Abstract
Background
Although the vast majority of respiratory tract symptoms are self-limiting, many patients visit their GP for these symptoms and antibiotics are overprescribed.
Aim
To explore determinants of patients visiting GPs for recent cough, sore throat, or earache; for being prescribed antibiotics; and for patients' satisfaction with visiting the GP.
Design of the study
Second Dutch National Survey of General Practice (DNSGP-2) with a health interview and an additional questionnaire.
Setting
A total of 7057 adult patients of 163 GPs in the Netherlands.
Method
Characteristics of patients and GPs as well as morbidity data were derived from the DNSGP-2 and a health interview. Characteristics of the symptoms, GPs' management and patients' satisfaction were measured by an additional written questionnaire. Data were analysed by means of multivariate logistic regression.
Results
About 40% of the responders (n = 1083) reported cough, sore throat, or earache in the 2 weeks preceding the interview and, of them, 250 visited their GP. Of this latter group, 97 patients were prescribed antibiotics. Apart from non-medical reasons, relevant medical factors played an important role in deciding to visit the GP. Smokers and patients with cardiac disease or diabetes mellitus were not especially inclined to see their GP. Smoking behaviour, fever, and views on respiratory tract symptoms and antibiotics of patients and GPs were associated with being prescribed antibiotics. Patients' perception of having been carefully examined was associated with their satisfaction, while receiving antibiotics was not.
Conclusion
GPs should inform patients with clear elevated risk when to visit their GP in cases of cough, sore throat, or earache. There is still a need for GPs and patients to be better informed about the limited significance of single inflammation signs (for example, fever and green phlegm) as an indication for antibiotics. Careful examination of the patient contributes to patient satisfaction.
Keywords: antibiotics, general practice, respiratory tract infections, satisfaction, views
INTRODUCTION
Respiratory tract symptoms such as cough, sore throat, and earache are among the most frequent reasons to see a GP. It has been estimated that only one to three of every 10 patients with an episode of respiratory tract symptoms consults a GP,1,2 the so-called ‘iceberg phenomenon’.3,4 The vast majority of these symptoms are self-limiting and require only symptomatic treatment to relieve symptoms, while antibiotics shorten the duration of these symptoms only modestly, if at all.
Patients require medical help only when they have an elevated risk for complications, or in the case of serious alarm symptoms (for example, shortness of breath, coughing up blood, and great difficulty in swallowing).4,5 In daily practice antibiotics are frequently prescribed, and often overprescribed in most western countries, even in a relatively ‘low prescribing’ country like the Netherlands.6 Negative consequences of over-prescribing are unnecessary expenditure, the increase of patients' dependence on doctors, risk of side effects, and development of antimicrobial resistant bacteria.7
To improve disease management and, more specifically, antibiotic use in frequent disease entities such as respiratory tract infections, it is important that two things are known. First, it is necessary to have up-to-date information about the illness behaviour of patients. It is well known that specific groups of patients are more inclined to visit their GP (for example, older patients, those who perceive their health as moderate to poor, who perceive their illness as serious, who perceive more benefits in consulting a GP, or who are urged by others to visit their GP).8 However, up-to-date information is warranted, since consultation rates for respiratory tract episodes have fallen in the last decade,9–11 and national guidelines for respiratory tract infections have been published in the last 15 years.12
How this fits in
Previous studies have shown that older patients and those who are worried are more inclined to visit their GP for respiratory tract infections. Antibiotics are too often prescribed for these infections with many GPs assuming that prescribing these antibiotics will increase patients' satisfaction. Apart from non-medical reasons, relevant medical factors play an important role in deciding to visit the GP, although some high-risk groups are not especially inclined to see their GP. GP-related determinants are not associated with patients' decision to visit their GP. Both patients' and GPs' views on respiratory tract symptoms and antibiotics are associated with antibiotic prescribing for cough, sore throat, and earache. Careful examination of patients contributes to their satisfaction.
Second, successful interventions to improve antibiotic use in respiratory tract infections should be based on valid information on the prescription behaviour of GPs. Several GP characteristics are known to be associated with antibiotic prescribing rates for respiratory tract symptoms (for example, years of practice, medical knowledge, placing too much emphasis on inflammation signs like purulent sputum, and the tendency to label respiratory tract episodes as infections rather than as symptoms).13–15 However, it is also known that patients' views and expectations related to respiratory tract symptoms and antibiotics do influence antibiotic prescribing.16–17 GPs often perceive patients to expect antibiotics for respiratory tract symptoms and assume that prescribing these antibiotics will increase patients' satisfaction, which may be only true for those patients who expect to be prescribed antibiotics.16–18
Exploration of patients' and GP characteristics is important for assessing their mutual role as determinants of visiting the GP, being prescribed antibiotics, and patients' satisfaction with visiting their GP for respiratory tract symptoms. The role of patients' and GPs' characteristics have yet to be examined together in relation to the same respiratory tract episode. This study aims to explore current GP- and patient-related determinants of visiting a GP, and of antibiotic treatment and patients' satisfaction with visiting their GP for acute cough, sore throat, and earache.
