Abstract
Aim
To evaluate symptoms in patients with functional (FNLDO) and primary acquired (PANDO) nasolacrimal duct obstruction, evaluated prospectively before and after successful dacryocystorhinostomy (DCR) surgery.
Design
A questionnaire delivered by interview, pre‐ and postintervention.
Methods
Consecutive patients with either FNLDO or PANDO were derived from a tertiary referral clinic and private practice of two surgeons (GW and ICF). The preoperative cohort consisted of 33 FNLDO patients and 28 PANDO patients. Of these, only 31 patients elected to proceed to DCR surgery. There were 12 FLNDO patients and 19 PANDO patients in the postoperative cohorts, all with definitive surgical success. Successful DCR surgery was indicated by positive endoscopic Jones 1 testing. Symptoms in relation to the patient's vision, reading, driving, mood, work and embarrassment were assessed. The severity of these symptoms was also graded.
Results
Vision and reading in particular were affected in both preoperative cohorts, and patients suffered significantly from embarrassment. Of the postoperative cohorts, the FNLDO cohort had a reduced percentage of patients suffering each symptom type, whereas the PANDO group had a reduction in percentage of patients reporting each symptom in some but not all areas. However, the overall severity was reduced in both groups, and embarrassment was significantly reduced in both groups.
Conclusion
In both FNLDO and PANDO populations, symptoms bother patients significantly, and successful DCR surgery has a positive effect on the patient's physical and psychological well‐being.
Nasolacrimal duct obstruction (NLDO) is a disorder in which the symptomatology and objective findings do not always correlate. Patients frequently report symptoms of visual blur, difficulty reading, driving, embarrassment and poor mood due to both functional (FNLDO) and primary acquired (PANDO) nasolacrimal duct obstruction. We have observed that objective surgical success does not necessarily correlate with symptom improvement. Sahlin and Rose similarly found that objective surgical success in FNLDO did not necessarily correlate with symptomatic success.1
In our study, following Jones' definition, FNLDO was defined as a positive fluorescein dye disappearance test (FDDT),a negative Jones 1 and a positive Jones 2 test, with normal lid apposition, no ocular surface disease and a normal sac washout. We have chosen this terminology as inferred from Jones' original article2 and a 1994 American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS) survey.3 Jones alludes to a FNLDO, without calling it that, as being a “partial” obstruction in the nasolacrimal duct. It is characterised by demonstrating a negative Jones 1 and a positive Jones 2 test, albeit at the time determined by cotton wool pledget staining rather than by intranasal endoscopy.2 In the 1994 ASOPRS survey,3 the term “functional” was first used in reference to patients symptomatic of tearing with no obvious mechanical obstruction indicated by normal syringing at a time when the approach to such watery eyes was ill‐defined. PANDO was defined as both Jones 1 and 2 tests negative, in the presence of a sac washout with total reflux from the lower to upper canaliculus.
In PANDO, an objective finding of complete blockage may not necessarily correlate with more severe symptoms than those of a patient with an FNLDO and an incomplete blockage. Thus, to understand how much these disorders are bothering our patients, we aimed to assess watery eye symptomatology between the two cohorts.
Dacryocystorhinostimy (DCR) surgery for FNLDO or PANDO has had objective, anatomical measures of success, as defined by an endoscopically confirmed positive Jones test.4 However, the effect of anatomically successful DCR surgery on patients' symptoms has often been limited to the severity of tearing. We felt that an evaluation of a broader range of watery eye symptoms was necessary to address the issue of whether patients had actually improved in real life terms following objectively successful surgery. Thus, we were interested to see how much successful DCR surgery, as measured by positive Jones 1 testing, altered symptomatology in each of the cohorts, that is objective versus subjective success.
