Abstract
The line joining the superior aspect of the iliac crests posteriorly (the intercristal line) is commonly stated to cross the midline at the L4 or L4–5 spinal level on imaging. This study aimed to assess the spinal level identified through palpation of surface anatomy (iliac crests and posterior superior iliac spines) in adults and the level of agreement compared with the intercristal line identified through imaging. The study participants included consecutive adult patients undergoing prone fluoroscopically guided spinal injections for chronic low back pain at the Royal Orthopaedic Hospital, Birmingham, between April and July 2004. Prior to fluoroscopic imaging, each patient's surface anatomy was palpated by two examiners and lines created to form the palpated intercristal line and the posterior superior iliac spine line. Following imaging, the mid-line spinal levels identified by these palpated lines were recorded and the level of agreement (kappa coefficient) with the intercristal line formed by imaging of the iliac crests was assessed. The results showed that although the L4 or L4–5 spinal levels were identified on imaging of the intercristal line in 86.7% of 75 patients (49 female), the intercristal line formed through palpation tended to identify higher levels; the L3 or L3–4 spinal levels in 77.3% of cases and more commonly in females than in males (85.7 vs. 61.5%) and in patients with higher body mass indices. The level of agreement between the two lines was poor (κ = 0.05). The posterior superior iliac spine line identified the S2 spinous process in 51% and the S1 in 44% of 60 (45 female) patients. The results suggest that formation of the intercristal line by palpation of the iliac crests identifies different spinal levels to those identified by imaging and that both methods should be regarded as different instruments. In the clinical situation, it may be more appropriate to consider that palpation of the intercristal line is a guide for identifying the L3 or L3–4 spinal levels rather than the L4 or L4–5 levels, particularly in females and patients with higher body mass indices.
Keywords: iliac crest, intercristal line, palpation, posterior superior iliac spine, spinal level
Introduction
The line joining the superior aspect of the iliac crests posteriorly – variously described as the intercrestal (Kim et al. 2003b), intercristal (Williams & Warwick, 1980), supracristal (Borley, 1997), Tuffier's (Tuffier, 1900) or Jacoby's (Kubota et al. 1992) line – is commonly stated to cross the midline at the L4 or L4–5 spinal level (Cunningham & Ramenes, 1979; Atkinson et al. 1987; Ellis & Feldman, 1993; Ombregt et al. 1998). This has been confirmed by several studies (Render 1996; Kim et al. 2003a,b; Jung et al. 2004) through analysis of lumbar spine images. Similarly, a line joining the two posterior superior iliac spines (PSIS) is also stated to cross the midline at the second sacral spinous process (Borley, 1997). In the clinical situation, however, using palpation of bony landmarks as a guide, it has been demonstrated that identification of the exact spinal level is frequently inaccurate (Van Gessel et al. 1993; Broadbent et al. 2000; Furness et al. 2002).
The aims of this study were two-fold: (1) to assess if the spinal level found by identification of the intercristal line (ICL) by palpation of the bony landmarks agrees with the level identified through X-ray imaging, and (2) to assess which spinal levels are identified by a line joining the inferior aspect of the PSIS.
Methods
The study group comprised consecutive adult patients at the Royal Orthopaedic Hospital, Birmingham, UK, under the care of the first author (R.C.), undergoing fluoroscopically guided lower lumbar spine injections for low back pain for the 3-month period from April 2004. Local hospital ethics committee approval for the study was granted prospectively. Patients were excluded from the study if high lumbar injections were being performed where imaging would not involve the relevant areas or if their lumbar anatomy was potentially compromised by spinal scoliosis, spondylolisthesis, severe disc height reduction, sacralization, lumbarization, previous spinal surgery or osteoporosis with loss of vertebral height. Consent was obtained from each patient. Age, sex, weight and height were recorded and body mass index (BMI) calculated.