METHOD
The Second Dutch National Survey of General Practice
The data used in this study were derived from the Second Dutch National Survey of General Practice (DNSGP-2), carried out by the Netherlands Institute for Health Services Research in 2001.19 Data were used from 163 GPs in 85 practices serving a population of 359 625 patients. The patients enlisted in the participating practices were comparable to the general Dutch population with respect to age, sex, and type of healthcare insurance. Participating GPs did not differ from the general population of Dutch GPs, except for type of practice; single-handed GPs were somewhat under-represented in the study population. The 2001 study is assumed to provide a representative impression of morbidity and prescribing habits in Dutch general practice.18
Patients, symptoms, and GP visits
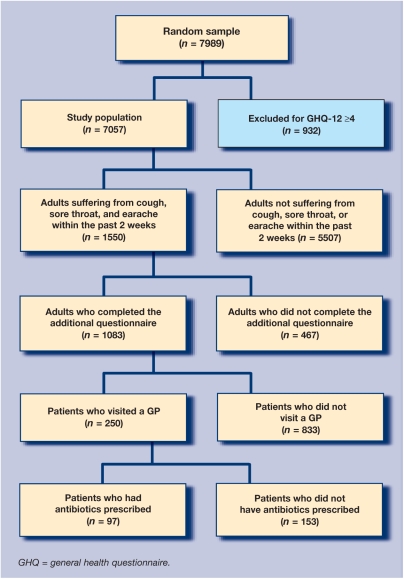
A random sample of 7989 adults (aged 18–96 years) drawn from the practice population participated in a health interview survey (Figure 1). The survey took place at the patients' homes and included items addressing personal characteristics: sex, age, level of education (primary school or less/beyond primary school); smoking behaviour (no/yes); type of insurance (public/private insurance); self-reported health (moderate to poor/[very] good); chronic respiratory comorbidity (asthma, chronic obstructive pulmonary disease and/or emphysema; no/yes); other comorbidity (diabetes mellitus, cardiovascular diseases, and/or hypertension; no/yes); and suffering from cough, sore throat, or earache in the 2 weeks preceding the interview (no/yes). Patients with a high score for psychiatric disturbance (GHQ-12 score of 4, n = 932) were excluded because of their participation in a separate study on mental illness in the DNSGP-2,20 leaving 7057 patients.
Figure 1.
Flow chart of GP visits and antibiotic prescription.
In total, 1550 patients (22%) reported recent respiratory tract symptoms. During the interview, these patients were invited to complete an additional questionnaire with items relating recent symptoms: duration ≥2 weeks (no/yes); presence of fever (no/yes); perceived seriousness (5-point scale; 1 = very low to 5 = very high), whether they were urged by others to visit a GP (no/yes); and whether they had used over-the-counter medication. Patients rated their endorsement on views on respiratory tract symptoms and antibiotics (relating to seriousness, self-limiting character) need to consult a GP if symptoms lasted for a longer period, need of antibiotics in cases of fever, white spots in the throat, or green phlegm, effectiveness of antibiotics, and the side effects of antibiotics, on a 5-point scale ranging from 1 (strongly disagree) to 5 (strongly agree).21 Patients were also asked whether they visited their GP for these symptoms (no/yes); and if so, they were asked about their experience of the consultation in terms of: listening carefully (no/yes); examining carefully (no/yes); giving advice and information (no/yes); and prescribing antibiotics (no/yes). Finally, they were asked whether they were satisfied with this visit (not [quite]/yes).
GP characteristics
All GPs completed a questionnaire containing items related to their personal characteristics: age and sex, degree of urbanisation (rural/urban); single-handed practice (no/yes); frequency of consulting national GP guidelines in general (once a week or less/more than once a week); seeing pharmaceutical representatives in the last 4 weeks (no/yes); and self-rated inclination to prescribe new drugs (1 = low to 5 = high). Similar to the patients, GPs rated their endorsement on views on respiratory tract symptoms and antibiotics.
Outcome measures
Outcome measures were: (a) symptoms of cough, sore throat, or earache in the past 2 weeks (no/yes) for the study population; (b) visiting a GP for cough, sore throat, or earache (no/yes) for adults with these symptoms within the past 2 weeks; (c) having antibiotics prescribed (no/yes); and (d) satisfaction with the visit to the GP (not [quite]/yes).
