Abstract
The term “columnar cell lesions” encompasses a spectrum of processes, characterised by variably dilated acini, lined by one to several layers of tightly packed, columnar‐shaped epithelial cells. These lesions have received renewed attention in the literature due to their high prevalence in biopsy specimens taken for assessment of mammographically detected microcalcification. In addition, increasing interest has been directed at the sub‐set of columnar cell lesions with varying degrees of cytological atypia. Recent observational and molecular genetic studies have provided strong circumstantial evidence to suggest that at least some of these lesions may represent the earliest morphologically identifiable, non‐obligate precursor of low grade breast carcinomas. However, the risk of both local recurrence and progression to invasive cancer appears to be exceedingly low. This review provides an update on recent clinicopathological and molecular data on columnar cell lesions and how these have changed our perception of, and the classification system for, these lesions. In addition, guidelines for the management of patients with columnar cell lesions diagnosed in core needle biopsy specimens are provided.
Columnar cell lesions in the breast have been recognised by histopathologists for a long period of time, but under a wide variety of names such as blunt duct adenosis, clinging carcinoma of monomorphic type,1 columnar alteration with prominent apical snouts and secretions,2 atypical cystic lobules,3 enlarged lobular units with columnar alteration4 and hyperplastic unfolded lobules,5 among others. This lack of clarity in nomenclature makes interpretation of the medical literature difficult with regard to incidence, behaviour and significance of these lesions. However, it is clear that such lesions are being seen more frequently as a result of breast screening mammography; they frequently present with, often low suspicion, microcalcifications on breast mammography and are, as a result, an increasingly common finding in non‐operative breast core samples. Indeed, columnar alterations were reported in 42% of 100 consecutive biopsy specifications for microcalcifications in one of the early seminal papers2 on these lesions. Specifically, the calcification was present within the columnar process itself in 74% of cases; these lesions are generally a direct cause of the radiological findings, not a coincidental histological finding.
The term “columnar cell lesions” is now widely used and incorporates a family of entities. The spectrum ranges from columnar cell change and columnar cell hyperplasia, through cytologically low grade but atypical lesions (flat epithelial atypia), architecturally complex lesions (now regarded as forms of atypical ductal hyperplasia (ADH), or indeed low grade ductal carcinoma in situ (DCIS) if more extensive). At the upper end of the spectrum one might include flat high grade DCIS, although the latter is not generally included in this group of entities. It should be noted that many columnar cell lesions in breast core biopsy samples cause no significant diagnostic difficulty. However, there is a small, but important sub‐group, that shows either cytological or architectural atypia and which can be problematic for the pathologist regarding diagnosis and classification, and the whole multidisciplinary team with respect to clinical behaviour and management. Such lesions can be especially difficult to interpret in core samples, due to the partial sampling of lesions inherent in the biopsy technique.
Microscopy of columnar cell lesions
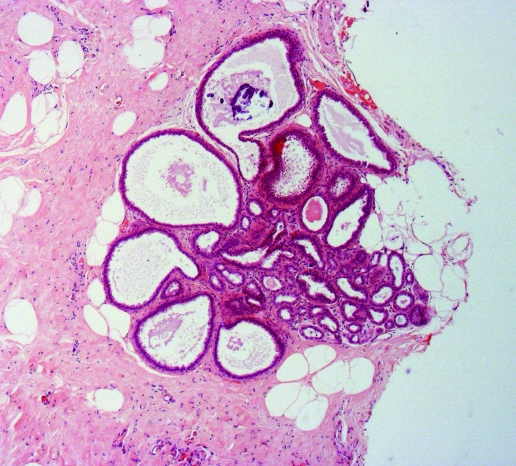
Table 1 summarises features which assist in distinguishing the forms of columnar cell lesion and ADH. It is useful to remember that columnar cell changes arise in the terminal duct lobular unit (TDLU), and in surgical specimens the low power assessment of the overall architecture and geographical nature is valuable (fig 1). This may not be assessable in core biopsy specimens, which include only small portions of tissue. At a higher power examination, columnar cell change can be seen to be formed from a single or a double layer of columnar cells that are of regular size and shape with relatively bland nuclear features and which are arranged perpendicular to the basement membrane. The nuclei are uniform, typically ovoid, with finely dispersed chromatin and do not bear conspicuous nucleoli. Mitoses are not generally seen. Secretions and calcifications are often present in the lumen and apical snouts are noted at the luminal aspect of the cells.
