Abstract
CD39 is the cell surface-located prototypic member of the ecto-nucleoside triphosphate diphosphohydrolase (E-NTPDase) family. Biological actions of CD39 are a consequence (at least in part) of the regulated phosphohydrolytic activity on extracellular nucleotides. This ecto-enzymatic cascade in tandem with CD73 (ecto-5–nucleotidase) also generates adenosine and has major effects on both P2 and adenosine receptor signalling. Despite the early recognition of CD39 as a B lymphocyte activation marker, little is known of the role of CD39 in humoral or cellular immune responses. There is preliminary evidence to suggest that CD39 may impact upon antibody affinity maturation. Pericellular nucleotide/nucleoside fluxes caused by dendritic cell expressed CD39 are also involved in the recruitment, activation and polarization of naïve T cells. We have recently explored the patterns of CD39 expression and the functional role of this ecto-nucleotidase within quiescent and activated T cell subsets. Our data indicate that CD39, together with CD73, efficiently distinguishes T regulatory cells (Treg) from other resting or activated T cells in mice (and humans). Furthermore, CD39 serves as an integral component of the suppressive machinery of Treg, acting, at least in part, through the modulation of pericellular levels of adenosine. We have also shown that the coordinated regulation of CD39/CD73 expression and of the adenosine receptor A2A activates an immunoinhibitory loop that differentially regulates Th1 and Th2 responses. The in vivo relevance of this network is manifest in the phenotype of Cd39-null mice that spontaneously develop features of autoimmune diseases associated with Th1 immune deviation. These data indicate the potential of CD39 and modulated purinergic signalling in the co-ordination of immunoregulatory functions of dendritic and Treg cells. Our findings also suggest novel therapeutic strategies for immune-mediated diseases.
Keywords: Apyrase, B cells, CD39, Dendritic cells, Ecto-ATPase, E-NTPD, Immunology, Kidney, Liver, NTPDase, Platelet, T cells, Vasculature
Introduction
Our research interests have been in the purinergic modulation of vascular inflammatory and cellular immune responses in transplantation settings [1, 2]. It is generally accepted that extracellular nucleotides [e.g., ATP, uridine triphosphate (UTP), adenosine diphosphate (ADP)], and the derivative nucleosides (e.g., adenosine from ATP), are released in a regulated manner by most all cells to provide the primary components for purinergic responses [3]. High levels of ATP may be released by CD4+ and CD8+ T cells upon stimulation with Con A or anti-CD3 mAb and serve to activate cells [4]. Importantly, ATP [or uridine diphosphate (UDP)] stimulation of monocytes, lymphocytes and endothelium induces largely proinflammatory responses, such as the release of interleukin (IL)-1 (or IL-8) [4–6]. On dendritic cells (DC), exposure to extracellular ATP induces migration and differentiation to drive cellular immune responses [7]. Adenosine is also recognized as a bioactive agent in vascular inflammatory states, with effects mediated on both vascular cells and leukocytes [8]. In addition, adenosine has known anti-thrombotic effects, modulates the expression of anti-apoptotic genes and is immunosuppressive [9]. Adenosine is constitutively present in the extracellular space at low concentrations, but under metabolically stressful and hypoxic conditions, the levels rise dramatically [10]. Primary release of the mediator could occur ab initio, or this might follow conversion of released nucleotides to adenosine (see later).
The nucleotide/nucleoside mediators alluded to above bind specific purinergic receptors that comprise the second requirement for this complicated signalling network. Almost all cells carry cell-surface type 2 purinergic (P2) receptors for nucleotides and adenosine or type 1 purinergic (P1) receptors [11]. There are seven ionotropic (P2X), at least eight metabotropic (P2Y) and four adenosine receptor subtypes that have been identified and characterized to date [12]. Multiple P2X and P2Y receptor subtypes are expressed by monocytes and dendritic cells, whereas lymphocytes express only P2Y receptors [11]. These various receptors operate in both auto- and paracrine loops and are considered to play a complex, important role in the regulation of vascular and immune cell-mediated responses. Depending on the P2 or adenosine receptor subtype, the cell types and signalling pathway involved, these receptors might preferentially trigger and mediate short-term (acute) processes that affect metabolism, adhesion, activation or migration. However, purinergic signalling also has profound impacts upon other more protracted reactions, including cell proliferation, differentiation and apoptosis, such as seen in several chronic inflammatory states [12]. These mechanisms could be also implicated in immune memory [9, 13].
The third, and final, component of purinergic signalling systems comprises ecto-nucleotidases [2, 14]. These ecto-enzymes hydrolyze extracellular nucleotides to generate nucleosides that in turn activate adenosine receptors, often with opposing effects to those seen with P2-mediated effects. Within the past decade, ecto-nucleotidases belonging to several enzyme families have been discovered, cloned and functionally characterized by pharmacological means.
In this review, we will focus on CD39, the prototype of the ecto-nucleoside triphosphate diphosphohydrolase (E-NTPDase) family (EC 3.6.1.5) [15, 16]. These proteins comprise a group of ecto-enzymes that hydrolyze extracellular nucleoside tri- and diphosphates. The ecto-nucleotidase chain or cascade, as initiated by NTPDases, is terminated by ecto-5–nucleotidase (CD73; EC 3.1.3.5) [2, 17]. Together, ecto-5–nucleotidase and adenosine deaminase (ADA; EC 3.5.4.4), another ecto-enzyme that is involved in purine salvage pathways by converting adenosine to inosine, closely regulate local and pericellular extracellular concentrations of adenosine [2]. Most notably, however, in many tissues and cells, NTPDases also comprise dominant parts of a complex cell surface-located nucleotide hydrolyzing and interconverting machinery. Such ensembles also include the ecto-nucleotide pyrophosphatase phosphodiesterases (E-NPPs), NAD-glycohydrolases, CD38/NADase activity, alkaline phosphatases, diadenosine polyphosphate hydrolases, adenylate kinase, nucleoside diphosphate kinase, and potentially ecto-F1-Fo ATP synthases [2].
Many aspects of these ecto-nucleotidase families and detailed expositions of structure/function relationships of the E-NTPDases and their role in the vasculature and nervous systems have been reviewed recently. The interested reader is referred to the recent special issue of Purinergic Signalling entitled ‘Ecto-nucleotidases–(PUSI 2, 2: 2006). This review will address only the immunobiology of CD39, focusing on T lymphocytes and alluding briefly to co-expression of CD73 by immunosuppressive T cell subsets.
CD39 in the immune system
Recently, almost all of the published investigative focus on CD39 has been on the thromboregulatory properties of CD39 with respect to platelet and endothelial activation [1]. However, CD39 was first described as a B lymphocyte activation marker [18]. This ecto-nucleotidase is also expressed on natural killer (NK) cells, monocytes, DC and subsets of activated T cells [19]. The relevance of the expression of CD39 by these cells is not yet clear.