Analysis
To describe independent associations between patient and GP-related characteristics and outcome measures, multivariate logistic regression analyses were carried out (P<0.05). Age, sex, and characteristics correlating with outcome measures with P<0.20 were included for patients and for GPs, with checks for interaction and colinearity carried out (P<0.05). Data were analysed using SPSS (version 12.0.1). As cluster effects of general practices were likely for visiting a GP, antibiotic prescribing, and satisfaction, Generalized Estimating Equations (GEE by SAS system for Windows version 8) was applied for these latter analyses (P<0.05).
RESULTS
Study population, responders and GPs
Table 1 presents data on patient characteristics. Around 20% of the study population were aged 65 years and over, and more than half were female. In total, 1550 of these 7057 patients (22%) reported recent respiratory tract symptoms (Figure 1). Of these, 1059 reported cough, 664 sore throat, and 224 reported earache, with many patients experiencing a combination of these symptoms. An additional questionnaire was returned by 1083 patients (response rate: 70%). There was no difference between responders and non-responders regarding their characteristics and recent respiratory tract symptoms except that non-responders were more likely to smoke than responders (44 and 34%, respectively; difference = 10%; 95% confidence interval [CI] = 5 to 16%). Table 2 presents data on participating GPs: mean age was 47 years, 25% were female, 62% practised in a rural area, and 25% had a single-handed practice.
Table 1.
Patient characteristics (n = 7057), %.
| Age (≥65 years) | 20.6 |
| Sex (female) | 53.8 |
| Level of education (low education) | 34.3 |
| Smoker | 29.5 |
| Type of insurance (publicly insured) | 65.5 |
| Chronic respiratory comorbidity | 7.4 |
| Other comorbiditya | 19.7 |
| Self-reported health (moderate to poor) | 14.7 |
Cardiovascular disease, diabetes mellitus, and/or hypertension
Table 2.
GP characteristics (n = 163).
| Age, mean (SD) | 47.1 (6.4) |
| Female sex, % | 26.4 |
| Degree of urbanisation, % | |
| Rural | 62.0 |
| Urban | 38.0 |
| Single-handed practice, % | 24.5 |
| Consulting national guidelines for GPs, % | |
| Once a week or less | 46.0 |
| More than once a week | 54.0 |
| Seeing pharmaceutical representatives, % yes | 56.4 |
| Higher inclination to prescribe new drugs, mean (SD)a | 2.4 (0.7) |
| Views on respiratory tract symptoms and antibiotics, mean (SD)b | |
| Seriousness | 2.0 (0.8) |
| Self-limiting character | 4.3 (0.6) |
| Need to consult a GP | 3.5 (0.8) |
| Need of antibiotics in cases of fever | 1.7 (0.7) |
| Need of antibiotics in cases of green phlegm | 1.7 (0.7) |
| Need of antibiotics in cases of white spots in the throat | 2.3 (1.1) |
| Effectiveness of antibiotics | 1.9 (0.8) |
| Side-effects of antibiotics | 3.7 (1.0) |
Scale ranged as follows: 1 (very reticent) to 5 (high inclination).
Scale ranged as follows: 1 (strongly disagree) to 5 (strongly agree). SD = standard deviation.
Suffering from respiratory tract symptoms and visiting the GP
Around 40% of the responding patients (n = 1083) reported symptoms lasting longer than 2 weeks, and 12% reported fever. Being female, aged younger than 65 years, reporting health as moderate to poor, smoking, and having chronic respiratory comorbidity were independent risk factors for suffering from cough, sore throat, or earache in the last 2 weeks.
Over-the-counter medication was used by 50% of the patients (mainly antitussives, paracetamol, and homeopathic preparations) and 12% were urged by others (for example, family members) to visit a GP. Around a quarter of those with symptoms visited the GP for recent symptoms (Figure 1): 24% of the patients with cough, 19% of the patients with sore throat, and 29% of the patients with earache. Six patient characteristics were independent determinants of visiting the GP: being aged 65 years and over, respiratory comorbidity, suffering from reported symptoms for more than 2 weeks, being urged by others to visit a GP, reporting serious symptoms, and low endorsement of the perception that respiratory tract symptoms are self-limiting (Table 3). Having other comorbidity (such as diabetes or a cardiovascular disease) was not associated with patients' illness behaviour, neither were GP-related determinants.
Table 3.