Table 1 Differential diagnosis of columnar cell change, columnar cell hyperplasia, flat epithelial atypia and atypical ductal hyperplasia.
| Feature | CCC | CCH | FEA | ADH |
|---|---|---|---|---|
| Cell morphology | Columnar | Columnar | Columnar and/or cuboidal | Cuboidal |
| Number of cell layers | ⩽2 | >2 | Variable | Variable |
| Architecture | Flat | Tufts/mounds | Flat or tufts/mounds. Not complex* | Complex architectural pattern* |
| Nuclear atypia† | Absent | Absent | Present | Present |
| Nuclear features† | Ovoid, bland, polarised nuclei arranged perpendicular to basement membrane | Ovoid, bland; some nuclear crowding and overlapping of nuclei may be observed. Nuclei arranged perpendicular to basement membrane | In typical form: round, uniform, evenly‐spaced with finely dispersed chromatin, as in low grade DCIS. Alternatively may show more “classical” cytonuclear atypia in the form of enlarged, more oval nuclei with mild to moderate pleomorphism; some clumping of chromatin may be seen | Round and evenly spaced as in low grade DCIS; finely dispersed chromatin |
| Nuclear to cytoplasmic ratio | Normal | Normal | Increased | Increased |
| Internal contours of acini | Irregular | Irregular | Typically smooth | Variable |
ADH, atypical ductal hyperplasia; CCC, columnar cell change; CCH, columnar cell hyperplasia; FEA, flat epithelial atypia; DCIS, ductal carcinoma in situ.
*True micropapillae (with bulbous tip extending into the lumen from a narrower stalk) or sieve‐like cribriform spaces.
†Cases with high grade nuclear atypia should be classified as flat high grade DCIS and do not fall within either the spectrum of FEA or of ADH.
Figure 1 Columnar cell change affecting a terminal duct lobular unit. Note the presence of a coarse microcalcification.
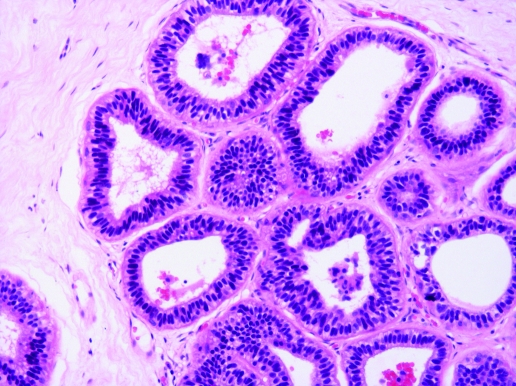
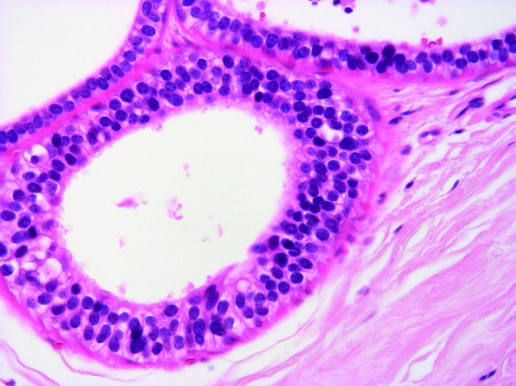
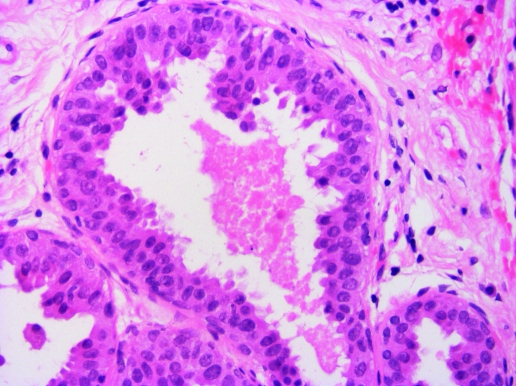
The morphology of the cells forming columnar cell hyperplasia is essentially similar to those of columnar cell change (figs 2 and 3). Rather than a single or double layer of cells, however, there is focal stratification; mounds or tufts of epithelial cells are often formed. True micropapillae (with bulbous tip extending into the lumen from a narrower stalk) or sieve‐like cribriform spaces are not a feature of columnar cell hyperplasia but should make one search for additional features of ADH/DCIS. There may, however, be some nuclear crowding and/or overlapping of nuclei in columnar cell hyperplasia. This should not be mistaken for an atypical proliferative process; of note, low grade neoplastic processes in the breast (ADH, DCIS and lobular in situ neoplasia) are typically formed from evenly‐spaced, regular, uniform cells. In columnar cell hyperplasia more overlapping and variation of cells is seen, although this is not as marked as in usual epithelial hyperplasia, which is truly formed from cells of a mixed phenotype. Apical snouts are often prominent in columnar cell hyperplasia and there is frequently abundant intraluminal secretion with microcalcification.
