – | – | – | |
| F | II:3 | p.R220fsX34 | 43 | 45 | 1.6 | 1.6 | ODS: small yellowish lesions in fovea, similar to lesions seen initially in proband B (fig 2) | – | – | – | – | – | – |
| III:1 | p.R220fsX34 | – | 29 | 1.0 | 1.0 | ODS: normal | – | – | – | – | – | – | |
| G | III:2 | c.581+4dupA | 49 | 50 | 0.8 | 0.8 | ODS: multifocal pattern dystrophy, atrophic confluence of STGD1‐like flecks | – | – | – | – | – | – |
| H | II:1 | p.R203fsX8 | – | 49 | 1.2 | 1.0 | ODS: small yellowish lesions in fovea, small STGD1‐like flecks around vascular arcades | N | A | N | N | 2.0 | 1.6 |
| II:2 | p.R203fsX8 | – | 45 | 0.9 | 0.8 | ODS: small yellowish lesions in fovea, small STGD1‐like flecks around vascular arcades (fig 2) | N | N | N | N | 1.8 | 1.6 | |
| I | III:2 | p.W21X | 30 | 30 | 0.8 | 0.5 | ODS: small yellow lesions with pigmented centre in foveal area, similar to lesions seen in proband B, many STGD1‐like flecks around vascular arcades | – | – | – | – | – | – |
| J | II:4 | p.P210R | 52 | 65 | 1.0 | 0.3 | OD: butterfly‐shaped pattern dystrophy, OS: foveal atrophy surrounded by pigmentary changes | N‡ | N‡ | A‡ | A‡ | 1.5‡ | 1.5‡ |
*ERG results are expressed in abbreviations that reflect the amplitude: N, normal (equal to or above the lower 5% of the range for a normal population: photopic ⩾78 μV, scotopic ⩾263 μV); A, abnormal (1–5% of normal range: photopic: ⩾69 μV and <78 μV, scotopic: ⩾195 μV and <263 μV); SA, severely abnormal (below 1% of normal range: photopic <69 μV, scotopic <195 μV); NR, non‐recordable. †Values are Arden ratios: ISCEV: normal if ⩾2.0, non‐ISCEV: normal if ⩾1.8. ‡Recorded prior to ISCEV regulations according to the protocol described by Thijssen et al.35
Clinical findings
The clinical characteristics are summarised in table 1. The mean age at onset was 45 (range: 34–55 years). The initial symptoms were metamorphopsia (6 patients), loss of visual acuity (4 patients), central scotomata (3 patients), and night blindness (5 patients). Seven probands reported additional family members with similar visual complaints. All probands retained reading vision in at least one eye, except for proband G, a 73‐year‐old man (c.581+4dupA). This patient experienced visual loss with metamorphopsia at age 45, in combination with night blindness. He lost the ability to read approximately 21 years later, at the age of 66 years.
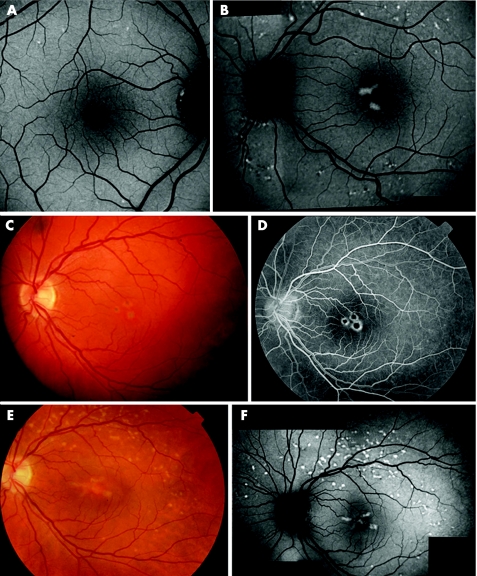
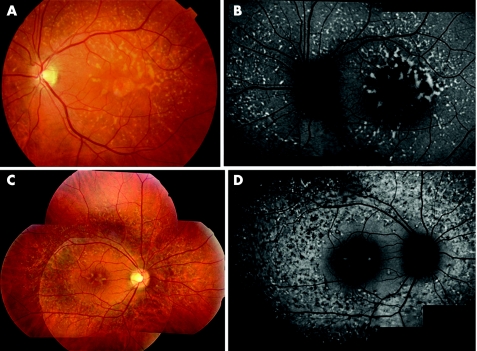
All patients showed irregular yellowish flecks in the posterior pole at a certain point in time, resembling the flecks seen in STGD1. These flecks were also found in variable size, shape and number in several asymptomatic family members who carried the same mutation as the proband of their family (fig 2). The flecks were mostly situated around the retinal vascular arcades, nasal and superior to the optic disc and in the macular area, where flecks were usually largest (figs 2 and 3). Probands A, C, D, G, I and J showed a variable degree of confluence and atrophy of the STGD1‐like flecks over a period of probably more than 5 years, based on the comparison of consecutive fluorescein angiograms (figs 3 and 4).
