Abstract
Background
Health locus of control influences health-related behaviour, but its association with healthcare use is unclear.
Aim
To investigate the association between individuals' health locus of control and the use of conventional and alternative health care.
Design of study
Prospective cohort study.
Setting
A nationally representative random sample of community-dwelling adult households in Japan.
Method
Health locus of control, symptom-related visits to physicians, and the use of dietary and physical complementary and alternative medicine (CAM) was measured. Dietary CAM included supplements, such as herbs and vitamins. Physical CAM included manipulations, such as acupuncture and acupressure.
Results
Of the 2453 adult participants studied, 2103 (86%; 95% CI [confidence interval] = 84 to 88%) developed at least one symptom during the 31-day study period. Of these symptomatic adults, 639 visited physicians (30%; 95% CI = 28 to 32%), 480 used dietary CAM (23%; 95% CI = 21 to 25%), and 156 (7%; 95% CI = 6 to 9%) used physical CAM. The likelihood of visiting a physician was not related significantly to individuals' health locus of control. Increased use of dietary CAM was weakly associated with control by spiritual powers (P = 0.028), internal control (P = 0.013), and less control by professionals (P = 0.020). Increased use of physical CAM was significantly associated with control by spiritual powers (P = 0.009) indicating a belief that supernatural forces control individuals' health status.
Conclusion
The likelihood of visiting a physician is not affected by individuals' health locus of control. Control by spiritual powers is involved with increased CAM use. Internal control is weakly associated with greater use of dietary CAM; professional control is weakly associated with less use of dietary CAM.
Keywords: beliefs, complementary therapies, health diaries, spiritual powers
INTRODUCTION
Health locus of control is one of the widely used measures of an individual's health belief,1–4 and is defined as the governing perception an individual has concerning their health. The multi-dimensional health locus of control scale (HLCS) has been designed to determine whether individuals are internalists or externalists. Internalists perceive that they control their own health and are classified as ‘internal control’. Externalists who are classified as ‘chance control’ believe that what happens to their health occurs more by accident or chance, and externalists classified as ‘external control’ believe that powerful or influential external figures control their health status. In the Japanese-specific HLCS, the dimensions of powerful external control are divided into three sub-dimensions based on particularly powerful ‘other’ individuals: medical professionals (professional control), family members (family control), and a belief in the supernatural or spiritual existence (control by spiritual powers).
Individuals' health locus of control influences their health-related behaviours, including health risk behaviour and adherence to recommended health care.4–9 For example, individuals with high internal control are more likely to abstain from smoking and drinking and to adhere to recommendations related to preventive medicine.10–13 However, few studies have evaluated the influence of health locus of control on healthcare utilisation including conventional and complementary and alternative medicine (CAM).14,15 Therefore, the weak association between individual health locus of control and the use of CAM was investigated. CAM assessment forms used in most previous investigations included spiritual healing, which is associated with control by spiritual powers.16 Consequently, the use of spiritual healing, prayer, or shaman from the CAM was excluded to avoid a bias resulting from a ‘plausible’ association between control by spiritual powers and the spiritual modalities of CAM.
How this fits in
Health beliefs of individuals influence their health-related behaviour, including health risk behaviour and adherence to recommended health care. Health locus of control is one of the widely used measures of individuals' health beliefs. The findings of this cohort study suggest that the likelihood of a patient visiting a physician did not differ significantly according to the individual's health locus of control. Use of dietary complementary and alternative medicine (CAM) by participants was associated with an increase in beliefs of high control by spiritual powers and high internal control, whereas the use of physical CAM was associated with a slight increase in high control by spiritual powers.
METHOD
Participants
A prospective cohort study of a representative sample of Japanese households nationwide was analysed. The methodology of this cohort study has been described elsewhere with different aspects of these results published.17 A population-weighted random sample of households controlled for the size of cities, towns, and villages represented, was analysed. Participants were limited to adults aged 18 years and older who filled out a baseline questionnaire and completed a daily health (health diary) and behaviour record, and reported having any pain or symptoms that caused them discomfort during the 31-day study period in October 2003.
Data collection
Health diaries required a daily record for 1 month, from 1 to 31 October 2003. Participants were requested to keep the diary as a record of all health-related events, symptoms, and healthcare utilisation. The aim of the health diary was to elicit responses to the following questions:
Did you have any pain or other health symptoms that caused discomfort?
If so, did you consult a physician? Did you use dietary supplements, such as nutritional drinks, vitamins, or calcium? Did you undergo physical treatment, such as acupressure, acupuncture, or massage?