Figure 2 Columnar cell hyperplasia composed of tightly packed, columnar shaped cells, with elongated nuclei, arranged in >2 layers. Note the presence of some nuclear crowding and overlapping of nuclei.
Figure 3 Columnar cell hyperplasia with rudimentary mounds/tufts of columnar‐shaped cells. Nuclei are ovoid and closely packed. Apical snouts are present. There is no significant atypia.
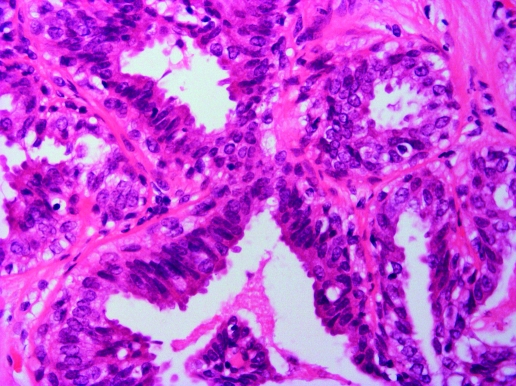
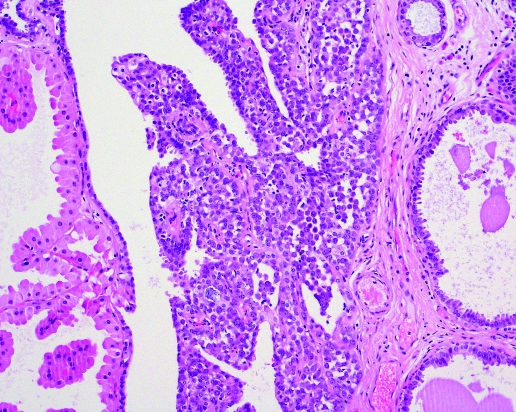
Superimposed on the columnar cell morphology of the one or two layers of epithelial cells of columnar cell change or the stratified layering of columnar cell hyperplasia, there may be atypia. In previous systems of classification6,7 this was subdivided into architectural or cytological types. Subsequently, the World Health Organization Working Group on the Pathology and Genetics of Tumours of the Breast8 applied the term flat epithelial atypia (FEA) for columnar cell lesions with cytological atypia. That this term encompasses both columnar cell change and columnar cell hyperplasia, with cytological atypia, is somewhat counterintuitive; it should be noted that flat epithelial atypia is not necessarily “flat”, but rather does not form complex architectural patterns such as cribriform spaces or micropapillae. Those lesions previously categorised as columnar cell hyperplasia with architectural atypia, due to the presence of bridges or micropapillary structures formed from epithelial cells showing mild cytonuclear atypia, are now classified within the spectrum of ADH (fig 4) or low grade DCIS. This latter categorisation depends, as in other situations, on the nature and the extent of the cytological and architectural atypia.
Figure 4 Lesion composed of a peripheral population formed from columnar cells with apical snouts. However there is architectural atypia in the form of rudimentary cribriform spaces. In the central portion of the space, the epithelial cell nuclei are more rounded and uniform and show mild cytological atypia. Lesions with such features should be classified within the spectrum of atypical ductal hyperplasia/low grade ductal carcinoma in situ, depending on extent of the process.
