SYNOPSIS
Objective
We evaluated the safety of room occupants in the Tuberculosis Ultraviolet Shelter Study (TUSS), a double-blind, placebo-controlled field trial of upper-room ultraviolet germicidal irradiation (UVGI) at 14 homeless shelters in six U.S. cities from 1997 to 2004.
Methods
Data collection involved administering questionnaires regarding eye and skin irritation to a total of 3,611 staff and homeless study subjects.
Results
Among these subjects, there were 223 reports of eye or skin symptoms. During the active UV period, 95 questionnaires (6%) noted such symptoms, and during the placebo period, 92 questionnaires (6%) did so. In the 36 remaining cases, either the UV period when symptoms took place was unknown or the symptoms spanned both periods. There was no statistically significant difference in the number of reports of symptoms between the active and placebo periods. One definite instance of UV-related keratoconjunctivitis occurred, resulting from a placement of a bunk bed in a dormitory where a single bed had been used when the UV fixtures were first installed.
Conclusion
These findings demonstrate that careful application of upper-room UVGI can be achieved without an apparent increase in the incidence of the most common side effects of accidental UV overexposure.
Bench-scale and room-scale experiments clearly demonstrate the effectiveness of ultraviolet germicidal irradiation (UVGI), which consists primarily of shortwave (254 nm or UV-C) energy, for inactivating a wide range of aerosolized microorganisms.1–9 Based on these and other data, UVGI technology is widely used as a protective measure to limit the transmission of airborne pathogens. To prevent spread of infectious agents within rooms, upper room rather than UVGI within ventilation ducts is the optimal implementation mode, using wall or ceiling-mounted fixtures that direct UV-C energy above the heads of room occupants. Existing or added mechanical air mixing within rooms delivers infectious aerosols into the germicidal beam and returns disinfected air back down to the breathing zone.
However, since its introduction more than 60 years ago, the application of upper-room UVGI has raised concerns of potential injury to room occupants, specifically to eyes (photokeratoconjunctivitis) and skin (photodermatitis). This article presents findings relating to the safety of the Tuberculosis Ultraviolet Shelter Study (TUSS), a double-blind, placebo-controlled field trial of upper-room UVGI at 14 homeless shelters in six U.S. cities, from 1997 to 2004.
EFFECTS OF EXPOSURE TO GERMICIDAL UV (UV-C)
Highly active photochemically, 254 nm UV would be expected to be more damaging to exposed skin and eyes than longer wavelengths, such as UV-A and UV-B, in sunlight. However, 254 nm UV is so completely absorbed by chromophores in the outer dead layer of skin that it is estimated that only 5% of 254 nm UV at the skin surface penetrates to the top viable cell layer, compared with 15% for 365 nm (UV-A) and 50% for 297 nm (UV-B).10 Impinging radiation is also reflected and scattered by the optical properties of the skin, but while the skin is somewhat protected from germicidal UV by its absorbing dead outer layer, the cornea has no such outer layer. Consequently, the cells of the cornea have greater exposure to UV irradiation injury.
Thus, when UVGI fixtures are improperly installed or when accidental direct high-intensity exposure occurs to room occupants, for example, working without UV protection in the upper room, UV-C can result in photodermatitis and, more commonly, photokeratoconjunctivitis. Photokeratoconjunctivitis is a painful inflammation of the cellular outer layer of the cornea, which is experienced several hours after overexposure and resolves within a 24- to 48-hour period in the absence of additional exposure.11,12 Overexposure symptoms are an uncommon consequence of upper-room UGVI installation and have invariably resulted from human error, as the following case citations demonstrate.
CASE REPORTS OF ACCIDENTAL HUMAN UV-C INJURY
Before the 1985–1992 resurgence of tuberculosis (TB) in the U.S., the application of germicidal UV had greatly decreased compared with its use in the pre-antibiotic era. There exist only a few earlier reports of UV injury. These include an episode in which eight workers developed photokeratoconjunctivitis from an inadvertent 20-minute exposure to direct, high-intensity, lower-room UVGI over an operating room table, where it was being used to reduce the rate of perioperative orthopedic infections.13 In this instance, the fixture was inadvertently left on after a surgical procedure was completed, and new employees touring the operating suite were exposed. For this high-intensity lower-room application, unlike upper-room UVGI, operating room staff must wear completely protective clothing.