Development of mutant mice either null for Cd39 or where human CD39 has been over-expressed have provided useful models to study the role of this ecto-nucleotidase in immune responses [20, 21]. In the Cd39-null mouse [20], B cell numbers [anti-CD45RA 14.8; anti-CD22.2 (Lyb-8.20; PharMingen, San Diego CA, USA)] in unstimulated blood and spleen have been noted to be normal (not shown). Somewhat surprisingly, elicited IgG xenoantibody responses to solubilized xenoantigens administered to Cd39-null mice were found to be markedly suppressed [14]. With Dr. M. Cascalho (Mayo Clinic, Rochester, MN, USA), we have investigated whether Cd39-null mice are capable of appropriate antibody responses. We have noted that Cd39-null mice exhibit impaired B cell memory responses to T-dependent antigens. Unexpectedly, however, these mutant mice show a significant increase in the frequency of somatic mutations post-immunization (not shown). These observations suggest that CD39 function may contribute to the affinity maturation of antibody responses and to facilitate post-germinal center terminal B cell differentiation (M. Cascalho et al., manuscript in preparation).
Although CD39 has been shown to be the dominant ecto-nucleotidase expressed by NK and NK-T cells and to impact upon cytokine production ([19]; G. Beldi, unpublished), the relevance of this has not yet been fully elucidated.
CD39 is also the major NTPDase expressed by monocyte-macrophages. Upregulation of tissue factor expression by these cells in vitro and alterations in splenic macrophage populations in vivo have been observed in Cd39-null mice. P2Y receptors that are impacted upon by CD39 are critically linked to monocyte and endothelial cell responsiveness [22, 23]. P2Y receptors on monocytes could be also subject to desensitization, comparable to what we have observed in platelet P2Y1 receptors in Cd39-null mice [20]. Therefore, we were interested to observe major defects in monocycle entry and migration into the substance of Matrigel plugs injected into the subcutaneous tissue of Cd39-null mice. In parallel, we also evaluated parameters of monocyte transendothelial migration influenced by ATP in vitro and noted failure of Cd39-null cells to migrate in response to exogenous nucleotides. This defect could be overcome by co-stimulation with serotonin, suggesting a degree of P2Y receptor desensitization in Cd39-null monocytes [14, 24].
Ecto-enzymes, specifically ecto-nucleotidases, are known to play an important role in leukocyte trafficking but this complex area will not be dealt with here (for an excellent review on this topic, see [25]). However, CD39 has been recognized as a critical control point in the regulation of leukocyte accumulation within hypoxic tissues and a sixfold increase in CD39/CD73 tandem functioning in the setting of hypoxia has been demonstrated [26, 27].
Langerhans cells (LC) are members of the DC family of antigen-presenting cells residing in the skin. NTPDase1 enzymatic function on antigen presenting DC is involved in the recruitment, activation and polarization of naïve T cells. Mizumoto et al. established that LC from the Cd39-null mice do not hydrolyze ATP and ADP, unlike wild-type cells [28]. Cd39-null DC are also markedly unresponsive to ATP and are susceptible to cell death, but only after prolonged exposure to nucleotides [28].
Mutant mice null for Cd39 have amplified inflammatory responses to irritant chemicals. In these Cd39-null mice, there are major defects in dendritic cell formation, antigen presentation and T cell responses to haptens. These result in markedly attenuated responses to contact allergens in type IV hypersensitivity cutaneous responses that are also seen in inflammatory bowel disease models following haptenic stimulation (not shown).
These data suggest that Cd39 expression is required for optimal stimulation of hapten-reactive T cells in mice [28]. Somewhat paradoxically, CD39 also appears to function as an additional recognition structure on haptenated target immunocytes for HLA-A1-restricted, hapten-specific cytotoxic T cells [29]. Curiously, following deletion of Cd39, LC are fully functional with respect to homing and phenotypic maturation. However, the major defect is that these cells appear less able to stimulate T cells. These abnormalities are potentially also relevant to allograft rejection processes [14]. Sequelae of these putative immune abnormalities include the relative failure of Cd39-null mice to reject allografts under limited co-stimulation blockade [30]. These data indicate a previously unrecognized role of CD39 and the effects on nucleotide-mediated signalling in immunological responses [28].
Localization of CD39 within lipid rafts implies that this ecto-enzyme may be involved in cell-cell contacts and signalling [31]. Such membrane micro-domains serve as the ‘message center–in which numerous signalling molecules are concentrated and scaffolding developed [32]. The Cd39-null DC might exhibit defective functions because of putative defects in initiating and maintaining cell-cell contacts. This mechanism speculatively involves facilitating integrin associations by purinergic signals within the ‘immunological synapse–and would have parallels to the way chemokines have been implicated in this process [33–36]. CD39 on DC and/or T cells may be likewise translocated to the immunological synapse during antigen presentation to facilitate intercellular signalling. More typically, CD39 is considered to play a cellular immunoregulatory role by hydrolyzing ATP (and perhaps ADP) released by T cells during antigen presentation and thereby generating adenosine, a known immunosuppressive molecule.
Recent work has also indicated that regulatory CD4+ve CD25+ve T cells (Treg cells) play important roles in the suppression of immunological reactivity and maintenance of tolerance [37, 38]. Patterns of expression of CD39 by Treg and the possibility that the balance of extracellular nucleotides/nucleosides influence(s) the function of these interesting cells have been a major focus of investigation in our laboratories of late.
CD39 expression by immunosuppressive regulatory T cells
Treg are central to the acquisition of immunological tolerance. Here the immune system does not mount cellular responses against specific antigens while reactivity towards other antigens is maintained. The precise mechanisms underlying the acquisition of tolerance are not fully understood. Transplanted graft outcomes in the absence of heavy immunosuppression depend on consistent balances between cytopathic effector cells and Treg [39]. Depletion of the cytopathic T cell clone has been proposed as one mechanism for the induction of tolerance. However, it is now clear that the long-term maintenance of tolerance is also dependent on self-perpetuating immunoregulatory mechanisms that limit or constrain alloresponses. The suppressive Treg populations are considered key to the development and maintenance of peripheral tolerance [33, 40].
Significant deficiencies are apparent in identifying Treg. Although traditionally defined by CD4+CD25+ expression, the latter marker along with other membrane proteins such as GITR and CTLA4 becomes non-specific and somewhat redundant following activation. Such markers are widely upregulated on other cells thereby losing specificity for the Treg population. The forkhead winged transcription factor FoxP3 is specific for Treg; however, its intracellular location limits its usefulness in the study of this population. Moreover, it is now apparent that CD25 does not encompass all Treg as defined by FoxP3+ expression [41].