The TDLUs bearing FEA have been described as typically having a rounded luminal shape, rather than an irregular internal outline as is seen in columnar cell changes without atypia; this feature may be valuable on low power examination of the section. Similarly, at low power examination the TDLUs bearing FEA may be darker appearing than usual, due to an increased nuclear to cytoplasmic ratio of the characteristic cells. In addition, on occasions visible on low power, a lymphoid infiltrate formed from collections of mature lymphoid cells may be present in the stroma associated with, and adjacent to, the FEA.
On higher power examination, FEA is most commonly formed from cuboidal cells with features of low grade DCIS; thus nuclei are round, small, uniform and evenly‐spaced (fig 5). The chromatin pattern is finely dispersed. Nucleoli tend not to be conspicuous and mitoses are rarely seen. Apical snouts are commonly present and secretions with microcalcification noted. This form of FEA may be subtle and care should be taken not to overlook the lesion in breast histology specimens.
Figure 5 Flat epithelial atypia composed of a population of cuboidal cells with features of low grade ductal carcinoma in situ. The small, monomorphic and evenly‐spaced nuclei are round rather than ovoid, with finely dispersed chromatin.
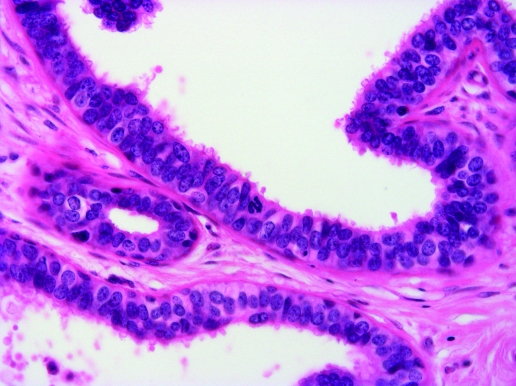
In other forms within the category of FEA, the cells retain more of an overt columnar morphology, and thus may be more elongated and polarised, with nuclei arranged perpendicular to the basement membrane. However, in addition to these architectural features of columnar cell change or hyperplasia, the cells also show cytologically atypical features, of more “classical” type, including cytological pleomorphism, clumping of chromatin and distinct nucleoli. The nuclei may, in essence, be essentially similar to those nuclei seen typically in tubular carcinomas with a more obvious increase in nuclear to cytoplasmic ratio (fig 6) than seen in the form of flat epithelial atypia with round, uniform, evenly spaced nuclei, described above. Less commonly, the nuclei may show a superficial resemblance to the cytology of colorectal adenomas.
Figure 6 Flat epithelial atypia formed from columnar cells showing mild to moderate nuclear atypia with an increased nuclear to cytoplasmic ratio. Mounding and tufting can be observed and apical snouts are present.
In core biopsy specimens in particular, cytological atypia in columnar cell change may be difficult to assess and a tightrope must be balanced between over‐diagnosis (and an excessively high benign biopsy rate in subsequent surgical diagnostic biopsy) and reporting as atypical any lesions of concern.
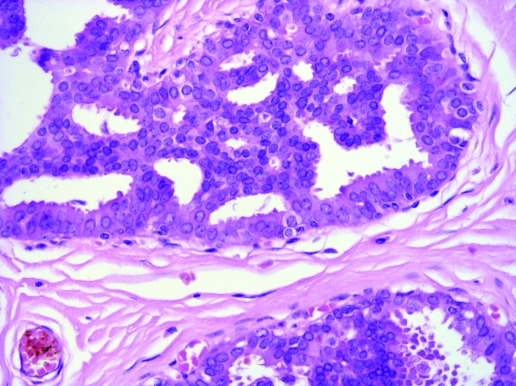
It should be remembered, however, if the cytonuclear features are those of high grade atypia, for example, formed from large cells showing marked pleomorphism and nuclear atypia, then the disease should be categorised as flat high grade DCIS and not as FEA. This too may be difficult to assess and caution is advised not to “over‐call” lesions with moderate atypia as flat high grade DCIS in core biopsy; in such cases prudence should be applied, and on occasions the suspicious (B4) category can be used (fig 7).
