Abstract
Recombinant polioviruses expressing foreign antigens may provide a convenient vaccine vector system to induce protective immunity against diverse pathogens. Replication-competent chimeric viruses can be constructed by inserting foreign antigenic sequences within the poliovirus polyprotein. When inserted sequences are flanked by poliovirus protease recognition sites the recombinant polyprotein is processed to mature and functional viral proteins plus the exogenous antigen. It previously has been shown that poliovirus recombinants can induce antibody responses against the inserted sequences but it is not known whether poliovirus or vaccine vectors derived from it can elicit effective cytotoxic T lymphocyte (CTL) responses. To examine the ability of the recombinant poliovirus to induce CTL responses, a segment of the chicken ovalbumin gene, which includes the H2-Kb-restricted CTL epitope SIINFEKL, was cloned at the junction of the P1 and P2 regions. This recombinant virus replicated with near wild-type efficiency in culture and stably expressed high levels of the ovalbumin antigen. Murine and primate cells infected with the recombinant virus appropriately processed the SIINFEKL epitope and presented it within major histocompatibility complex class I molecules. Inoculation of mice with recombinant poliovirus that expresses ovalbumin elicits an effective specific CTL response. Furthermore, vaccination with these recombinant poliovirus induced protective immunity against challenge with lethal doses of a malignant melanoma cell line expressing ovalbumin.
Protective immunity against many infectious diseases and effective immunotherapies for cancer may require priming of both humoral and cellular immune responses. In particular, the generation of an effective CD8+ cytotoxic T lymphocyte (CTL) activity is thought to be especially important for control of virally infected cells and tumors. CTLs recognize antigens as short fragments of proteins (8–10 amino acids long) bound to major histocompatibility complex (MHC) class I molecules on the cell surface. Most of these peptide epitopes are derived from the cytosolic degradation of proteins that are synthesized within the host cell and are translocated by specific transporters from the cytosol into the endoplasmic reticulum where they bind to MHC class I molecules. The peptide-MHC class I complex then is transported, through the Golgi apparatus, to the cell surface where it is presented to CD8+ T lymphocytes (1).
A current challenge for vaccine development is to find new ways to efficiently deliver relevant antigens into the MHC class I pathway. Recombinant viruses represent a particularly promising approach because they can replicate in a variety of host cell types and induce both humoral and cell-mediated immune responses. A number of different viruses, including vaccinia and adenovirus, have been used to develop recombinant vaccines to immunize against a variety of pathogens (2). Recently, poliovirus, a member of the picornavirus family, has been proposed as a candidate vaccine vector (3–7). Advantages of the life-attenuated poliovirus vaccine (Sabin strains) include its extensive use in humans, its safety, and its ability to induce long-lasting protective immunity. In addition, poliovirus vaccines are easy to administer by the oral route, have a sufficiently low cost to enable their distribution in the developing world, and induce both systemic humoral immunity and local intestinal mucosal resistance to poliovirus infection (8). Induction of mucosal immunity is thought to be important to protect against pathogens that cause disease at the mucosal surfaces, such as respiratory or gastrointestinal pathogens, or that gain access through a mucosal port of entry, such as sexually transmitted diseases.
Given these favorable characteristics of the Sabin poliovirus vaccine a number of laboratories have developed several strategies for the construction of recombinant polioviruses (3–7). We previously have constructed poliovirus recombinants that express genes derived from HIV, simian immunodeficiency virus, and hepatitis B virus. All of these constructs induced potent antibody responses against the foreign antigen in mouse and monkeys (3, 9, 10). However, despite decades of use of the poliovirus vaccine, the ability of poliovirus, or the attenuated vaccine strain, to elicit MHC class I-restricted CD8+-CTL responses has not been documented (2). Although inoculation of purified poliovirus particles in mice has been reported to induce CTL responses to poliovirus capsid protein, the immunological significance of those observations is difficult to assess because the mice used in those studies lacked the specific human poliovirus receptor and thus were not susceptible to infection (11). Although viruses from diverse families (e.g., poxviruses, adenovirus, and herpesvirus) have been found to posses a variety of strategies that enable them to resist clearance by the host immune response (12–17), it is not known whether or not poliovirus has similar mechanisms. In fact, Kirkegaard and coworkers (18, 19) have shown that protein transport through the host secretory pathway is inhibited during poliovirus infection caused by the action of viral proteins 2B, 2BC, and 3A, each of which is capable of inhibiting protein secretion. These findings led to speculations that, by down-regulation of MHC class I transport to the cell surface, poliovirus-infected cells may escape CD8-mediated CTL immunity.
To evaluate the ability of replication-competent recombinant poliovirus to induce specific CD8+ lymphocyte responses, we constructed Polio-Ova, a recombinant poliovirus that expresses the C-terminal half of chicken ovalbumin (Ova). Polio-Ova stably expresses and appropriately processes the Ova fragment, and the specific Ova peptide epitope is efficiently presented by MHC class I in infected cells. Importantly, infection of poliovirus-susceptible mice with Polio-Ova induces a specific CTL response and protects against experimental challenge with a lethal dose of malignant melanoma cells that express Ova.
MATERIALS AND METHODS
Recombinant Polioviruses.
Construction of Polio-Sp27 has been described previously (10). Polio-Ova was constructed by using a similar procedure. Briefly, the C-terminal half of Ova was amplified by PCR from the plasmid pBSK-Ova (20) by using primers 1 (5′-GGGGAGGTGAATTCGTGACTGAGCAAGAAA-3′) and 2 (5′-GTCAGATCCTCGAGAGGGGAAACACATCTG-3′) that included restriction enzyme sites EcoRI and XhoI, which were used to insert the PCR-amplified exogenous DNA into the vector polylinker. PCR fragments used in cloning were digested with EcoRI and XhoI restriction enzymes and ligated to the poliovirus vector pMoV 2.11 digested with the same enzymes (10). Replication-competent chimeric polioviruses were recovered by transfection of HeLa S3 cells with in vitro-transcribed RNA from recombinant cDNA clones (9).
Virus Stock.
Poliovirus recombinant stocks were produced as described previously (10). Recombinant vaccinia virus expressing Ova was a kind gift of Jonathan Yewdell, National Institutes of Health, Bethesda, MD.
Immunofluorescence.
