Abstract
Aims
To study the incidence, systemic associations, presenting features and natural history of Purtscher's retinopathy in the UK and Ireland.
Methods
Cases were collected prospectively by active surveillance through the British Ophthalmological Surveillance Unit. Clinical details were obtained using an incident questionnaire, with follow‐up at 1 and 6 months.
Results
Clinical details were obtained for 15 cases over 12 months. These were associated with road traffic accidents in 6 cases, chest compression in 6 cases and acute pancreatitis in 3 cases. All cases were symptomatic and presented with loss of visual acuity, visual field or a combination. Bilateral involvement was noted in 9 cases. The acute retinal signs of cotton wool spots, retinal haemorrhage and Purtscher flecken cleared within 1 month in 26% of eyes and within 6 months in all eyes. The most common chronic signs were optic disc pallor and atrophy of the retinal pigment epithelium. Without treatment, 50% of eyes improved by at least 2 Snellen lines at final follow‐up and 23% improved by at least 4 Snellen lines. Only 1 of the 24 eyes had a final acuity worse than that recorded at presentation.
Conclusion
Purtscher's retinopathy is a rare but sight‐threatening eye condition, most commonly seen in young or middle‐aged men and after trauma. Spontaneous visual recovery of at least 2 Snellen lines is seen in half of the cases.
Purtscher's retinopathy was first described in 1910 by Otmar Purtscher, in a patient with severe head trauma.1 Since then, a similar retinal appearance has also been described in a variety of conditions including acute pancreatitis, crush injury, long bone fracture, orthopaedic surgery and childbirth.2,3,4,5 The main aims of this study were to determine the incidence, systemic associations, clinical features and natural history of Purtscher's retinopathy.
Method
In a prospective observational study, cases presenting with Purtscher's retinopathy between April 2004 and March 2005 were determined through the British Ophthalmic Surveillance Unit (BOSU) active reporting scheme.6,7 Following notification of a new case to BOSU, the respondents were sent the first of two questionnaires to collect initial data at presentation and follow‐up data at 1 month. A second questionnaire was then sent to collect data at 6 months from the time of presentation. Non‐responders received subsequent reminders, up to a maximum of three.
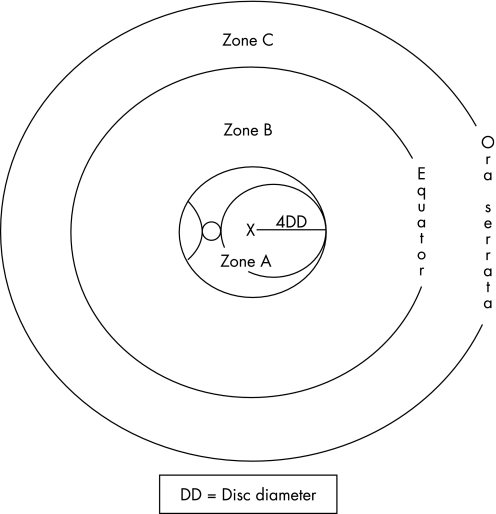
A broad case definition was used to avoid under‐reporting (table 1). In this study the term Purtscher's retinopathy was used for all cases, regardless of the cause. The extent of the retinal involvement was identified using the diagram shown in fig 1.8,9,10
Table 1 Case definition (in varying combination).
| (1) An associated contributing illness such as acute pancreatitis, long bone fracture, orthopaedic surgery, chest compression or crush injury |
| (2) Multiple areas of polygonal retinal whitening between the retinal arterioles and venules (Purtscher flecken) and/or superficial cotton wool spots in one or both eyes |
| • typically restricted to the posterior pole |
| • accompanied by minimal, if any, retinal haemorrhage |
| • no visible emboli in the large retinal vessels |
| • no direct ocular trauma |
Figure 1 Retinal zones.