Similarly, the mechanisms of Treg action are poorly defined. Putative mechanisms of suppression by Treg include cell-to-cell contact predominant in vitro and the release of soluble mediators that may predominate in vivo. As an example, IL-10 and transforming growth factor β have been identified as soluble factors that may mediate Treg suppression. Our recent studies and data from other groups have indicated that adenosine is an important mediator generated by Treg cells, and appears responsible for, at least in part, their functions [42].
Patterns of immune expression of CD39 by Treg were determined using standard techniques; using the Cd39-null mouse cells as negative controls. CD3+, CD8+, NK1.1+, B220+, CD11b+ and CD11c+ cells were positively selected from spleens and lymph nodes of 8- to 10-week-old C57BL6 mice through the use of MACS Sort magnetic beads in MACS LS Separation columns (Miltenyi Biotec, Bergisch Gladbach, Germany). T cells enriched for CD4 were obtained from lymph node and spleen preparations using CD4 T cell columns (R&D Systems, Minneapolis, MN, USA). CD4+/CD25+ and CD4+/CD39+ were positively selected using the relevant antibody and MACS Sort magnetic beads in MACS MS Separation columns (Miltenyi Biotech, Bergisch Gladbach, Germany). Where indicated, the same subsets were also sorted after staining the purified CD4+ cells with CD25 or CD39, using the MoFlo cell sorter (BD Biosciences, San Jose, CA, USA). In selected experiments, CD4+/CD25+ cells were purified using the murine CD4+CD25+ T regulatory cell isolation kit from Miltenyi Biotech (Bergisch Gladbach, Germany). The purity of the different cell populations was verified by flow cytometry on FACSort (BD Biosciences, San Jose, CA, USA). Anti-mouse and anti-human CD4, CD8, CD19, B220, NK1.1 and CD25 were from eBiosciences (San Diego, CA, USA), as were anti-mouse CD5, CD62L, CD45RB, interferon (IFN)-γ and IL-4. Purified anti-mouse CD3 and CD28 were from PharMingen (BD Biosciences,San Diego CA, USA). Rabbit anti-mouse CD39 polyclonal antibody was used to stain cells purified from wild-type lymph nodes and from spleen, as described [43].
Using cells harvested from naïve C57BL6 mice, CD39 was found to be expressed by the majority of monocytes and by subsets of lymphocytes, also inferred by gating on forward scatter (FSC) and side scatter (SSC; not shown). Among node-derived lymphocytes, the majority of CD39+ cells are found in CD19+ (or B220+) B cells. The remaining CD39+ cells were shown to reside almost totally within the CD4+ subset (Fig. 1a). There, they consistently range from 8 to 12% of all CD4+ cells in lymph node (and spleen). Further characterization of resting C57BL6 lymphocytes revealed that CD39 is selectively expressed on CD4+/CD25+ T cells (Fig. 1a). CD39 is consistently and abundantly expressed in CD4+/CD25high T cells, while the CD4+/CD25dim populations show a dichotomic expression pattern of CD39, with ~50% of the cells positive. Less than 1% of CD39+ cells were found in the CD4+/CD25− compartment. The majority of peripheral CD4+/CD39+ cells are also CD45RBlow and mostly CD62Llow, with similar expression patterns observed in BALB/c mice (not shown).
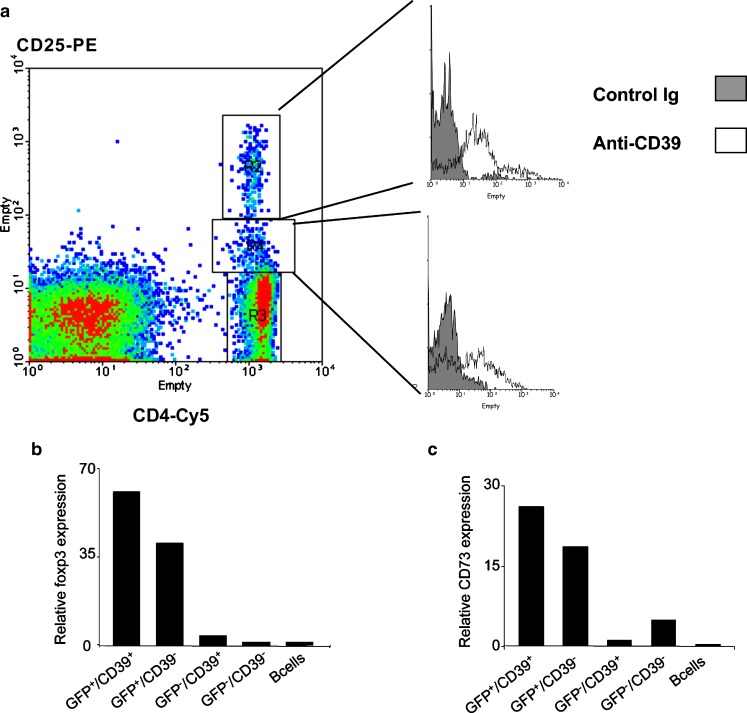
Fig. 1.
a Expression of CD39 on mouse lymphoid cells. Lymph node cell suspensions were prepared from 8-week-old C57/BL6 mice and were gated based on FSC and SSC parameters (not shown). CD4+ cells were gated based on CD25 expression. CD39 expression on the different subsets is shown in the histograms (open profiles) plotted against an irrelevant control (gray profiles). Differential expression of CD39 on CD4+ cells can be shown to be closely associated with CD25. b RT-PCR analysis of foxp3 mRNA expression. This was done in sorted cells with the following markers: Foxp3+/CD39+, Foxp3+/CD39-, Foxp3-/CD39+ and Foxp3-/CD39-. CD4+ cells obtained from the Foxp3-GFP ‘knockin–animals that had been generated by Mohamed Oukka and Vijay K. Kuchroo with colleagues (Ref). B lymphocytes were used as CD39+ control and included for comparison (striped bars). c RT-PCR analysis of CD73 mRNA expression. This was done in sorted cells with the following markers: Foxp3+/CD39+, Foxp3+/CD39-, Foxp3-/CD39+ and Foxp3-/CD39-. B lymphocytes were used as CD39+ control and included for comparison (striped bars). CD73 is also a useful immunophenotypic marker for Treg cells (not shown); and when combined with CD39 provides near-concordance with foxp3 expression. The Foxp3-/CD39+ subset does not express CD73 and these cells resemble the memory phenotype (not shown)
These results were confirmed by reverse transcription polymerase chain reaction (RT-PCR) analysis of selected cell populations. Both CD11b+ and CD11c+ cells expressed high levels of CD39 mRNA, indicating that macrophages and dendritic cells constitutively express CD39. Within the T cell compartment, the highest expression levels of CD39 transcripts were found in CD4+ cells. Gene expression profiling of CD4+ T cells, sorted on the basis of CD39 cell surface expression, indicated that the CD4+/CD39+, but not CD4+/CD39−, T cells robustly express markers of Treg cells [40], viz. Foxp3, CD25, GITR and CTLA-4. Further, CD4+/CD39+ cells are anergic in the absence of IL-2 (not shown) and suppress T effector (CD4+/CD25−) proliferation with an efficacy similar to that observed with classic CD4+/CD25+ Treg (S. Deaglio et al., submitted manuscript).