The therapeutic index of an intervention represents the ratio of the desired effects as the numerator, to the unwanted effects of an intervention as the denominator.5 Fortunately, with DCR surgery, the ratio is quite high, but there are nevertheless significant risks with this surgery.6 Thus, it is important to know if this intervention leads to subjectively “successful” outcomes as defined by an improvement in patient symptomatology. This will aid patients in their decision‐making, regarding DCR surgery, by assessing their own therapeutic index.
Methods
Patients were selected prospectively and consecutively from both private practice and tertiary referral hospital clinics of two surgeons (GW and ICF). The study was approved by the Human Research Ethics Committee of the University of New South Wales. A questionnaire was delivered in person by a single interviewer (ICF) to all participants. The questionnaire assessed symptomatology as related to their NLDO, and included the following data (table 1). The patient was asked whether their watery eye affected the following: vision, reading, driving, mood and work. The overall severity of this symptomatology was graded as not at all (0), mild (grade 1), moderate (grade 2) or severe (grade 3). The final question was related to the patient's embarrassment, and whether it affected the patient, again, not at all (grade 0), or to a mild (grade 1), moderate (grade 2) or severe (grade 3) degree.
Table 1 Patient questionnaire.
| Does your watery‐eye problem bother you? | Y | N | |
| If it does bother you, does it interfere with your: | Sight? | Y | N |
| Reading? | Y | N | |
| Driving? | Y | N | |
| Mood? | Y | N | |
| Work? | Y | N | |
| If it does interfere, is it: (choose one) | A little? (mild) | ||
| A moderate amount? | |||
| A great deal? (severe) | |||
| Does your watery eye become embarrassing? | Y | N | |
| If it does become embarrassing, is it: (choose one) | A little? (mild) | ||
| A moderate amount? | |||
| A great deal? (severe) |
After informed consent was obtained, patients were offered DCR surgery by either an endoscopic or external approach. Endoscopic surgery was performed under a general anaesthetic, whereas external surgery was performed under a local anaesthetic with sedation. Both techniques involved the mechanical formation of a bony ostium, apposition of sac mucosa to nasal mucosa, and intubation with silicone tubes for 3–4 weeks. Wormald's technique was followed for the endoscopic surgery.4 Objective surgical success was defined as positive endoscopic Jones 1 testing at the 1‐month review, and was achieved in all patients.
Postoperatively, at a minimum of 2 months, patients were delivered the same questionnaire in person by the same interviewer to reassess their responses. This cohort formed the postoperative cohort for assessment of symptoms in patients following successful DCR surgery for both FNLDO and PANDO.
The frequency of symptom reporting was compared between PANDO and FNLDO cases using proportions tests. For this exploratory analysis of individual symptoms, the α‐value was set at 0.1 and was adjusted for multiple comparisons. The adjusted p value for statistical significance was set at 0.02.
An unweighted symptom score was derived for each case, based on the report for each symptom type (vision, reading, driving, mood, embarrassment). The effect of surgery on symptom score was determined using a Wilcoxon paired test for both groups of cases. Symptom score was compared between FNLDO and PANDO using a Mann–Whitney test. The p value for statistical significance was set at p<0.05.
The effect of surgery on frequency of individual symptom reporting was determined for both groups of cases using McNemar paired tests. For this exploratory analysis of individual symptoms, the α‐value was set at 0.1 and was adjusted for multiple comparisons. The adjusted p value for statistical significance was set at 0.02.
The effect of surgery on the report of any symptom and subjective rating of disease severity and embarrassment was determined using a Wilcoxon paired test with a p value for statistical significance set at p<0.05.