Final models for risk factors of experiencing cough, sore throat, and earache and determinants of visiting the GP for these symptoms, being prescribed antibiotics, and satisfaction with the visit (multilevel) multivariate logistic regression analysis; adjusted odds ratio (95% CI).
| Symptoms (n = 7057) | Visiting the GP (n = 1083) | Prescribed antibiotics (n = 250) | Satisfaction (n = 250) | |
|---|---|---|---|---|
| Female | 1.3 (1.1 to 1.4)a | 1.1 (0.8 to 1.6)a | 1.5 (0.8 to 3.0)a | 1.4 (0.7 to 2.7)a |
| Aged ≥65 years | 0.8 (0.7 to 0.9) | 1.8 (1.2 to 2.7) | 0.8 (0.3 to 2.1)a | 1.5 (0.7 to 3.5)a |
| Reporting own health as moderate to poor | 1.7 (1.5 to 2.0) | — | — | — |
| Smoker | 1.5 (1.4 to 1.7) | — | 2.8 (1.3 to 6.0) | — |
| Chronic respiratory comorbidity | 2.2 (1.8 to 2.7) | 2.2 (1.3 to 3.6) | — | — |
| Duration of the symptoms if more than 2 weeks | 6.3 (4.2 to 9.4) | — | — | |
| Presence of fever | — | 6.7 (2.2 to 19.1) | — | |
| Urged by others to visit a GP | 16.0 (7.8 to 32.8) | — | — | |
| Endorsing the seriousness of the reported symptoms | 1.8 (1.5 to 2.2) | — | 0.7 (0.5 to 0.9) | |
| Endorsing the need of antibiotics in cases of green phlegm | 1.8 (1.3 to 2.4) | — | — | |
| Endorsing the self-limiting character of respiratory tract symptoms | 0.6 (0.5 to 0.8) | — | — | |
| Concern about side-effects of antibiotics | — | 0.6 (0.5 to 0.9) | — | |
| Being carefully examined by the GP | — | — | 4.1 (2.1 to 8.2) | |
| GPs' endorsement of the effectiveness of antibiotics | — | 1.5 (1.0 to 2.1) | 1.9 (1.2 to 2.9) | |
| GPs' endorsement of the need for antibiotics in cases of white spots in the throat | — | 1.6 (1.1 to 2.2) | — | |
— indicates not applied in the final model (not significant in the regression analysis)
Difference not significant in the final model.
Table 4.
Data on all patients, patients with and without recent symptoms (cough, sore throat, or earache), who did/did not visit their GP for these symptoms, who were/were not prescribed antibiotics and who were/were not satisfied.
| Patients with recent symptoms (n = 1083) | Patients visiting their GP (n = 250) | Patients not visiting their GP (n = 833) | Prescribed antibiotics (n = 97) | Not prescribed antibiotics (n = 153) | Satisfied (n = 188) | Not (quite) satisfied (n = 59) | |
|---|---|---|---|---|---|---|---|
| Personal characteristics, % | |||||||
| Aged ≥65 years | 17.7 | 28.0 | 14.6 | 27.8 | 28.1 | 29.8 | 20.3 |
| Female sex | 57.6 | 55.6 | 58.2 | 55.7 | 55.6 | 54.8 | 59.3 |
| Level of education (low education) | 32.2 | 43.2 | 28.9 | 46.4 | 41.2 | 44.7 | 39.0 |
| Smoker | 33.5 | 30.0 | 34.3 | 39.2 | 24.2 | 30.9 | 27.1 |
| Type of insurance (publicly insured) | 66.8 | 70.4 | 65.7 | 71.1 | 69.9 | 69.1 | 72.9 |
| Chronic respiratory comorbidity | 13.4 | 27.6 | 9.1 | 33.0 | 24.2 | 28.2 | 25.4 |
| Other comorbiditya | 19.5 | 26.0 | 17.5 | 26.8 | 25.5 | 25.0 | 30.5 |
| Self-reported health (moderate to poor) | 28.1 | 13.2 | 32.6 | 8.2 | 16.3 | 13.8 | 11.9 |
| Characteristics of the recent respiratory tract symptoms, % | |||||||
| Duration of the reported symptoms ≥2 weeks | 38.4 | 77.6 | 26.0 | 73.9 | 79.9 | 73.4 | 78.0 |
| Fever present during the reported symptoms | 11.9 | 18.8 | 9.8 | 35.1 | 8.5 | 18.6 | 20.3 |
| Urged by others to visit a GP | 11.7 | 40.8 | 3.0 | 46.4 | 37.3 | 41.5 | 39.0 |
| Perceived seriousness of the symptoms, mean (SD)b | 2.1 (1.1) | 2.8 (1.1) | 1.8 (0.9) | 3.0 (1.1) | 2.7 (1.0) | 2.7 (1.1) | 3.0 (1.1) |
| Over-the-counter medication | 50.8 | 43.6 | 52.9 | 51.5 | 38.6 | 41.5 | 52.5 |
| Views on respiratory tract symptoms and antibiotics, mean (SD)c | |||||||
| Seriousness | 3.2 (0.9) | 3.5 (1.0) | 3.2 (0.9) | 3.6 (1.0) | 3.4 (1.0) | 3.5 (1.0) | 3.4 (0.9) |
| Self-limiting character | 3.3 (0.7) | 3.1 (0.8) | 3.4 (0.7) | 3.1 (0.8) | 3.1 (0.8) | 3.1 (0.8) | 3.0 (0.8) |
| Need to consult a GP | 3.8 (0.6) | 4.0 (0.5) | 3.8 (0.6) | 4.0 (0.6) | 4.0 (0.5) | 4.0 (0.5) | 3.8 (0.6) |
| Need of antibiotics in cases of fever | 3.1 (1.0) | 3.4 (1.1) | 3.0 (1.0) | 3.5 (1.0) | 3.2 (1.2) | 3.4 (1.1) | 3.2 (1.1) |