The independent variables of this study were demographic and clinical data and HLCS. One of the dependent variables was the report of symptom-related visits to a physician during the study period, whether to a primary care physician, community hospital, university hospital, or an emergency department. The other dependent variables were self-reported CAM use, which could be either dietary supplements or physical treatments. Any CAM use during the study period after symptom onset was counted as a single positive use per participant, regardless of the frequency of use. The CAM was divided into two major categories:
Dietary CAM included nutritional drinks, herbs, Kampo (a Japanese herbal medicine), over-the-counter dietary supplements, vitamins and minerals, and other dietary substances.
Physical CAM included massage, acupuncture, acupressure, Judo-seifuku, moxibustion, and chiropractic and other physical manipulations. Spiritual healing, prayer, shaman, and psychotherapy were excluded from CAM modalities, as these practices were related to control by spiritual or other forces.
The Japanese version of the HLCS was used to determine covariates of interest. This version was developed and validated in the general population in Japan and scored on a Likert scale for each response category. A higher or lower individual score indicated a greater or lesser belief for the health locus of control respectively.
The SF-8™ Health Survey, which measures health-related quality of life, was also included in the questionnaire, as the status of physical and mental health may influence use of health care.18 The SF-8 generates a health profile, consisting of eight scales and two summary measures: a physical summary (PCS8) and a mental summary (MCS8). A higher or lower individual score indicates a better or worse health status than the mean respectively. Lastly, having a designated primary care physician and the number of comorbidities that the participants had were also included as covariates, as these factors may also influence healthcare utilisation.19
Statistical analysis
Descriptive statistics for each of the dimensions of the HLCS and for the use of different types of health care were obtained. Proportions of healthcare use for visiting a physician and dietary and physical CAM along with 95% confidence intervals (CIs) were calculated. These frequencies were also analysed by demographic and clinical characteristics. Three separate multivariable-adjusted logistic regression models were constructed to assess associations between use of the three different types of health care and the covariates, and to calculate adjusted odds ratios (OR) and 95% CIs. Due to concerns with the multiple tests of logistic regressions, ‘significant’ was interpreted only for the association with P-value of less than 0.01 and ‘weak’ for the association with P-value of less than 0.05, but more than 0.01. SPSS software (version 14.0J; SPSS-Japan, Tokyo, Japan) was used for all statistical analyses.
RESULTS
Of the 3568 participants in the study, 3477 completed the diary (response rate 97%). Of these participants, there were 2453 aged 18 years and older, of which 2103 (86%; 95% CI = 84 to 88%) had developed at least one symptom. Table 1 shows the descriptive statistics of the HLCS. The minimum score was 5 and the maximum score was 30 for all subscales. Median scores were 24 (internal control), 22 (family), 19 (professional), 15 (chance), and 12 (spiritual powers). The univariate distributions of internal control, family, and professional subscales exhibited negative skewness, while those of chance control and control by spiritual powers exhibited positive skewness.
Table 1.
Descriptive statistics of each subscale of the health locus of control scale (HLCS).
| External HLCS | |||||
|---|---|---|---|---|---|
| Internal HLCS | Family | Professional | Chance | Spiritual Powers | |
| n | 2022 | 2021 | 2021 | 2021 | 2018 |
| Minimum score | 5 | 5 | 5 | 5 | 5 |
| Maximum score | 30 | 30 | 30 | 30 | 30 |
| Median score | 24 | 22 | 19 | 15 | 12 |
| Mean score | 23.53 | 22.15 | 18.86 | 14.83 | 12.51 |
| Standard deviation | 3.369 | 3.944 | 4.068 | 4.344 | 4.752 |
| Standard error of mean | 0.075 | 0.088 | 0.090 | 0.097 | 0.106 |
| Kurtosis | 0.360 | 0.732 | 0.163 | −0.156 | −0.399 |
| Skewness | −0.256 | −0.423 | −0.250 | 0.154 | 0.305 |
Table 2 shows the symptom-related use of health care by demographics, HLCS, and clinical characteristics. Of the 2103 symptomatic adults, 1234 (59%) were women, and the mean age was 46 years. Twenty per cent of participants lived in large cities, 25% in medium-sized cities, 36% in small-sized cities, and 19% lived in rural areas. Eight hundred and forty-seven of the participants (41%) had a primary care physician and 552 (31%) exhibited at least one comorbidity.
Table 2.