Figure 7 Cytonuclear atypia in a columnar cell process. Note the apical snouts and columnar morphology, but in association with nuclei showing atypia in the form of mild pleomorphism, variation in shape, clumped chromatin and prominent nucleoli. The degree is insufficient for the diagnosis of flat high grade ductal carcinoma in situ (DCIS); lesions such as this also fall within the spectrum of flat epithelial atypia. Note the mitotic figure; these are unusual in flat epithelial atypia, as in atypical ductal hyperplasia/low grade DCIS.
Differential diagnosis
The differential diagnosis of columnar cells lesion includes apocrine metaplasia and other fibrocystic changes, such as small benign cysts. Careful examination of the cytological features of the epithelium should be undertaken to avoid missing the diagnosis of FEA in particular, which can be subtle and which can be overlooked completely or misinterpreted as microcysts. Both apocrine change and columnar cell lesions arise in the TDLU and although both have apical snouts, morphological assessment will show the granular, eosinophilic cytoplasm with inclusions in apocrine change. The nuclei of apocrine cells are also typically larger, have one or more prominent nucleoli, and may show some variation in size; the nuclei of columnar cell change are blander, more uniform and lack prominent nucleoli.
Unfortunately additional and special stains are, in general, of little assistance in the assessment and diagnosis of columnar cell lesions, with or without atypia. The cells of the columnar cell processes typically express luminal cytokeratins, such as cytokeratin 19, and both oestrogen and progesterone receptors.7 In particular, the pattern of oestrogen receptor staining in columnar cell change is typically diffusely positive when compared to heterogeneous positivity of usual epithelial hyperplasia and normal breast lobules.7,9,10,11 Conversely, columnar cell lesions do not express basal markers such as cytokeratin 5/6.7 In cases when the there is uncertainty in distinguishing columnar cell change from apocrine change, immunohistochemistry may prove helpful as columnar cells invariable express oestrogen receptor and also bcl‐2,10 while apocrine cells typically express gross cystic disease fluid protein 15 but are negative for bcl‐2 and oestrogen receptor.
Molecular and genetic studies and clinical studies of columnar cell lesions
The clinical significance of the columnar cell lesions remains poorly understood. Although this is in part due to the difficulties in interpretation of the medical literature due to the nomenclature used, as noted above, such lesions have recently been studied in small numbers and in few observational series. Flat epithelial atypia is more frequently identified in association with established DCIS than one would see purely by chance.2,3 Columnar cell lesions, in particular those with nuclear atypia, may also co‐exist with lobular in situ neoplasia12,13 (fig 8). Observational studies have, in addition, noted a relationship with tubular carcinoma,11,14 and Rosen suggested some years ago that that tubular carcinoma “might sometimes arise when the hyperplastic lesion transformed”.12
Figure 8 Terminal duct lobular unit concurrently affected by columnar cell change (right), lobular neoplasia (centre) and apocrine metaplasia (left).
Apart from this, somewhat circumstantial, evidence and opinion, robust data on the clinical behaviour of these lesions is very scarce; Eusebi et al found 25 cases of monomorphic/low grade “clinging” carcinoma from 80 cases of DCIS out of a total of 9446 biopsy specimens originally diagnosed as benign.15 However, only one of the 25 cases developed a so‐called recurrence, at a mean follow up of 17.5 years, and this as the same “clinging” carcinoma, which would now be classified as FEA.16 Importantly, no cases developed invasive disease. Similarly, in the EORTC 10853 DCIS trial,17 59 patients with low grade “clinging” carcinoma were noted; with a median follow‐up of 5.4 years, no local recurrences have been reported. De Mascarel et al have reported in abstract form on 115 patients with columnar cell hyperplasia with atypia,18 45 of who had had radiotherapy; they identified three cases of subsequent invasive carcinoma, one case of DCIS in the contralateral breast and three “recurrences” of FEA. Thus, overall, authorities on the subject suggest that the risk of patients developing invasive breast carcinoma in the same breast as an index case of FEA is very low,19 albeit based on the limited date available to date regarding the precursor risk of columnar cell lesions.