In another instance of human error, two nurses and a housekeeper experienced eye discomfort and facial skin peeling from exposure to a bare (unshielded) 36-watt UVGI lamp that was turned on accidentally.14 The office had previously been used as a sputum induction room, but the UVGI lamp remained functional, with a switch located next to that for the fluorescent light. At the UV intensities measured, the calculated eight-hour weighted mean threshold limit value (TLV) for 254 nm UV would be exceeded in 120 to 300 seconds. The symptoms resolved completely in two to four days.
Another episode, reported in 2006, occurred in Italy. Twenty-six medical students were exposed to a bare-bulb direct (lower-room) germicidal UV source for 90 minutes during an autopsy demonstration.15 A timer that was intended to disinfect the area at night when the suite was unoccupied had malfunctioned. All subjects reported both eye and skin symptoms. Although the calculated absorbed irradiation was approximately 700 mJ/cm2, based on meter measurements, the effective irradiance according to skin phototype and symptoms was far less—between 50 and 100 mJ/cm2. This finding supports UV monitoring data by First and colleagues that peak meter readings poorly predict actual exposure of room occupants.16 Despite UV-C exposure 20 to 100 times higher than the TLV, all but one student had complete resolution of skin symptoms within two weeks of the incident. Ocular symptoms lasted two to four days, with no residual findings.
An extreme example of such error occurred among 58 people over a nearly four-month period, when a germicidal UV lamp was accidentally used to replace a fluorescent lamp in a desk fixture in the ward of a psychiatric hospital.17 Eye symptoms and signs predominated, including pain and the sensation of a foreign body, excessive tearing, conjunctival injection, and periorbital edema. In this unusual exposure situation, room occupants were much closer to the UV source than when UVGI is used in the upper room, and UV exposure quickly exceeded the tolerable dose. The direct and reflected 254 nm UV irradiance from the fixture was measured and exceeded the eight-hour TLV in 2 to 5 minutes at a distance of 51 cm from the fixture, and 20 minutes at a distance of 173 cm.
We are aware of only one report of UV overexposure resulting from properly installed UV. During the 1985–1992 TB resurgence in New York City, Miami, and many other U.S. cities, commercial UVGI fixture designs available in the United States tended to produce excessive levels of irradiance when installed in rooms with low, UV-reflective ceilings. The human error in this case was that post-installation commissioning measurements were not taken as required before the lamps were activated in occupied rooms. Soon afterward, employees complained of eye and skin irritation that was worse during the workweek, but better over the weekends despite outdoor solar exposure. Photometry measurements confirmed eye-level UV irradiance levels as much as 10 times higher than anticipated.18 The fixtures were modified and the symptoms resolved. This experience stimulated the design of new, tightly louvered UVGI fixtures that produced a narrow beam of UV in the upper room with minimal reflection into the occupied space.19
GUIDELINES FOR UV INSTALLATION
The American Conference of Governmental Industrial Hygienists (ACGIH) Committee on Physical Agents20 has established a TLV for UV-C exposure to avoid such skin and eye injuries among those most susceptible. For 254 nm UV, this TLV is 6 mJ/cm2 over an eight-hour period. The TLV function differs by wavelengths because of variable energy and potential for cell damage. This TLV is supported by the International Commission on Non-Ionizing Radiation Protection21 and is used in setting lamp safety standards by the Illuminating Engineering Society of North America.22 When TUSS was planned, and until quite recently, this TLV was interpreted as if eye exposure in rooms was continuous over eight hours and at the highest eye-level irradiance found in the room. In those highly unlikely conditions, a 6.0 mJ/cm2 dose is reached under the ACGIH TLV after just eight hours of continuous exposure to an irradiance of 0.2 μW/cm2. Thus, 0.2 μW/cm2 was widely interpreted as the upper permissible limit of irradiance at eye height.