We have also confirmed the utility of CD39 in defining human Treg populations as comparable patterns of CD39 antigen expression in human cells are observed. The majority of human CD19+ B cells express CD39; however, within the T cell compartment CD39+ cells are present in the CD4+ subset (not shown). As in the mouse, CD39 is highly expressed in the CD4+/CD25high T cells, with only ~50% of cells CD39+ within the CD4+/CD25dim population. Negligible CD39 expression is found in the CD4+/CD25− population (not shown). Gene expression profiling of human CD4+/CD39+ T cells also confirms that these cells express Foxp3, GITR and CD25 in a pattern analogous to that of traditional CD4+/CD25+ Treg (K. Dwyer et al., submitted). Our analysis demonstrates that CD39 expression in both murine and human T cells is restricted to a subpopulation of CD4+/CD25+ cells that expresses markers associated with T regulatory function.
We have further examined the exact relationship between CD39 expression and the regulatory phenotype by using T cells from mutant mice with the green fluorescent protein (GFP) reporter gene introduced into the endogenous Foxp3 locus [designated as ‘Foxp3+(GFP+) knockin–cells; kindly provided for these experiments by M. Oukka and V. K. Kuchroo, Boston, MA, USA] [44]. Four populations could be defined by differential CD39 and Foxp3 expression: Foxp3+/CD39+, Foxp3+/CD39− (minor population grouping), Foxp3−/CD39+ and Foxp3−/CD39−. These populations were sorted and gene expression profiles determined. The GFP+/CD39+ fraction was shown to mirror the genetic profile of Treg, as defined by the presence of Foxp3 transcripts in this positive control (Fig. 1b). Interestingly, the next major subpopulation Foxp3–/CD39+ cells contain T lymphocytes that are not classic Treg and yet appear to be associated with the memory compartment (W. Gao, manuscript in preparation; Fig. 1b).
Foxp3+(GFP+) Treg however were also found to co-express the ecto-nucleotidase CD73, a unique situation amongst T lymphocytes (Fig. 1c). Consistent with other phenotypic data (not shown), RT-PCR analysis confirms that Foxp3+/CD39+ cells have high levels of gene expression of both CD39 and CD73 (Fig. 1b). CD73, which converts AMP to adenosine downstream of CD39, has been independently identified on CD25+ (FoxP3+) Treg and CD25− uncommitted primed precursor Th cells [42]. This recent work further supports our observations that the expression of ecto-nucleotidases and consequent adenosine generation play a role in the mediation of some of the suppressive capabilities of Treg cells. Hence, CD73 is co-expressed with CD39 as a cell surface marker of murine Tregs (Fig. 1c).
Adenosine as a Treg effector molecule
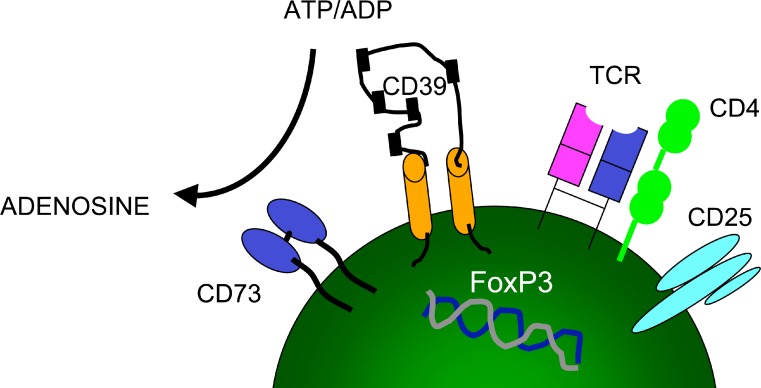
Tregs from mutant mice deficient in CD39 have impaired regulatory function manifesting as a 50% decrease in the ability of Cd39-null Tregs to modulate effector T cell function in vitro and in vivo. These results indicate that CD39 expressed by Treg is the major and rate limiting ecto-nucleotidase responsible for the generation of adenosine and suggest that a putative CD39/CD73-adenosinergic axis (i.e., generating adenosine) may contribute to the immunoregulatory function of Treg (S. Deaglio et al., manuscript submitted; also Fig. 2).
Fig. 2.
Schematic representation of Treg markers. The cellular phenotype of these suppressive T cells can be defined by FoxP3+/CD39+/CD73+ expression. Phosphohydrolysis of extracellular nucleotides by CD39 and CD73 generates adenosine, which exerts a component of the immunosuppressive effect
Adenosine plays a central and direct role in the regulation of inflammatory responses and limiting inflammatory tissue destruction [9, 10, 45]. Potentially, close cell-cell contacts with pericellular generation of adenosine and regulated expression of adenosine receptors may be important modulatory factors directly suppressing T cell responses. Early in the immune response, adenosine favors recruitment of DC, which initiates specific immune responses [9, 10, 28]. The immunosuppressive effects of adenosine on T cells are thought to be mediated primarily through the A2A receptor. Adenosine inhibits the production of proinflammatory cytokines and superoxide anions. Adenosine activation of A2A receptor also induces heterologous desensitization of chemokine receptors, which are critical in leukocyte trafficking, through the activation of protein kinase A [46].
It is also feasible that the suppression mediated via Treg-generated adenosine could be exerted indirectly through downregulation of co-stimulatory molecules on DC or by competition for other non-characterized signal molecules [47]. Irrespective of the mechanism of action, we have shown that FoxP3+ Tregs are the only T cells that contain the full enzymatic machinery necessary to generate adenosine. This effect, in conjunction with the expression of the adenosine A2A receptor on effector (CD4+/CD25−) T cells, generates immunosuppressive loops limiting effector cell proliferation both in vitro and in vivo (S. Deaglio et al., submitted).