In order to estimate visual recovery in a meaningful way, this was expressed as either a 2 or 4 Snellen line improvement. In this method, a 2‐line Snellen improvement would be equal to a halving of the visual angle or a 3‐line Early Treatment of Diabetic Retinopathy Study (ETDRS) change and considered to be clinically significant. Analysis of visual acuity change during the 6‐month follow‐up was performed for the whole group and then according to the cause and the duration of the acute retinal signs. Given the different methods of recording acuity data used by the participating ophthalmologists, acuities of less than 6/120, including counting fingers and hand movements, were included in a single acuity group. A change of acuity from 6/6 to 6/5 was assumed to be equal to one ETDRS line.
Statistical analysis was performed using SPSS for windows software, version 14.0. Analysis of categorical data was performed using Χ2 and Fisher's exact test, while for continuous variables the Mann–Whitney U test and Kruskal–Wallis test were employed.
The study was approved by the South West Multi‐centre Research Ethics Committee.
Results
Over a 1‐year period, a total of 23 cases were notified through BOSU and 1 case was excluded having been notified by two different ophthalmologists. Of the remaining 22 cases, data could be collected for 17 cases, of which 2 cases did not meet the inclusion criteria and were excluded. For the remaining 15 cases, data at presentation were obtained for all cases, at 1 month for 14 cases and at 6 months for 11 cases. None of the patients had a history of prior Purtscher's retinopathy, nor did any have further episodes during the 6‐month follow‐up.
The mean age of the 15 cases was 42 years (range 25–76 years) and 10 subjects were men. Mean follow‐up was 4.5 months (range 1–8 months). Trauma was the most common precipitant. Road traffic accidents (RTA) contributed to 6 cases, of which 4 also had long bone fractures. Chest compression not involving RTA contributed to another 6 cases. Acute pancreatitis was the precipitant in the remaining 3 cases (table 2).
Table 2 Patient characteristics.
| Case | Age | Sex | Precipitating injury | Eye | Presenting features | Initial acuity | Final acuity |
|---|---|---|---|---|---|---|---|
| 1 | 36 | F | Acute pancreatitis | Right | PF, CWS, RH | CF | CF |
| Left | PF, CWS | CF | CF | ||||
| 2 | 38 | F | Acute pancreatitis | Right | PF, CWS, RH | CF | 6/60 |
| Left | PF, CWS, RH | CF | CF | ||||
| 3 | 31 | M | Acute pancreatitis | Right | PF, CWS, RH | 6/18 | 6/6 |
| Left | PF, CWS, RH | HM | CF | ||||
| 4 | 30 | M | Chest compression | Right | RH | 6/5 | 6/5 |
| Left | RH | 6/6 | 6/5 | ||||
| 5 | 50 | M | Chest compression | Right | CWS, RH | 6/60 | 6/6 |
| Left | CWS, RH | 2/60 | 6/6 | ||||
| 6 | 48 | M | Chest compression | Right | CWS, RH | 6/12 | 6/6 |
| Left | CWS, RH | 6/12 | 6/6 | ||||
| 7 | 37 | M | Chest compression | Right | PF, CWS, RH | HM | HM |
| Left | CWS, RH | 6/5 | 6/6 | ||||
| 8 | 76 | F | Chest compression | Right | PF, CWS, RH | HM | 6/6 |
| Left | — | — | — | ||||
| 9 | 25 | M | Chest compression | Right | PF, CWS, RH | 6/60 | 6/60 |
| Left | — | — | — | ||||
| 10 | 67 | F | RTA + long bone fracture | Right | CWS | 6/9P | 6/9 |
| Left | CWS | 6/9P | 6/6 | ||||
| 11 | 38 | M | RTA + long bone fracture | Right | CWS, RH | 6/36 | 6/18 |
| Left | — | — | — | ||||
| 12 | 44 | F | RTA + long bone fracture | Right | PF, CWS, RH | 6/18 | 6/5 |
| Left | — | — | — | ||||
| 13 | 44 | M | RTA + long bone fracture | Right | PF, CWS, RH | 6/9 | 6/9 |
| Left | — | — | — | ||||
| 14 | 32 | M | Road traffic accident | Right | CWS, RH | HM | 6/5 |
| Left | CWS, RH | HM | 6/5 | ||||
| 15 | 37 | M | Road traffic accident | Right | — | — | — |
| Left | CWS, RH | HM | 6/60 |
CF, count fingers; CWS, cotton wool spot; HM, hand movements; P, part; PF, Purtscher flecken; RH, retinal haemorrhage; RTA, road traffic accident.