Figure 2 The development of lesions in multifocal pattern dystrophy. (A) Autofluorescence (AF) image of the 37‐year‐old daughter (E‐IV:1, p.P147fsX4) of proband E, demonstrating small dots of increased AF, in the absence of foveal lesions. This picture may represent an early stage of multifocal pattern dystrophy. (B) Composition of AF images of individual H‐II:2 (p.R203fsX8), showing two irregular lesions with increased autofluorescence in the macular area and small irregular flecks around the retinal vessels. Note that most of these flecks show adjacent zones of decreased AF. (C) Fundus photograph of proband B (p.D145fsX30) taken at the age of 35, demonstrating three pigmented spots with a depigmented border in the macula. (D) These lesions display a “dot and halo” aspect on the fluorescein angiogram, which was made before it was possible to perform AF imaging in the patients. (E) Six years later, the phenotype had evolved to a picture mimicking STGD1, with irregular yellow–white flecks around the vascular arcades, which showed predominantly increased AF on the composition of autofluorescence images (F). The macular lesion had a butterfly‐shaped configuration both on ophthalmoscopy and on the AF image (E, F).
Figure 3 Advanced multifocal pattern dystrophy. (A) Fundus photograph of proband F (p.R220fsX34) showing numerous yellowish flecks, scattered throughout the posterior pole, with the larger flecks situated around a central area of well‐circumscribed chorioretinal atrophy. (B) Autofluorescence (AF) image showing increased AF of the yellow lesions, together with a complete absence of AF in the central atrophic area. (C) A composition of fundus photographs of proband A (p.D157N) demonstrated a central lesion typical for pattern dystrophy. A large ring‐shaped, atrophic‐appearing area can be seen surrounding the macular area and optic disc. (D) These lesions could be delineated with more detail on a composition of AF images. The ring‐shaped zone showed confluence of the flecks. Granular zones of decreased AF were seen within this area of increased AF, which reflects the beginning atrophy. Towards the periphery, the flecks became less confluent and could be identified individually.
Figure 4 Fundus photograph of patient E‐III:14 (p.P147fsX4), showing a characteristic retinitis pigmentosa phenotype.
Besides these flecks, all patients displayed macular changes, ranging from a variety of patterns of yellow or greyish deposits in the foveomacular area to atrophic lesions in proband F (p.R220fsX34) (fig 3 and 4). Typical “dot and halo” lesions were observed in patient B (p.D145fsX30) (fig 2). The central dot and halo lesions in the left eye gradually developed into a butterfly‐shaped pattern dystrophy of the macula (fig 2). None of the patients in this study developed subretinal neovascularisation. Four patients (probands C, D, E and G) demonstrated pigmentary changes in the peripheral retina. All four patients suffered from a variable degree of night blindness. Typical retinitis pigmentosa characteristics were observed only in proband D.