HeLa cells were infected at low multiplicity of infection (MOI) (<1) with Polio-Ova or Polio-Sp27 obtained after two successive passages in HeLa cells. Five hours postinfection cells were fixed with 2% paraformaldehyde and subsequently stained with monoclonal mouse anti-polio 2C (kindly provided by Kurt Bienz, University of Basel, Switzerland) and polyclonal rabbit anti-Ova (Biodesign International, Kennebunkport, ME). Secondary antibodies (both horse anti-mouse IgG fluorescein isothiocyanate and goat anti-rabbit IgG Texas red) were obtained from Vector Laboratories and visualized by epi-fluorescence microscopy.
Western Blot Analysis.
Western blotting was performed essentially as described (9). Briefly, HeLa cells were infected with Polio-Ova and Polio-Sp27 recombinant polioviruses (MOI of 10) and incubated for 4, 7, and 9 hr at 37°C. Cells were harvested and lysed in buffer H (10 mM Hepes, pH 7.9/10 mM KCl/1.5 mM MgCl2/1 mM DTT/1% Triton X-100/0.1 mM phenymethylsulfonyl fluoride), and the nuclei were removed by centrifugation. Approximately 4 μg of proteins of total lysates were subjected to electrophoresis through a 12% SDS-polyacrylamide gel and analyzed by immunoblotting using antibodies directed against Ova (polyclonal rabbit anti-Ova Serum).
Cell Lines and Antigen Presentation Assay.
Construction of an EL4 cell line expressing human poliovirus receptor. A complete cDNA fragment corresponding to the human poliovirus receptor (PVR) was obtained by PCR of total HeLa cDNA using oligonucleotides 3 (5′-GCTAAGCTTTCAATTACGGCAGCTCTG-3′) and 4 (5′-GAGGTCGACCTGCTCGGAGCAACTGGCATG-3′). To construct pPVR-9, the PCR product was digested with SalI and HindIII and ligated to SalI/HindII-digested pKS 25 plasmid, which carries a 4,300-bp fragment corresponding to the murine β-actin promoter and an 880-bp fragment corresponding to the 3′ untranslated region of the murine β-actin mRNA (21). EL 4 cells (107 cells in 0.8 ml/PBS) were cotransfected by electroporation with 20 μg of plasmid pPVR-9 and 5 μg of pKO-Neo and selected in the presence of 0.5 mg/ml of G418. Cells growing were analyzed by flow cytometry in a FACSCALIBUR system (Becton Dickinson) by staining with the PVR-specific mAb D171 (a kind gift of Eckard Wimmer, State University of New York, Stony Brook) followed by fluorescein isothiocyanate-labeled goat anti-mouse IgG γ chain specific (KPL) secondary antibody.
Cell lines.
C57BL/6-derived melanoma B16F0 (15) was obtained from American Cell Culture Collection. B16-Ova (Mo5.20.10) was constructed by transfection of B16F0 with the pAc-neo-Ova plasmid as described (22, 23). RF33.70 is a C57BL/6-derived anti-Ova-Kb-specific hybridoma described previously (24). HeLa Kb B3Z, and EL4-SL8 (a kind gift from Nilabh Shastri, University of California Berkley) cells were grown in RPMI medium 1640. Cos Kb cells, transfected with sequences encoding murine H2-Kb molecule (K.L.R. unpublished work), were grown in the same media. EG-7 cells stably express ovalbumin.
Antigen Presentation Assay.
Single lacZ assay. EL-4-PVR cells were mock-infected or infected with a MOI of 40. Cells were incubated at room temperature for 20 min to allow the virus to adsorb to the cells, washed in PBS, and resuspended in media to a concentration of 5 × 105 cells/ml. One-hundred microliters of B3Z cells (5 × 105 cells/ml) were cocultured with 100 μl of poliovirus-infected cells in 96-well plates at 37°C for 24 hr. As controls, B3Z cells were incubated alone, with mock-infected EL-4-PVR cells or with 5 × 104 EL4-SL8 cells (which are stably transfected with SIINFEKL). To determine expression of β-galactosidase, cultures were washed once with PBS and fixed with cold 2% formaldehyde/0.2% glutaraldehyde for 5 min at 4°C. Cells were washed again and subsequently overlaid with 5-bromo-4-chloro-3-indolyl β-d-galactopyranoside (X-Gal) solution (1 mg/ml X-Gal, 5 mM potassium ferrocyanide, 5 mM potassium ferricyanide, and 2 mM MgCl2 in PBS). Cells were incubated at 37°C overnight and examined microscopically for the presence of blue cells the next day.
Bulk lacZ assay.
After overnight incubation with infected cells, cultures were washed once in PBS and lysed by addition of 100 μl of Z buffer (100 mM 2-mercaptoethanol/9 mM MgCl2/0.125% Triton X-100/15 mM chlorophenol red β-galactoside) (Calbiochem). After 4 hr of incubation, 50 μl of stop solution (300 mM glycine and 15 mM EDTA in water) was added, and total lacZ activity in individual cultures was determined by measuring absorption at 595 nm with 635 nm as the reference wavelength using a 96-well plate reader (SLT rainbow).
Interleukin 2 (IL-2) production by RF33.70 T cell hybridoma.
Antigen presenting cells (106) in 200 μl of Opti-mem (GIBCO) were infected for 30 min at room temperature with 10 plaque-forming units (pfu)/cell of the indicated viruses. Cells were washed once with cDMEM [DMEM (Irvine Scientific), supplemented with 10% FCS, 5 × 10−5 M 2-mercaptoethanol (Sigma), 2 mM l-glutamine, antibiotics, 0.01 M Hepes buffer (Irvine Scientific), and nonessential amino acids (Irvine Scientific)] and cultured for 16 hr at 37°C at the appropriate concentrations in 96-well plates together with 105 RF33.70 cells in a final volume of 200 μl of cDMEM. Next, 100 μl of supernatant from each well was transferred to another 96-well plate, frozen, and thawed, and 5,000 CTLL-2 cells (an IL-2-dependent cell line) in 25 μl of cDMEM were added. The plates then were cultured at 37°C for 24 hr followed by the addition of 1 μCi/well of 3H thymidine in 25 μl of cDMEM and 4-hr incubation at 37°C. Finally, the CTLL-2 cells were harvested by using a Tomtec cell harvester (Wallac, Turku, Finland), and 3H thymidine incorporation was measured by using a Microbeta counter (Wallac).