Clinical features
All the cases were symptomatic, with 33% reporting loss of acuity alone, 60% reporting loss of both acuity and visual field and 7% reporting loss of visual field only. None described positive visual phenomena. Thirteen of the 15 cases reported visual symptoms within a day of the initial injury.
Nine cases had bilateral involvement and, of the six cases with unilateral involvement, the right eye was involved in four cases. Bilateral involvement was seen in all the cases precipitated by acute pancreatitis, compared to 67% and 33% of the cases precipitated by chest compression and RTA, respectively. Signs were mainly noted in the posterior pole and involved zone A alone in 67% of eyes, zone B alone in 13% and a combination of zones A and B in 20%. No cases had signs in zone C. There was no apparent difference in the extent of retinal involvement between unilateral and bilateral cases.
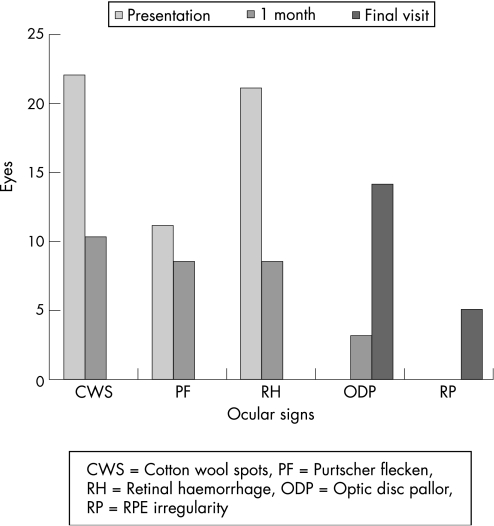
Acute retinal signs included Purtscher flecken in 11 eyes, cotton wool spots in 22 eyes and retinal haemorrhage in 21 eyes. These acute signs had resolved completely within a month of the initial injury in 6 of the 23 eyes for which 1‐month follow‐up data were available and were not present in any eye, 6 months after the initial presentation. The acute changes were replaced by optic disc pallor in 14 eyes and this was first noted after 1 month in 3 eyes. Irregularity of the central, retinal pigment epithelium was noted in 5 eyes but never before the 6‐month examination (fig 2).
Figure 2 Natural history of the ocular signs.
Visual outcome
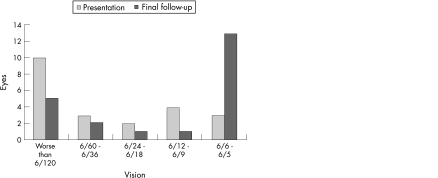
At presentation, 13 of the 24 eyes (54%) had a visual acuity of 6/60 or worse and 8 eyes (33%) had an acuity of 6/12 or better. There was no significant difference in the presenting acuity between the three systemic associations of acute pancreatitis, RTA and chest compression (p = 0.27, Kruskal–Wallis test).
No treatment for the visual symptoms was given in 13 cases. Two patients with unilateral Purtscher's retinopathy after RTA (cases 13 and 15) were treated with intravenous methyl prednisolone within 3 days of presentation. Although follow‐up was incomplete at 2 and 1 months, respectively, the single affected eye of case 15 had an acuity improvement equivalent to more than 2 Snellen lines.