On fluorescein angiography, the flecks were hyperfluorescent in the early and late phase of the examination, sometimes with a central hypofluorescent spot. None of the patients displayed a so‐called dark choroid on fluorescein angiography. On fundus AF imaging, the flecks showed a highly increased AF, often with small adjacent zones of decreased AF (figs 2 and 3). Lesions that were yellowish and seemed to contain a lipofuscin‐like substance on ophthalmoscopy mostly corresponded with an increased AF signal. On OCT, some of the STGD1‐like flecks appeared as a highly reflective focal thickening of the hyper‐reflective outer red line (ORL).37 Macular lesions showed thickening of the ORL, with a variable increase in underlying reflectivity.
Full‐field ERG results varied from normal to non‐recordable (table 1). The photopic ERG was abnormal to non‐recordable in all patients with confluence of the yellowish flecks. The EOG also varied largely from normal to an absent light rise and was abnormal in 11 of 20 eyes. Humphrey 10‐2 SITA‐Fast analysis of the central 10° of the visual field showed normal to near‐normal results in 4 cases (probands A, B, C and E), while probands D, F and G displayed a severely decreased sensitivity in both eyes. Proband I showed a decrease in sensitivity at the inferior and temporal edges of the central visual field of both eyes. Goldmann perimetry was normal only in proband F, whereas the other patients showed a mild‐to‐marked constriction of the peripheral visual field.
Twenty family members, in whom the same mutation as in the proband was found, were examined (table 2). Nine of these individuals experienced visual disturbances. The genetically affected family members of probands C, D, H, G and I all showed the phenotype of multifocal pattern dystrophy, except for patient C‐IV:1, who was 34 years of age. Other phenotypes were observed in families B, E, F and J, although these individuals carried the same mutation as the proband with multifocal pattern dystrophy. Three family members showed no retinal abnormalities despite carrying a pathologic peripherin/RDS mutation.
Discussion
The phenotype of the multifocal pattern dystrophy described in this report is caused by autosomal dominant inheritance of mutations in the peripherin/RDS gene, with variable expressivity and a reduced penetrance. The type and distribution of the flecks in this pattern dystrophy strongly resembled the flecks observed in the fundus flavimaculatus phenotype of STGD1, an autosomal recessive retinal dystrophy caused by mutations in the ABCA4 gene.41 This resemblance was evident on ophthalmoscopy as well as on AF and OCT.42,43,44,45,46
All probands demonstrated a variable number of irregularly shaped yellow–white flecks scattered throughout the posterior pole and around the retinal vascular arcades. These yellowish flecks were preceded either by typical macular pattern dystrophy or by non‐specific pigmentary changes in the fovea. The lesions were best defined by AF imaging. Discrete retinal abnormalities were also easily identified with this technique in several asymptomatic family members carrying the same peripherin/RDS mutation as the proband. Extensive atrophy of the central retina tends to occur with increasing age as demonstrated by the four probands who were over 60 years of age. The fact that multifocal pattern dystrophy, like many other “macular” dystrophies, may involve the peripheral retina is demonstrated by the abnormal photopic and scotopic ERGs in almost half of the probands and an abnormal EOG in the majority of the probands.
Of the nine different mutations that were identified, there were five different frameshift mutations and one nonsense mutation, which led to a premature termination by a stop codon. This may lead to either a shorter protein product or it may induce degradation of the mRNA by nonsense‐mediated decay. The mechanism of pathogenicity of the mutation may be haploinsufficiency in case of the frameshift mutations, the nonsense mutation and the splice site mutation. In case of the two missense mutations that were found, a dominant negative effect may also be possible, although there is plausible evidence that these mutations may also lead to haploinsufficiency.47,48 The frameshift mutation p.P147fsX4 has been previously described in patients with central areolar choroidal dystrophy.39 This p.P147fsX4 mutation was found in two unrelated probands, patients D and E. Both patients had multifocal pattern dystrophy, but in patient D the phenotype progressed to a panretinal dystrophy resembling retinitis pigmentosa, with widespread involvement of the rod and cone system. The missense mutation p.D157N has been reported previously in patients with pattern dystrophy,38 while the p.P210R missense mutation was found in patients with adult‐onset foveomacular vitelliform dystrophy.27,40
In our study, a genotype–phenotype correlation could not be established. The present study again demonstrates the highly divergent phenotypes in family members who carry identical peripherin/RDS mutations. The retinal abnormalities range from minor foveal abnormalities to multifocal pattern dystrophy and even retinitis pigmentosa. This remarkable clinical heterogeneity precludes a straightforward genotype–phenotype correlation even with larger patient series.5,8,10,12,16,18,20,29,49 Obviously, modifying factors besides the specific mutation in the peripherin/RDS gene exert an important influence on the resulting phenotype.