CTL Assay.
Mice and inoculations. C57BL/6 mice (H-2b) were purchased from Taconic Farms or the Jackson Laboratory and used between 6–8 weeks of age. PVR transgenic mice with a C57BL6/J × CBA1 background (H-2b/k) were obtained from American Cyanamid (a kind gift) and used between 6–8 weeks of age. For immunization groups of mice (three mice per group) were infected i.p. with 2 × 107 pfu of recombinant poliovirus or 2 × 107 pfu of recombinant Vaccinia virus in 0.2 ml of PBS and sacrificed 6–14 days later.
Restimulation and CTL assays.
Spleens from immunized mice were removed and dispersed to single cell suspensions. Splenocytes from mice of the same group were pooled, and 4 × 107 splenocytes were restimulated by cocultivation with 1.5 × 106 of mitomycin C (50 μg/ml)-treated EG7 cells in upright T25 tissue culture flasks (Becton Dickinson) in 10 ml of cRPMI medium (RPMI medium supplemented as cDMEM). Effector cells were harvested 5 days later, and cytotoxicity of CTLs was determined by 51Cr-release assay. Briefly, restimulated effector cells were harvested and cultured in 200 μl of cRPMI with 6 × 103 51Cr-labeled target cells at the indicated effector/target cell ratio for 5 hr. Percentage of specific release was calculated by using the formula [(experimental release − spontaneous release)/(maximum release − spontaneous release)] × 100, where spontaneous release is cpm obtained from targets cells cultured in media in the absence of splenocytes and maximum release targets cells lysed with 1% Triton X-100. The experiment was repeated three times, and for each experiment three mice were used per experimental group. Values represent averages of triplicate wells and variation between wells was consistently less than 5%.
Tumor Challenge.
Transgenic mice expressing the PVR (26) were infected i.p. with 100 μl of 5 × 105 pfu of the recombinant viruses in PBS solution. Mice received 2–3 booster shots of 1 × 106 of the same virus and were challenged 12 days after the last immunization. Mice were challenged by s.c. injection of 1 × 105 Ova expressing or parental B16F0 melanoma cells in 100 μl of PBS. Melanoma cells were harvested by limited trypsinization of tissue culture and washed once with PBS. More than 95% of the injected cells were viable as determined by trypan blue exclusion. For every experiment a fresh batch of tumor cells was thawed, and it was cultured in tissue culture for less than 2 weeks. The size of tumors was determined twice a week and expressed as tumor area corresponding to the largest perpendicular diameter. All experiments included five mice per group and were repeated at least three times. Mice that became moribund or had tumors >2.5 cm2 were killed.
RESULTS
Expression of Chicken Ova by Recombinant Poliovirus.
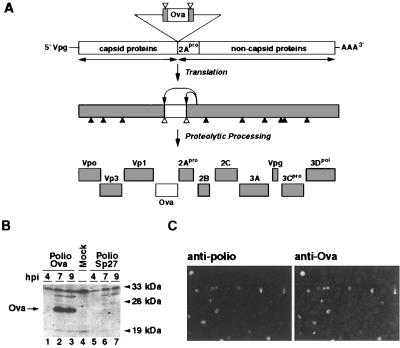
Our strategy to engineer recombinant poliovirus uses basic aspects of the viral life cycle and permits the generation of replication-competent recombinant polioviruses that are able to replicate without the need of a helper virus (3, 9, 10). Foreign sequences are inserted in-frame at different positions within the poliovirus polyprotein precursor, flanked by artificial poliovirus protease recognition sites. In this way, a larger than normal precursor initially is made, but is appropriately cleaved into the usual array of constituent proteins. The viral protease 2Apro accurately recognizes and cleaves the inserted synthetic proteolytic site, freeing the exogenous protein sequences from the rest of the poliovirus polyprotein (Fig. 1A). In this manner, all of the poliovirus proteins are correctly produced and viral replication proceeds normally.
Figure 1.
Expression and stability of recombinant poliovirus expressing Ova. (A) Schematic diagram of a recombinant poliovirus Polio-Ova and strategy for expression of Ova. The bar represents recombinant poliovirus genomic RNA. The sequence of the C-terminal half of Ova (empty bar) was inserted at the junction between the coding regions for capsid and noncapsid proteins. The Ova sequence was flanked by cleavage sites for the viral protease 2Apro. After translation, the viral polyprotein is proteolytically processed, resulting in the release of the foreign peptide and the generation of mature and functional viral proteins. ▴ indicate 3Cpro cleavage sites, ▵ represent 2Apro cleavage sites. (B) Expression of the exogenous protein in cells infected with the recombinant virus Polio-Ova. Cytoplasmic lysates from HeLa cells infected with Polio-Ova or Polio-Sp27 recombinant viruses were analyzed by Western blot with antibodies directed against Ova. Cytoplasmic lysates were prepared after 4 (lanes 1 and 5), 7 (lanes 2 and 6), and 9 hr (lanes 3 and 7) postinfection (hpi). Lanes 1–3, extracts from Polio-Ova-infected HeLa cells; lanes 5–7, Polio-Sp27-infected cells; and lane 4, mock-infected cells. Molecular weight markers indicate relative mobility. Specific bands detected by antibodies directed against the Ova are indicated by an arrow. (C) Analysis of the stability of the recombinant poliovirus Polio-Ova by immunofluorescence. HeLa cells were infected at low MOI (<1) with Polio-Ova obtained after two successive passages in HeLa cells. Five hours postinfection, cells were fixed with 2% paraformaldehyde and stained with a mAb directed against poliovirus 2C protein and a polyclonal rabbit antibody that reacts with Ova. A portion of the entire field studied is shown. More than 200 infected cells were examined to determine the proportion of revertants in the viral stock.
Polio-Ova was constructed by inserting a 600-nt sequence encoding the C-terminal half of Ova at the junction of the P1 and P2 regions of a biologically active cDNA clone (MoV-2.11) of Mahoney type 1 strain (10). The inserted fragment includes the coding sequence for SIINFEKL, an Ova epitope restricted to the murine MHC class I molecule H-2 Kb (27). Replication competent chimeric poliovirus was recovered by transfection of HeLa cells with in vitro-synthesized RNA. The virus was cloned from individual plaques and viral stocks were generated by two sequential passages in HeLa cells. At 37°C, the recombinant Polio-Ova produced plaques that were smaller than wild-type poliovirus as we have observed with previously constructed recombinant viruses (9, 10). However, Polio-Ova yielded viral titers similar to wild-type virus.