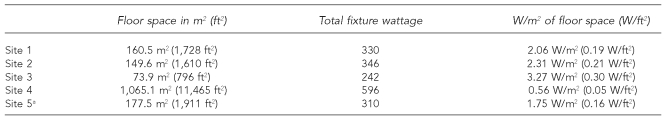
In TUSS, placement guidelines for upper-air germicidal systems followed manufacturers' recommendations developed in the 1940s, when buildings typically had floor-to-ceiling heights of more than 3 m. Studies by Riley in the 1970s provided the basis for assumed UVGI efficacy and specified one nominal 30-watt fixture for every 18.6 m2 of floor area, as long as this could be accomplished without exceeding exposure limits for safety in the lower room.23–25 As modern buildings replaced the typical pre-1940s structures, the floor-to-ceiling height decreased. Wall-mounted and open-pendant mounted UVGI fixtures thus were sited closer to room occupants. As noted, for safety, these placement guidelines specified that radiometric measurements taken at mean eye level (1.68 m) with an instrument designed and calibrated for 254 nm UV should not exceed 0.2 μW/cm2 anywhere in the room. The end result of employing these guidelines, with the diverse rooms and the variable ceiling heights found in the shelters, was a wide range of average wattage emitted per fixture per square meter of floor area, as seen in Table 1. This is because the greater reflected UV irradiance from low ceilings limited the number and UV power of the fixtures that could be installed, compared to high-ceilinged rooms.
Table 1.
Watts of UV emitted by fixtures per square meter of floor space, NYC TUSS shelters
The original Site 4 was closed partway through TUSS. The shelter moved to a new site, designated as Site 5.
UV = ultraviolet
NYC = New York City
TUSS = Tuberculosis Ultraviolet Shelter Study
W/m2 = watts per square meter
W/ft2 = watts per square foot
To test the hypothesis that peak eye-level irradiance in rooms would not predict actual UV exposure by room occupants, First et al. conducted a study in which room occupants wore a small, continuous-readout UV monitor around their necks for long durations as they performed their duties in a variety of environments with UV installations: hospital (patients and nurses), homeless shelter (staff), and a primary school (teacher).16 The results showed that all 19 room occupants registered only a small fraction (mean 9.1%, confidence interval [CI] 0.5, 37) of the irradiance extrapolated to eight hours from peak eye-level measurements. The authors of the study assumed that greater exposure was prevented by subject movement within rooms to areas with less than peak irradiance levels, by subjects turning away from the UV source, and by shielding of the portable meter during various maneuvers. While it could not mimic the unique position of the cornea and the shielding provided by facial contours, the meter's position was considered an adequate surrogate for the effect of motion and position on eye and skin exposure.
The current challenge is finding the appropriate balance between UVGI efficacy and safety. Experience has shown that peak eye-level measurements in the range of 2.0 μW/cm2 will likely result in occupant eye and skin irritation, and the aforementioned data suggest that 0.2 μW/cm2 may be overly restrictive, potentially adversely impacting germicidal efficacy, which is the purpose of such installations. As noted in the Methods section, we have been using 0.4 μW/cm2 as an arbitrary higher (but still conservative) maximum eye-level irradiance, pending additional data on occupant exposure based on time-motion studies.
METHODS
TUSS was conducted as a large-scale, double-blind, placebo-controlled field trial to determine whether upper-room UVGI could reduce TB transmission in homeless shelters.26 TUSS was carried out from 1997 to 2004 and involved the application of upper-room UVGI at 14 homeless shelters in six U.S. cities. Although the trial was inconclusive with regard to UVGI efficacy because of insufficient numbers of documented TB skin test conversions, valuable data were collected on the performance and maintenance of the UV fixtures and lamps,27 and on the side effects on room occupants of upper-room UVGI.
Prior to beginning the study or the inclusion of additional shelters during the study, approvals of research protocols were obtained from the following: the institutional review boards of St. Vincent's Hospital in New York City and the Harvard School of Public Health, Boston; review boards covering the homeless shelters in Houston, Birmingham, Alabama, and New Orleans; and review boards of any associated academic institutions. In addition, an unblinded data monitoring and safety committee regularly assessed interim results for efficacy and safety and had the power to stop the study at any time based on preestablished criteria.
System design and installation
TUSS involved the installation of more than 1,200 UVGI fixtures, covering a total of roughly 18,580 m2, in a range of highly diverse indoor spaces. The spaces were diverse because the shelters typically existed in buildings not originally designed for residential purposes, such as a factory, a school, a church basement, and rooms in transportation systems. Moreover, shelters usually served a variety of functions: they often contained crowded dormitories, lounge areas, kitchens, dining rooms, offices, chapels, clinics, bathrooms, showers, and laundries. One of the photos shows a picture of a TUSS shelter in a New York City church basement. With the exception of one facility built specifically for use as a shelter during TUSS, all UV fixtures were retrofitted. These diverse spaces presented a challenge for the effective and safe design of upper-room UVGI systems.