Zhang et al. reported the histopathological findings in a patient with butterfly‐shaped pattern dystrophy with Stargardt‐like flecks caused by a p.C213Y substitution in peripherin/RDS.8,21 Adjacent to a central area of atrophy, the RPE cells were greatly distended by lipofuscin. This is in accordance with the predominantly increased AF signal of the lesions described in the present study. The same accumulation of lipofuscin in RPE cells has been demonstrated for STGD1.50,51,52 It is likely that the lipofuscin accumulation in multifocal pattern dystrophy is less pronounced in view of the better visual prognosis as well as the absence of choroidal blockage on the fluorescein angiogram. The small adjacent zones with a decreased AF signal, which were seen in association with the majority of flecks, are probably caused by RPE atrophy. This is reflected in the predominant hyperfluorescence of the flecks on the fluorescein angiogram. As the disease progresses, the flecks tend to evolve towards a confluent atrophic area which shows larger zones of decreased AF intensity. The multifocal nature of this pattern dystrophy may be explained by local differences in cell interactions, distribution, morphology and metabolism.53
Autosomal dominant multifocal pattern dystrophy should not be confused with autosomal recessive STGD1 and infrequent autosomal dominant retinal disorders such as STGD3 (ELOVL4 gene) and STGD4.54,55,56 Clinical findings that may help to distinguish this pattern dystrophy from STGD1 are the autosomal dominant pattern of inheritance, the relatively late age of onset (fifth decade), the comparatively good and stable visual acuity and the absence of a “dark choroid”. However, the incomplete penetrance (10% in this study) and the variable expression may mask the dominant inheritance pattern. Conversely, due to the high carrier frequency of ABCA4 mutations, STGD1 patients may have relatives with some form of retinal dystrophy.57 Three of the probands in this study received the proper diagnosis only after analysis of the peripherin/RDS gene in a group of 15 patients with presumed STGD1, but without detectable mutations in the ABCA4 gene. Therefore, an analysis of the peripherin/RDS gene should be considered in the absence of ABCA4 mutations, especially when confronted with the aforementioned phenotype.
Acknowledgements
The authors thank the patients and their families for their participation. They also thank Liesbeth Hoeks for the technical assistance.
Abbreviations
EOG - electro‐oculography
ERG - electroretinography
OCT - optical coherence tomography
ORL - outer red line
RPE - retinal pigment epithelium
STGD1 - Stargardt disease
Footnotes
Competing interests: None.
References
- 1.Fishman G A. Inherited macular dystrophies: a clinical overview. Aust N Z J Ophthalmol 199018123–128. [DOI] [PubMed] [Google Scholar]
- 2.Gass J D.Stereoscopic atlas of macular diseases: diagnosis and treatment. Volume 1. 4th edn. St Louis: CV Mosby, 1997314–325.