To determine whether the recombinant virus expressed the Ova fragment, HeLa cells were infected with Polio-Ova or with control virus (Polio-Sp27) carrying the coding sequence for a segment of the SIV p27 Gag protein (229 amino acids) (10). Cytoplasmic extracts were obtained at different times after infection and analyzed by immunoblotting (Fig. 1B). At 7 hr postinfection, extracts infected with Polio-Ova displayed a major polypeptide that reacted with the specific antibody directed against Ova (Fig. 1B, lanes 1–3). This polypeptide was absent in extracts from mock-infected cells or cells infected with control Polio-Sp27 (Fig. 1B, lanes 4–7). Based on molecular weight (≈20 kDa), this major polypeptide corresponds to the free C-terminal half of Ova, suggesting that proteolytic processing at the artificial cleavage site proceeds to completion.
Poliovirus exhibits a high rate of genetic variation (28), thus foreign antigenic sequences, which are dispensable for poliovirus replication, can be rapidly deleted after a few passages in tissue culture. We have extensively studied the genetic stability of different poliovirus vectors and established that the relative genetic instability of the foreign sequences is determined by both the length and the nature of the particular inserted sequence (3, 9, 10). Recently, we have found ways to improve the stability of the foreign sequences and this led to a enhancement on the ability of recombinant viruses to elicit immune responses in transgenic mice (10). To determine whether Ova sequence inserted into poliovirus are retained after a few passages in tissue culture, we examined the proportion of cells infected by individual viruses that express both poliovirus proteins and Ova by immunofluorescence. HeLa cells were infected with recombinant Polio-Ova at low MOI and double-stained with antibodies directed against the poliovirus protein 2C and Ova. More than 85% of the cells stained with both antibodies, suggesting that only a small proportion of the virus population deleted the inserted sequences after two passages in tissue culture cells. Based on these results, all further experiments presented in this paper were performed by using viral stocks obtained after two passages in HeLa cells.
Cells Infected with Polio-Ova Present the Ova-Peptide SIINFEKL in a MHC Class I-Restricted Manner.
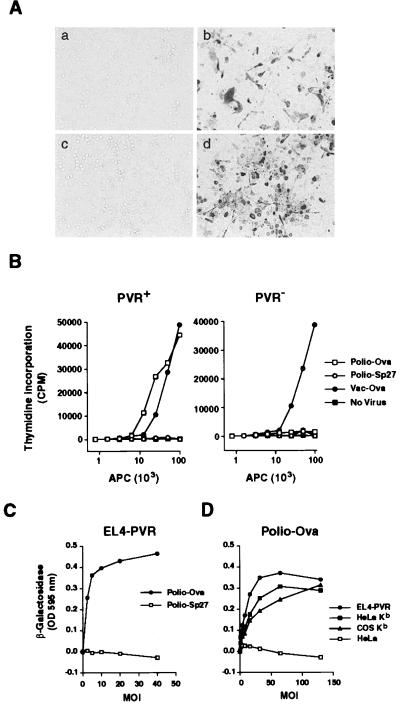
To determine whether cells infected with poliovirus are able to present antigens in a MHC class I-restricted manner, we generated a H-2 Kb murine cell line (EL4-PVR) that stably expresses the human PVR (29) and, therefore is susceptible to poliovirus infection (data not shown). Presentation of the Ova peptide SIINFEKL in the context of Kb MHC class I can be recognized by specific CD8+ T cell hybridomas (24, 30). Binding of the T cell receptor (TCR) of these hybridomas to its antigen/MHC ligand triggers a series of intracellular events that lead to functional activation of the T cell hybridomas. Two SIINFEKL-specific CD8+ T cell hybridomas were used, RF33.70, which produces IL-2 on activation (24), and B3Z, which is transfected with a lacZ reporter gene under the transcriptional control of the IL-2 enhancer element. Thus, TCR-specific stimulus in B3Z can be assessed by the production of β-galactosidase (30, 31).
EL4-PVR cells were infected with Polio-Ova and cocultivated with the hybridoma B3Z. Cells infected with Polio-Ova activated the T cell hybridoma after cocultivation (Fig. 2Ad). As a positive control, we used a EL4 cell line transfected with SIINFEKL peptide (EL4-SL8); cocultivation with this cell line also induced β-galactosidase production (Fig. 2Ab). In contrast, cocultivation of uninfected EL4-PVR cells, or the hybridoma B3Z alone, did not produce β-galactosidase activity (Fig. 2A a and c). Next, we compared MHC class I presentation of antigens expressed by poliovirus with antigens expressed by vaccinia virus, a well established recombinant virus system. EL4-PVR+, or EL4 cells, were infected with either Polio-Ova, Polio-Sp27, or vaccinia virus expressing Ova (Vac-Ova) and subsequently cocultivated with RF33.70 cells. After 24 hr, IL-2 released into the supernatant was determined by using a second indicator cell line CTLL-2. EL4-PVR cells infected with Polio-Ova presented the Ova SIINFEKL peptide with similar efficiency to cells infected with vaccinia virus. In contrast, cells infected with the control Polio-Sp27 or uninfected EL4-PVR did not stimulate the T cell hybridoma to produce IL-2. Cells that do not express PVR (parental EL4) stimulated the T cell hybridoma only when infected with Vac-Ova (Fig. 2B). In addition, stimulation of the T cell hybridoma was dependent on the dose of infectious poliovirus used as shown for B3Z stimulation (Fig. 2C).
Figure 2.