TUSS used a variety of fixture designs, produced by several reliable manufacturers, but in most settings, louvered wall or ceiling-mounted fixtures (Figure 2) were selected that limited lower-room irradiation to less than 0.2–0.4 μW/cm2.28 Fixtures were mounted at a height of no less than 2.13 m from the bottom of the fixture to the floor, allowing at least an additional 0.3 m above the bottom of the fixture for air disinfection to occur. To determine actual lower-room irradiance of UV systems prior to room occupancy, measurements with an International Light 1400 (IL 1400) radiometer were taken for each UV installation in a standardized fashion. The IL 1400 was equipped with an SEL240 UV-C sensor. This instrument was spectrally weighted to provide direct measurement of effective germicidal radiation using a solar blind vacuum photodiode and filters with band passes in accordance with the action spectra published by IES Luckiesh29 and DIN standards.30 Measurements were taken at a height of 1.68 m, which approximates the eye-level range for most people, assuming an average height for males in the U.S. of 1.75 m.31,32 TUSS engineers systematically measured output of UV fixtures nearby, those across the room, and those in between. This allowed detection of potential UV hot spots caused by overlapping upper-room UVGI fields.
Louvered upper-air ultraviolet germicidal irradiation in Tuberculosis Ultraviolet Shelter Study New York City shelter. Photo: ©Randall Perry Photography.
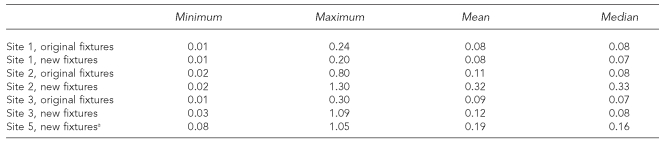
As emphasized previously, exposures for room occupants are rarely continuous for eight hours and highly unlikely to be sustained at the maximum, measured at eye level. Recognizing this, Riley recommended greater irradiance tolerances for corridors, for example, where occupants normally spend little stationary time, but which he considered important conduits for airborne pathogens within buildings.33 TUSS systems installed after 1999 were designed according to a less stringent guideline used in South Africa, which allows for irradiance at eye height of up to 0.4 μW/cm2.34 TUSS followed this practice of higher tolerance during a 2000 retrofit of the four New York City TUSS shelters in areas where occupancy was known to be brief. As Table 2 shows, readings as high as 1.3 μW/cm2 were considered acceptable. Generally, however, radiometer readings were within the 0.2–0.4 μW/cm2 range.
Table 2.
Radiometric readings at eye level of 1.68 m (shown in UV μWs), NYC TUSS shelters
The original Site 4 was closed partway through TUSS. The shelter moved to a new site, designated as Site 5.
UV = ultraviolet
NYC = New York City
TUSS = Tuberculosis Ultraviolet Shelter Study
Additional safety precautions were taken. The equipment contained switches that deactivated fixtures when opened, and the UV systems were installed on dedicated electrical circuits that could be turned off only with special keys possessed by maintenance personnel. This allowed specific UV sections to be deactivated during routine maintenance. Training was given to all shelter personnel, and bilingual notices about safety practices were placed in prominent places in each TUSS shelter to inform occupants that UV was in use.
Approximately every 12 months, the unblinded head of the data safety and monitoring committee randomly assigned each shelter to either a placebo or active UV status. Ultimately each shelter experienced both placebo and active phases, but because of this random assignment method, UV status did not necessarily alternate between active and UV periods every 12 months (e.g., a shelter could be active the first year, placebo the second and third years, and active the fourth year). Also, the duration of the active and placebo time periods was not necessarily equal within each shelter, but among all shelters the total number of shelter days was nearly equal: 10,324 shelter days were active, while 10,314 were placebo. Placebo status was achieved either by installing specially manufactured placebo lamps or by inserting a piece of glass, impenetrable to UV, in the fixture in front of the active UV lamp. By appearance, the active UV and placebo lamps were indistinguishable.
