Abstract
Aims
To describe the long‐term risk of bullous keratopathy following argon laser iridotomy (ALI) in Japan and to compare it with other centres in the world.
Methods
We retrospectively reviewed the case records of all patients with ALI‐induced bullous keratopathy that underwent penetrating keratoplasty at Kyoto Prefectural University of Medicine (KPUM) from January 2001 to December 2004. The results were compared with the other representative centres in Singapore and the UK.
Results
Thirty‐nine eyes of 33 patients were included in the study. The mean age of patients was 73.3±6.9 years (range, 58 to 87 years). Patients developed bullous keratopathy at a mean duration of 6.9±4.9 years (range, 0.2 to 16 years) after the laser iridotomy procedure. The majority of eyes that developed bullous keratopathy (59.0%) occurred following prophylactic ALI. KPUM had the highest percentage of ALI‐induced bullous keratopathy cases that underwent penetrating keratoplasties, as compared with other centres in Singapore and the UK (20.0%, 1.8% and 0%, respectively).
Conclusion
Bullous keratopathy may arise many years following ALI, and is a growing problem in Asian countries. This condition is a major cause of ocular morbidity in Japan, which has seen a worrying increase in the number of cases in recent years.
Argon laser iridotomy (ALI) is a well‐established procedure for the treatment and prevention of angle‐closure glaucoma.1,2 This procedure has largely replaced surgical iridectomy as the treatment of choice because it is a non‐invasive procedure that can be performed easily in the clinic, without the attendant risks associated with incisional invasive surgery. Long‐term studies have demonstrated the relative safety of this procedure, with the absence of significant sight‐threatening complications.1,2 Corneal complications during or immediately following ALI include corneal opacities and oedema, epithelial and endothelial burns.1,2,3,4 The long‐term significance of these complications is uncertain, with human and animal studies demonstrating variable results.3,5,6
Despite the apparent safety of the procedure, several authors have described the development of corneal decompensation following ALI.4,7,8 Some predisposing risk factors that have been identified include a history of repeated intraocular pressure elevations, anterior segment inflammation, pre‐existing corneal guttate, diabetes mellitus and higher levels of laser energy used to create a patent iridotomy.4,7,8 Reports of this complication have primarily been restricted to isolated case series, with small patient numbers. As such, ALI is generally regarded as being extremely safe, with minimal long‐term sequelae.
The aims of our study were to evaluate the potential long‐term risk of bullous keratopathy following ALI, as well as to highlight the worrying increase in incidence of this condition, particularly in Japan. The results of our centre were compared with those from other representative centres in Asia and the UK. Singapore was selected as the comparison Asian country, as it has a unique multiethnic population of Chinese, Malay and Indian inhabitants, and it has the highest incidence of acute primary angle closure glaucoma of any country studied to date.9 Previous studies conducted in Singapore demonstrated that the majority of patients afflicted with acute angle closure glaucoma were Chinese (84–90%), while Malays (6–9%) and Indians (approximately 5%) formed the minority.9,10,11 The centre in Nottingham (UK) was selected for comparison because of its predominantly Caucasian patient population.
Methods
The case records of all patients that underwent penetrating keratoplasty from January 2001 to December 2004 at Kyoto Prefectural University of Medicine (KPUM) were retrospectively reviewed. The demographic data, preoperative recipient diagnosis, physical findings and ophthalmic examination were recorded. These results were compared with the clinical audit results for penetrating keratoplasty at the Singapore National Eye Centre (SNEC), Singapore, and Nottingham Queen's Medical Centre (NQMC), UK.
Results
From 2001 to 2004, a total of 39 eyes of 33 consecutive patients with ALI‐induced bullous keratopathy that underwent penetrating keratoplasty were included in the study. The mean age of patients was 73.3±6.9 years (range, 58–87 years). There were 8 males and 25 females.
