This prospective, open‐label, non‐comparative, interventional case series evaluates the results of photodynamic therapy (PDT) in juxtafoveal and extrafoveal choroidal neovascularization (CNV) secondary to pathologic myopia in 27 eyes of 27 patients.
The average visual acuity dropped from 58.5 letters to 49.19. The visual acuity remained stable in 13 patients (48.1%), whereas 14 patients (51.9%) lost more than 8 letters due to the extension of the lesion to subfoveal space. A strong association was found between advanced age and a worse visual prognosis (p = 0.001).
PDT may stabilise visual acuity in young patients with non‐subfoveal CNV secondary to pathologic myopia.
The long‐term visual prognosis of myopic CNV is poor;1 however, favourable prognostic factors such as young age, good initial visual acuity and the extrafoveal location of the lesion have been described.2
The present study aims to analyse the results of PDT in juxtafoveal and extrafoveal CNV secondary to pathologic myopia.
Case report
The study included 27 eyes of 27 patients (21 women and 6 men), with non‐subfoveal CNV secondary to pathologic myopia, with a follow‐up period of 1 year.
The mean best corrected visual acuity (BCVA; see table 1) dropped nine letters.
Table 1 Demographics and initial and final CNV characteristics.
| Mean (SD) | Range | |
|---|---|---|
| Age (years) | 56.41 (12.33) | 38–73 |
| Initial VA (letters) | 58.56 (10.79) | 37–76 |
| Final VA (letters) | 49.19 (19.90) | 12–78 |
| Initial GLD (microns) | 1210.78 (396.88) | 650–2425 |
| Final GLD (microns) | 1706.15 (847.90) | 310–3800 |
| Initial distance to fovea (microns) | 387.05 (225.40) | 102–975 |
| Final distance to fovea (microns) | 194.93 (284.26) | 0–1080 |
| No. of treatments | 2..11 (0.75) | 1–3 |
VA, visual acuity; GLD, greatest linear dimension
PDT has stabilised the BCVA in 13 patients (48.1%). In 14 patients (51.9%), a visual loss of more than 8 letters was found.
A highly significant correlation exists between the change in visual acuity and the patients' age (p<0.001 , <0.05), the diminution of visual acuity being more probable in older patients.
An increase in the average size of the lesion was observed and the distance of the lesion from the fovea was reduced. Involvement of the fovea was observed in 15 patients (55%) after a 1‐year follow‐up. A total of 93% of these patients showed a visual loss of more than 8 letters.
No statistically significant relationship was found between the change in visual acuity and the initial size (p = 0.212) or the initial distance to fovea (p = 0.626).
Patients with poorer visual acuity were treated more times (2.43 vs 1.77).
Comment
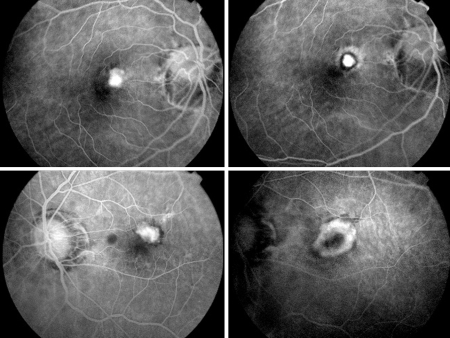
A strong statistical relationship was found between the patients' age and the visual prognosis. Patients who did not experience a moderate or severe visual loss (fig 1A and 1B) were younger (average age: 47.5 years), did not have extension of the lesion towards the fovea and needed less treatment sessions.
Figure 1 (top left) Case 1, a 37‐year‐old female before treatment; BCVA, 62 letters. (top right) Case 1, after 1 year and one PDT treatment; closure of CNV; BCVA, 74 letters. (bottom left) Case 2, a 73‐year‐old female before treatment; BCVA, 60 letters. (bottom right) Case 2, after 1 year and three PDT treatments; enlargement of CNV; BCVA, 42 letters.
On the contrary, patients with moderate or severe visual loss (fig 1C and 1D) were older (average age: 64.6 years), had extension of the lesion towards the fovea and required more treatment sessions.
These findings are similar to those found in the series evaluating PDT in subfoveal CNV secondary to myopia, in which an elderly age is associated with a worse visual prognosis.3 In comparison with the study carried out by Lam et al.,4 the higher average age in our study can explain why these authors have better results.
In conclusion, PDT may stabilise the visual acuity in non‐subfoveal CNV secondary to myopia. However, in a high percentage of elderly patients, this does not prevent the progression of the lesion towards the centre of the fovea, with a significant visual loss. Our study has several limitations; future studies are required.
Footnotes
Competing interests: None declared
References
- 1.Ohno‐Matsui K, Yoshida T. Myopic choroidal neovascularization: natural course and treatment. Curr Opin Ophthalmol 200415197–202. [DOI] [PubMed] [Google Scholar]
- 2.Hayashi K, Ohno‐Matsui K, Yoshida T.et al Characteristics of patients with a fovorable natural course of myopic choroidal neovascularization. Graefes Arch Clin Exp Ophthalmol 200524313–19. [DOI] [PubMed] [Google Scholar]
- 3.Axer‐Siegel R, Ehrlich R, Weinberger D.et al Photodynamic therapy of subfoveal choroidal neovascularization in high myopia in a clinical setting: visual outcome in relation to age at treatment. Am J Ophthalmol 2004138602–607. [DOI] [PubMed] [Google Scholar]
- 4.Lam D S, Liu D T, Fan D S.et al Photodynamic therapy with verteporfin for juxtafoveal choroidal neovascularization secondary to pathologic myopia: 1 year results of a prospective series. Eye 200519834–840. [DOI] [PubMed] [Google Scholar]