Immune deviation and autoimmune diathesis in Cd39-null mice
The pathophysiological relevance of the CD39-adenosinergic loop was further tested by examining effects of exogenous, pharmacological adenosine A2A receptor agonists on T cells, committed to either Th1 or Th2 lineages [48]. Adenosine might contribute to the resolution of inflammation by facilitating Th2 pathways by the inhibition of Th1 cell functions [49]; this property has been addressed further in the Cd39-null mice. Subsets of naïve CD4+ T cells were polarized to a Th1 or Th2 phenotype through the addition of IL-12 (10 ng/ml) and anti-IL-4 (10 μg/ml) or IL-4 (10 ng/ml) and anti-IFN-γ (10 μg/ml), respectively, following stimulation with plate-bound anti-CD3 (5 μg/ml) and soluble anti-CD28 (2.5 μg/ml). The polarization of cells was confirmed by intracellular cytokine staining and gene profiling via RT-PCR analysis.
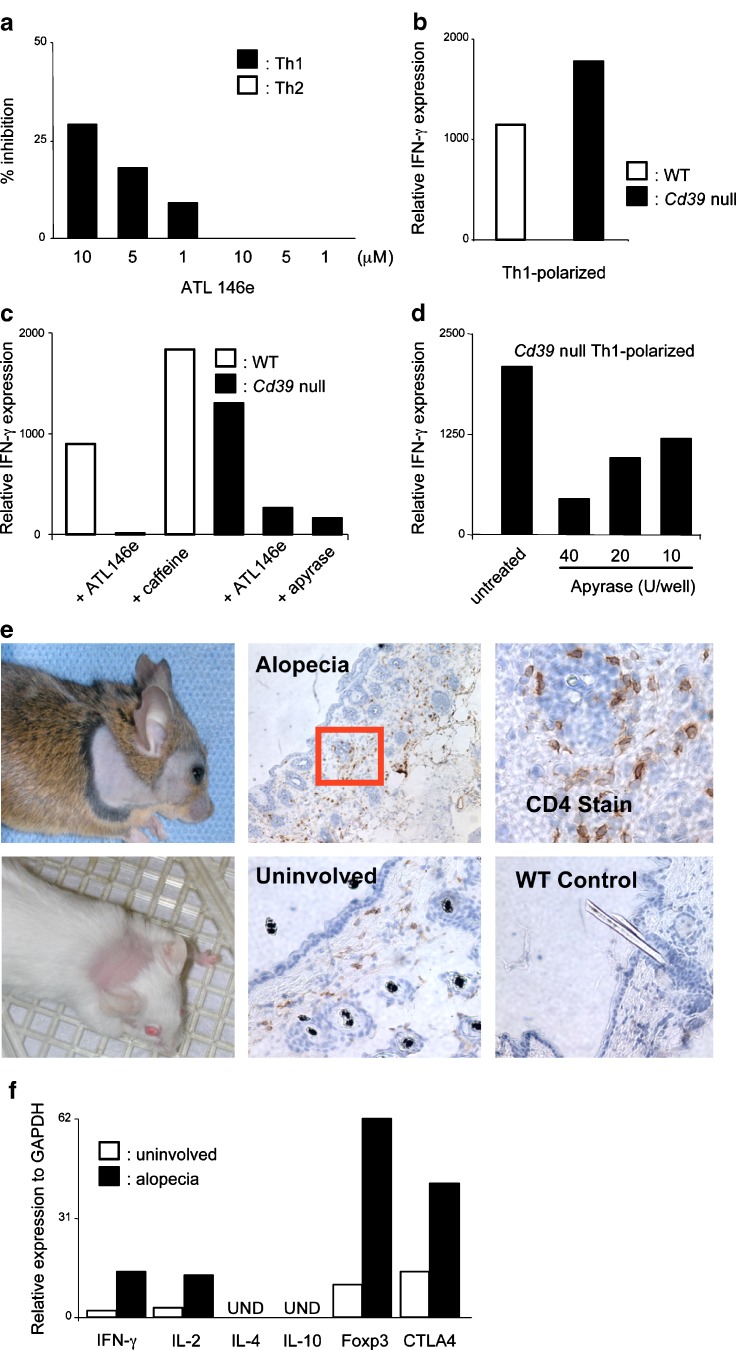
Heightened expression of the A2A receptor, as measured by RT-PCR, could be detected in CD4+/CD25− cells polarized in vitro to Th1, but not Th2, phenotypes at day 3 (not shown). In keeping with this observation, the addition of the adenosine A2A receptor agonist, ATL146e (kind gift from J. Linden, Adenosine Therapeutics), at day 3 of culture, when all cells are already committed to either a Th1 or Th2 phenotype, selectively inhibits Th1 proliferation. This suggests once more that the A2A receptor is the critical immunomodulatory adenosine receptor [9]. No inhibition of the Th2 proliferation response by ATL146e [50] could be noted (Fig. 3a).
Fig. 3.
CD39 generation of adenosine preferentially regulates Th1 immune responses. a 3H-thymidine incorporation of CD4+ T cells purified from WT mice as polarized towards a Th1 or a Th2 phenotype for 5 days. The selective adenosine A2A agonist ATL146e was added after 3 days of culture. Data are expressed as % of inhibition and are the mean of duplicates; error bars represent the SEM of three independent experiments. b CD4+ T cells were purified from Cd39-null (filled histograms) or WT (open histograms) mice and polarized towards a Th1 phenotype. The mRNA was extracted at day 3 and assayed for IFN-g (left panel) by RT-PCR. Data are representative of more than four independent experiments. c CD4+ T cells were purified from Cd39-null (filled histograms) or WT (open histograms) mice and polarized towards a Th1 phenotype. The indicated adenosine receptor agonists and antagonists were added at the beginning of the experiment (left panel). d This panel shows the effects of apyrase on IFN-g production by Cd39-null CD4+ T cells polarized towards a Th1 phenotype. For these experiments, mRNA was extracted at day 3 and assayed for IFN-g (RT-PCR). Representative data are shown from three independent experiments for each. e Representative images of Cd39-null mouse on C57BL/6/129 SVJ (upper panel) or BALB/c backgrounds (lower panel) manifesting alopecia. Histology of skin samples obtained from Cd39-null mice affected by alopecia. Uninvolved skin areas from the same animals as well as samples from WT mice were used for comparison. Biopsies were fixed and stained for CD4 cells. Original magnifications: ×10 for the upper middle panel, ×40 for the upper right and ×20 for the lower panels. f Skin samples were obtained from Cd39-null mice affected by alopecia, the tissue homogenized and mRNA extracted. Cytokine profiling was performed by RT-PCR, using a preamplification technique. Uninvolved skin from the same animal or a matched WT mouse used as controls. Representative data are from three animals
Consistent with these results, in vitro polarization of CD4+ T cells towards a Th1 phenotype results in the increased production of IFN-γ by Cd39-null T cells, with a Th1-deviated phenotype (Fig. 3b). Addition of ATL146e [50], or soluble NTPDases (apyrase), strongly inhibits the Th1 response in both the wild-type and Cd39-null polarized cells confirming that A2A receptors are present and functional in both groups. These data suggest lack of substrate in the Cd39-null cells to be responsible for the observed Th1 bias (Fig. 3c). The A2A antagonist 8-(3-chloro-styryl) caffeine was shown to augment IFN-γ production in wild-type cells polarized to a Th1 phenotype (Fig. 3c), further supporting this hypothesis. In addition, reconstitution of Cd39-null cells with apyrase restores the catalytic potential of the cells, producing adenosine and inhibiting IFN-γ production in a dose-dependent manner, effects similar to that of ATL146e (Fig. 3d).
