Melanocytoma, a benign uveal melanocytic tumour, represents only 3% of iris naevi, and seldom undergoes malignant transformation.1,2 We report an unusual case of an iris melanocytoma suggested by two separate biopsies, which evolved into ring melanoma of the iris.
Case report
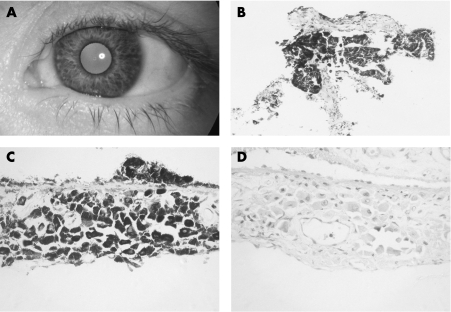
A 33‐year‐old Caucasian female, with a family history of open‐angle glaucoma, presented with ‘darkening of the left eye' since the age of 16 years, left hemicranial headache for 18 months and reduced vision in the left eye for 2 days. Visual acuity was 6/9 with a left relative afferent pupillary defect. There was left heterochromia iridis, with patchy iris hyperpigmentation (fig 1A), that was flat except for one inferonasal area. Intraocular pressure (IOP) was 50 mm Hg. Gonioscopy revealed the drainage angle to be hyperpigmented. The optic disc had a cup:disc ratio of 0.9 with a disc haemorrhage. Visual field tests (Humphrey 24‐2) confirmed an obliterated field. All findings in the right eye were normal.
Figure 1 A: Anterior segment photograph of the left eye on presentation in 1995, showing dark, mainly flat patches of pigmentation. B: Initial biopsy specimen of inferonasal iris, showing a small iris fragment with large melanocytic cells on both sides of the iris (haematoxylin‐eosin ×200). C: Iridectomy specimen showing well‐orientated iris with large, densely pigmented, well‐separated cells involving the stroma (haematoxylin‐eosin ×400). D: Bleached section (×400) showing the morphology of the epithelioid cells in greater detail. Although most cells contain small nuclei, occasional cells show larger nuclei within which single nucleoli are present.
Biopsy of the inferonasal iris tumour (fig 1B) showed large, densely pigmented epithelioid cells diffusely infiltrating the iris tissue. The cells were separated from each other, without a spindle‐cell appearance. Bleached sections showed large cells, a few of which contained small nucleoli. The findings were reported as iris naevus, which is consistent with melanocytoma. A trabeculectomy with mitomicin C was subsequently required to normalise IOP. The surgical iridectomy from this yielded another specimen, with better orientation of the iris tissue. Large polygonal heavily pigmented cells (fig 1C) were noted within the iris tissue, with occasional anteriorly located fine vessels that were indicative of rubeosis iridis. There was no evidence of proliferation in Ki67 immunostained sections. Bleached sections (fig 1D) showed large epithelioid cells with relatively small nuclei and generally indistinct nucleoli. The histological diagnosis was again thought to be most in keeping with melanocytoma. Post‐operatively, the IOP was in the normal range and the patient was lost to follow‐up.
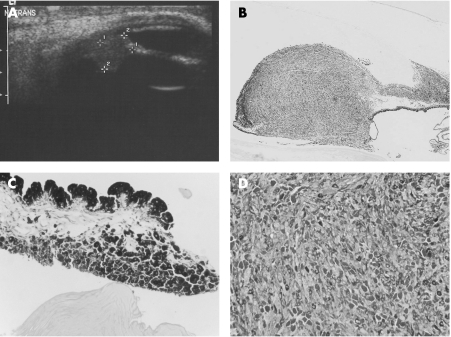
Five years later, the patient presented with a left IOP of 50 mm Hg again and advanced pigmentary changes. There were two new raised pigmented areas in the inferotemporal iris, with pigment seeding into the bleb and subconjunctival infiltration of pigment. Anterior segment ultrasound (fig 2A) confirmed two raised areas on the iris and ciliary body, one elevated 4.4 mm (nasally) and the other 6.2 mm (temporally). Gonioscopy revealed a pigmented mass in the iris periphery and iridocorneal angle. Metastatic evaluation was negative and the patient underwent enucleation.