Results
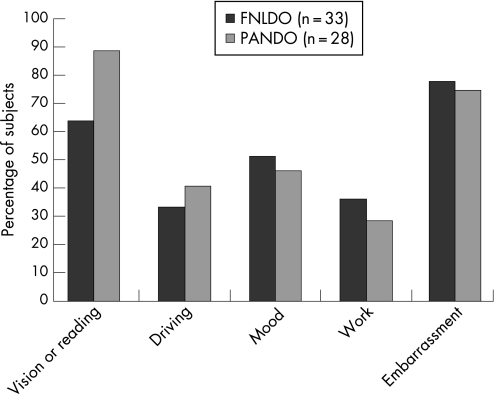
The average age of the PANDO cohort was similar to the FNLDO cohort at 65 and 64 years, respectively. The frequency of symptom reporting is shown in fig 1. Difficulties with vision or reading were slightly but not statistically significantly more frequently reported by PANDO cases (89%) compared with FNLDO cases (64%, p = 0.049). There were no significant differences between the groups in the report of difficulties with driving, mood, work or embarrassment due to watery eye. Overall symptom report scores were not significantly different between FNLDO (3.06 (SD 2.05)) and PANDO (3.39 (1.62)).
Figure 1 Symptom reporting in watery eye.
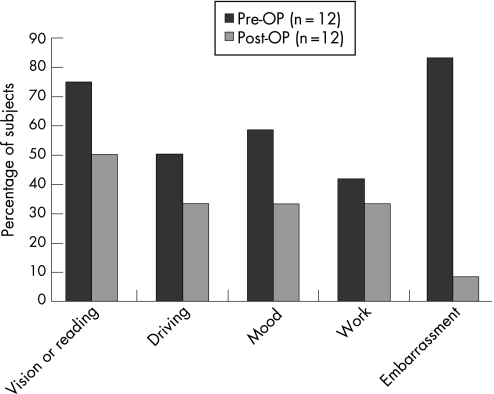
Overall symptom report scores were significantly reduced following successful DCR surgery in FNLDO patients. The mean preoperative symptom score was 3.50 (SD 2.07) and postoperative 2.00 (1.65) (p<0.05). The frequency of individual symptom reporting is shown in fig 2. While fewer subjects reported postoperative symptoms, embarrassment was the only individual symptom to reduce significantly (in frequency) following surgery (p<0.005). Fewer patients reported visual problems after surgery (50% vs 75%); however, individual comparisons did not reach statistical significance.
Figure 2 Effect of DCR surgery on symptom reporting in FNLDO cases.
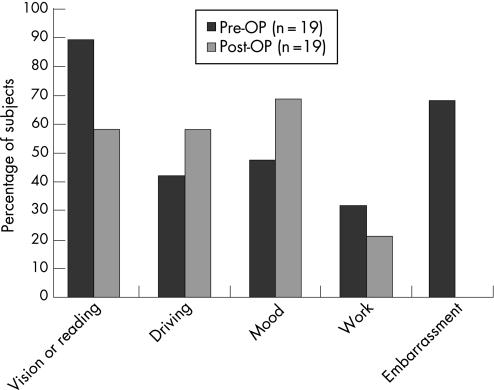
Overall symptom report scores were unchanged following DCR surgery in PANDO patients. The mean preoperative symptom score was 3.21 (SD 1.69) and postoperatively 2.74 (1.91) (p = 0.15). The frequency of individual symptom reporting is shown in fig 3. DCR surgery in PANDO patients significantly improved symptoms of embarrassment (p<0.001), and there was a small but not statistically significant reduction in the frequency of visual symptoms (89% vs 58%, p = 0.065). Six subjects reported their mood worsening after surgery. There was no association between mood reporting and the number of weeks taken for recovery.
Figure 3 Effect of DCR surgery on symptom reporting in PANDO cases.
Perceived (symptom) severity and embarrassment due to watery eye was significantly reduced by surgery for both patient groups (p<0.005, table 2). Perceived (symptom) severity was not affected by the type of disease.
Table 2 Effect of DCR surgery on perceived embarrassment and disease severity in FNLDO and PANDO.
| Disease severity (0 to 3) | Embarrassment (0 to 3) | |||
|---|---|---|---|---|
| Preoperative* | Postoperative | Preoperative | Postoperative | |
| FNLDO (n = 12) | 2 (0 to 3) | 0 (0 to 1) | 1 (0 to 3) | 0 (0) |
| PANDO (n = 19) | 2 (0 to 3) | 0 (0) | 1 (0 to 3) | 0 (0) |
*Median (range).