Polio-Ova infected cells present the Ova-peptide SIINFEKL in a Kb-restricted manner and activate Ova/Kb-specific T cell hybridomas. (A) CD8+ T cell hybridoma B3Z cells, which express β-galactosidase on activation, were incubated either alone (a), with 5 × 104 EL4 cells expressing SIINFEKL (EL4-SL8) (b), or with EL-4 cells expressing poliovirus receptor (EL4-PVR) either not infected (c) or infected (d) with the recombinant poliovirus Polio-Ova. After 24 hr at 37°C, cells were fixed and stained with 5-bromo-4-chloro-3-indolyl β-d-galactopyranoside. Activated lacZ+ T cells are stained, unstained lacZ− cells correspond to antigen-presenting cells and nonactivated T cell hybridomas. (B) CTLL-2 assay measuring IL-2 production by the CD8+ T-cell hybridoma RF 33.70. EL4-PVR (PVR+) or control EL4 cells (PVR−) were not infected (No Virus) or infected with Polio-Ova (Polio-Ova), Polio-Sp27 (Polio-Sp27) or vaccinia virus expressing Ova (Vac-Ova) and assay performed as described in Materials and Methods. (C) Antigen presentation is proportional to the MOI of the recombinant Polio-Ova. T cell hybridoma B3Z cells were cultured with EL4-PVR cells infected with different MOI (pfu/cell) either with Polio-Ova or Polio-Sp27 as described in A. After 20 hr of incubation, β-galactosidase activity was determined in cytoplasmic extracts of infected cells. Enzymatic activity is expressed as absorbance at 595 nm. Each point represent an average of duplicate cultures. Absorbance yielded by uninfected cells was deducted as background. (D) Ova-peptide SIINFEKL is presented by murine, human, and nonhuman primates cells on infection with Polio-Ova. EL4-PVR, HeLa Kb, COS Kb, and wild-type HeLa cells were infected with Polio-Ova at the indicated MOI and cocultured with B3Z cells. After 20 hr of incubation, β-galactosidase activity was determined as described in C.
Mechanisms used by viruses to inhibit antigen presentation can be species specific (32). Because mice are not a natural host for poliovirus it could be argued that the effect of poliovirus infection on the inhibition of the secretory pathway is specific for primates and that murine cells are not affected by poliovirus proteins. To examine this possibility we infected human (HeLa Kb) and nonhuman primate cells (Cos Kb) with Polio-Ova. These cell lines express the mouse Kb molecule, thus, antigen presentation on Polio-Ova infection can be determined by using the same T cell hybridomas and assays as described above. Both human- and monkey-derived cell lines infected with Polio-Ova were able to process and present the ovalbumin epitope SIINFEKL and to stimulate the Kb + SIINFEKL-specific T cell hybridomas in a dose-dependent manner (Fig. 2D). Furthermore, there was no significant difference in the ability to present antigen between different cell lines. These results provide evidence that poliovirus-infected cells process and present polypeptides in a MHC class I-restricted manner and stimulate CD8+ T cell hybridomas.
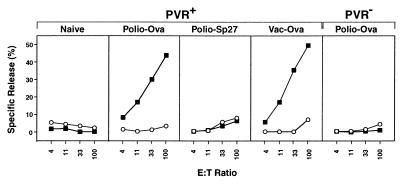
Induction of Specific CTL by Recombinant Polio-Ova.
To determine whether recombinant polioviruses are able to induce specific CD8+ CTLs, PVR-transgenic mice (26) were immunized with either Polio-Ova, Polio-Sp27, or Vaccinia-Ova (Vac-Ova) (33) as a positive control. Splenocytes obtained from Polio-Ova- and Vac-Ova-immunized mice specifically lysed the lymphoma cell line, EG7, which expresses Ova, but not the parental lymphoma EL4 (Fig. 3). In contrast, splenocytes from naive mice, or mice that were immunized with control virus Polio-Sp27, failed to lyse either target, indicating that the response was antigen specific. The CTL responses were dependent on the ability of poliovirus to infect the mice, because inoculation of Polio-Ova in PVR− animals failed to elicit any significant CTL response against Ova-expressing target cells (Fig. 3, Far Right).
Figure 3.
Immunization of poliovirus receptor-transgenic mice with the Polio-Ova recombinant poliovirus elicited a CTL response against Ova-transfected EL4 cells. PVR+ or PVR− mice were mock-infected with saline (Naive) or injected with 1 × 107 pfu of Polio-Ova, Polio-Sp27, or Vac-Ova. Animals were infected by i.p. injection with 100 μl of 1 × 108 pfu/ml of viral stock. Spleen cells from immunized mice were harvested 7 days after immunization and stimulated for 5 days with EG7 (EL4 transfected with Ova). CTL activity was determined by a standard 51Cr release assay as described in Materials and Methods.
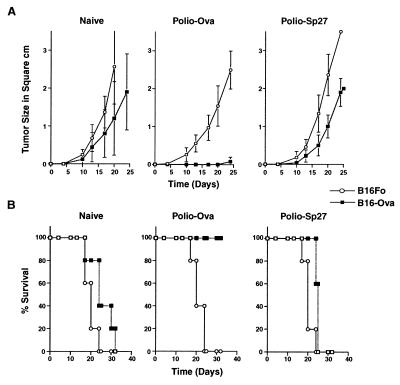
Protective Immunity in Vivo.
To investigate whether immunization with poliovirus recombinants induces protective CTL immunity we used a tumor model in which CTLs play an important role in protecting the host from experimental challenge with a lethal dose of malignant cells (22). PVR-transgenic mice were inoculated with Polio-Ova, and 2 weeks later the animals were challenged with a C57BL/6-derived melanoma, B16-Ova, which stably expresses ovalbumin (22). Subcutaneous inoculation of naive mice with B16-Ova cells or parental melanoma cells, B16, yielded tumors that grow with similar kinetics, produced metastatic foci at distant sites, and killed the animals in a few weeks (Fig. 4A). Immunization with Polio-Ova, but not with Polio-Sp27, protected animals against a challenge with a dose of B16-Ova that is 10 times the amount required to produce tumors in 50% of the animals injected. Immunization protected mice from local tumor growth (Fig. 4A) and death (Fig. 4B). This effect was specific for Ova because mice vaccinated with Polio-Ova were not protected against a challenge with parental B16 melanoma cells that do not express Ova. In addition, melanoma cell lines grew in mice inoculated with Polio-Sp27 at the same rate as in nonimmunized mice, excluding the possibility of nonspecific protection induced by poliovirus replication. Finally, no protective immunity was observed in C57BL/6 mice that do not express PVR, indicating that viral replication is required to induce an effective tumor-protective immunity (data not shown).
Figure 4.