Small series examining the molecular and genetic changes in atypical columnar cell lesions have begun to appear in the medical literature; the numbers in many of these are small. Moinfar et al20 noted a high level (77%) of loss of heterozygosity (LOH), most commonly at 11q, 16q and 3p. Eighteen cases were associated with DCIS or invasive carcinoma, in which similar genetic changes were present. Similarly, Simpson et al7 found changes in FEA and in associated columnar cell change and columnar cell hyperplasia using comparative genomic hybridisation. In five of eight cases, there were also similar abnormalities in associated DCIS or invasive carcinoma, suggesting an evolutionary spectrum. The genetic changes were few in number, but recurrent losses (eg, of 16q, 17p) and gains (eg, of 16p) were present across the spectrum of 81 lesions from 18 patients. Interestingly, the degree of hyperplasia and atypia at the morphological level was associated with a stepwise increase in the number of unbalanced chromosomal changes at the molecular level.7 Several of the reported series to date have thus examined somewhat biased groups of columnar cell lesions that have included, in the same patients, a range of abnormalities through to DCIS and invasive carcinoma. Very few cases of the commoner and less worrisome end of the spectrum that are not associated with more advanced disease in the same breast have been examined. Dabbs et al21 reported that neither of two examples of pure columnar cell change showed abnormalities with LOH assessment, but losses at one or more loci were present in two of three cases of columnar cell hyperplasia and in two‐thirds of the 15 cases of FEA. However, the most frequent loci reported to be affected in CCL/FEA, 16q and 11q7,10,20 in other series, were not analysed in that study.21 As in the other molecular studies described, some of the genetic alterations in the columnar cell lesions in this study were similar to those in associated DCIS and invasive carcinoma. Thus, at least a proportion of columnar cell lesions almost certainly represents the earliest form of precursor of low grade DCIS and of invasive breast carcinoma recognised to date. Interestingly, the idea that columnar cell changes could be the earliest morphologically identifiable precursor of breast cancer was first put forward in British literature by Muir, in 1941, who suggested that in the evolution of breast cancer, the “earliest change to be observed in the epithelium of the acini is an increased prominence of the cells; they become…often of more columnar type; sometimes this is a marked feature”.22
Management of columnar cell lesions in breast core biopsy specimens
Despite the emerging molecular information regarding the neoplastic and precursor nature of, at least a subset of, columnar cell lesions, the management of these lesions is also based on very limited data. There is an urgent need for clarity regarding the clinical behaviour, and guidance regarding management of these lesions, both when identified in breast cores and in subsequent diagnostic surgical samples.
Columnar cell change or columnar cell hyperplasia is regarded as benign and should be categorised as such (B2) on core biopsy. There is no need to undertake additional assessment in the form of further levels or immunohistochemistry (the latter, as noted above is often unhelpful) and the case should be managed as per the multidisciplinary team discussion. Thus if the histopathological findings are concordant with the radiological/clinical features, the available data suggests that diagnostic surgical excision is not required when columnar cell change or columnar cell hyperplasia is identified in a breast core biopsy specimen.
When, however, cytological atypia is present and the lesion is reported histologically as FEA, the core biopsy should be classified as bearing a lesion of uncertain malignant potential (B3). Similarly, if there is architectural atypia the core should be categorized according to the extent and degree of this; this will often be placed within the B3 category, akin to ADH (although the term ADH is not recommended in core biopsy reporting, as per the UK NHS BSP Guidelines23).
There is, it must be noted, very limited outcome data which indicates that subsequent excision shows a more advanced lesion in 20%24 to 30% of cases25 when columnar cell atypia/FEA is identified in a core biopsy; this is almost entirely derived from abstracts rather than peer‐reviewed manuscripts and the numbers in the series are small.24,25,26,27,28,29,30,31 It is clear that there is an association with malignancy, for example tubular carcinoma as noted above, and these additional data are sufficiently worrisome that most authorities recommend diagnostic surgical excision following diagnosis of columnar cell atypia/FEA in a breast core biopsy.32 However, further series of larger numbers of cases of core biopsies with columnar cell atypia with follow‐up surgery are urgently required to clarify the clinical association with more established malignancy, which remains in doubt.