Discussion
Our study has shown both FNLDO and PANDO affect patients in relation to visual tasks, driving, mood and work, as well as causing embarrassment to these patients. Predictably, difficulties with visual tasks were most often reported, likely due to the visual distortion induced by the raised tear meniscus of NLDO particularly in down‐gaze.7 The percentage of patients affected by embarrassment due to their watery eye was over 65% of respondents in both cohorts, quite a significant finding.
The frequency of symptom reporting (reflected in the average symptom report scores) and the overall severity of the symptoms were not significantly different between the two groups. Thus, it appears that an FNLDO causes a similar severity of symptomatology to a PANDO, which seems counterintuitive given that PANDO is a complete obstruction. This may be because of the negative feedback in tear production occurring with obstructed lacrimal drainage in comparison with a relatively more positive feedback in FNLDO.8
In the FNLDO group, there was a non‐significant reduction in the frequency of all symptoms, but a significant reduction in the severity of the overall symptoms and embarrassment. Thus, we can tell our patients with FNLDO that, following successful surgery, their symptoms will improve, at least in severity, and that their embarrassment will improve significantly.
The results for the PANDO postoperative cohort were surprising in part. There was an increase in percentage of patients affected for mood and driving compared with the preoperative cohort, although not significantly. We were unable to identify the reason for this. A possible consideration is the way in which the diagnosis of a complete obstruction influences surgical counselling and expectations as compared with a functional obstruction. Potentially higher expectations from surgery in the PANDO group may have contributed to the increased percentage of patients reporting mood disturbance postoperatively. However, the success of surgery for FNLDO is very high, as exemplified in the study by O'Donnell et al.9
Despite the partly surprising result of an increase in the frequency of some symptoms, the overall severity of symptoms was significantly reduced following surgery, and no patient in the PANDO cohort suffered embarrassment postoperatively.
Many studies have assessed patient satisfaction or resolution of tearing but have not assessed a broader range of symptoms related to watery eye, and have not distinguished FNLDO from PANDO. Mathew et al described “patient satisfaction” in a retrospective study and telephone questionnaire comparing non‐laser endoscopic DCR and external DCR, and found no significant difference between the two for patient satisfaction (75% vs 86%, respectively).10 Tarbet and Custer found that 87% of patients had resolution of symptoms (tearing or dacryocystitis) following external DCR, and all patients would recommend the procedure.11 Moore et al evaluated mechanical and laser endoscopic DCR in 62 patients with PANDO including subjective reporting of tearing as an outcome measure.12 There was a 71% and 83% subjective success rate, respectively, but again, tearing alone was measured. Interestingly, only 69% of patients were endoscopic Jones 1 positive, that is, there was less objective success than subjective success. Mansour et al found that, in 139 patients with PANDO who had external DCR, the subjective success rate based on a retrospective symptom score was 89% after 1 year.13 Bakri et al compared quality of life (QOL) outcomes following either external or endonasal laser DCR using the Glasgow Benefit Inventory (GBI).14 The GBI is a global assessment of social interaction and QOL designed to be used following otolaryngological procedures. The study showed a “significant benefit in their healthcare status”. It did not compare FNLDO and PANDO, and did not assess activities related to watery eye.
Tripathi et al assessed the success of laser endonasal endoscopic DCR using both subjective (questionnaire) and objective (sac washout) measures.15 The questionnaire asked to what degree the watering was cured, with 65% of patients declaring a complete cure, compared with 91% of patients with objective success.
In our study, we concentrated on the presence or absence of a wide range of symptoms related to watery eye. Further strengths of our paper are that it was prospective and consecutive, and that the interviews were done by the same examiner, thus limiting observer bias. Unfortunately, the examiner was not masked to the underlying diagnosis of the patient.