| Need of antibiotics in cases of green phlegm | 3.1 (1.3) | 3.4 (1.3) | 3.0 (1.3) | 3.8 (1.1) | 3.1 (1.3) | 3.4 (1.3) | 3.3 (1.2) |
| Need of antibiotics in cases of white spots in the throat | 3.7 (1.1) | 3.9 (1.1) | 3.7 (1.1) | - | - | - | - |
| Effectiveness of antibiotics | 3.6 (0.9) | 3.6 (0.9) | 3.5 (0.9) | 3.8 (0.9) | 3.5 (0.8) | 3.6 (0.9) | 3.5 (0.9) |
| Side effects of antibiotics | 3.1 (1.0) | 3.0 (1.0) | 3.2 (1.0) | 2.8 (1.0) | 3.1 (1.0) | 3.0 (1.0) | 2.9 (0.9) |
| Aspects of GPs' management, % yes | |||||||
| GP listened carefully | - | - | - | 79.4 | 75.2 | 78.7 | 72.9 |
| GP examined carefully | - | - | - | 62.9 | 52.9 | 63.3 | 37.3 |
| GP gave information and advice | - | - | - | 55.7 | 43.1 | 48.4 | 49.2 |
| GP prescribed antibiotics | - | - | - | 100 | 0 | 41.0 | 33.9 |
| Satisfaction with GPs' visit | - | - | - | 79.4 | 73.8 | 100 | 0 |
Cardiovascular disease, diabetes mellitus and/or hypertension.
Scale ranged from: 1 (very low) to 5 (very high).
Scale ranged from: 1 (strongly disagree) to 5 (strongly agree).
Receiving antibiotics and patient satisfaction
Most patients reported that their GP carefully listened to their complaints, over 50% reported that their GP carefully examined them, and around 50%, reported that their GP gave information and advice. Forty per cent of patients reported that their GP prescribed antibiotics.
Six patient characteristics were independently associated with being prescribed antibiotics: smoking, having a fever, endorsing the need of antibiotics in cases of green phlegm, having a GP who reported a stronger endorsement of the effectiveness of antibiotics in cases of respiratory tract symptoms, and having a GP who endorsed the need for antibiotics in cases of white spots in the throat. These factors made it more likely that antibiotics would be prescribed (Table 3). Patients who were more concerned about the side effects of antibiotics were less likely to be prescribed them.
Almost 75% of those who visited the GP were satisfied with their visit. Three factors were independently associated with patients' satisfaction with their visit to the GP: patients who perceived their recent symptoms as more serious were less likely to be satisfied with their visit to the GP, while patients who reported that they were carefully examined by the GP and whose GP reported a stronger endorsement of the effectiveness of antibiotics were more likely to be satisfied (Table 3). Being prescribed antibiotics was not independently associated with patients' satisfaction.
No interaction or colinearity was found between the determinants in any of the regression analyses.
DISCUSSION
One in five responders suffered from acute respiratory symptoms 2 weeks prior to the study. Of these, one in four contacted the GP. Relevant medical factors (for example, age, duration of symptoms, and comorbidity) played an important role in deciding to visit the GP. No GP-related determinants were associated with the patients' decision to visit their GP was an unexpected finding.
Concerning antibiotic treatment, perceptions and beliefs of both patients and GPs regarding effects and side effects of antibiotics were independently associated with having antibiotics prescribed for cough, sore throat, or earache. Interestingly, patients who reported careful examination by the GP, and whose GP more strongly endorsed the effectiveness of antibiotics in cases of respiratory tract symptoms were more likely to be satisfied with their visit to the GP.
Strength and weaknesses of the study
Patients' characteristics in the DNSGP–2 sample were comparable with those of the general Dutch population;19 responders' characteristics did not differ from non-responders except for smoking behaviour. Therefore, the results of the present study can be assumed to represent morbidity in daily primary care and patients' illness behaviour in the Netherlands. However, some points need to be taken into consideration.