Conclusion
In conclusion, columnar cell lesions are being identified with increasing frequency in breast core biopsy specimens undertaken for the assessment of mammographic microcalcifications, often of low radiological suspicion. Although the majority of these lesions do not cause significant diagnostic difficulty, a sub‐group of these lesions shows atypical histological features; these should be classified as B3, lesion of uncertain malignant potential, on core biopsy. Such atypical columnar cell lesions remain poorly understood, but small studies have begun to describe the molecular and clinical findings in these lesions. Although there are still very limited data, these suggest that FEA may be the earliest morphologically identifiable non‐obligate precursor of low grade breast carcinomas. The true precursor risk appears very low, but these lesions may co‐exist with entities such as low grade DCIS and low grade invasive carcinoma. Thus when FEA is identified in a breast core biopsy specimen, at present it is recommended that diagnostic surgical excision should be undertaken to search for more established adjacent malignant disease.
Take‐home messages
Columnar cell lesions are frequently seen as a cause of mammographic microcalcification.
The majority are benign (B2), but a minority show low grade cytological atypia (flat epithelial atypia) and should be reported as B3 on core biopsy.
There is emerging evidence that such low grade atypical columnar cell lesions are the earliest non‐obligate precursors of breast cancer, to date.
If architectural atypia is also present, the lesion should be reported as atypical ductal hyperplasia or low grade ductal carcinoma in situ, according to extent.
Footnotes
Competing interests: None declared.
References
- 1.Azzopardi J G.Problems in breast pathology. Philadelphia, PA: WB Saunders, 1978193–202.
- 2.Fraser J L, Raza S, Chorny K.et al Columnar alteration with prominent apical snouts and secretions: a spectrum of changes frequently present in breast biopsies performed for microcalcifications. Am J Surg Pathol 1998221521–1527. [DOI] [PubMed] [Google Scholar]
- 3.Oyama T, Maluf H, Koerner F. Atypical cystic lobules: an early stage in the formation of low‐grade ductal carcinoma in situ. Virchows Arch 1999435413–421. [DOI] [PubMed] [Google Scholar]
- 4.McLaren B K, Gobbi H, Schuyler P A.et al Immunohistochemical expression of estrogen receptor in enlarged lobular units with columnar alteration in benign breast biopsies: a nested case‐control study. Am J Surg Pathol 200529105–108. [DOI] [PubMed] [Google Scholar]
- 5.Arpino G, Laucirica R, Elledge R M. Premalignant and in situ breast disease: biology and clinical implications. Ann Intern Med 2005143446–457. [DOI] [PubMed] [Google Scholar]
- 6.Schnitt S J, Vincent‐Salomon A. Columnar cell lesions of the breast. Adv Anat Pathol 200310113–124. [DOI] [PubMed] [Google Scholar]
- 7.Simpson P T, Gale T, Reis‐Filho J S.et al Columnar cell lesions of the breast: the missing link in breast cancer progression? A morphological and molecular analysis. Am J Surg Pathol 200529734–746. [DOI] [PubMed] [Google Scholar]
- 8.Tavassoli F A, Hoefler H, Rosai J.et al Intraductal proliferative lesions. In: Tavassoli FA, Devilee P, eds. Pathology and genetics: tumours of the breast and female genital organs. Lyon: IARC Press, 200363–73.