Symptom-related use of health care by demographics, health locus of control scale (HLCS), and clinical factors.
| Participant | Visited physicians | Used dietary CAM | Used physical CAM | ||||
|---|---|---|---|---|---|---|---|
| Variable | n (%) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) |
| All participants | 2103 | 639 | 30.4 (28.4 to 32.4) | 480 | 22.8 (21.0 to 24.6) | 156 | 74 (6.3 to 8.5) |
| Demographics (n = 2103) | |||||||
| Sex | |||||||
| Male | 869 (94.13) | 236 | 27.2 (24.2 to 30.1) | 155 | 17.8 (15.3 to 20.4) | 50 | 5.8 (4.2 to 7.3) |
| Female | 1234 (58.7) | 403 | 32.7 (30.0 to 35.3) | 325 | 26.3 (23.9 to 28.8) | 106 | 8.6 (7.0 to 10.2) |
| Age, years | |||||||
| 18–29 | 414 (19.7) | 96 | 23.2 (19.1 to 27.3) | 74 | 17.9 (14.2 to 21.6) | 22 | 5.3 (3.1 to 7.5) |
| 30–39 | 415 (19.7) | 96 | 23.1 (19.1 to 27.2) | 81 | 19.5 (15.7 to 23.3) | 21 | 5.1 (2.9 to 7.2) |
| 40–49 | 445 (21.2) | 106 | 23.8 (19.8 to 27.8) | 112 | 25.2 (21.2 to 29.2) | 31 | 7.0 (4.6 to 9.3) |
| 50–59 | 299 (14.2) | 78 | 26.1 (21.2 to 31.1) | 74 | 24.7 (19.8 to 29.7) | 22 | 7.4 (4.4 to 10.3) |
| 60–69 | 305 (14.5) | 131 | 43.0 (37.4 to 48.5) | 75 | 24.6 (19.7 to 29.5) | 32 | 10.5 (7.0 to 14.0) |
| ≥70 | 225 (10.7 | 132 | 58.7 (52.2 to 65.2) | 64 | 28.4 (22.5 to 34.4) | 28 | 12.4 (8.1 to 16.1) |
| Area of residence | |||||||
| Large city | 424 (20.2) | 117 | 28.7 (24.3 to 33.2) | 113 | 26.7 (22.4 to 30.9) | 50 | 11.8 (8.7 to 14.9) |
| Middle-sized city | 515 (24.5) | 224 | 29.6 (26.3 to 32.8) | 108 | 21.0 (17.4 to 24.5) | 33 | 6.4 (4.3 to 8.5) |
| Small-sized city | 757 (36.0) | 168 | 32.6 (28.6 to 36.7) | 165 | 21.8 (18.8 to 24.7) | 45 | 5.9 (4.3 to 7.6) |
| Rural area | 407 (19.4) | 130 | 30.7 (26.3 to 35.1) | 94 | 23.1 (19.0 to 27.2) | 28 | 6.9 (4.4 to 9.3) |
| HLCS | |||||||
| Internal (n = 2022) | |||||||
| <median score | 985 (48.7) | 294 | 29.8 (27.0 to 32.7) | 220 | 22.3 (19.7 to 24.9) | 70 | 7.1 (5.5 to 8.7) |
| >median score (24)a | 1037 (51.3) | 299 | 28.8 (26.1 to 31.6) | 241 | 23.2 (20.7 to 25.8) | 77 | 7.4 (5.8 to 9.0) |
| Family (n = 2021) | |||||||
| <median score | 881 (43.6) | 261 | 29.6 (26.6 to 32.6) | 188 | 21.3 (18.6 to 24.1) | 63 | 7.2 (5.4 to 8.9) |
| >median score (22)a | 1140 (56.4) | 331 | 29.0 (26.4 to 31.7) | 273 | 23.9 (21.5 to 26.4) | 84 | 7.4 (5.8 to 8.9) |
| Professional (n = 2021) | |||||||
| <median score | 916 (45.3) | 259 | 28.3 (25.4 to 31.2) | 217 | 23.7 (20.9 to 26.4) | 60 | 6.6 (4.9 to 8.2) |
| >median score (19)a | 1105 (54.7) | 333 | 30.1 (27.4 to 32.8) | 244 | 22.1 (19.6 to 24.5) | 87 | 7.9 (6.3 to 9.5) |
| Chance (n = 2021) | |||||||
| <median score | 938 (46.4) | 289 | 30.8 (27.9 to 33.8) | 227 | 24.2 (21.5 to 26.9) | 62 | 6.6 (5.0 to 8.2) |
| >median score (15)a | 1083 (53.6) | 303 | 28.0 (25.3 to 30.7) | 234 | 21.6 (19.2 to 24.1) | 85 | 7.8 (6.2 to 9.5) |
| Spiritual powers (n = 2018) | |||||||
| <median score | 892 (44.2) | 259 | 29.0 (26.1 to 32.0) | 181 | 20.3 (17.6 to 22.9) | 56 | 6.3 (4.7 to 7.9) |
| >median score (12)a | 1126 (55.8) | 333 | 29.6 (26.9 to 32.2) | 280 | 24.9 (22.3 to 27.4) | 91 | 8.1 (6.5 to 9.7) |
| Clinical characteristics | |||||||
| Having a PCP (n = 2059) | |||||||
| No | 1212 (58.9) | 242 | 20.0 (17.7 to 22.2) | 249 | 20.5 (18.3 to 22.8) | 68 | 5.6 (4.3 to 6.9) |
| Yes | 847 (41.1) | 382 | 45.1 (41.7 to 48.5) | 215 | 25.4 (22.4 to 28.3) | 84 | 9.9 (7.9 to 11.9) |