Information about visiting a GP was obtained by means of patients' self-reports with a recall period of 2 weeks. Close inspection of GPs' electronic records showed that for most patients who reported visiting a GP this contact was registered (82%); this percentage is similar to the data of children in the first DNSGP.22 While electronic records are not completely reliable (as not all visits may be registered by every GP) and the recall period was rather short, it was assumed the patients' reports were an adequate source to assess GP visits.24 However, the number of GP visits measured in this study may be slightly underestimated, as patients with a high risk of psychiatric disturbance were excluded. Those at high risk of psychiatric disturbance reported more symptoms in the past 2 weeks than the study population (30% and 22%, respectively; difference = 8%; 95% CI = 4 to 10%). Smokers were under-represented in the patients responding to the additional questionnaire, but it was assumed that this difference did not bias the results, as smoking behaviour was not associated with visiting a GP.
The frequency of consulting national guidelines and the inclination to prescribe new drugs were obtained by self-reporting by GPs. However, both ratings were assumed to be correct and, while these factors refer to concrete behaviour and it has been shown that the former factor was negatively associated with a higher volume of actual prescriptions of second-choice (mostly newer) antibiotics, the latter was positively associated.15 Finally, it should be pointed out that the study had a cross-sectional design and partially a retrospective design, so associations can only be assumed while causal relationships cannot be reported on.
Comparison with existing literature
Smokers and patients with chronic respiratory comorbidity suffered more frequently from cough, sore throat, and earache than non-smokers and patients without chronic respiratory comorbidity. These latter findings correspond with earlier studies.24,25 Of those patients reporting recent cough, sore throat, or earache, around 25% visited the GP. For children higher visiting rates have been found.2
The finding that being female, aged over 65 years, having chronic respiratory comorbidity, higher perceived severity, longer duration, less endorsement of the self-limiting character, and being urged by other persons, were related to a visit to the GP are consistent with previous and recent studies.8,26–28 The finding that personal characteristics (sex and level of education) and having diabetes mellitus or a cardiovascular disease were not correlated with visiting a GP, were also consistent with the findings of these earlier studies. Therefore, it can be concluded that the main determinants of this kind of illness behaviour have not changed in the last decade, despite the fall in incidence of presented respiratory tract symptoms and the publication of national guidelines for respiratory tract infections.
In the current study, 39% of those visiting a GP reported being prescribed antibiotics; this percentage is comparable with other Dutch studies.13,29 The finding that fever was independently associated with being prescribed antibiotics is also in accordance with other studies.29,30 Patients' perceived need of antibiotics in cases of green phlegm was independently associated with receiving antibiotics. This finding may corroborate similar findings in other studies that have shown that patients' perceived need of antibiotics is a strong predictor of GPs' antibiotic prescribing.16,17,31
In contrast to the expectations based on the findings in another Dutch study,12 number of years since registration as GP was not independently correlated with having antibiotics prescribed. Differences in study population (national versus the middle region of the Netherlands) and outcome measure (being prescribed antibiotics in a recent respiratory tract episode versus prescription rates over a 3-week period in the winter), could account for these differences. Careful examination was independently associated with patient's satisfaction with their visit to the GP. Until now, no other studies have examined the relation between history taking, physical examination, and patients' satisfaction. Receiving antibiotics was not related to patients' satisfaction which is partly consistent with other studies.16,18,32
Although patients and GPs are known to differ in their views on respiratory tract symptoms and antibiotics,21 this study found no association between the differences in views between patients and their respective GPs, visiting the GP for respiratory tract symptoms, being prescribed antibiotics, or being satisfied with the visit to the GP.
Implications for clinical practice and future research
Most patients with recent cough, sore throat, or earache do not visit a GP, but those who do often have good reasons for doing so. Factors related to a higher risk for complications include: older age, respiratory comorbidity, and long duration of symptoms.33,34 However, some high-risk groups such as smokers and patients with cardiac disease or diabetes are not especially inclined to see their GP. While more research is needed on the prognosis of respiratory tract infections in primary care to determine which subgroups of patients should in fact be treated and monitored, patients with clear elevated risks such as those with cardiac failure, should nonetheless be informed when to contact their GP.
Fever appeared to be the most important independent determinant for having antibiotics prescribed, despite the fact that fever itself is not necessarily an indication to prescribe antibiotics. GPs still need to be reminded that there is hardly any evidence that single signs of inflammation (for example, fever, and white spots in the throat) are an indication to prescribe antibiotics, and should prescribe non-antibiotic drugs to relieve the symptoms.4,5
Patients' endorsement of the need of antibiotics was related to having them prescribed. However, antibiotic prescribing was not related to patients' satisfaction, in contrast to careful physical examination of patients. It seems important that GPs explore patients' expectations and understand that patients seem to be ready to accept to a ‘wait-and-see-policy’ in many cases. This finding applies not only to the Netherlands, but also to countries with comparable primary care characteristics.