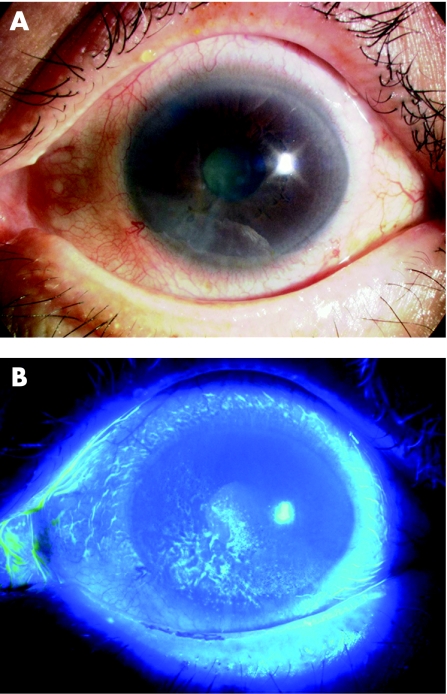
At our centre, 41.0% (16/39) of eyes with bullous keratopathy occurred in the attack eye, while 59.0% (23/39) occurred following prophylactic laser iridotomy to the fellow eye. Most patients presented with generalised corneal oedema, while some eyes were noted to have inferior corneal oedema (fig 1) that later progressed to become generalised. Patients developed bullous keratopathy at a mean duration of 6.9±4.9 years (range, 0.2 to 16 years) after the laser iridotomy procedure. Eight patients (24.2%) had pre‐existing Fuchs' endothelial dystrophy or corneal guttate.
Figure 1 (A) Anterior segment photograph of an eye with early ALI‐induced bullous keratopathy, with corneal oedema present in the inferior segment of the cornea. (B) Fluorescein staining demonstrating an irregular staining pattern over the localised area of oedema.
The proportion of patients with ALI‐induced bullous keratopathy as an indication for penetrating keratoplasty in the 3 centres is shown in table 1. Over the 4 years, KPUM saw the highest percentage of ALI‐induced bullous keratopathy cases (20.0%) that underwent penetrating keratoplasties. This far exceeded the situation in the Singapore and UK institutes over a corresponding time period, where the proportions of cases with the condition were 1.8% and 0%, respectively.
Table 1 Incidence of ALI‐induced bullous keratopathy (ALI‐BK) as a primary indication for penetrating keratoplasty (PKP) in 3 centres from 2001 to 2004.
| Institution | 2001 | 2002 | 2003 | 2004 | ||||
|---|---|---|---|---|---|---|---|---|
| Total PKPs | No. of ALI‐BK cases (%) | Total PKPs | No. of ALI‐BK cases (%) | Total PKPs | No. of ALI‐BK cases (%) | Total PKPs | No. of ALI‐BK cases (%) | |
| KPUM, Japan | 48 | 9 (18.8) | 45 | 10 (22.2) | 54 | 10 (18.5) | 48 | 10 (20.8) |
| SNEC, Singapore | 121 | 1 (0.8) | 145 | 1 (0.7) | 123 | 6 (4.9) | 172 | 2 (1.2) |
| NQMC, UK | 75 | 0 (0) | 52 | 0 (0) | 52 | 0 (0) | 66 | 0 (0) |
We compared the proportion of ALI‐induced bullous keratopathy among all eyes with bullous keratopathy among the 3 centres (table 2). KPUM had the greatest overall proportion of ALI‐induced bullous keratopathy (average of 4 years, 2001–2004: 30.5%). In SNEC, the average proportion over 4 years was 6.5%. In contrast, NQMC had no reported cases of ALI‐induced bullous keratopathy throughout the study period.
Table 2 Proportion of bullous keratopathy (BK) cases with ALI as the primary cause, among 3 centres from 2001 to 2004.
| Institution | 2001 | 2002 | 2003 | 2004 | ||||
|---|---|---|---|---|---|---|---|---|
| Total BK | No. of ALI‐induced BK cases (%) | Total BK | No. of ALI‐induced BK cases (%) | Total BK | No. of ALI‐induced BK cases (%) | Total BK | No. of ALI‐induced BK cases (%) | |
| KPUM, Japan | 27 | 9 (33.3) | 37 | 10 (27.0) | 33 | 10 (30.3) | 31 | 10 (32.3) |
| SNEC, Singapore | 22 | 1 (4.5) | 34 | 1 (2.9) | 47 | 6 (12.8) | 51 | 2 (3.9) |
| NQMC, UK | 22 | 0 (0) | 17 | 0 (0) | 16 | 0 (0) | 27 | 0 (0) |
Discussion
ALI has replaced surgical iridectomy as the procedure of choice in the treatment and prevention of primary angle‐closure glaucoma. Previous reports on the long‐term complication of corneal endothelial decompensation after this procedure have been isolated case series.4,7,8 KPUM is a major ophthalmic referral centre that receives patients all across the country. Although our study reports data from a single centre in Japan, these results probably reflect the situation in this country. Our study therefore serves to highlight this potential complication, as well as the widespread problem in Japan, where the incidence of this condition is alarmingly high. A previous nationwide survey conducted in Japan found that up to 13% of registered ophthalmic facilities recorded bullous keratopathy as a complication of laser iridotomy.12
The effect of ALI on the endothelium has been investigated by various investigators, with varying results.5,13,14,15,16 Several authors have demonstrated no significant short‐ or long‐term differences in endothelial cell counts, morphology, as well as corneal thickness after ALI.5,13,14 Conversely, Robin and Pollack15 reported a significant central corneal endothelial loss in argon‐laser‐treated eyes. A few small case series have described the potential long‐term risk of corneal decompensation following ALI.4,7,8 In our study, 20.1% of patients undergoing penetrating keratoplasty had ALI‐induced bullous keratopathy as the primary cause for visual loss, making this among the top 3 leading indications for penetrating keratoplasty in this centre. Endothelial cell damage or loss probably arises from a combination of factors. These include direct focal injury to the endothelium by the laser, heat dissipated from the iris, thermal damage from a rise in temperature of aqueous humor, the mechanical shock waves and turbulent flow of anterior chamber aqueous during the destruction of the iris, anterior chamber inflammation, iris pigment dispersion, pre‐existing corneal guttate and a transient rise in intraocular pressure.4,5,7,8