Data collection
Participation in TUSS by both shelter clients and staff involved interviews and tuberculin skin tests. The interviews were conducted in three stages. The participants were administered a Form A during their first interview, a Form B during their second interview, and a Form C in all subsequent interviews, providing a total of 8,057 Form As, 2,495 Form Bs, and 1,116 Form Cs. Each interview after a participant's first interview included questions regarding experience of eye or skin symptoms since the previous interview. While some questions were revised as the study progressed, and questions on Form Bs varied from those on Form Cs, all safety questions focused on eye and skin symptoms. Attempts were made to administer Form Bs two to six weeks after Form A, and to administer Form Cs every three months after the previous interview. Because homeless participants in TUSS were frequently absent from the shelter, considerably greater periods of time often elapsed between interviews.
RESULTS
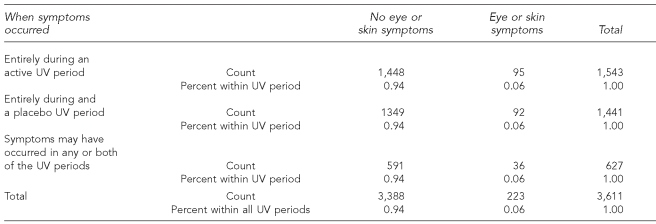
Overall, 3,611 interviews containing questions about eye and skin irritation were administered. Among these, 223 or 6% of interviews included a report of a skin or eye symptom. In most instances it was possible to determine if reports of eye or skin symptoms had been experienced entirely during a placebo or active UV period; however, because months sometimes elapsed between interviews, this was not always feasible. For example, some participants reported symptoms during interviews that occurred during a placebo period, while their previous interviews occurred in an active period. Of the 223 reports of eye or skin symptoms, 95 occurred entirely in active UV periods and 92 entirely in placebo periods. In the remaining 36 cases, the period when symptoms occurred was uncertain. Within each of the three periods, 6% of participants reported eye and/or skin symptoms. The frequency of complaints by shelter is shown in Table 3. Cross-tabulating UV status (active vs. placebo) by reports of symptoms (no report of eye or skin symptoms vs. any report of eye or skin symptoms) produces a Pearson Chi-square value of 0.066 (p=0.399, one-sided test), which is not statistically significant.
Table 3.
Frequency of reports of eye and/or skin irritation by UV status when symptoms occurred
UV = ultraviolet
Further, reports of symptoms during the active period revealed that most were unlikely to be caused by UV exposure; i.e., they included comments such as “eczema” or “bacterial infection on face.” One definite instance of UV-related keratoconjunctivitis occurred, caused by human error. The person involved occupied the upper bunk of a double bunk bed that had been placed in a dormitory where a single bed was located when the UV fixtures were first installed. This problem was resolved by moving the fixture higher on the wall.
DISCUSSION
TUSS constitutes the largest study of UV safety to date. This study also has provided a rich experience in upper-room UV application, design, engineering, acceptance, and maintenance. At the time that TUSS was planned and conducted, upper-room UV fixture designs and guidelines for their installation and monitoring had not progressed over several decades, except for the introduction of closely spaced louvers to permit their use in buildings with lower contemporary ceiling heights.19 Despite these limitations, the results showed no statistically significant difference in symptoms between the active UV and placebo periods, indicating that the installation of upper-room UVGI fixtures was achieved in a manner unlikely to compromise human safety.
TUSS data, and those from other reported studies, reveal the importance of preventative measures to avoid accidental UV exposure, especially those caused by human error. We have already noted an exposure due to the location of a bunk bed. In addition, maintenance staff at one shelter dusted fixtures while they were turned on. Fortunately, the fixtures contained placebo lamps, so no injury was sustained. But this instance highlights the importance of staff training about safety protocols to be followed when working with UV lamps.