- 9.Shoker B S, Jarvis C, Clarke R B.et al Abnormal regulation of the oestrogen receptor in benign breast lesions. J Clin Pathol 200053778–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fraser JL R S, Chorny K, Connolly J L.et al Immunophenotype of columnar alteration with prominent apical snouts and secretions (CAPSS). Lab Invest 20008021A [Google Scholar]
- 11.Tremblay G, Deschenes J, Alpert L.et al Overexpression of estrogen receptors in columnar cell change and in unfolding breast lobules. Breast J 200511326–332. [DOI] [PubMed] [Google Scholar]
- 12.Rosen P P. Columnar cell hyperplasia is associated with lobular carcinoma in situ and tubular carcinoma. Am J Surg Pathol 1999231561. [DOI] [PubMed] [Google Scholar]
- 13.Sahoo S, Recant W M. Triad of columnar cell alteration, lobular carcinoma in situ, and tubular carcinoma of the breast. Breast J 200511140–142. [DOI] [PubMed] [Google Scholar]
- 14.Ho B C, Tan P H. Flat epithelial atypia: concepts and controversies of an intraductal lesion of the breast. Pathology 200537105–111. [DOI] [PubMed] [Google Scholar]
- 15.Eusebi V, Feudale E, Foschini M P.et al Long‐term follow‐up of in situ carcinoma of the breast. Semin Diagn Pathol 199411223–235. [PubMed] [Google Scholar]
- 16.Viale G. Histopathology of primary breast cancer 2005. Breast 200514487–492. [DOI] [PubMed] [Google Scholar]
- 17.Bijker N, Peterse J L, Duchateau L.et al Risk factors for recurrence and metastasis after breast‐conserving therapy for ductal carcinoma‐in‐situ: analysis of European Organization for Research and Treatment of Cancer Trial 10853. J Clin Oncol 2001192263–2271. [DOI] [PubMed] [Google Scholar]
- 18.de Mascarel I, MacGrogan G, Picot V.et al Results of a long term follow‐up study of 115 patients with flat epithelial atypia. Lab Invest 20068625A [Google Scholar]
- 19.Schnitt S J. The diagnosis and management of pre‐invasive breast disease: flat epithelial atypia—classification, pathologic features and clinical significance. Breast Cancer Res 20035263–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moinfar F, Man Y G, Bratthauer G L.et al Genetic abnormalities in mammary ductal intraepithelial neoplasia‐flat type (“clinging ductal carcinoma in situ”): a simulator of normal mammary epithelium. Cancer 2000882072–2081. [PubMed] [Google Scholar]
- 21.Dabbs D J, Carter G, Fudge M.et al Molecular alterations in columnar cell lesions of the breast. Mod Pathol 200619344–349. [DOI] [PubMed] [Google Scholar]
- 22.Muir R. The evolution of carcinoma of the mamma. J Pathol Bacteriol 194152155–172. [Google Scholar]
- 23.Non‐operative Diagnosis Subgroup of the National Coordinating Group for Breast Screening Pathology Guidelines for non‐operative diagnostic procedures and reporting in breast cancer screening. NHS BSP Publication No 50. Sheffield: NHS, 2001
- 24.Lim C N, Ho B C, Bay B H.et al Nuclear morphometry in columnar cell lesions of the breast: is it useful? J Clin Pathol 2006591283–1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brogi E, Tan L K. Findings at excisional biopsy (EBX) performed after identification of columnar cell change (CCC) of ductal epithelium in breast core biopsy (CBX). Mod Pathol 20021529A–30A. [Google Scholar]
- 26.Harigopal M Y D, Hoda S A, DeLellis R A.et al Columnar cell alteration diagnosed on mammotome core biopsy for indeterminate microcalcifications: results of subsequent mammograms and surgical excision. Mod Pathol 20021536A [Google Scholar]
- 27.Nasser S, Fan M J. Does atypical columnar cell hyperplasia on breast core biopsy warrant follow‐up excision? Mod Pathol 20031642A [Google Scholar]
- 28.Kunju L P, Kleer C G. Significance of flat epithelial atypia (FEA) on mammotome core needle biopsy: should it be excised? Lab Invest 20068632A. [DOI] [PubMed] [Google Scholar]
- 29.Lubelsky S M, Bane A L, Shin V.et al Columnar cell lesions and flat epithelial atypia: incidence and significance in a mammographically screened population. Lab Invest 20058541A [Google Scholar]
- 30.Bai H, Sung C J, Wu Q.et al Flat epithelial atypia in breast needle core biopsies: a correlative followup study. Lab Invest 20058525A [Google Scholar]
- 31.Xu C, Chung A, Giri D. Diagnosis of columnar cell change with atypia on breast core biopsy: impact of inter‐observer variability, degree of atypia and the volume of lesional changes on surgical management. Lab Invest 20058555A [Google Scholar]
- 32.Jacobs T W, Connolly J L, Schnitt S J. Nonmalignant lesions in breast core needle biopsies: to excise or not to excise? Am J Surg Pathol 2002261095–1110. [DOI] [PubMed] [Google Scholar]