The reason for the dramatic increase in numbers in Japan compared with other countries is at yet uncertain, although possible aetiologies include inappropriate laser‐treatment protocols, as well as possible anatomical and physiological predisposing factors, that may be peculiar to the Japanese population. In addition, we found that the condition was not only isolated to eyes with acute angle‐closure attacks, but also occurred in fellow eyes following prophylactic laser treatment. In eyes with acute angle‐closure attacks, the presence of corneal oedema may necessitate higher laser energies being required for iris penetration, while the presence of iris bombe increases the proximity of thermal energy dissipating from the iris to the corneal endothelium. The corneal endothelium may be further compromised by the presence of glaucoma, and intraocular inflammation. Despite this, we found that the majority of patients (58.1%) developed ALI‐induced bullous keratopathy in the fellow eye, with some patients developing bullous keratopathy only in the fellow eye.
Laser iridotomies in dark‐coloured irides are associated with higher complication and failure rates.15,17 Pigmented irides require higher laser energies for iris penetration, and the risk of developing ALI‐induced bullous keratopathy is significantly higher in pigmented irides compared with non‐pigmented irides in Caucasian populations.1,4,18 Schwartz et al,4 using a pulsed argon laser, reported a 20% failure rate in penetrating brown eyes, while Quigley1 reported needing 2 or more sessions to achieve patent argon iridotomies in 58% of his patients with dark brown irides. Argon laser energy is well absorbed by dark brown irides. This high‐energy absorption often causes significant charring that may act as a barrier to further penetration. Because the brown pigmented iris is often thicker also, often many more shots are needed to create a patent iridotomy.
Several authors have described the advantages of Q‐switched neodymium (Nd):YAG laser over argon laser for performing iridotomies. Because of its high‐power density, fewer and shorter duration spots are required with Nd:YAG laser iridotomy, resulting in less energy required for iris penetration and less endothelial cell damage and loss.15,17,19,20
Robin and Pollack reported an 8%±7% decrease in central endothelial cell counts after ALI compared with a 0%±5% decrease after Nd:YAG laser iridotomy (p<0.01).15 Most of the previous reports on LI‐induced bullous keratopathy have been in patients that received ALI, rather than Nd:YAG laser iridotomy.4,7 However, Nd:YAG laser alone may not work effectively in dark brown irides, and a combination of both lasers, described as sequential argon‐YAG laser iridotomy, has the benefit that large patent iridotomies can be created with a fraction of the energy required using a pure argon laser alone.10,18 Many centres in Japan perform pure argon laser iridotomies, while sequential argon‐YAG laser iridotomy is the procedure of choice in Singapore.10,11 This may help to explain the lower incidence of laser peripheral iridotomy‐induced bullous keratopathy in Singapore compared with Japan, despite the fact that Singapore has the highest incidence of primary angle‐closure glaucoma reported to date.9
Our study highlights the potential long‐term risk of corneal decompensation and bullous keratopathy in patients undergoing ALI and the growing problem in Asian countries. This is an area of major concern in Japan, which is seeing a worrying increase in the number of patients with this condition. Asian patients with dark pigmented irides are particularly at risk, and these patients should be properly counselled regarding the potential risk of this condition. The use of sequential argon‐YAG laser iridotomy may help to reduce the amount of laser energy used and the amount of corneal endothelial loss, which may in turn help to reduce the risk of corneal decompensation in the long‐term.