We have argued that in TUSS the flawed application of the widely accepted UV TLV produced extremely safe, but possibly less than optimally effective, upper-room air disinfection systems. The question remains of how to design systems that achieve the goals of both safety and efficacy. Simply substituting a higher peak eye level, as was done in the later years of TUSS, was likely to have improved efficacy without compromising safety. However, this substitution did not take into account actual time-motion patterns of room occupants and may still unnecessarily limit efficacy. Monitoring additional personnel in a wider range of upper-room installations may lead to greater confidence in yet higher peak irradiance limits. More efficient fixture designs may also help. In fact, designers of new UVGI fixtures now allow wider spacing between louvers and the ability to adjust UV output electronically. This permits designers to turn down UV output initially to control excess UV, and when output later decreases with lamp usage, as expected, to turn output up again to provide a sustained flux.35 Additional progress in improved understanding of germicidal UV air moving systems has flowed from the development of a sophisticated mathematical model that takes into account microorganism susceptibility, UVGI luminaire power and location, ventilation design, air exchange rate, and vertical room air mixing in a model room.36 From this model it is clear that UV efficacy, like the efficacy of room ventilation and air filtration, varies substantially based on quantifiable factors particular to each installation, but that attention to these critical factors can result in highly effective UV systems.37
Further UVGI studies are needed to define improved design parameters for installations that are both safe and maximally effective. With a greater understanding of the application of UVGI, the full potential of this technology to improve control of person-to-person transmission of human airborne pathogens, including TB and influenza, should be realized.
Limitations
We anticipated that a substantial portion of people in the shelter at any time would not be involved in TUSS. This was because either they already had a positive tuberculin skin test and therefore would not be interviewed further, or they did not remain in the shelter long enough to be enrolled or retested. In addition, participants were not questioned regarding eye or skin symptoms during their initial interview (Form A), but rather only during the second or subsequent interviews. These factors precluded a random sampling of people interviewed regarding safety. Hence, bias may have occurred, whereby people more or less affected by UV exposure were disproportionately lost to attrition. It is possible that people who had eye or skin symptoms caused by UV exposure simply left the shelter without being interviewed, although TUSS staff was never informed of such an instance.
Another limitation of the study is that the nature of responses to questions (e.g., missing comments, unreported duration of symptoms) made it impossible in some situations to determine the etiology of the symptoms. This problem was caused partly by the occasional lengthy passage of time between interviews, which may have presented an obstacle to recollection of the specific nature of eye or skin symptoms experienced. However, this limitation applied to both control and UV exposure periods.
As noted, an inappropriately low 0.2 μW/cm2 guideline for eye-level exposure was used until 1999, after which it was increased to 0.4 μW/cm2 for the remainder of the study. As explained, this guideline was an interpretation of the well-established 6.0 mJ/cm2 TLV for 254 nm UV for eight hours of continuous exposure.
CONCLUSIONS
The threat of airborne contagion in congregate settings from pathogens as diverse as multiple drug-resistant and extreme drug-resistant TB, pandemic influenza, severe acute respiratory syndrome, and bioterrorism agents such as smallpox has never been greater. Upper-room UVGI has the potential to offer significant protection at relatively low cost, and is especially well-suited for retrofitting older buildings. Based on the results reported here, concerns regarding safety—particularly the possibility of photokeratoconjunctivitis and skin erythema from excessive UV-C exposure—should not deter application of carefully designed and maintained upper-room UVGI systems.
TUSS demonstrates that current upper-room UVGI technologies, with proper engineering, installation, and maintenance, can be placed safely in a wide range of indoor spaces, even in buildings as diverse as homeless shelters. During TUSS, accidental UV overexposure, the main cause of reported UV injury, was reported only once despite thousands of person-hours of use. Further UVGI studies are needed to define improved design parameters for installations that are both safe and maximally effective. With a greater understanding of the application of UVGI, the full potential of this technology to improve control of person-to-person transmission of human airborne pathogens in buildings should be realized.
Tuberculosis Ultraviolet Shelter Study New York City shelter in a church basement. Note the ultraviolet germicidal irradiation fixtures located on the upper wall, directly below the vents. Photo: ©Randall Perry Photography.