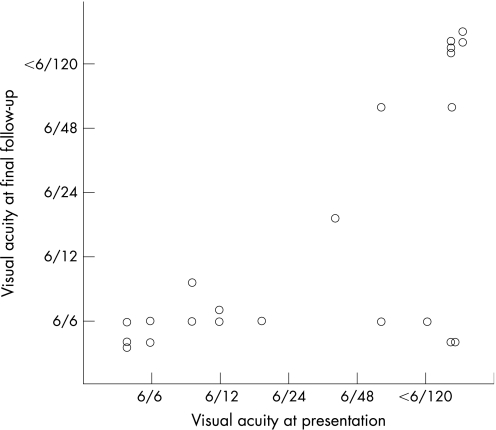
For the 13 cases with no specific treatment for the visual symptoms, an acuity improvement of at least 2 Snellen lines was seen in 11 of the 22 eyes and of at least 4 Snellen lines was seen in 5 of the 22 eyes (figs 3 and 4). The mean improvement in this group was 2.7 (SD 3.6) Snellen lines. There was no significant difference in the number of lines of acuity improvement between the three systemic associations (p = 0.41, Kruskal–Wallis test). The final acuity was worse than at presentation in a single eye of one individual, although the change from 6/5 to 6/6 may not be meaningful.
Figure 3 Visual acuity at presentation and final follow‐up for the affected eyes (n = 22) of the cases not receiving systemic steroids.
Figure 4 Scatter plot of visual acuity at presentation and final follow‐up for the affected eyes (n = 22) of the cases not receiving systemic steroids.
Excluding the two cases with unilateral involvement who had intravenous methyl prednisolone and the single case without 1‐month follow‐up data, acute changes were still present at the 1‐month examination in 15 eyes (group A) but were absent in 6 eyes (group B). Group A eyes had a worse acuity at presentation than group B eyes and this was statistically significant (p = 0.002, Mann–Whitney U test). There was a mean of 3.6 Snellen lines of improvement in group A compared to 1.0 lines of improvement in group B (p = 0.3, Mann–Whitney U test). In group A, an acuity improvement of at least 2 Snellen lines was seen in 9 eyes (60%) and 4 Snellen lines in 5 eyes (33.3%). In contrast, in group B, an acuity improvement of at least 2 Snellen lines was seen in 2 eyes (33.3%) and 4 Snellen lines in 0 eyes.
The final visual acuity was better in group B although the difference was not statistically significant (p = 0.18, Mann–Whitney U test). Of the 15 eyes in group A, 6 eyes (40%) had a final acuity of 6/60 or worse. In contrast, of the 6 eyes in group B, the final acuity was 6/60 or worse in 0 eyes (p = 0.12, Fisher exact test). These data suggest that there may be a non‐significant trend for the earlier resolution of the acute changes to be associated with a better initial and final visual outcome.
Discussion
Over a 1‐year period, data were collected for 15 cases. Based on the UK population of 58.8 million (2001 census) and the Republic of Ireland population of 3.9 million (2002 census), the annual incidence of symptomatic Purtscher's retinopathy from this study is estimated to be 0.24 cases per million population per year. However, this probably represents a minimum incidence as five possible additional cases were notified to us but the notifying ophthalmologist was unable to supply data and it is possible that other cases may not have presented to ophthalmology departments. Furthermore, there may be a degree of under‐reporting in any surveillance scheme, although the response rate from participating ophthalmologists in the BOSU scheme has been consistently more than 70%.11 However, it is still possible to conclude that symptomatic Purtscher's retinopathy is rare, seen most often in young men and as a consequence of trauma. The true incidence can only be ascertained by a prospective review of cases with the known systemic associations and this was not the intention of this study.