Additional evidence that the perturbation in adenosine generation causes Th1 deviation, is that Cd39-null mice spontaneously develop autoimmune alopecia. Fifteen per cent (9/59) of designated Cd39-null animals develop skin lesions characterized by extensive and well-demarcated hair loss (Fig. 3e). No lesions are observed in age-matched WT controls (0/28). Similar lesions were observed in Cd39-null mice on the BALB/c background suggesting that the phenotype is strain independent (Fig. 3e). The alopecia typically appears at ~20–0 weeks of age in the facial region and thereafter extends out to include the trunk. The skin lesions are characterized by the presence of a population of CD4+ and CD8+ lymphocytes within the damaged hair follicles (Fig. 3e). Moreover, sixfold increases in IFN-γ transcript levels are noted in areas of skin with active disease, when compared to areas of uninvolved skin from the same animal or from wild type controls (Fig. 3f). In addition, there is increased expression of IL-2, Foxp3 and CTLA-4, consistent with the cellular infiltration. IL-4 and IL-10 were not detected (Fig. 3f). Autoimmune manifestations impacting other organ systems and on renal function are under evaluation (D. Friedman, not shown).
These data validate the importance of adenosine in directing T cell subset differentiation and support a role for CD39 in orchestrating Treg cell suppressive responses under both in vitro and in vivo conditions.
Summation
This review summarizes components of extracellular nucleotide-mediated signalling pathway in T cells that are impacted upon largely by CD39, the prototypic member of the E-NTPDase family of ecto-nucleotidases. Modulated, distinct NTPDase expression appears to regulate nucleotide- and nucleoside-mediated signalling in the immune system. As the vasculature uses similar mediators to regulate blood fluidity and hemostasis, expression of CD39 on either endothelial or immune cells might allow for full integration of vascular inflammatory and immune cell reactions at sites of injury.
There is a wide field for future investigations of the role of nucleotides, nucleosides and ecto-nucleotidases in immune-mediated diseases. Increasing interest in this field may open up new avenues for investigation and the development of new treatment modalities for a large variety of illnesses, including atherosclerosis and the vascular or immune inflammation seen in transplant-related diseases.
Acknowledgements
SCR acknowledges grant support from NIH HL57307, HL63972 and HL076540. Mutant mice with the green fluorescent protein (GFP) reporter gene introduced into the endogenous Foxp3 locus were kindly provided by M. Oukka and V. K. Kuchroo, Boston, MA, USA. ATL146e was a kind gift of J. Linden, Adenosine Therapeutics, Charlottesville, VA, USA.
Abbreviations
- ACR
apyrase conserved regions
- ATPDase
ATP diphosphohydrolase
- DC
dendritic cell
- EC
endothelial cell
- E-NTPDase
ecto-nucleoside triphosphate diphosphohydrolase
- IL
interleukin
- LC
Langerhans cells
- NPP
nucleotide pyrophosphatase/phosphodiesterase
- Treg
T regulatory cells
References
- 1.Robson SC, Wu Y, Sun X, Knosalla C, Dwyer K, Enjyoji K. Ectonucleotidases of CD39 family modulate vascular inflammation and thrombosis in transplantation. Semin Thromb Hemost. 2005;31:217–233. doi: 10.1055/s-2005-869527. [DOI] [PubMed] [Google Scholar]
- 2.Robson SC, Sevigny J, Zimmermann H. The E-NTPDase family of ectonucleotidases: structure function relationships and pathophysiological significance. Purinergic Signalling. 2006;2:409–430. doi: 10.1007/s11302-006-9003-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luthje J. Origin, metabolism and function of extracellular adenine nucleotides in the blood [published erratum appears in Klin Wochenschr (1989) 67(10):558] Klin Wochenschr. 1989;67:317–327. doi: 10.1007/BF01741386. [DOI] [PubMed] [Google Scholar]
- 4.la Sala A, Ferrari D, Di Virgilio F, Idzko M, Norgauer J, Girolomoni G. Alerting and tuning the immune response by extracellular nucleotides. J Leukoc Biol. 2003;73:339–343. doi: 10.1189/jlb.0802418. [DOI] [PubMed] [Google Scholar]
- 5.Imai M, Goepfert C, Kaczmarek E, Robson SC. CD39 modulates IL-1 release from activated endothelial cells. Biochem Biophys Res Commun. 2000;270:272–278. doi: 10.1006/bbrc.2000.2410. [DOI] [PubMed] [Google Scholar]
- 6.Warny M, Aboudola S, Robson SC, Sevigny J, Communi D, Soltoff SP, Kelly CP. P2Y(6) nucleotide receptor mediates monocyte interleukin-8 production in response to UDP or lipopolysaccharide. J Biol Chem. 2001;276:26051–26056. doi: 10.1074/jbc.M102568200. [DOI] [PubMed] [Google Scholar]
- 7.la Sala A, Ferrari D, Corinti S, Cavani A, Di Virgilio F, Girolomoni G. Extracellular ATP induces a distorted maturation of dendritic cells and inhibits their capacity to initiate Th1 responses. J Immunol. 2001;166:1611–1617. doi: 10.4049/jimmunol.166.3.1611. [DOI] [PubMed] [Google Scholar]
- 8.Ogura Y, Sutterwala FS, Flavell RA. The inflammasome: first line of the immune response to cell stress. Cell. 2006;126:659–662. doi: 10.1016/j.cell.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 9.Sitkovsky MV, Lukashev D, Apasov S, Kojima H, Koshiba M, Caldwell C, Ohta A, Thiel M. Physiological control of immune response and inflammatory tissue damage by hypoxia-inducible factors and adenosine A2A receptors. Annu Rev Immunol. 2004;22:657–682. doi: 10.1146/annurev.immunol.22.012703.104731. [DOI] [PubMed] [Google Scholar]