Immunization with Polio-Ova induces protective and antigen-specific immunity to melanoma B16 expressing Ova. PVR-transgenic mice were immunized i.p. with Polio-Ova. As a control, mice were inoculated with either poliovirus Polio-Sp27 or saline (Naive). Six days after immunization (day 0) animals were challenged with 1 × 105 B16-Ova (▪) or B16 melanoma cells (○). (A) Local tumor growth. The size of the tumor was determined twice a week and is plotted as the average tumor area ± SD in square cm vs. time postchallenge (days). (B) Survival is plotted as the percentage of surviving animals vs. time. All experiments included five mice per group and were repeated at least three times.
DISCUSSION
To induce protection against diverse pathogens through vaccination, both humoral and cellular arms of the immune system may be required. Humoral immunity plays a key role in neutralizing the infectivity of extracellular pathogens and therefore is crucial for the clearance of cytopathic viruses and in prevention of reinfection. In contrast, the essential function of the CD8+ T cells in viral immunity is to kill virus-infected cells, thereby eliminating any reservoir of virus and preventing spread of the infection. We and others (3, 9, 10, 34) already have demonstrated that poliovirus vaccine vectors can effectively deliver antigens derived from other pathogens to induce both IgG and IgA, but it was not known whether a poliovirus-based vaccine could induce a CTL response. In this study, we have shown that peptides derived from proteins expressed by poliovirus vectors reach the surface of the infected cell and are presented in a MHC class I-restricted manner. In addition, vaccination of susceptible mice with replication competent poliovirus elicits an antigen-specific CTL response and protects 100% of the immunized animals from challenge with B16-Ova, a highly aggressive melanoma cell line. It has been shown previously by using a different method of vaccination, namely Ova bound to Fe-beads, that the Ova-specific CD8+ CTLs are responsible for B16 melanoma tumor rejection (22). Thus, it is likely that in the experiments described here CD8+ CTLs are also responsible for tumor protection.
Viruses have evolved mechanisms to escape T cell recognition by interfering with the mechanism of presentation of antigenic peptides in the context of MHC class I molecules on the surface of the cell. For example, the herpes simplex protein ICP47 binds the human TAP transporter, blocking the translocation of peptides from the cytosol to the endoplasmic reticulum (12, 13). Likewise, several human cytomegalovirus proteins inhibit MHC class I expression at the cell surface by blocking TAP or relocating class I molecules from the endoplasmic reticulum into the cytosol (14, 15). Also, human cytomegalovirus down-regulates HLA class I expression by reducing the stability of class I α chains (16). In addition, human cytomegalovirus US3 gene product impairs transport and maturation of MHC class I heavy chains (17). The finding that several poliovirus proteins inhibit protein secretion suggested that the virus may interfere early in infection with the antigen presentation by inhibiting the transport of the MHC class I molecules to the surface of the cell. Therefore, it was proposed that poliovirus-infected cells may escape clearance by down-regulation of MHC class I presentation (18, 19). Our data demonstrate that both murine and primates cells infected with poliovirus can efficiently present antigens in a MHC class I-restricted manner to activate primed T cells. Thus, it is likely that poliovirus-infected cells are susceptible to CD8-mediated T cell immunity in vivo and that CD8+ T cells could play a role in poliovirus pathogenesis and in the clearance of infection.
For a different picornavirus, Theiler’s virus, the outcome of infection is controlled in part by CD8+ class I-restricted CTLs. Mice infected with Theiler’s virus elicit CD8+ cytotoxic T cells specific for viral proteins. Mice in which the beta 2-microglobulin gene had been disrupted and therefore lacked CD8+ T cells fail to clear the virus, suggesting that CD8+ T cells are required for clearance of Theiler’s virus infection (35). For Coxsackievirus, another member of the picornavirus family, the situation appears to be more complex. Coxsackievirus infections previously have been shown to cause acute or chronic myocarditis, and there is evidence to suggest that myocardial injury may result from direct viral effects and/or may be immune mediated. Mice lacking CD8+ T cells showed enhanced survival and a reduced incidence of the later myocarditis. However, removal of the CD8+ T cells, although protecting against early death and later myocarditis, led to markedly increased virus titers in the heart, suggesting that CD8+ T cells also may be required to clear Coxsackievirus infection (36). The role of CD8+ T cells in poliovirus pathogenesis or immunity never has been adequately assessed and remains poorly understood. Because we discovered that infection with recombinant poliovirus induces a specific CTL response against a foreign antigen, it would be interesting to further examine whether poliovirus-specific CTLs are generated and what role they play in natural or vaccine-induced immunity in humans. Likewise, the potential role of antivirus CTL in the pathogenesis of the poliovirus-associated disease warrants study. For instance, the postpolio syndrome is characterized by recurrent neuromuscular symptoms occurring 30–40 years after the acute episode of poliomyelitis paralysis (37). Serologic and molecular techniques have provided evidence indicating that poliovirus genomes can persist for many years after the primary infection (38, 39). The presence of the poliovirus RNA genome in the cerebrospinal fluid suggests persistent viral infection in the central nervous system related to the presence of poliovirus genomes. Because neurons express little or no MHC class I molecules, it is possible that poliovirus-infected neurons are not readily eliminated by CD8+, MHC class I-restricted CTLs, thereby permitting viral persistence in the nervous system.
Antigens associated with MHC class I on any cell type can be recognized by already primed CD8+ CTL, leading to the activation of the these T cells. In contrast, only professional antigen-presenting cells (APCs) are able to prime naive T cells (40). Our results demonstrate that immunization of mice with recombinant poliovirus induces CD8+ CTL specific directed against a nonstructural protein, in this case the foreign antigen ovalbumin. How is the antigen presented within MHC class I molecules by APCs in vivo? One possibility is that poliovirus infected professional APCs such as dendritic cells or macrophages. Although macrophages express the poliovirus receptor it remains unclear whether poliovirus is able to efficiently replicate in these cells (41). Alternatively, macrophages could ingest and present antigens released by infected cells after cell lysis. Recently we and others have demonstrated MHC class I restricted presentation of exogenous proteins by macrophages (42–44), and different pathways for this presentation have been postulated cells (40). We currently are further investigating the mechanism of CTL induction by poliovirus.