Acknowledgments
We would like to thank Peter Zuithoff for his statistical assistance.
Ethics committee
This study was carried out according to Dutch legislation on privacy
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Van der Linden MW, Westert GP, de Bakker DH, Schellevis FG. Tweede nationale studie naar ziekten en verrichtingen in de huisartsenpraktijk: klachten en aandoeningen in de bevolking en in de huisartspraktijk. Utrecht/Bilthoven: NIVEL/RIVM; 2004. [Second Dutch national survey on morbidity and interventions in general practice: complaints and diseases in the population and in general practice; in Dutch] [Google Scholar]
- 2.Bruijnzeels MA, Foets M, van der Wouden JC, van den Heuvel WJA. Everyday symptoms in childhood: occurrence and general practitioner consultation rates. Br J Gen Pract. 1998;48(426):880–884. [PMC free article] [PubMed] [Google Scholar]
- 3.Last JM. The iceberg: completing the clinical picture in general practice. Lancet. 1963;ii:28–31. doi: 10.1093/ije/dyt113. [DOI] [PubMed] [Google Scholar]
- 4.Arroll B. Antibiotics for upper respiratory tract infections: an overview of Cochrane reviews. Respir Med. 2005;99(3):255–261. doi: 10.1016/j.rmed.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 5.Smucny J, Fahey T, Becker L, Glazier R. Antibiotics for acute bronchitis. Cochrane Database Syst Rev. 2004;(4) doi: 10.1002/14651858.CD000245.pub2. CD000245. [DOI] [PubMed] [Google Scholar]
- 6.Akkerman AE, Kuyvenhoven MM, van der Wouden JC, Verheij TJM. Determinants of antibiotics overprescribing in respiratory tract infections in general practice. J Antimicrob Chemother. 2005;56(5):930–936. doi: 10.1093/jac/dki283. [DOI] [PubMed] [Google Scholar]
- 7.Wise R. The relentless rise of resistance? J Antimicrob Chemother. 2004;54(2):306–310. doi: 10.1093/jac/dkh340. [DOI] [PubMed] [Google Scholar]
- 8.McKinlay JB. Some approaches and problems in the study of the use of services — an overview. J Health Soc Behav. 1972;13(2):115–152. [PubMed] [Google Scholar]
- 9.Ashworth M, Charlton J, Ballard K, et al. Variations in antibiotic prescribing and consultation rates for acute respiratory infection in UK general practices 1995-2000. Br J Gen Pract. 2005;55(517):603–608. [PMC free article] [PubMed] [Google Scholar]
- 10.Fleming DM, Ross AM, Cross KW, Kendall H. The reducing incidence of respiratory tract infection and its relation to antibiotic prescribing. Br J Gen Pract. 2003;53(495):778–783. [PMC free article] [PubMed] [Google Scholar]
- 11.Hak E, Rovers MM, Kuyvenhoven MM, et al. Incidence of GP-diagnosed respiratory tract infections according to age, gender and high-risk co-morbidity: the Second Dutch National Survey of General Practice. Fam Pract. 2006;23(3):291–294. doi: 10.1093/fampra/cmi121. [DOI] [PubMed] [Google Scholar]
- 12.Wiersma T, Goudswaard AN. Utrecht: Bohn Stafleu Van Loghum; 2006. NHG-Standaarden voor de huisarts. [NHG-Guidelines for the general practitioner] [Google Scholar]
- 13.Akkerman AE, Kuyvenhoven MM, van der Wouden JC, Verheij TJM. Prescribing antibiotics for respiratory tract infections by GPs; management and prescriber characteristics. Br J Gen Pract. 2005;55(511):114–118. [PMC free article] [PubMed] [Google Scholar]
- 14.Gonzales R, Barrett PH, Steiner JF. The relation between purulent manifestations and antibiotic treatment of upper respiratory tract infections. J Gen Int Med. 1999;14(3):151–156. doi: 10.1046/j.1525-1497.1999.00306.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Van Duijn HJ, Kuyvenhoven MM, Schellevis FG, Verheij TJM. Determinants of prescribing second-choice antibiotics in Dutch general practice. J Antimicrob Chemother. 2005;56(2):420–22. doi: 10.1093/jac/dki214. [DOI] [PubMed] [Google Scholar]
- 16.Cockburn J, Pit S. Prescribing behaviour in clinical practice: patients' expectations and doctors' perceptions of patients' expectations — a questionnaire study. BMJ. 1997;315(7107):520–523. doi: 10.1136/bmj.315.7107.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davey P, Pagliari C, Hayes A. The patient's role in the spread and control of bacterial resistance to antibiotics. Clin Microbiol Infect. 2002;8(suppl 2):43–68. doi: 10.1046/j.1469-0691.8.s.2.6.x. [DOI] [PubMed] [Google Scholar]