In this series, all the cases presented with loss of visual acuity, visual field or both and none described positive visual phenomena. The majority of the cases had bilateral involvement, although 40% had unilateral involvement and this has been reported before.12,13,14,15 The most common acute signs finding were cotton wool spots and retinal haemorrhage. The pathognomonic Purtscher flecken were recognised in only 50% of cases. These polygonal areas of retinal whitening occur in the inner retina, between retinal arterioles and venules and have a characteristic clear zone, without retinal whitening, extending for an average of 50 μm on either side of the retinal arteries and pre‐capillary arterioles.16 Cotton wool spots were seen in 92% and retinal haemorrhage was seen in 83% of cases. The late finding of atrophy of the retinal pigment epithelium, and possibly also the optic disc pallor, may provide further evidence of the involvement of the choroidal vasculature in the acute phase.17,18
Isolated case reports suggest that treatment of Purtscher's retinopathy with high‐dose, intravenous steroids may be beneficial.19,20 Only two patients in this series received intravenous methylprednisolone and, of the 2 eyes, 1 improved by at least 2 Snellen lines and none by 4 lines. In comparison, a significant visual recovery of at least 2 and 4 Snellen lines was seen in 50% and 23% of eyes without treatment. Other published case series have also reported similar results, with improvement in the visual function seen without any specific treatment in the majority of patients.4,12,21 Although we cannot be certain that some of the cases in this BOSU series were not given steroids as part of the treatment for the systemic association and this was not recognised or initiated by the notifying ophthalmologist, current guidance relating to the management of the systemic associations would suggest that this is unlikely.22,23 Given the frequency of spontaneous recovery, it is also difficult to draw conclusions from other small, non‐randomised case reports suggesting a possible benefit from systemic steroids and hyperbaric oxygen therapy.19,20,24 A potential weakness of our data is the need to include all levels of acuity below 6/120 into a single group. However, we were not able to ascertain if notifying units routinely recorded acuities below 6/60 at a distance of less than 6 m before testing for finger counting and hand movements. The method described was a pragmatic solution to this problem and may overestimate or underestimate visual recovery for an initial acuity of either counting fingers or hand movements. A trend towards a worse visual outcome was also seen in the eyes in which acute changes were still present 1 month after the initial presentation. The group A eyes had worse initial and final acuity than the group B eyes in which the acute changes resolved within 1 month. This trend has been noted previously.25
In conclusion, Purtscher's retinopathy is rare and most often seen after trauma. The acute retinal signs include Purtscher flecken, cotton wool spots and retinal haemorrhage and often persist for at least 1 month after the initial injury. Spontaneous visual recovery of at least 2 Snellen lines is seen in half of the cases. There is some evidence that poor initial and final acuities may be associated with persistent acute changes in the retina.
Acknowledgements
The authors are very grateful for the opportunity to perform this project in conjunction with the British Ophthalmological Surveillance Unit and wish to thank Mr Barny Foot for his valuable advice. The authors also acknowledge the contribution of the ophthalmologists throughout the UK who made this study possible by reporting cases to BOSU and providing the necessary information about the patients.
Abbreviations
BOSU - British Ophthalmic Surveillance Unit
ETDRS - Early Treatment of Diabetic Retinopathy Study
RTA - road traffic accidents
Footnotes
Funding: The study was jointly funded by the British Ophthalmological Surveillance Unit and Yorkshire Eye Research.
Competing interests: None.