| Number of comorbidities (n = 177) | |||||||
| None | 1226 (69.0) | 254 | 20.7 (18.4 to 23.0) | 261 | 21.3 (19.0 to 23.6) | 63 | 5.1 (3.9 to 6.4) |
| 1 | 357 (20.1) | 138 | 38.7 (33.6 to 43.7) | 79 | 22.1 (17.8 to 26.5) | 36 | 10.1 (6.9 to 13.2) |
| ≥2 | 195 (11.0) | 1111 | 56.9 (49.9 to 63.9) | 61 | 31.3 (24.7 to 37.8) | 30 | 15.4 (10.3 to 20.5) |
| PCS8 score (n = 2204) | |||||||
| ≥50 | 1016 (50.2) | 223 | 21.9 (19.4 to 24.5) | 196 | 19.3 (16.9 to 21.7) | 50 | 4.9 (3.6 to 6.3) |
| <50 | 1008 (49.8) | 391 | 38.8 (35.8 to 41.8) | 267 | 26.5 (23.8 to 29.2) | 104 | 10.3 (8.4 to 12.2) |
| MCS8 score (n = 2024) | |||||||
| ≥50 | 826 (40.8) | 254 | 30.8 (27.6 to 33.9) | 185 | 22.4 (19.5 to 25.2) | 58 | 7.0 (5.3 to 8.8) |
| <50 | 1198 (59.2) | 385 | 30.1 (27.5 to 32.6) | 278 | 23.2 (20.8 to 25.6) | 96 | 8.0 (6.5 to 9.6) |
Figures in brackets indicate median scoree. Large city indicates with population >1 000 000; Middle-sized city population 100 000–1 000 000; Small-sized city indicates city with population <100 000. MCS8 = mental component summary SF-8; PCP = primary care physician; PCS8 = physical component summary of SF-8.
Of the 2103 symptomatic adults, 639 visited physicians (30.4%; 95% CI = 28.4 to 32.4%); 156 adults used physical CAM (7.4%; 95% CI = 6.3 to 8.5%); and 480 used dietary CAM (22.8%; 95% CI = 21.0 to 24.6%) during the study period. Visits to physicians were more frequent than the use of physical CAM (P<0.001). There was no significant difference in frequency between visits to physicians and the use of dietary CAM (P = 0.09).
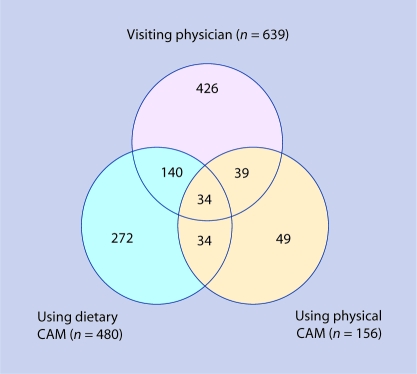
Figure 1 presents the number of participants for symptom-related healthcare choice for these three modalities. Of the 639 adults who visited physicians, 174 (27% of those visiting physicians) also used dietary CAM and 73 (11 %) also used physical CAM. There were 34 adults (5% of those visiting physicians) who visited physicians and used dietary and physical CAM.
Figure 1.
Symptom-related healthcare choices of participants (n = 2103). CAM = complementary and alternative medicine.
Frequent symptoms (n>50 [n = number of patients with each symptom]) reported by participants who visited physicians included back pain (n = 87); sore throat (n = 82); cough (n = 80); toothache (n = 57); headache (n = 57); and neck pain (n = 55). Frequent symptoms (n>100) reported by the dietary CAM users included back pain (n = 183); fatigue (n = 183); headache (n = 177); neck pain (n = 176); sore throat (n = 129); and cough (n = 101). Frequent symptoms (n>30) reported by physical CAM users included back pain (n = 80); neck pain (n = 71); headache (n = 41); and fatigue (n = 34).
Among adults with a higher score of control by spiritual powers of the HLCS (n = 1126): 280 (24.9%) used dietary CAM and 91 (8.1 %) used physical CAM during the study period (Table 2). Among adults with a lower score of control by spiritual powers of the HLCS (n = 892), 181 (20.3%) used dietary CAM and 56 (6.3%) used physical CAM. Among adults with a higher score of internal control (n = 1037), 241 (23.2%) used dietary CAM. Among adults with a lower score of internal control (n = 985), 220 (22.3%) used dietary CAM. Further, among adults with a higher score of professional control (n = 1105), 244 (22.1%) used dietary CAM. Among adults with a lower score of professional control (n = 916), 217 (23.7%) used dietary CAM.