Prior to imaging and injection, each patient was examined in the prone position on the fluoroscopy table by two examiners (R.C. and K.I.), both experienced in palpating the iliac crests in their day-to-day management of patients. Iliac crests were palpated and a mark was made on the overlying skin at the uppermost margin of each iliac crest. Examiners were not blinded to the other examiner's mark. If there was disagreement over the height of the crests the patient was re-examined by each examiner until agreement was reached. A long, small-diameter, rigid metal rod was then placed on the skin surface between the two marks to act as a radio-opaque marker, forming the ICL. Anterior–posterior fluoroscopic images were then obtained, centralized over the radio-opaque markers and the spinal level where the marker crossed the midline was recorded. Following this the ICL was again formed, this time between the superior aspects of the two iliac crests according to the fluoroscopic image, and the midline level was again recorded (Fig. 1). Imaging was kept to a minimum throughout and patients did not undergo any further radiation exposure than would normally be required for the injection procedure. The null hypothesis was that there would be no difference in the spinal level identified by palpation and imaging. In this study, spinal level refers to either a spinous process (e.g. L3) or to the space between two spinous processes (e.g. L3–4). The kappa coefficient (κ) was used to assess the agreement between the two methods. Confidence intervals (CI) are given for the statistics at a 95% level.
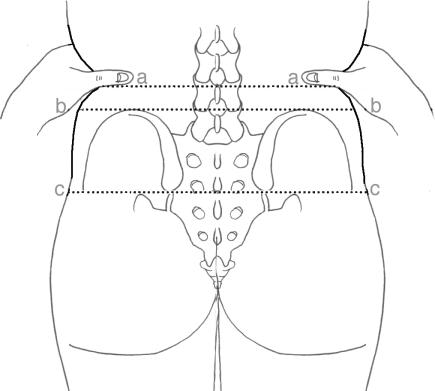
Fig 1.
The lines referred to in the study: the palpated intercristal line (a), the imaged intercristal line (b) and the palpated posterior superior iliac spine line (c).
For the second experiment, during the same study period, only patients who were to undergo injections where the imaging was likely to involve the sacrum were included. The first author (R.C.) palpated both PSIS and marked the skin overlying their inferior margins prior to the fluoroscopic images being obtained. Again a linear radio-opaque marker was placed between the marks (the PSIS line) and the midline spinous process was recorded (Fig. 1).
Results
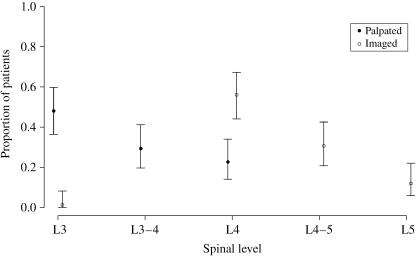
Sevety-five patients (49 female) were eligible for inclusion in part 1 of the study. Mean values at assessment were: age, 45.0 years (range 18–71); height, 167.5 cm (range 150–191); weight, 73.3 kg (range 50–104); BMI, 25.8 kg m−2 (range 19–38). Table 1 shows the frequency that spinal levels were identified, using the ICL, on palpation and imaging. Figure 2 illustrates the proportion of samples hitting a particular spinal level together with error bars showing the 95% confidence limits.
Table 1.
Spinal level identified by palpation and by imaging of the intercristal line by sex (SP = spinous process, IS = interspinous space)
| Palpated | Imaged | |||
|---|---|---|---|---|
| Female | Male | Female | Male | |
| L3 SP | 28 | 8 | 0 | 1 |
| L3–4 IS | 14 | 8 | 0 | 0 |
| L4 SP | 7 | 10 | 23 | 19 |
| L4–5 IS | 0 | 0 | 18 | 5 |
| L5 SP | 0 | 0 | 8 | 1 |
| Totals | 49 | 26 | 49 | 26 |
Fig 2.
Proportion of spinal levels identified by imaging and palpation of the intercristal line, together with error bars showing the 95% confidence intervals.