Figure 2 A: Anterior segment B mode ultrasound showing one of the two iris masses. This nasal tumour was elevated by 4.4 mm. B: The tumour is seen infiltrating the iris and iridocorneal angle of the enucleated globe under low power (haematoxylin‐eosin ×20). C: The iris has melanocytic cells on the posterior surface as well as a thickened sheet‐like proliferation on the anterior surface (haematoxylin‐eosin ×200). D: High‐power photomicrograph of the centre of the tumour, showing mixed epithelioid and spindle cell types (bleach ×200).
Histology of the enucleated globe (fig 2B‐D) showed an iris ring melanoma of mixed cell type with both epithelioid and spindle cells. Over the iris, there was a plaque‐like extension of cells, which were both larger and more pigmented than those infiltrating the ciliary body and forming the bulk of the tumour. These larger cells were similar to those seen in the initial iris biopsies, probably representing residual melanocytoma. The trabeculectomy bleb contained pigmented macrophages and extrascleral extension was absent. Review of the second iris biopsy does show occasional larger nuclei within the epithelioid cells, although with copious cytoplasm, and it should be noted that the subsequent melanoma is composed mainly of spindle cells, with a different appearance.
Comment
We present a case of documented transition from a lesion showing the features of iris melanocytoma to ring melanoma. Two separate biopsies were thought to contain only benign melanocytoma cells and the enucleated eye contained residual melanocytoma‐like cells, so it is conceivable that de‐differentiation to melanoma had occurred over time, or that the initial samples had missed a deeper small ciliary‐body lesion. Malignant transition from melanocytoma of the optic disc,3,4 choroid,5,6 ciliary body7 and meninges8 has been described, but malignant transformation of iris melanocytoma was not found in one series at 5 years.1 However, Cialdini et al.2 reported a discrete, rather than ring configuration, iris tumour that contained malignant and melanocytoma cells.
Ring melanoma of the iris or ciliary body (involving at least 6 clock hours) is a rare and often misdiagnosed cause of unilateral pigmentary glaucoma.9,10 Acquired heterochromia was noticed by our patient 17 years before presentation and, subsequently, ring melanoma was diagnosed after another 7 years. Although the possibility of sampling error exists in the original biopsy, this time course argues against a misdiagnosis on two separate histological specimens. We therefore believe that malignant transition from iris melanocytoma to ring melanoma can occur and that careful long‐term observation of iris melanocytomas is warranted.
Footnotes
Conflicting interests: None
References
- 1.Demirci H, Mashayekhi A, Shields C L.et al Iris melanocytoma: clinical features and natural course in 47 cases. Am J Ophthalmol 2005139468–475. [DOI] [PubMed] [Google Scholar]
- 2.Cialdini A P, Sahel J A, Jalkh A E.et al Malignant transformation of an iris melanocytoma. A case report. Graefes Arch Clin Exp Ophthalmol 1989227348–354. [DOI] [PubMed] [Google Scholar]
- 3.Apple D J, Craythorn J M, Reidy J J.et al Malignant transformation of an optic nerve melanocytoma. Can J Ophthalmol 198419320–325. [PubMed] [Google Scholar]
- 4.Meyer D, Ge J, Blinder K J.et al Malignant transformation of an optic disk melanocytoma. Am J Ophthalmol 1999127710–714. [DOI] [PubMed] [Google Scholar]
- 5.Barker‐Griffith A E, McDonald P R, Green W R. Malignant melanoma arising in a choroidal magnacellular nevus (melanocytoma). Can J Ophthalmol 197611140–146. [PubMed] [Google Scholar]
- 6.Leidenix M, Mamalis N, Goodart R.et al Malignant transformation of a necrotic melanocytoma of the choroid in an amblyopic eye. Ann Ophthalmol 19942642–46. [PubMed] [Google Scholar]
- 7.Heitman K F, Kincaid M C, Steahly L. Diffuse malignant change in a ciliochoroidal melanocytoma in a patient of mixed racial background. Retina 1988867–72. [DOI] [PubMed] [Google Scholar]
- 8.Uozumi Y, Kawano T, Kawaguchi T.et al Malignant transformation of meningeal melanocytoma: a case report. Brain Tumor Pathol 20032021–25. [DOI] [PubMed] [Google Scholar]
- 9.Manschot W A. Ring Melanoma. Arch Ophthalmol 196471625–632. [DOI] [PubMed] [Google Scholar]
- 10.Lee V, Cree I A, Hungerford J L. Ring melanoma—a rare cause of refractory glaucoma. Br J Ophthalmol 199983194–198. [DOI] [PMC free article] [PubMed] [Google Scholar]