Among adults with a primary care physician (n = 847), 382 (45.1%) visited physicians, 215 (25.4%), used dietary CAM, and 84 (9.9%) used physical CAM in the study period (Table 2). Among adults without a primary care physician (n = 1212), 242 (20.0%) visited physicians, 249 (20.5%) used dietary CAM, and 68 (5.6%) used physical CAM.
In 2103 symptomatic adults, there were 1645 participants who had complete data for demographics, clinical characteristics, and all five dimensions of the HLCS. Multivariable-adjusted ORs for the use of different healthcare modalities in the logistic regression models were calculated for these 1645 participants (Table 3). The likelihood of visiting a physician was not significantly influenced by the HLCS sub-dimensions. The increased use of dietary CAM was weakly associated with higher scores of control by spiritual powers (P = 0.028), internal control (P = 0.013), and a lower score for professional control (P = 0.020). The increased use of physical CAM was significantly associated only with a higher score for control by spiritual powers (P = 0.009). An increased rate of visiting physicians was observed for participants with a primary care physician (P<0.001), with a higher number of comorbidities (P<0.001), and with a lower score of PCS8 (P<0.001). The likelihood of using dietary and physical CAM was not influenced by having a primary care physician. Increased use of dietary CAM was weakly associated with female sex (P = 0.015), older age (P = 0.038), and those with lower score of PCS8 (P = 0.049). A significant increase in the use of physical CAM was observed in participants living in larger cities (P = 0.001), and in those with a lower PCS8 score (P = 0.002).
Table 3.
Adjusted odds ratios for symptom-related use of health care in the multivariable logistic model.a
| Visited physicians | Used dietary CAM | Used physical CAM | ||||
|---|---|---|---|---|---|---|
| Variable | OR (95% CI) | P-value | OR (95% CI) | P-value | OR (95% CI) | P-value |
| Demographics | ||||||
| Sex, female | 1.154 (0.909 to 1.466) | 0.240 | 1.362 (1.061 to 1.749) | 0.015 | 1.212 (0.806 to 1.821) | 0.356 |
| Age, years | 1.006 (0.998 to 1.015) | 0.153 | 1.010 (1.001 to 1.019) | 0.038 | 1.003 (0.989 to 1.018) | 0.677 |
| Area of residence | ||||||
| Large city | reference | reference | reference | |||
| Middle-sized city | 1.137 (0.806 to 1.604) | 0.466 | 0.759 (0.535 to 1.077) | 0.123 | 0.437 (0.255 to 0.748) | 0.003 |
| Small-sized city | 1.052 (0.764 to 1.448) | 0.757 | 0.765 (0.556 to 1.053) | 0.100 | 0.431 (0.267 to 0.698) | 0.001 |
| Rural area | 1.051 (0.729 to 1.517) | 0.789 | 0.832 (0.576 to 1.202) | 0.327 | 0.386 (0.213 to 0.697) | 0.002 |
| HLCS | ||||||
| Internal | 0.987 (0.952 to 1.023) | 0.471 | 1.048 (10.010 to 1.087) | 0.013 | 1.032 (0.972 to 1.096) | 0.299 |
| Family | 1.013 (0.981 to 1.047) | 0.419 | 1.013 (0.980 to 1.047) | 0.448 | 0.967 (0.916 to 1.022) | 0.234 |
| Professional | 0.994 (0.963 to 1.026) | 0.698 | 0.962 (0.932 to 0.994) | 0.020 | 1.035 (0.979 to 1.093) | 0.224 |
| Chance | 0.978 (0.949 to 1.009) | 0.157 | 0.973 (0.943 to 1.004) | 0.092 | 0.990 (0.941 to 1.041) | 0.692 |
| Spiritual powers | 1.001 (0.974 to 1.029) | 0.939 | 1.033 (1.004 to 1.062) | 0.028 | 1.063 (1.016 to 1.114) | 0.009 |
| Clinical characteristics | ||||||
| Having a PCP | 1.743 (1.342 to 2.264) | <0.001 | 1.056 (0.800 to 1.295) | 0.701 | 0.967 (0.916 to 1.022) | 0.234 |
| Comorbidities, n | 1.431 (1.223 to 1.673) | <0.001 | 1.056 (0.905 to 1.232) | 0.492 | 1.209 (0.982 to 1.488) | 0.074 |
| PCS8 | 0.960 (0.943 to 0.978) | <0.001 | 0.982 (0.964 to 1.000) | 0.049 | 0.957 (0.931 to 0.984) | 0.002 |
| MCS8 | 1.011 (0.993 to 1.030) | 0.227 | 0.989 (0.971 to 1.006) | 0.210 | 1.017 (0.987 to 1.047) | 0.283 |
Odds ratios (ORs) and P-values are calculated using logistic regression adjusted for all variables shown above. ORs continuous covariates are related to an increase of one unit or one score for each covariate. Large city indicates city with population >1 000 000; middle-sized city with population of 100 000–1 000 000; small-sized city indicates city with population <100 000. HLCS = health locus of control scale; MCS8 = mental component summary SF-8; PCP = primary care physician; PCS8 = physical component summary of SF-8.