REFERENCES
- 1.First M, Rudnick SN, Banahan KF, Vincent RL, Brickner PW. Fundamental factors affecting upper-room ultraviolet germicidal irradiation—part I. Experimental. J Occup Environ Hyg. 2007;5:321–31. doi: 10.1080/15459620701271693. [DOI] [PubMed] [Google Scholar]
- 2.Lai KM, Burge HA, First MW. Size and UV germicidal irradiation susceptibility of Serratia marcescens when aerosolized from different suspending media. Appl Environ Mircobiol. 2004;70:2021–7. doi: 10.1128/AEM.70.4.2021-2027.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ko G, First MW, Burge HA. The characterization of upper-room ultraviolet germicidal irradiation in inactivating airborne microorganisms. Environ Health Perspect. 2002;110:95–101. doi: 10.1289/ehp.0211095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Riley RL, Knight M, Middlebrook G. Ultraviolet susceptibility of BCG and virulent tubercle bacilli. Am Rev Respir Dis. 1976;113:413–8. doi: 10.1164/arrd.1976.113.4.413. [DOI] [PubMed] [Google Scholar]
- 5.Riley RL, Permutt S, Kaufman JE. Convection, air mixing, and ultraviolet air disinfection in rooms. Arch Environ Health. 1971;22:200–7. doi: 10.1080/00039896.1971.10665833. [DOI] [PubMed] [Google Scholar]
- 6.Riley RL, Permutt S. Room air disinfection by ultraviolet irradiation of upper air. Air mixing and germicidal effectiveness. Arch Environ Health. 1971;22:208–19. doi: 10.1080/00039896.1971.10665834. [DOI] [PubMed] [Google Scholar]
- 7.Riley RL, Permutt S, Kaufman JE. Room air disinfection by ultraviolet irradiation of upper air. Further analysis of convective air exchange. Arch Environ Health. 1971;23:35–9. doi: 10.1080/00039896.1971.10665951. [DOI] [PubMed] [Google Scholar]
- 8.Xu P, Peccia J, Fabian P, Martyny JW, Fennelly KP, Hernandez M, et al. Efficacy of ultraviolet germicidal irradiation of upper-room air in inactivating airborne bacterial spores and mycobacteria in full-scale studies. Atmospheric Environment. 2003;37:405–19. [Google Scholar]
- 9.Vincent R, editor. CIE technical report. Vienna (Austria): International Commission on Illumination; 2003. CIE 155:2003 Ultraviolet air disinfection; pp. 1–64. [Google Scholar]
- 10.Bruls WA, Slaper H, van der Leun JC, Berrens L. Transmission of human epidermis and stratum corneum as a function of thickness in the ultraviolet and visible wavelengths. Photochem Photobiol. 1984;40:485–94. doi: 10.1111/j.1751-1097.1984.tb04622.x. [DOI] [PubMed] [Google Scholar]
- 11.International Commission on Non-Ionizing Radiation Protection. Guidelines on limits of exposure to ultraviolet irradiation of wavelengths between 180 nm and 400 nm (incoherent optical radiation) Health Phys. 2004;87:171–86. doi: 10.1097/00004032-200408000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Sliney DH. Ultraviolet radiation and the eye. In: Granddolfo M, Rindi A, Sliney DH, editors. Lights, lasers, and synchronous radiation: a health assessment. New York: Plenum; 1991. pp. 237–45. [Google Scholar]
- 13.Purcell JJ, Krachmer JH. Letter: hazards of ultraviolet light. N Engl J Med. 1976;294:116. doi: 10.1056/nejm197601082940226. [DOI] [PubMed] [Google Scholar]
- 14.Talbot EA, Jensen P, Moffat HJ, Wells CD. Occupational risk from ultraviolet germicidal irradiation (UVGI) lamps. Int J Tuberc Lung Dis. 2002;6:738–41. [PubMed] [Google Scholar]
- 15.Trevisan A, Piovesan S, Leonardi A, Bertocco M, Nicolosi P, Pelizzo MG, et al. Unusual high exposure to ultraviolet-C radiation. Photochem Photobiol. 2006;82:1077–9. doi: 10.1562/2005-10-27-ra-728. [DOI] [PubMed] [Google Scholar]
- 16.First MW, Weker RA, Yasui S, Nardell EA. Monitoring human exposures to upper-room germicidal ultraviolet irradiation. J Occup Environ Hyg. 2005;2:285–92. doi: 10.1080/15459620590952224. [DOI] [PubMed] [Google Scholar]
- 17.Rose RC, Parker RL. Erythema and conjunctivitis. Outbreaks caused by inadvertent exposure to ultraviolet light. JAMA. 1979;242:1155–6. doi: 10.1001/jama.242.11.1155. [DOI] [PubMed] [Google Scholar]
- 18.Moss C, Seitz TA. Ultraviolet radiation exposure to health care workers from germicidal lamps. Appl Occup Environ Hyg. 1991;6:168–70. [Google Scholar]