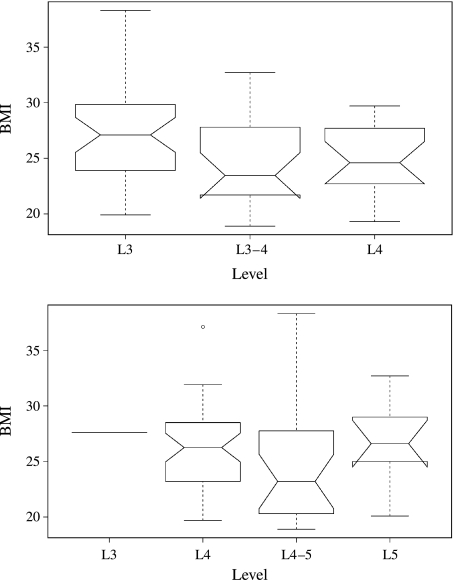
In the case of palpation it can be seen that when the ICL crossed an interspinous space, this was always at L3–4 and, when it crossed a spinous process, this was more likely to be the L3 process than the L4 in females (ratio 4 : 1) and equally likely to be either the L3 or the L4 in males. In 86.7% of patients the imaged ICL passed through either the L4 or the L4–5 spinal levels with 12% passing through the L5 and 1.3% through the L3 spinous processes. Agreement between the imaged and palpated lines was poor [κ = 0.05 (CI = −0.01 to 0.12)] and occurred in just nine (12%) of the 75 patients, with the palpated level being one spinal level higher in 17 (22.7%), two levels higher in 34 (45.3%), three higher in 12 (16%) and four higher in three (4%) (Table 2). On no occasions did the palpated line identify a lower level than the imaging. Although there is a tendency for higher spinal levels to be identified by the palpated ICL with increasing patient BMI, the difference between the median values did not reach significance, as judged by the 95% confidence limits (Fig. 3a). Similarly, there was no relationship between the spinal level identified by the imaged ICL and BMI (Fig. 3b).
Table 2.
A cross-tabulation showing the frequency of spinal levels identified by palpation and imaging of the intercristal line (SP = spinous process, IS = interspinous space)
| Imaged | ||||||
|---|---|---|---|---|---|---|
| L3 SP | L3–4 IS | L4 SP | L4–5 IS | L5 SP | Total | |
| Palpated | ||||||
| L3 SP | 1 | 0 | 23 | 9 | 3 | 36 |
| L3–4 IS | 0 | 0 | 11 | 8 | 3 | 22 |
| L4 SP | 0 | 0 | 8 | 6 | 3 | 17 |
| L4–5 IS | 0 | 0 | 0 | 0 | 0 | 0 |
| L5 SP | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 1 | 0 | 42 | 23 | 9 | 75 |
Fig 3.
Distribution of BMI against spinal level identified by (a) the palpated intercristal line and (b) the imaged intercristal line.
Sixty patients (45 female) were eligible for inclusion in part 2 of the study. Mean values at treatment were: age, 45.7 years (range 18–83); height, 165.8 cm (range 150–191); weight, 73.5 kg (range 50–104); BMI, 25.3 kg m−2 (range 19–38). On palpation, the PSIS line identified the S2 spinous process in 51% of cases and the S1 in 44%. The upper and lower levels identified were the L5 and S3 spinous processes, respectively (Table 3).
Table 3.
Spinal levels identified by the PSIS line by sex
| Female | Male | Total | |
|---|---|---|---|
| L5 | 1 | 0 | 1 |
| S1 | 18 | 6 | 24 |
| S2 | 23 | 8 | 31 |
| S3 | 3 | 1 | 4 |
| Total | 45 | 15 | 60 |
Discussion
Identification of the correct spinal level through examination is a necessary part of spinal medicine but its importance is most clearly evident when performing lumbar injections without fluoroscopy. The main hazard would be selecting too high a level, thus injecting a level more cephalad than the conus medullaris, which can extend as low as to the upper aspect of the L3 vertebral segment (Kim et al. 2003a). Various methods of identifying the correct spinal level by examination have been described, including dropping a vertical line downwards from the uppermost iliac crest with the patient in a side-lying position (half-Tuffier's line) (Ievins, 1991), construction of a line between the two PSISs (Borley, 1997) and constructing a line between the lowermost margins of the tenth ribs (Jung et al. 2004). However, construction of the ICL through palpation of the iliac crests, first described by Jacoby and Tuffier (Tuffier, 1900; Kubota et al. 1992) in the late 19th century, has proven to be the most popular method, with several authoritative textbooks referring to it as crossing the L4 or L4–5 spinal level (Cunningham & Ramenes, 1979; Atkinson et al. 1987; Ellis & Feldman, 1993; Ombregt et al. 1998).