- 10.Sitkovsky M, Lukashev D. Regulation of immune cells by local-tissue oxygen tension: HIF1 alpha and adenosine receptors. Nat Rev Immunol. 2005;5:712–721. doi: 10.1038/nri1685. [DOI] [PubMed] [Google Scholar]
- 11.Burnstock G, Knight G. Cellular distribution and functions of P2 receptor subtypes in different systems. Int Rev Cytol. 2004;240:31–304. doi: 10.1016/S0074-7696(04)40002-3. [DOI] [PubMed] [Google Scholar]
- 12.Burnstock G. Purinergic signaling and vascular cell proliferation and death. Arterioscler Thromb Vasc Biol. 2002;22:364–373. doi: 10.1161/hq0302.105360. [DOI] [PubMed] [Google Scholar]
- 13.Koshiba M, Kojima H, Huang S, Apasov S, Sitkovsky MV. Memory of extracellular adenosine A2A purinergic receptor-mediated signaling in murine T cells. J Biol Chem. 1997;272:25881–25889. doi: 10.1074/jbc.272.41.25881. [DOI] [PubMed] [Google Scholar]
- 14.Robson SC, Enjyoji K, Goepfert C, Imai M, Kaczmarek E, Lin Y, Sevigny J, Warny M. Modulation of extracellular nucleotide-mediated signaling by CD39/nucleoside triphosphate diphosphohydrolase-1. Drug Dev Res. 2001;53:193–207. doi: 10.1002/ddr.1188. [DOI] [Google Scholar]
- 15.Kaczmarek E, Koziak K, Sevigny J, Siegel JB, Anrather J, Beaudoin AR, Bach FH, Robson SC. Identification and characterization of CD39 vascular ATP diphosphohydrolase. J Biol Chem. 1996;271:33116–33122. doi: 10.1074/jbc.271.51.33116. [DOI] [PubMed] [Google Scholar]
- 16.Zimmermann H, Braun N, Heine P, Kohring K, Sevigny J, Robson SC (2000) Molecular and functional properties of E-NTPDase-1, E-NTPDase-2 and 5–ectonucleotidase. Proceedings of the Second International Workshop on Ecto-ATPases and Related Ectonucleotidases. In: Vanduffel L (ed). Shaker Publishing BV, Maastricht, The Netherlands, pp 18–5
- 17.Resta R, Yamashita Y, Thompson LF. Ecto-enzyme and signaling functions of lymphocyte CD73. Immunol Rev. 1998;161:95–109. doi: 10.1111/j.1600-065X.1998.tb01574.x. [DOI] [PubMed] [Google Scholar]
- 18.Maliszewski CR, Delespesse GJ, Schoenborn MA, Armitage RJ, Fanslow WC, Nakajima T, Baker E, Sutherland GR, Poindexter K, Birks C, et al. The CD39 lymphoid cell activation antigen. Molecular cloning and structural characterization. J Immunol. 1994;153:3574–3583. [PubMed] [Google Scholar]
- 19.Koziak E, Sevigny J, Robson SC, Siegel JB, Kaczmarek K. Analysis of CD39/ATP diphosphohydrolase (ATPDase) expression in endothelial cells, platelets and leukocytes. Thromb Haemost. 1999;82:1538–1544. [PubMed] [Google Scholar]
- 20.Enjyoji K, Sevigny J, Lin Y, Frenette PS, Christie PD, Esch JSA, Imai M, Edelberg JM, Rayburn H, Lech M, Beeler DL, Csizmadia E, Wagner DD, Robson SC, Rosenberg RD. Targeted disruption of cd39/ATP diphosphohydrolase results in disordered hemostasis and thromboregulation. Nature Med. 1999;5:1010–1017. doi: 10.1038/12447. [DOI] [PubMed] [Google Scholar]
- 21.Dwyer KM, Robson SC, Nandurkar HH, Campbell DJ, Gock H, Murray-Segal LJ, Fisicaro N, Mysore TB, Kaczmarek E, Cowan PJ, d’Apice AJ. Thromboregulatory manifestations in human CD39 transgenic mice and the implications for thrombotic disease and transplantation. J Clin Invest. 2004;113:1440–1446. doi: 10.1172/JCI19560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaczmarek E, Erb L, Koziak K, Jarzyna R, Wink MR, Guckelberger O, Blusztajn JK, Trinkaus-Randall V, Weisman GA, Robson SC. Modulation of endothelial cell migration by extracellular nucleotides: involvement of focal adhesion kinase and phosphatidylinositol 3-kinase-mediated pathways. Thromb Haemost. 2005;93:735–742. doi: 10.1267/THRO05040735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weisman GA, Griffin K, Santiago-Perez LI, Liu J, Krugh B, Flores RV, Chorna NE, Santos-Berrios C, Vivas-Mejia PE, Garrad RC, Gonzalez FA, Erb L. P2Y(2) receptors regulate multiple signal transduction pathways in monocytic cells. Drug Dev Res. 2001;53:186–192. doi: 10.1002/ddr.1187. [DOI] [Google Scholar]
- 24.Goepfert C, Sundberg C, Sevigny J, Enjyoji K, Hoshi T, Csizmadia E, Robson S. Disordered cellular migration and angiogenesis in cd39-null mice. Circulation. 2001;104:3109–3115. doi: 10.1161/hc5001.100663. [DOI] [PubMed] [Google Scholar]
- 25.Salmi M, Jalkanen S. Cell-surface enzymes in control of leukocyte trafficking. Nat Rev Immunol. 2005;5:760–771. doi: 10.1038/nri1705. [DOI] [PubMed] [Google Scholar]
- 26.Eltzschig HK, Ibla JC, Furuta GT, Leonard MO, Jacobson KA, Enjyoji K, Robson SC, Colgan SP. Coordinated adenine nucleotide phosphohydrolysis and nucleoside signaling in posthypoxic endothelium: role of ectonucleotidases and adenosine A2B receptors. J Exp Med. 2003;198:783–796. doi: 10.1084/jem.20030891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eltzschig HK, Thompson LF, Karhausen J, Cotta RJ, Ibla JC, Robson SC, Colgan SP. Endogenous adenosine produced during hypoxia attenuates neutrophil accumulation: coordination by extracellular nucleotide metabolism. Blood. 2004;104:3986–3992. doi: 10.1182/blood-2004-06-2066. [DOI] [PubMed] [Google Scholar]
- 28.Mizumoto N, Kumamoto T, Robson SC, Sevigny J, Matsue H, Enjyoji K, Takashima A. CD39 is the dominant Langerhans cell associated ecto-NTPDase: modulatory roles in inflammation and immune responsiveness. Nature Med. 2002;8:358–365. doi: 10.1038/nm0402-358. [DOI] [PubMed] [Google Scholar]