Abbreviations
ALI - argon laser iridotomy
KPUM - Kyoto Prefectural University of Medicine
NQMC - Nottingham Queen's Medical Centre
SNEC - Singapore National Eye Centre
Footnotes
Financial support: None.
Commercial interests: The authors have no commercial interest in any of the material discussed in the paper.
References
- 1.Quigley H A. Long‐term follow‐up of laser iridotomy. Ophthalmology 198188218. [DOI] [PubMed] [Google Scholar]
- 2.Ritch R, Podos S M. Argon laser treatment of angle‐closure glaucoma. Perspect Ophthalmol 19804129 [Google Scholar]
- 3.Robin A L, Pollack I P. Argon laser peripheral iridotomies in the treatment of primary angle‐closure glaucoma. Long‐term follow‐up. Arch Ophthalmol 1982100919. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz A, Martin N F, Weber P A. Corneal decompensation after argon laser iridotomy. Arch Ophthalmol 19881061572–1574. [DOI] [PubMed] [Google Scholar]
- 5.Smith J, Whitted P. corneal endothelial changes after argon laser iridotomy. Am J Ophthalmol 198498153–156. [DOI] [PubMed] [Google Scholar]
- 6.Hirst L, Robin A, Sherman S.et al Corneal endothelial changes after argon‐laser iridotomy and panretinal photocoagulation. Am J Ophthalmol 198293473. [DOI] [PubMed] [Google Scholar]
- 7.Wilhelmus K R. Corneal edema following argon laser iridotomy. Ophthal Surg 199223533–537. [PubMed] [Google Scholar]
- 8.Lim L S, Ho C L, Ang L P.et al Inferior corneal decompensation following laser peripheral iridotomy in the superior iris. Am J Ophthalmol. 2006 Jul 142166–168. [DOI] [PubMed] [Google Scholar]
- 9.Seah S K L, Foster P J, Chew P T K.et al Incidence of acute primary angle closure glaucoma in Singapore. An island‐wide survey. Arch Ophthalmol 19971151436–1440. [DOI] [PubMed] [Google Scholar]
- 10.Aung T, Ang L P K, Chew P T K. Acute primary angle‐closure glaucoma: Long‐term intraocular pressure outcome in an Asian population. Am J Ophthalmol 200117–12. [DOI] [PubMed] [Google Scholar]
- 11.Ang L P K, Aung T, Chew P T K. Acute primary angle closure in an asian population: Long‐term outcome of the fellow eye after prophylactic laser peripheral iridotomy. Ophthalmology 20001072092–2096. [DOI] [PubMed] [Google Scholar]
- 12.Kashiwagi K, Tsukahara S. Examination and treatment of patients with angle‐closure glaucoma in Japan: results of a nationwide survey. Jpn J Ophthalmol 200448133–140. [DOI] [PubMed] [Google Scholar]
- 13.Panek W C, Lee D A, Christensen R E. Effects of argon laser iridotomy on the corneal endothelium. Am J Ophthalmol 1988105395–397. [DOI] [PubMed] [Google Scholar]
- 14.Thoming C, Buskirk M V, Samples J R. The corneal endothelium after laser therapy for glaucoma. Am J Ophthalmol 1987103518–522. [DOI] [PubMed] [Google Scholar]
- 15.Robin A L, Pollack I P. A comparison of Nd:YAG and argon laser iridotomies. Am J Ophthalmol 1984911011–1016. [DOI] [PubMed] [Google Scholar]
- 16.Hong C, Kitazawa Y, Tanishima T. Influence of argon laser treatment of glaucoma on corneal endothelium. Jpn J Ophthalmol 198327567–574. [PubMed] [Google Scholar]
- 17.Tomey K F, Traverso C E, Shammas I V. Neodymium‐YAG laser iridotomy in the treatment and prevention of angle closure glaucoma. Arch Ophthalmol 1987105476–481. [DOI] [PubMed] [Google Scholar]
- 18.Ho T, Fan R. Sequential argon‐YAG laser iridotomies in dark irides. Br J Ophthalmol 199276329–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robin A L, Pollack I P. Q‐switched Nd:YAG laser iridotomy in patients in whom the argon laser fails. Arch Ophthalmol 1986104531–535. [DOI] [PubMed] [Google Scholar]
- 20.Moster M R, Chwartz L W, Spaeth G L.et al Laser iridotomy: a controlled study comparing argon and neodymium:YAG. Ophthalmology 19869320–24. [PubMed] [Google Scholar]