Successful DCR surgery improves all individual symptoms assessed in patients with FNLDO, but not all symptoms in PANDO. We know that patient satisfaction is related to preoperative expectations which are set by the surgeon. Modifying these expectations on the basis of our results may improve patient satisfaction postoperatively.
Abbreviations
DCR - dacryocystorhinostomy
FDDT - fluorescein dye disappearance test
FNLDO - functional nasolacrimal duct obstruction
NLDO - nasolacrimal duct obstruction
PANDO - primary acquired nasolacrimal duct obstruction
Footnotes
Competing interests: None declared.
Presented in part at the British and European OculoPlastics Surgery Society Meeting, London, September 2006.
References
- 1.Sahlin S, Rose G E. Lacrimal drainage capacity and symptomatic improvement after dacrocystorhinostomy in adults presenting with patent lacrimal drainage systems. Orbit 200120173–179. [DOI] [PubMed] [Google Scholar]
- 2.Jones L T, Linn M L. The diagnosis of the causes of epiphora. Am J Ophthalmol 196967751–754. [Google Scholar]
- 3.Conway S T. Evaluation and management of “functional” nasolacrimal blockage: results of a survey of the American Society of Ophthalmic Plastic and Reconstructive Surgery. Ophthal Plast Reconstr Surg 199410185–188. [PubMed] [Google Scholar]
- 4.Tsirbas A, Wormald P J. Mechanical endonasal dacryocystorhinostomy with mucosal flaps. Br J Ophthalmol 20038743–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zimmerman T J. Cost of beta‐blocker therapy. Arch Ophthalmol 1997115914. [DOI] [PubMed] [Google Scholar]
- 6.Brown M M, Brown G C. Value based medicine. Br J Ophthalmol 200488979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Francis I C, Chan D, Papalkar D G.et al Videoreflective dacryomeniscometry in normal adults and in patients with functional or primary acquired nasolacrimal duct obstruction. Am J Ophthalmol 2005139493–497. [DOI] [PubMed] [Google Scholar]
- 8.Stahl U, Francis I C, Stapleton F. Prospective controlled study of vapor pressure tear osmolality and tear meniscus height in nasolacrimal duct obstruction. Am J Ophthalmol 20061411051–1056. [DOI] [PubMed] [Google Scholar]
- 9.O'Donnell B, Shah R. Dacryocystorhinostomy for epiphora in the presence of a patent lacrimal system. Clin Exp Ophthalmol 20012927–29. [DOI] [PubMed] [Google Scholar]
- 10.Mathew M R, McGuiness R, Webb L A.et al Patient satisfaction in our initial experience with endonasal endoscopic non‐laser dacryocystorhinostomy. Orbit 20042377–85. [DOI] [PubMed] [Google Scholar]
- 11.Tarbet K J, Custer P L. External dacryocystorhinostomy. Surgical success, patient satisfaction, and economic cost. Ophthalmology 19951021065–1070. [DOI] [PubMed] [Google Scholar]
- 12.Moore W M H, Bentley C R, Olver J M. Functional and anatomic results after two types of endoscopic endonasal dacryocystorhinostomy: surgical and holmium laser. Ophthalmology 20021091575–1582. [DOI] [PubMed] [Google Scholar]
- 13.Mansour K, Sere M, Oey A G.et al Long‐term patient satisfaction of external dacryocystorhinostomy. Ophthalmologica 200521997–100. [DOI] [PubMed] [Google Scholar]
- 14.Bakri S J, Carney A S, Robinson K.et al Quality of life outcomes following dacryocystorhinostomy: external and endonasal laser techniques compared. Orbit 19991883–88. [DOI] [PubMed] [Google Scholar]
- 15.Tripathi A, Lesse T H J, O'Donnel N P.et al Local anaesthetic endonasal endoscopic laser dacryocystorhinostomy:analysis of patients' acceptaibility and various factors affecting the success of this procedure. Eye 200216146–149. [DOI] [PubMed] [Google Scholar]