DISCUSSION
Summary of main findings
In this prospective cohort study based on the daily health record of 2453 participants, 86% developed at least one symptom during the 31-day study period. Of these symptomatic adults, 30% visited physicians, 23% used dietary CAM, and 7% used physical CAM; many used two or more modalities of these healthcare choices. The likelihood of visiting a physician was not significantly influenced by health locus of control. However, the increased use of dietary CAM was weakly associated with beliefs of control by spiritual powers and internal control, and low professional control. Control by spiritual powers was associated significantly with use of physical CAM. To understand CAM use among patients, it may be important to consider an individual's health locus of control as a psychosocial motivation for the use of alternative medicine.20
There are several explanations for the result that the use of dietary or physical CAM was associated with control by spiritual powers. First, some participants with this view are likely to use alternative medicine because they feel that spiritual powers are involved more frequently with this medicine compared with other forms.21,22 Second, they may believe that it is important to treat illnesses within a non-conventional context using alternative medicine rather than conventional forms based on modern science and technology.21,22 Finally, some of the participants may have changed their health locus of control toward control by spiritual powers after being involved with a successful experience to treat illness using alternative medicine, and felt that spiritual powers affected the health outcome to a greater degree than other forms of health care.
These findings indicate that the use of dietary CAM slightly increased with high internal control of HLCS, but decreased with high professional control. People with these control views may seek out more CAM, as they consider alternative medicine to be less paternalistic, more empowering, and offering autonomy and control over their healthcare decision-making process.
Strengths and limitations of the study
This study may be the first to analyse the influence of individuals' health locus of control on behaviour related to healthcare utilisation among conventional and alternative medicine. Spiritual modalities were excluded from the CAM modalities in this study; however, it was then shown that the participants with high control by spiritual powers still exhibited a higher likelihood of using dietary and physical CAM.
There were several limitations of the study. First, although it was based on a random, nationally-representative sample, selection bias may have been caused by differences in response rates regarding questionnaires for the HLCS and decreased sample sizes as a result of missing data. A second limitation may be related to data collection for CAM use. A more detailed classification of CAM was not used for specific modalities of physical manipulations. However, most previous studies evaluated CAM therapy combining dietary and physical treatment. Thirdly, although CAM therapy may be more likely to be used for maintenance of health than for treatment of illness,23 the use of dietary and physical CAM was determined to treat symptoms. However, this outcome measure may be better suited to compare the health-related critical decision between conventional and alternative medicine, as this outcome is likely to avoid a bias from baseline of the regular use of CAM among a small proportion of people. Finally, the sample median score of each subscale of the HLCS was used as the estimated approximation of population median score in a Japanese general population with the cut-off scores constructed for a descriptive analysis of this study. The median scores used in this study may not be accurate estimates of population median scores in the general population of Japan.
Comparison with existing literature
Although previous studies have indicated that health locus of control is associated with several health-related behaviours, the results of this study demonstrate that the likelihood of visiting a physician does not differ significantly according to health locus of control. Further, in this study adults with high control by spiritual powers are shown to use dietary and physical CAM more frequently; this confirms the findings of previous studies.16,24,25 Moreover, in this study, adults with high internal control use dietary CAM more often, whereas adults with high professional control are less likely to use dietary CAM. These results may be new findings and therefore need further confirmation.
The frequency of symptoms reported in this study (86%) was relatively similar to those in a previous study.26 Green et al showed that among 1000 men, women, and children in the US, 800 (80%) experienced symptoms on average each month.26 In the current study, however, participants were asked to report symptoms that caused ‘discomfort’. Therefore, it is likely that the participants may not have reported minor symptoms. The likelihood of visiting a physician in this study may be higher than that in previous studies.27–29 A higher frequency for visiting a physician may result from several factors that are specific to Japan, including universal health insurance coverage, ready access to physicians, standardised rates of medical payment, availability of numerous clinics and hospitals, and a relatively low level of income inequality.29–31 As these backgrounds are related to the conventional healthcare system in Japan, if the Japanese were to become symptomatic, they are likely to visit physicians regardless of each individual's health locus of control.