- 3.Marmor M F, Byers B. Pattern dystrophy of the pigment epithelium. Am J Ophthalmol 19778432–44. [DOI] [PubMed] [Google Scholar]
- 4.Watzke R C, Folk J C, Lang R M. Pattern dystrophy of the retinal pigment epithelium. Ophthalmology 1982891400–1406. [DOI] [PubMed] [Google Scholar]
- 5.Francis P J, Schultz D W, Gregory A M.et al Genetic and phenotypic heterogeneity in pattern dystrophy. Br J Ophthalmol 2005891115–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marmor M F, McNamara J A. Pattern dystrophy of the retinal pigment epithelium and geographic atrophy of the macula. Am J Ophthalmol 1996122382–392. [DOI] [PubMed] [Google Scholar]
- 7.Yang Z, Li Y, Jiang L.et al A novel RDS/peripherin gene mutation associated with diverse macular phenotypes. Ophthalmic Genet 200425133–145. [DOI] [PubMed] [Google Scholar]
- 8.Zhang K, Garibaldi D C, Li Y.et al Butterfly‐shaped pattern dystrophy: a genetic, clinical, and histopathological report. Arch Ophthalmol 2002120485–490. [DOI] [PubMed] [Google Scholar]
- 9.Prensky J G, Bresnick G H. Butterfly‐shaped macular dystrophy in four generations. Arch Ophthalmol 19831011198–1203. [DOI] [PubMed] [Google Scholar]
- 10.Gorin M B, Jackson K E, Ferrell R E.et al A peripherin/retinal degeneration slow mutation (Pro‐210‐Arg) associated with macular and peripheral retinal degeneration. Ophthalmology 1995102246–255. [DOI] [PubMed] [Google Scholar]
- 11.Richards S C, Creel D J. Pattern dystrophy and retinitis pigmentosa caused by a peripherin/RDS mutation. Retina 19951568–72. [DOI] [PubMed] [Google Scholar]
- 12.Apfelstedt‐Sylla E, Theischen M, Ruther K.et al Extensive intrafamilial and interfamilial phenotypic variation among patients with autosomal dominant retinal dystrophy and mutations in the human RDS/peripherin gene. Br J Ophthalmol 19957928–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ayazi S, Fagan R. Pattern dystrophy of the pigment epithelium. Retina 19811287–289. [DOI] [PubMed] [Google Scholar]
- 14.de Jong P T, Delleman J W. Pigment epithelial pattern dystrophy. Four different manifestations in a family. Arch Ophthalmol 19821001416–1421. [DOI] [PubMed] [Google Scholar]
- 15.Giuffre G. Autosomal dominant pattern dystrophy of the retinal pigment epithelium. Intrafamilial variability. Retina 19888169–173. [DOI] [PubMed] [Google Scholar]
- 16.Grover S, Fishman G A, Stone E M. Atypical presentation of pattern dystrophy in two families with peripherin/RDS mutations. Ophthalmology 20021091110–1117. [DOI] [PubMed] [Google Scholar]
- 17.Hsieh R C, Fine B S, Lyons J S. Patterned dystrophies of the retinal pigment epithelium. Arch Ophthalmol 197795429–435. [DOI] [PubMed] [Google Scholar]
- 18.Khoubian F J, Shakin E P, Tantri A.et al Autosomal dominant pattern dystrophy: identification of a novel splice site mutation in the peripherin/RDS gene. Retina 200525999–1004. [DOI] [PubMed] [Google Scholar]
- 19.Puech B, Hache J C, Turut P.et al X‐shaped macular dystrophy with flavimaculatus flecks. Ophthalmologica 1989199146–157. [DOI] [PubMed] [Google Scholar]
- 20.Sears J E, Aaberg Sr T A, Daiger S P.et al Splice site mutation in the peripherin/RDS gene associated with pattern dystrophy of the retina. Am J Ophthalmol 2001132693–699. [DOI] [PubMed] [Google Scholar]
- 21.Singerman L J, Berkow J W, Patz A. Dominant slowly progressive macular dystrophy. Am J Ophthalmol 197783680–693. [DOI] [PubMed] [Google Scholar]
- 22.Thomann U, Buchi E R, Suppiger M.et al Age‐dependent phenotypic expression of a pattern dystrophy of the retina. Eur J Ophthalmol 19955107–112. [DOI] [PubMed] [Google Scholar]