- 18.Welschen I, Kuyvenhoven MM, Hoes A, Verheij TJM. Antibiotics for acute respiratory tract symptoms: Patients' expectations, GPs' management and patients' satisfaction. Fam Pract. 2004;21(3):234–237. doi: 10.1093/fampra/cmh303. [DOI] [PubMed] [Google Scholar]
- 19.Westert GP, Schellevis FG, de Bakker DH, et al. Monitoring health inequalities through the Second Dutch National Survey of General Practice. Eur J Public Health. 2005;15(1):59–65. doi: 10.1093/eurpub/cki116. [DOI] [PubMed] [Google Scholar]
- 20.Hoeymans N, Garssen AA, Westert GP, Verhaak PFM. Measuring mental health of the Dutch population: a comparison of the GHQ-12 and the MHI-5. Health Qual Life Outcome. 2004;2(1):23–28. doi: 10.1186/1477-7525-2-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van Duijn HJ, Kuyvenhoven MM, Schellevis FG, Verheij TJM. Views on respiratory tract symptoms and antibiotics of Dutch general practitioners, practice staff and patients. Patient Educ Couns. 2006;61(3):342–347. doi: 10.1016/j.pec.2005.03.012. [DOI] [PubMed] [Google Scholar]
- 22.Bruijnzeels MA, van der Wouden JC, Prins A, van den Heuvel WJA. Validity and accuracy of interview and diary data on children's medical utilisation in the Netherlands. J Epidemiol Comm Health. 1998;52:65–69. doi: 10.1136/jech.52.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Petrou S, Murray L, Cooper P, Davidson LL. The accuracy of self-reported healthcare resource utilization in health economy studies. Int J Technol Assess Health Care. 2002;18(3):705–710. doi: 10.1017/s026646230200051x. [DOI] [PubMed] [Google Scholar]
- 24.Widdicombe JG. Advances in understanding and treatment of cough. Monaldi Arch Chest Dis. 1999;54(3):275–279. [PubMed] [Google Scholar]
- 25.Arcavi L, Benowitz NL. Cigarette smoking and infection. Arch Intern Med. 2004;164(20):2206–2216. doi: 10.1001/archinte.164.20.2206. [DOI] [PubMed] [Google Scholar]
- 26.Bellón JÁ, Delgado A, De Dios Luna J, Lardelli P. Psychosocial and health belief variables associated with frequent attendance in primary care. Psychol Med. 1999;29(6):1347–1357. doi: 10.1017/s0033291799008995. [DOI] [PubMed] [Google Scholar]
- 27.Eriksson T, Maclure M, Kragstrup J. Consultation with the general practitioner triggered by advice from social network members. Scand J Prim Health Care. 2004;22(1):54–59. doi: 10.1080/02813430310003192. [DOI] [PubMed] [Google Scholar]
- 28.Van de Kar A, Knottnerus A, Meertens R, et al. Why do patients consult the general practitioner? Determinants of their decision. Br J Gen Pract. 1992;42(361):313–316. [PMC free article] [PubMed] [Google Scholar]
- 29.Akkerman AE, van der Wouden JC, Kuyvenhoven MM, et al. Antibiotic prescribing for respiratory tract infections in Dutch primary care according to patients' age and clinical entities. J Antimicrob Chemother. 2004;54(6):1116–1121. doi: 10.1093/jac/dkh480. [DOI] [PubMed] [Google Scholar]
- 30.Fischer T, Fischer S, Kochen MM, Hummers-Pradier E. Influence of patient symptoms and physical findings in general practitioners' treatment of respiratory tract infections: a direct observation study. BMC Fam Pract. 2005;6(1):6. doi: 10.1186/1471-2296-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Butler CC, Rollnick S, Pill R, et al. Understanding the culture of prescribing: qualitative study of general practitioners' and patients' perceptions of antibiotics for sore throats. BMJ. 1998;317(7159):637–642. doi: 10.1136/bmj.317.7159.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hamm RM, Hicks RJ, Bemben DA. Antibiotics and respiratory infections: are patients more satisfied when expectations are met? J Fam Pract. 1996;43(1):56–62. [PubMed] [Google Scholar]
- 33.Lim WS, Lewis S, Macfarlane JT. Severity prediction rules in community acquired pneumonia: a validation study. Thorax. 2000;55:219–223. doi: 10.1136/thorax.55.3.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kuyvenhoven M, van Essen G, Schellevis F, Verheij T. Management of upper respiratory tract infections in Dutch general practice; antibiotic prescribing and incidences in 1987 and 2001. Fam Pract. 2006;23(2):175–179. doi: 10.1093/fampra/cmi122. [DOI] [PubMed] [Google Scholar]