It has been argued that preexisting immunity against poliovirus in the human population is a constrain for the use of poliovirus as vaccine vector. However, 50% of previously immunized individuals will show at least a 4-fold increase in antibody titers after administration of an oral polio vaccine booster (44–48). Furthermore, it is possible that at higher doses, recombinant polioviruses might be able to establish infection and elicit primary immune responses against foreign antigens in individuals previously immunized against poliovirus. In fact, it has been shown that poliovirus replicons expressing foreign antigens can induce an antibody response in previously poliovirus-vaccinated mice (49). Furthermore, a vaccine effective in immunizing children would be extremely worthwhile, and if poliovirus recombinants are effective in experimental models and in children, it would strengthen the argument to adapt other picornaviruses as vaccine vectors to overcome limitations imposed by prevailing antipolio immunity.
In summary, the results presented here begin to illuminate a poorly understood aspect of poliovirus immunology and suggest that poliovirus-based vaccines can induce both humoral and cellular immune responses specific for the inserted foreign antigen. In addition, the in vivo biology of poliovirus replication suggests that it may provide a useful vehicle for the delivery of antigens to the mucosal immune system (50–52). Thus, poliovirus vectors may provide an effective system to induce both humoral and cellular immune responses systemically and also at local mucosal sites.
Acknowledgments
We are grateful to Drs. Nilabh Shastri for B3Z, HeLa Kb, and EL4-SL8 cell lines, Kurt Bienz for anti-2C antibodies, Dina San Juan for excellent technical assistance, and Mark Feinberg and Andres McAllister for their useful comments on the manuscript. This work was supported by Public Health Service Grant AI36178 to R.A., several National Institutes of Health grants to K.L.R., and National of Institutes of Health Research Training Grant AI07394 to L.J.S.
Footnotes
This paper was submitted directly (Track II) to the Proceedings Office.
Abbreviations: CTL, cytotoxic T lymphocyte; MHC, major histocompatibility complex; Ova, chicken ovalbumin; MOI, multiplicity of infection; PVR, poliovirus receptor; pfu, plaque-forming units; IL-2, interleukin 2; FCS, fetal calf serum; GPS, l-glutamine, 1% penicillin/streptomycin.
S.M. and L.J.S. contributed equally to this work.
References
- 1.York I A, Rock K L. Annu Rev Immunol. 1996;14:369–396. doi: 10.1146/annurev.immunol.14.1.369. [DOI] [PubMed] [Google Scholar]
- 2.Rolph M S, Ramshaw I A. Curr Opin Immunol. 1997;9:517–524. doi: 10.1016/s0952-7915(97)80104-5. [DOI] [PubMed] [Google Scholar]
- 3.Andino R, Silvera D, Suggett S D, Achacoso P L, Miller C J, Baltimore D, Feinberg M B. Science. 1994;265:1448–1451. doi: 10.1126/science.8073288. [DOI] [PubMed] [Google Scholar]
- 4.Burke K L, Dunn G, Ferguson M, Minor P D, Almond J W. Nature (London) 1988;332:81–82. doi: 10.1038/332081a0. [DOI] [PubMed] [Google Scholar]
- 5.Alexander L, Lu H H, Wimmer E. Proc Natl Acad Sci USA. 1994;91:1406–1410. doi: 10.1073/pnas.91.4.1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mattion N M, Reilly P A, DiMichele S J, Crowley J C, Weeks-Levy C. J Virol. 1994;68:3925–3933. doi: 10.1128/jvi.68.6.3925-3933.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morrow, C. D., Porter, D. C., Ansardi, D. C., Moldoveanu, Z. & Fultz, P. N. (1994) Aids Res. Hum. Retroviruses10, Suppl. 2 S61–S66. [PubMed]
- 8.Melnick J L. In: Vaccines. Plotkin S A, Mortimer E A Jr, editors. Philadelphia: Saunders; 1988. pp. 115–157. [Google Scholar]
- 9.Yim T J, Tang S, Andino R. Virology. 1996;218:61–70. doi: 10.1006/viro.1996.0166. [DOI] [PubMed] [Google Scholar]
- 10.Tang S, van Rij R, Silvera D, Andino R. J Virol. 1997;71:7841–7850. doi: 10.1128/jvi.71.10.7841-7850.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kutubuddin M, Simons J, Chow M. J Virol. 1992;66:5967–5974. doi: 10.1128/jvi.66.10.5967-5974.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.York I A, Roop C, Andrews D W, Riddell S R, Graham F L, Johnson D C. Cell. 1994;77:525–535. doi: 10.1016/0092-8674(94)90215-1. [DOI] [PubMed] [Google Scholar]
- 13.Hill A, Jugovic P, York I, Russ G, Bennink J, Yewdell J, Ploegh H, Johnson D. Nature (London) 1995;375:411–415. doi: 10.1038/375411a0. [DOI] [PubMed] [Google Scholar]
- 14.Wiertz E J, Jones T R, Sun L, Bogyo M, Geuze H J, Ploegh H L. Cell. 1996;84:769–779. doi: 10.1016/s0092-8674(00)81054-5. [DOI] [PubMed] [Google Scholar]
- 15.Wiertz E J, Mukherjee S, Ploegh H L. Mol Med Today. 1997;3:116–123. doi: 10.1016/S1357-4310(96)10059-9. [DOI] [PubMed] [Google Scholar]
- 16.Beersma M F, Bijlmakers M J, Ploegh H L. J Immunol. 1993;151:4455–4464. [PubMed] [Google Scholar]