This study's findings indicate that the use of dietary and physical CAM increase with control by spiritual powers. This may confirm the previous hypothesis introduced by Petry et al.24 The significant predictors for CAM use in the exploratory study by Astin included holistic philosophy, cultural creativity, and transformational experience,16 while those in the study by Testerman et al included holistic beliefs and control by spiritual powers.25 The predictors involved with this dimension in these previous studies are somewhat arbitrary and do not systematically measure all dimensions of individuals' health beliefs.16,25 However, the HLCS was used as a validated systematic measure for each individual's health beliefs. Further, a natural association between control by spiritual powers and spiritual forms of CAM was excluded by eliminating these CAM forms from the CAM modalities as a dependent variable. Therefore, the methodology used in this study appears to be a powerful tool to demonstrate the association between control by spiritual powers and CAM use compared with the previous studies,16,25 which may have been biased through the inclusion of a spiritual form of CAM.
Implications for future research
A large proportion of participants used combinations of two or more healthcare modalities including conventional health care as well as alternative medicine. With the increased popularity of alternative medicine, it may be important to understand why a large proportion of people seek approaches that are outside conventional health care. Adults with high control by spiritual powers are more likely to use dietary and physical CAM. Adults with beliefs of high internal control are more likely to use dietary CAM. In contrast, adults with high professional control are less likely to use dietary CAM. Based on the findings of the current study, an individual's health locus of control may be a psychosocial motivation for the use of alternative medicine. Therefore, when assessing an individual's CAM use, it may be important for healthcare practitioners, public health professionals, and policy makers to consider the health locus of control of the these individuals. Individuals' health locus of control is unrelated to the use of conventional health care in this study. Investigation of other reasons for the difference in terms of frequency of seeking conventional health care is needed.
Acknowledgments
We would like to thank the participants in this cohort study and W Kenji Sakurai and Masaaki Shakudo for their support, as well as Mikio Kumagai, Riki Tanaka, and Yumiko Yotsumoto for their excellent secretarial assistance.
Funding body
St Luke's Life Science Institute
Ethics committee
The Research Ethics Committee of the Kyoto University Graduate School of Medicine
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Wallston BS, Wallston KA, Kaplan GD, Maides SA. Development and validation of the health locus of control (HLC) scale. J Consult Clin Psychol. 1976;44(4):580–585. doi: 10.1037//0022-006x.44.4.580. [DOI] [PubMed] [Google Scholar]
- 2.Wallston KA, Wallston BS, DeVellis R. Development of the multidimensional health locus of control (MHLC) scales. Health Educ Monogr. 1978;6(2):160–170. doi: 10.1177/109019817800600107. [DOI] [PubMed] [Google Scholar]
- 3.Wallston KA. The validity of the multidimensional health locus of control scales. J Health Psychol. 2005;10(5):623–631. doi: 10.1177/1359105305055304. [DOI] [PubMed] [Google Scholar]
- 4.Kuwahara A, Nishino Y, Ohkubo T, et al. Reliability and validity of the multidimensional health locus of control scale in Japan: relationship with demographic factors and health-related behaviour. Tohoku J Exp Med. 2004;203(1):37–45. doi: 10.1620/tjem.203.37. [DOI] [PubMed] [Google Scholar]
- 5.Yoshida Y, Takagi H, Inaba Y. [Health locus of control and acquisition of health-related information] Nippon Koshu Eisei Zasshi. 1995;42(2):69–77. (In Japanese.) [PubMed] [Google Scholar]
- 6.Yoshida Y, Takagi H. [Relationships between resting behaviour and health locus of control among elementary schoolgirls] Nippon Koshu Eisei Zasshi. 1997;44(11):836–844. (In Japanese.) [PubMed] [Google Scholar]
- 7.Ogawa Y, Nakamura H, Nagase H, et al. [Structural analysis for psychosocial factors including health locus of control (HLC) and sense of coherence (SOC) associated with lifestyle-related diseases] Nippon Eiseigaku Zasshi. 2001;55(4):597–606. doi: 10.1265/jjh.55.597. (In Japanese.) [DOI] [PubMed] [Google Scholar]
- 8.O'Hea EL, Grothe KB, Bodenlos JS, et al. Predicting medical regimen adherence: the interactions of health locus of control beliefs. J Health Psychol. 2005;10(5):705–717. doi: 10.1177/1359105305055330. [DOI] [PubMed] [Google Scholar]