- 23.van Lith‐Verhoeven J J, Cremers F P, van den Helm B.et al Genetic heterogeneity of butterfly‐shaped pigment dystrophy of the fovea. Mol Vis 20039138–143. [PubMed] [Google Scholar]
- 24.Giuffre G, Lodato G. Vitelliform dystrophy and pattern dystrophy of the retinal pigment epithelium: concomitant presence in a family. Br J Ophthalmol 198670526–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Keen T J, Inglehearn C F. Mutations and polymorphisms in the human peripherin‐RDS gene and their involvement in inherited retinal degeneration. Hum Mutat 19968297–303. [DOI] [PubMed] [Google Scholar]
- 26.Kohl S, Christ‐Adler M, Apfelstedt‐Sylla E.et al RDS/peripherin gene mutations are frequent causes of central retinal dystrophies. J Med Genet 199734620–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sohocki M M, Daiger S P, Bowne S J.et al Prevalence of mutations causing retinitis pigmentosa and other inherited retinopathies. Hum Mutat 20011742–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weigell‐Weber M, Kryenbuhl C, Buchi E R.et al Genetic heterogeneity in autosomal dominant pattern dystrophy of the retina. Mol Vis 199626. [PubMed] [Google Scholar]
- 29.Weleber R G, Carr R E, Murphey W H.et al Phenotypic variation including retinitis pigmentosa, pattern dystrophy, and fundus flavimaculatus in a single family with a deletion of codon 153 or 154 of the peripherin/RDS gene. Arch Ophthalmol 19931111531–1542. [DOI] [PubMed] [Google Scholar]
- 30.Boesze‐Battaglia K, Goldberg A F. Photoreceptor renewal: a role for peripherin/rds. Int Rev Cytol 2002217183–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Farjo R, Naash M I. The role of Rds in outer segment morphogenesis and human retinal disease. Ophthalmic Genet 200627117–122. [DOI] [PubMed] [Google Scholar]
- 32.Goldberg A F. Role of peripherin/rds in vertebrate photoreceptor architecture and inherited retinal degenerations. Int Rev Cytol 2006253131–175. [DOI] [PubMed] [Google Scholar]
- 33.Miller S A, Dykes D D, Polesky H F. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res 1988161215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Holz F G, Bellman C, Staudt S.et al Fundus autofluorescence and development of geographic atrophy in age‐related macular degeneration. Invest Ophthalmol Vis Sci 2001421051–1056. [PubMed] [Google Scholar]
- 35.Thijssen J M, Pinckers A, Otto A J. A multipurpose optical system for ophthalmic electrodiagnosis. Ophthalmologica 1974168308–314. [DOI] [PubMed] [Google Scholar]
- 36.Reese M G, Eeckman F H, Kulp D.et al Improved splice site detection in Genie. J Comput Biol 19974311–323. [DOI] [PubMed] [Google Scholar]
- 37.Ghazi N G, Dibernardo C, Ying H S.et al Optical coherence tomography of enucleated human eye specimens with histological correlation: origin of the outer “red line”. Am J Ophthalmol 2006141719–726. [DOI] [PubMed] [Google Scholar]
- 38.Jacobson S G, Cideciyan A V, Maguire A M.et al Preferential rod and cone photoreceptor abnormalities in heterozygotes with point mutations in the RDS gene. Exp Eye Res 199663603–608. [DOI] [PubMed] [Google Scholar]
- 39.Trujillo M J, Bueno J, Osorio A.et al Three novel RDS‐peripherin mutations (689delT, 857del17, G208D) in Spanish families affected with autosomal dominant retinal degenerations. Mutations in brief no. 147. Online. Hum Mutat 19981270. [DOI] [PubMed] [Google Scholar]
- 40.Feist R M, White M F, Jr, Skalka H.et al Choroidal neovascularization in a patient with adult foveomacular dystrophy and a mutation in the retinal degeneration slow gene (Pro 210 Arg). Am J Ophthalmol 1994118259–260. [DOI] [PubMed] [Google Scholar]