References
- 1.Purtscher O. Noch unbekannte befunde nach schadeltrauma. Ber Dtsch Ophthalmol Ges 191036294–301. [Google Scholar]
- 2.Agrawal A, McKibbin M A. Purtscher's and Purtscher‐like retinopathies: a review. Surv Ophthalmol 200651129–136. [DOI] [PubMed] [Google Scholar]
- 3.Jacob H S, Goldstein I M, Shapiro I.et al Sudden blindness in acute pancreatitis, possible role of complement‐induced retinal leukoembolization. Arch Intern Med 1981141134–136. [PubMed] [Google Scholar]
- 4.Blodi B A, Johnson M W, Gass D M. Purtscher's‐like retinopathy after childbirth. Ophthalmology 1990901654–1659. [DOI] [PubMed] [Google Scholar]
- 5.Chuang E L, Miller F S, Kalina R E. Retinal lesions following long bone fractures. Ophthalmology 198592370–374. [DOI] [PubMed] [Google Scholar]
- 6.Foot B, Stanford M, Rahi J.et al The British Ophthalmological Surveillance Unit: an evaluation of the first 3 years. Eye 2003179–15. [DOI] [PubMed] [Google Scholar]
- 7.Ling R, Cole M, James C.et al Suprachoroidal haemorrhage complicating cataract surgery in the UK: epidemiology, clinical features, management, and outcomes. Br J Ophthalmol 200488478–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dollery C T, Henkind P, Paterson J W.et al Ophthalmoscopic and circulatory changes in focal retinal ischemia. Br J Ophthalmol 196650285–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wise G N, Dollery C T, Henhind P.The retinal circulation. New York: Harper & Row, 1971
- 10.Henkind P. Radial peripapillary capillaries of the retina. Br J Ophthalmol 196751115–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stanford M. British Ophthalmological Surveillance Unit Steering Committee. Five years of surveillance. Br J Ophthalmol 200286838–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burton T C. Unilateral Purtscher's retinopathy. Ophthalmology 1980871096–1105. [DOI] [PubMed] [Google Scholar]
- 13.Lemagne J M, Michiels X, Van Causenbroeck S.et al Purtscher‐like retinopathy after retrobulbar anesthesia. Ophthalmology 199097859–861. [DOI] [PubMed] [Google Scholar]
- 14.Wilkinson W S, Morgan C M, Baruh E.et al Retinal and choroidal vascular occlusion secondary to corticosteroid embolization. Br J Ophthalmol 19897332–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kocak N, Kaynak S, Kaynak T.et al Unilateral Purtscher‐like retinopathy after weight lifting. Eur J Ophthalmol 200313395–397. [DOI] [PubMed] [Google Scholar]
- 16.Michaelson I C, Campbell A C P. The anatomy of the finer retinal vessels. Trans Ophthal Soc UK 19406071–111. [Google Scholar]
- 17.Haq F, Vajaranant T S, Szlyk J P.et al Sequential multifocal electroretinogram findings in a case of Purtscher‐like retinopathy. Am J Ophthalmol 2002134125–128. [DOI] [PubMed] [Google Scholar]
- 18.Gomez‐Ulla F, Fente B, Torreiro M G.et al Choroidal vascular abnormality in Purtscher's retinopathy shown by indocyanine green angiography. Am J Ophthalmol 1996122261–263. [DOI] [PubMed] [Google Scholar]
- 19.Wang A G, Yen M Y, Liu J H. Pathogenesis and neuroprotective treatment in Purtscher's retinopathy. Jpn J Ophthalmol 198842318–322. [DOI] [PubMed] [Google Scholar]
- 20.Atabay C, Kansu T, Nurlu G. Late visual recovery after intravenous methyl prednisolone treatment of Purtscher's retinopathy. Ann Ophthalmol 199325330–333. [PubMed] [Google Scholar]
- 21.Schmidt D, Otto T. Prognose und Differenzialdiagnose des Morbus Purtscher. Ophthalmologe 2004101576–583. [DOI] [PubMed] [Google Scholar]
- 22.UK Working Party on Acute Pancreatitis UK guidelines for the management of acute pancreatitis. Gut 200554(Suppl 3)1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Klein Y, Cohn S M, Proctor K G. Lung contusion: pathophysiology and management. Curr Opin Anaesthesiol 20021565–68. [DOI] [PubMed] [Google Scholar]
- 24.Lin Y C, Yang C M, Lin C L. Hyperbaric oxygen treatment in Purtscher's retinopathy induced by chest injury. J Chin Med Assoc 200669444–448. [DOI] [PubMed] [Google Scholar]
- 25.Holak H M, Holak N H, Schenk C.et al Correlation of retinal thickness with the extent of Purtscher's retinopathy. Ophthalmologe 2006103798–805. [DOI] [PubMed] [Google Scholar]