- 29.Stockl J, Majdic O, Fischer G, Maurer D, Knapp W. Monomorphic molecules function as additional recognition structures on haptenated target cells for HLA-A1-restricted, hapten-specific CTL. J Immunol. 2001;167:2724–2733. doi: 10.4049/jimmunol.167.5.2724. [DOI] [PubMed] [Google Scholar]
- 30.Li Y, Csizmadia E, Sevigny J, Enjyoji K, Robson SC. CD39/nucleoside triphosphate diphosphohydrolase-1 (NTPDase-1) modulates allograft rejection and cellular immune responses. Am J Transplant Suppl. 2003;3:545. [Google Scholar]
- 31.Koziak K, Kaczmarek E, Kittel A, Sevigny J, Blusztajn JK, Esch JSA, Imai M, Guckelberger O, Goepfert C, Qawi I, Robson SC. Palmitoylation targets CD39/endothelial ATP diphosphohydrolase to caveolae. J Biol Chem. 2000;275:2057–2062. doi: 10.1074/jbc.275.3.2057. [DOI] [PubMed] [Google Scholar]
- 32.Shaul PW, Anderson RGW. Role of plasmalemmal caveolae in signal transduction. Am J Physiol. 1998;275:L843–L851. doi: 10.1152/ajplung.1998.275.5.L843. [DOI] [PubMed] [Google Scholar]
- 33.Dustin ML. Stop and go traffic to tune T cell responses. Immunity. 2004;21:305–314. doi: 10.1016/j.immuni.2004.08.016. [DOI] [PubMed] [Google Scholar]
- 34.Tooley AJ, Jacobelli J, Moldovan MC, Douglas A, Krummel MF. T cell synapse assembly: proteins, motors and the underlying cell biology. Semin Immunol. 2005;17:65–75. doi: 10.1016/j.smim.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 35.Friedl P, Storim J. Diversity in immune-cell interactions: states and functions of the immunological synapse. Trends Cell Biol. 2004;14:557–567. doi: 10.1016/j.tcb.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 36.Maldonado RA, Irvine DJ, Schreiber R, Glimcher LH. A role for the immunological synapse in lineage commitment of CD4 lymphocytes. Nature. 2004;431:527–532. doi: 10.1038/nature02916. [DOI] [PubMed] [Google Scholar]
- 37.Holm T, Nielsson J, Claesson M. CD4+ and CD25+ regulatory T cells: I. Phenotype and physiology. APMIS. 2004;112:629–641. doi: 10.1111/j.1600-0463.2004.apm1121001.x. [DOI] [PubMed] [Google Scholar]
- 38.Shevach EM, DiPaolo RA, Andersson J, Zhao DM, Stephens GL, Thornton AM. The lifestyle of naturally occurring CD4+ CD25+ foxp3+ regulatory T cells. Immunol Rev. 2006;212:60–73. doi: 10.1111/j.0105-2896.2006.00415.x. [DOI] [PubMed] [Google Scholar]
- 39.Stassen M, Schmitt E, Jonuleit H. Human CD4+CD25+ regulatory T cells and infectious tolerance. Transplantation. 2004;77:S23–S25. doi: 10.1097/00007890-200401151-00009. [DOI] [PubMed] [Google Scholar]
- 40.Walsh PT, Taylor DK, Turka LA. Tregs and transplantation tolerance. J Clin Invest. 2004;114:1398–1403. doi: 10.1172/JCI23238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fontenot JD, Rasmussen JP, Williams LM, Dooley JL, Farr AG, Rudensky AY. Regulatory T cell lineage specification by the forkhead transcription factor foxp3. Immunity. 2005;22:329–341. doi: 10.1016/j.immuni.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 42.Kobie JJ, Shah PR, Yang L, Rebhahn JA, Fowell DJ, Mosmann TR. T regulatory and primed uncommitted CD4 T cells express CD73, which suppresses effector CD4 T cells by converting 5–adenosine monophosphate to adenosine. J Immunol. 2006;177:6780–6786. doi: 10.4049/jimmunol.177.10.6780. [DOI] [PubMed] [Google Scholar]
- 43.Sevigny J, Sundberg C, Braun N, Guckelberger O, Csizmadia E, Qawi I, Imai M, Zimmermann H, Robson SC. Differential catalytic properties and vascular topography of murine nucleoside triphosphate diphosphohydrolase 1 (NTPDase1) and NTPDase2 have implications for thromboregulation. Blood. 2002;99:2801–2809. doi: 10.1182/blood.V99.8.2801. [DOI] [PubMed] [Google Scholar]
- 44.Bettelli E, Carrier Y, Gao W, Korn T, Strom TB, Oukka M, Weiner HL, Kuchroo VK. Reciprocal developmental pathways for the generation of pathogenic effector Th17 and regulatory T cells. Nature. 2006;441:235–238. doi: 10.1038/nature04753. [DOI] [PubMed] [Google Scholar]
- 45.Lappas CM, Day YJ, Marshall MA, Engelhard VH, Linden J. Adenosine A2A receptor activation reduces hepatic ischemia reperfusion injury by inhibiting CD1d-dependent NKT cell activation. J Exp Med. 2006;203:2639–2648. doi: 10.1084/jem.20061097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang N, Yang D, Dong H, Chen Q, Dimitrova DI, Rogers TJ, Sitkovsky M, Oppenheim JJ. Adenosine A2A receptors induce heterologous desensitization of chemokine receptors. Blood. 2006;108:38–44. doi: 10.1182/blood-2005-06-2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Takahashi T, Kuniyasu Y, Toda M, Sakaguchi N, Itoh M, Iwata M, Shimizu J, Sakaguchi S. Immunologic self-tolerance maintained by CD25+CD4+ naturally anergic and suppressive T cells: induction of autoimmune disease by breaking their anergic/suppressive state. Int Immunol. 1998;10:1969–1980. doi: 10.1093/intimm/10.12.1969. [DOI] [PubMed] [Google Scholar]
- 48.Rocken M, Shevach EM. Immune deviation-the third dimension of nondeletional T cell tolerance. Immunol Rev. 1996;149:175–194. doi: 10.1111/j.1600-065X.1996.tb00904.x. [DOI] [PubMed] [Google Scholar]
- 49.Erdmann AA, Gao ZG, Jung U, Foley J, Borenstein T, Jacobson KA, Fowler DH. Activation of Th1 and Tc1 cell adenosine A2A receptors directly inhibits IL-2 secretion in vitro and IL-2-driven expansion in vivo. Blood. 2005;105:4707–4714. doi: 10.1182/blood-2004-04-1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Linden J. Molecular approach to adenosine receptors: receptor-mediated mechanisms of tissue protection. Annu Rev Pharmacol Toxicol. 2001;41:775–787. doi: 10.1146/annurev.pharmtox.41.1.775. [DOI] [PubMed] [Google Scholar]