- 41.Allikmets R. A photoreceptor cell‐specific ATP‐binding transporter gene (ABCR) is mutated in recessive Stargardt macular dystrophy. Nat Genet 199717122. [DOI] [PubMed] [Google Scholar]
- 42.Fishman G A, Stone E M, Grover S.et al Variation of clinical expression in patients with Stargardt dystrophy and sequence variations in the ABCR gene. Arch Ophthalmol 1999117504–510. [DOI] [PubMed] [Google Scholar]
- 43.Lois N, Holder G E, Fitzke F W.et al Intrafamilial variation of phenotype in Stargardt macular dystrophy‐Fundus flavimaculatus. Invest Ophthalmol Vis Sci 1999402668–2675. [PubMed] [Google Scholar]
- 44.Lois N, Holder G E, Bunce C.et al Phenotypic subtypes of Stargardt macular dystrophy‐fundus flavimaculatus. Arch Ophthalmol 2001119359–369. [DOI] [PubMed] [Google Scholar]
- 45.Lois N, Halfyard A S, Bird A C.et al Fundus autofluorescence in Stargardt macular dystrophy‐fundus flavimaculatus. Am J Ophthalmol 200413855–63. [DOI] [PubMed] [Google Scholar]
- 46.Querques G, Leveziel N, Benhamou N.et al Analysis of retinal flecks in fundus flavimaculatus using optical coherence tomography. Br J Ophthalmol 2006901157–1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stricker H M, Ding X Q, Quiambao A.et al The Cys214→Ser mutation in peripherin/rds causes a loss‐of‐function phenotype in transgenic mice. Biochem J 2005388605–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ding X Q, Nour M, Ritter L M.et al The R172W mutation in peripherin/rds causes a cone‐rod dystrophy in transgenic mice. Hum Mol Genet 2004132075–2087. [DOI] [PubMed] [Google Scholar]
- 49.van Lith‐Verhoeven J J, van den Helm B, Deutman A F.et al A peculiar autosomal dominant macular dystrophy caused by an asparagine deletion at codon 169 in the peripherin/RDS gene. Arch Ophthalmol 20031211452–1457. [DOI] [PubMed] [Google Scholar]
- 50.Birnbach C D, Jarvelainen M, Possin D E.et al Histopathology and immunocytochemistry of the neurosensory retina in fundus flavimaculatus. Ophthalmology 19941011211–1219. [DOI] [PubMed] [Google Scholar]
- 51.Eagle R C, Jr, Lucier A C, Bernardino V B., Jret al Retinal pigment epithelial abnormalities in fundus flavimaculatus: a light and electron microscopic study. Ophthalmology 1980871189–1200. [DOI] [PubMed] [Google Scholar]
- 52.Steinmetz R L, Garner A, Maguire J I.et al Histopathology of incipient fundus flavimaculatus. Ophthalmology 199198953–956. [DOI] [PubMed] [Google Scholar]
- 53.Besch D, Jagle H, Scholl H P.et al Inherited multifocal RPE‐diseases: mechanisms for local dysfunction in global retinoid cycle gene defects. Vision Res 2003433095–3108. [DOI] [PubMed] [Google Scholar]
- 54.Bernstein P S, Tammur J, Singh N.et al Diverse macular dystrophy phenotype caused by a novel complex mutation in the ELOVL4 gene. Invest Ophthalmol Vis Sci 2001423331–3336. [PubMed] [Google Scholar]
- 55.Edwards A O, Miedziak A, Vrabec T.et al Autosomal dominant Stargardt‐like macular dystrophy: I. Clinical characterization, longitudinal follow‐up, and evidence for a common ancestry in families linked to chromosome 6q14. Am J Ophthalmol 1999127426–435. [DOI] [PubMed] [Google Scholar]
- 56.Kniazeva M, Chiang M F, Morgan B.et al A new locus for autosomal dominant stargardt‐like disease maps to chromosome 4. Am J Hum Genet 1999641394–1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Klevering B J, Maugeri A, Wagner A.et al Three families displaying the combination of Stargardt's disease with cone‐rod dystrophy or retinitis pigmentosa. Ophthalmology 2004111546–553. [DOI] [PubMed] [Google Scholar]