- 9.Holt CL, Clark EM, Kreuter MW, Rubio DM. Spiritual health locus of control and breast cancer beliefs among urban African American women. Health Psychol. 2003;22(3):294–299. doi: 10.1037/0278-6133.22.3.294. [DOI] [PubMed] [Google Scholar]
- 10.Schlenk EA, Hart LK. Relationship between health locus of control, health value, and social support and compliance of persons with diabetes mellitus. Diabetes Care. 1984;7(6):566–574. doi: 10.2337/diacare.7.6.566. [DOI] [PubMed] [Google Scholar]
- 11.Brown S, Steele K. Nurse-mediated serum cholesterol reduction and health locus of control — a device for targeting health promotion? Br J Gen Pract. 1999;49(443):467–468. [PMC free article] [PubMed] [Google Scholar]
- 12.Booth-Butterfield M, Anderson RH, Booth-Butterfield S. Adolescents' use of tobacco, health locus of control, and self-monitoring. Health Commun. 2000;12(2):137–148. doi: 10.1207/S15327027HC1202_2. [DOI] [PubMed] [Google Scholar]
- 13.Burkhart PV, Rayens MK. Self-concept and health locus of control: factors related to children's adherence to recommended asthma regimen. Pediatr Nurs. 2005;31(5):404–409. [PubMed] [Google Scholar]
- 14.Ramos-Remus C, Watters CA, Dyke L, et al. Assessment of health locus of control in the use of nonconventional remedies by patients with rheumatic diseases. J Rheumatol. 1999;26(11):2468–2474. [PubMed] [Google Scholar]
- 15.Schafer T, Riehle A, Wichmann HE, Ring J. Alternative medicine and allergies: life satisfaction, health locus of control and quality of life. J Psychosom Res. 2003;55(6):543–546. doi: 10.1016/s0022-3999(03)00015-1. [DOI] [PubMed] [Google Scholar]
- 16.Astin JA. Why patients use alternative medicine. JAMA. 1998;279(19):1548–1553. doi: 10.1001/jama.279.19.1548. [DOI] [PubMed] [Google Scholar]
- 17.Fukui T, Rhaman M, Takahashi O, et al. The ecology of medical care in Japan. JMAJ. 2005;48(4):163–167. [Google Scholar]
- 18.Fukuhara S, Suzukamo Y. Manual of the SF-8 Japanese version, (in Japanese) Kyoto: Institute for Health Outcomes and Process Evaluation Research; 2004. [Google Scholar]
- 19.Al-Windi A. Determinants of complementary alternative medicine (CAM) use. Complement Ther Med. 2004;12(2–3):99–111. doi: 10.1016/j.ctim.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 20.Hinohara S. Medicine and religion: spiritual dimension of health care. Hum Health Care. 2001;1(2):E2. [PubMed] [Google Scholar]
- 21.Bessinger D, Kuhne T. Medical spirituality: defining domains and boundaries. South Med J. 2002;95(12):1385–1388. [PubMed] [Google Scholar]
- 22.Foster E. The spiritual encounter within a complementary therapy treatment. Complement Ther Clin Pract. 2006;12(2):163–169. doi: 10.1016/j.ctcp.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 23.Bair YA, Gold EB, Greendale GA, et al. Ethnic differences in use of complementary and alternative medicine at midlife: longitudinal results from SWAN participants. Am J Public Health. 2002;92(11):1832–1840. doi: 10.2105/ajph.92.11.1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Petry JJ, Finkel R. Spirituality and choice of health care practitioner. J Altern Complement Med. 2004;10(6):939–945. doi: 10.1089/acm.2004.10.939. [DOI] [PubMed] [Google Scholar]
- 25.Testerman JK, Morton KR, Mason RA, Ronan AM. Patient motivations for using complementary and alternative medicine. Complement Health Pract Rev. 2004;9(2):81–92. [Google Scholar]
- 26.Green LA, Fryer GE, Yawn BP, et al. The ecology of medical care revisited. N Eng J Med. 2001;344:2021–2025. doi: 10.1056/NEJM200106283442611. [DOI] [PubMed] [Google Scholar]
- 27.Freeman HE, Blendon RJ, Aiken LH, et al. Americans report on their access to health care. Health Aff (Millwood) 1987;6(1):6–8. doi: 10.1377/hlthaff.6.1.6. [DOI] [PubMed] [Google Scholar]
- 28.Stoddard JJ, St Peter RF, Newacheck PW. Health insurance status and ambulatory care for children. N Engl J Med. 1994;330(20):1421–1425. doi: 10.1056/NEJM199405193302006. [DOI] [PubMed] [Google Scholar]
- 29.Anderson G, Hussey PS. Comparing health system performance in OECD countries. Organization for economic cooperation and development. Health Aff (Millwood) 2001;20(3):219–232. doi: 10.1377/hlthaff.20.3.219. [DOI] [PubMed] [Google Scholar]
- 30.Ikegami N. Japan: maintaining equity through regulated fees. J Health Polit Policy Law. 1992;17(4):689–713. doi: 10.1215/03616878-17-4-689. [DOI] [PubMed] [Google Scholar]
- 31.Yajima R, Takayanagi K. The Japanese health care system: citizen complaints, citizen possibilities. J Health Hum Serv Adm. 1998;20(4):502–519. [PubMed] [Google Scholar]