- 19.Nardell E, Riley RL. A new ultraviolet germicidal irradiation (UVGI) fixture design for upper room air disinfection with low ceilings. Bethesda (MD): World Congress on Tuberculosis; 1992. Abstract and conference proceedings. [Google Scholar]
- 20.American Conference of Governmental Industrial Hygienists. TLVs and BEIs. Cincinnati: ACGIH; 1999. [Google Scholar]
- 21.International Commission on Non-Ionizing Radiation Protection. Guidelines on UV radiation exposure limits. Health Phys. 1996;71:978. [PubMed] [Google Scholar]
- 22.Illuminating Engineering Society of North America. RP-27.2-00. IESNA Photobiology Committee. Recommended practice for photobiological safety for lamps and lamp systems—measurement systems, techniques. New York: IESNA; 2000. [Google Scholar]
- 23.Martin A, Morcillo N, Lemus D, Montoro E, Telles MA, Simboli N, et al. Multicenter study of MTT and resazurin assays for testing susceptibility to first-line anti-tuberculosis drugs. Int J Tuberc Lung Dis. 2005;9:901–6. [PubMed] [Google Scholar]
- 24.First MW, Nardell EA, Chaisson WT, Riley RL. Guidelines for the application of upper-room ultraviolet germicidal irradiation for preventing transmission of airborne contagion—part II: design and operational guidance. ASHRAE Transactions. 1999;105:869–76. [Google Scholar]
- 25.First MW, Nardell EA, Chaisson WT, Riley RL. Guidelines for the application of upper-room ultraviolet germicidal irradiation for preventing transmission of airborne contagion—part I: basic principles. ASHRAE Transactions. 1999;105:877–87. [Google Scholar]
- 26.Brickner PW, Vincent RL, Nardell EA, Pilek C, Chaisson WT, First MW, et al. Ultraviolet upper room air disinfection for tuberculosis control: an epidemiological trial. J Healthcare Saf Compliance – Inf Control. 2000;4:123–31. [Google Scholar]
- 27.First MW, Banahan KF, Dumyahn TS. Performance of ultraviolet germicidal irradiation lamps and luminaires in long-term service. Leukos. 2007;3:181–8. [Google Scholar]
- 28.Dumyahn T, First MW. Characterization of ultraviolet upper room air disinfection devices. American Industrial Hygiene Association Journal. 1999;60:219–27. [Google Scholar]
- 29.Rea MS, editor. Illuminating Engineering Society of North America. IESNA lighting handbook. 9th edition. New York: IESNA; 2000. pp. 5–17. [Google Scholar]
- 30.DIN 5031. Berlin: Deutsches Institut für Normung e.V.; 1979. Strahlungsphysik im optichen Bereich und Lichttechnik. [Google Scholar]
- 31.Dreyfuss H. Humanscale 1/2/3. Cambridge (MA): MIT Press; 1974. [Google Scholar]
- 32.Molarius A, Kuulasmaa K, Sans S. Quality assessment of weight and height measurements in the WHO MONICA Project. Geneva: World Health Organization; 1998. [Google Scholar]
- 33.Riley RL, Kaufman JE. Air disinfection in corridors by upper air irradiation with ultraviolet. Arch Environ Health. 1971;22:551–3. doi: 10.1080/00039896.1971.10665899. [DOI] [PubMed] [Google Scholar]
- 34.Coker I, Nardell EA, Fourie B, Brickner PW, Parsons S, Bhagwandin N, et al. Guidelines for the utilisation of ultraviolet germicidal irradiation (UVGI) technology in controlling the transmission of tuberculosis in health care facilities in South Africa. Pretoria (South Africa): South African Centre for Essential Community Services and National Tuberculosis Research Programme, Medical Research Council; 2001. pp. 1–40. [Google Scholar]
- 35.Boyce P. Controlling tuberculosis transmission with ultraviolet irradiation. In: Delta, editor. Lighting Research Center. Troy (NY): Rensselaer Polytechnic Institute; 2003. [Google Scholar]
- 36.Rudnick SN, First MW. Fundamental factors affecting upper-room germicidal irradiation—part II. Predicting effectiveness. J Occup Environ Hyg. 2007;4:352–62. doi: 10.1080/15459620701298167. [DOI] [PubMed] [Google Scholar]
- 37.Miller SL, Fennelly K, Hernandez M. Efficacy of ultraviolet irradiation in controlling the spread of tuberculosis. Atlanta: Centers for Disease Control and Prevention (US); 2002. [Google Scholar]