- 17.Jones T R, Wiertz E J, Sun L, Fish K N, Nelson J A, Ploegh H L. Proc Natl Acad Sci USA. 1996;93:11327–11333. doi: 10.1073/pnas.93.21.11327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Doedens J R, Kirkegaard K. EMBO J. 1995;14:894–907. doi: 10.1002/j.1460-2075.1995.tb07071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Doedens J R, Giddings T J, Kirkegaard K. J Virol. 1997;71:9054–9064. doi: 10.1128/jvi.71.12.9054-9064.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Craiu A, Akopian T, Goldberg A, Rock K L. Proc Natl Acad Sci USA. 1997;94:10850–10855. doi: 10.1073/pnas.94.20.10850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beddington R S, Morgernstern J, Land H, Hogan A. Development (Cambridge, UK) 1989;106:37–46. doi: 10.1242/dev.106.1.37. [DOI] [PubMed] [Google Scholar]
- 22.Falo L J, Kovacsovics B M, Thompson K, Rock K L. Nat Med. 1995;1:649–653. doi: 10.1038/nm0795-649. [DOI] [PubMed] [Google Scholar]
- 23.Moore M W, Carbone F R, Bevan M J. Cell. 1988;54:777–785. doi: 10.1016/s0092-8674(88)91043-4. [DOI] [PubMed] [Google Scholar]
- 24.Rock K L, Rothstein L, Gamble S. J Immunol. 1990;145:804–811. [PubMed] [Google Scholar]
- 25.Moore M W, Carbone F R, Bevan M J. Cell. 1988;54:777–785. doi: 10.1016/s0092-8674(88)91043-4. [DOI] [PubMed] [Google Scholar]
- 26.Ren R B, Costantini F, Gorgacz E J, Lee J J, Racaniello V R. Cell. 1990;63:353–362. doi: 10.1016/0092-8674(90)90168-e. [DOI] [PubMed] [Google Scholar]
- 27.Rotzschke O, Falk K, Stevanovic S, Jung G, Walden P, Rammensee H G. Eur J Immunol. 1991;21:2891–2894. doi: 10.1002/eji.1830211136. [DOI] [PubMed] [Google Scholar]
- 28.Helen C, Wimmer E. In: Human Enterovirus Infections. Rotbart H, editor. Washington, DC: Am. Soc. Microbiol.; 1995. pp. 25–72. [Google Scholar]
- 29.Mendelsohn C L, Wimmer E, Racaniello V R. Cell. 1989;56:855–865. doi: 10.1016/0092-8674(89)90690-9. [DOI] [PubMed] [Google Scholar]
- 30.Shastri N, Gonzalez F. J Immunol. 1993;150:2724–2736. [PubMed] [Google Scholar]
- 31.Karttunen J, Shastri N. Proc Natl Acad Sci USA. 1991;88:3972–3976. doi: 10.1073/pnas.88.9.3972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tomazin R, Van Schoot N E G, Goldsmith K, Jugovic P, Sempe P, Fruh K, Johnson D C. J Virol. 1998;72:2560–2563. doi: 10.1128/jvi.72.3.2560-2563.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Restifo N P, Bacik I, Irvine K R, Yewdell J W, McCabe B J, Anderson R W, Eisenlohr L C, Rosenberg S A, Bennink J R. J Immunol. 1995;154:4414–4422. [PMC free article] [PubMed] [Google Scholar]
- 34.Moldoveanu Z, Porter D C, Lu A, McPherson S, Morrow C D. Vaccine. 1995;13:1013–1022. doi: 10.1016/0264-410x(95)00018-v. [DOI] [PubMed] [Google Scholar]
- 35.Fiette L, Aubert C, Brahic M, Rossi C P. J Virol. 1993;67:589–592. doi: 10.1128/jvi.67.1.589-592.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Henke A, Huber S, Stelzner A, Whitton J L. J Virol. 1995;69:6720–6728. doi: 10.1128/jvi.69.11.6720-6728.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stone R. Science. 1994;264:909. doi: 10.1126/science.8178150. [DOI] [PubMed] [Google Scholar]
- 38.Sharief M K, Hentges R, Ciardi M. N Engl J Med. 1991;325:749–755. doi: 10.1056/NEJM199109123251101. [DOI] [PubMed] [Google Scholar]
- 39.Leparc G I, Julien J, Fuchs F, Janatova I, Aymard M, Kopecka H. J Clin Microbiol. 1996;34:2023–2026. doi: 10.1128/jcm.34.8.2023-2026.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bevan M J. J Exp Med. 1995;182:639–641. doi: 10.1084/jem.182.3.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Freistadt M S, Fleit H B, Wimmer E. Virology. 1993;195:798–803. doi: 10.1006/viro.1993.1433. [DOI] [PubMed] [Google Scholar]
- 42.Kovacsovics B M, Rock K L. Science. 1995;267:243–246. doi: 10.1126/science.7809629. [DOI] [PubMed] [Google Scholar]
- 43.Nair S, Buiting A M, Rouse R J, Van R N, Huang L, Rouse B T. Int Immunol. 1995;7:679–688. doi: 10.1093/intimm/7.4.679. [DOI] [PubMed] [Google Scholar]
- 44.Srivastava P K, Udono H, Blachere N E, Li Z. Immunogenetics. 1994;39:93–98. doi: 10.1007/BF00188611. [DOI] [PubMed] [Google Scholar]
- 45.Henry J L, Jaikaran E S, Davies J R, Tomlinson A J, Mason P J, Barnes J M, Beale A J. J Hyg. 1966;64:105–120. doi: 10.1017/s0022172400040389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Magrath D, Bainton D, Freeman M. Dev Biol Stand. 1981;47:223–226. [PubMed] [Google Scholar]
- 47.Nishio O, Ishihara Y, Sakae K, Nonomura Y, Kuno A, Yasukawa S, Inoue H, Miyamura K, Kono R. J Biol Stand. 1984;12:1–10. doi: 10.1016/s0092-1157(84)80015-3. [DOI] [PubMed] [Google Scholar]
- 48.Public Health Laboratory Service. Monthly Bull Ministry Health. 1965;24:365–369. [PubMed] [Google Scholar]
- 49.Porter D C, Wang J, Moldoveanu Z, McPherson S, Morrow C D. Vaccine. 1997;15:257–264. doi: 10.1016/s0264-410x(96)00187-9. [DOI] [PubMed] [Google Scholar]
- 50.Sicinski P, Rowinski J, Warchol J B, Jarzabek Z, Gut W, Szczygiel B, Bielecki K, Koch G. Gastroenterology. 1990;98:56–58. doi: 10.1016/0016-5085(90)91290-m. [DOI] [PubMed] [Google Scholar]
- 51.Bodian D. Science. 1955;122:105–108. doi: 10.1126/science.122.3159.105. [DOI] [PubMed] [Google Scholar]
- 52.Rueckert R R. In: Fundamental Virology. Fields B N, Knipe D M, Chanock R M, Hirsch M S, Melnick J L, Monath T P, Roizman B, editors. New York: Raven; 1991. pp. 409–450. [Google Scholar]