Several authors have attempted to verify the spinal level identified by the ICL by reviewing plain radiographs or MRI scans of the lumbar spine. The level identified appears to follow a symmetric distribution with the L4 spinous process or L4–5 interspinous space being identified in 70–90% of cases using this method. The L5 spinous process is the next most frequently identified with the L3–4 and L5–S1 interspinous spaces identified in 3.7% or fewer of cases (Render, 1996; Kim et al. 2003a; Jung et al. 2004). Our study also found that the imaged ICL crossed the L4 spinous process or the L4–5 interspinous space in the majority (86.7%) of adult patients with normal spinal anatomy and crossed the L5 spinous process next most frequently (12%) and rarely (1.3%) passed above the L4 spinal level.
Despite the consistency of these findings, several authors have demonstrated difficulty in identifying the exact spinal level through palpation of bony landmarks. Using the ICL as a guide, these authors have found that a more cephaled level is more likely to be identified than the correct level (41–57% vs. 29–41%), with the error of margin extending up to four spinal levels too high. Less frequently, a level more caudal is identified (3.6–28%) (Van Gessel et al. 1993; Broadbent et al. 2000; Furness et al. 2002). Agreement between clinicians on the estimated level through palpation, however, has been found to be good, at 60% (Broadbent et al. 2000), and thus it appears that it is the use of L4 or L4–5 as the guide rather than the execution of the method of forming the line that appears to lead to errors. Only one author has found a reasonable percentage (78.3%) identification of the correct spinal level compared with half-Tuffier's line (59.3%) but the study sample was small and cadavers, rather than live subjects, were used (Ievins, 1991).
Factors that have been shown to influence poor identification of the correct spinal level include selection of a high lumbar spinal level and obesity (Broadbent et al. 2000; Furness et al. 2002). Positioning of the patient in a sitting or lateral position does not affect the accuracy even though in nearly half the patients, the spinal level intersected by the ICL on imaging moves downward by one level on full lumbar flexion (Kim et al. 2003b).
The present study may help to explain the frequent inaccurate identification of the correct spinal levels found in previous studies. The use of the ICL as a guideline for the L4 or L4–5 spinal levels holds true for the imaged ICL but not for the palpated ICL, which identifies the L3 spinous process or L3–4 intraspinous space in the majority of cases (77.3%). We found the agreement between the two lines to be poor (κ = 0.05), suggesting that the two lines are entirely different instruments. It is therefore important to distinguish between these two methods of identifying the ICL when considering it as a guide for the correct spinal level. The difference between the two is most likely explained by the subcutaneous tissue between the bony landmarks and the palpating hand. Perhaps not surprisingly, adult females who have more percentage body fat for equivalent BMIs, different fat distribution and who develop progressively greater waist to hip ratios with age than adult males were found to have proportionately more higher levels identified on palpation (Gallagher et al. 1996; Bartali et al. 2002). This study also showed that use of the PSIS line as an alternative indicator of correct spinal level is limited by the relatively high frequency of identification of both the S1 and the S2 levels. It is important to stress that our study only included patients with normal lumbar spine anatomy and further inaccuracies in identification of the correct spinal level might be expected if there were sacralization or lumbarization of the lower spine (prevalence 8–15%) (Ford & Goodman, 1966; O'Driscoll et al. 1996), spondylolisthesis (prevalence up to 6%) (Frederickson et al. 1984), lumbar scoliosis or loss of vertebral height.
One potential limitation in the methodology of the present study is that after identification of the palpated ICL, the fluoroscopic beam was then not re-centred on the imaged ICL. This was to ensure that the patient had no more radiation exposure than would normally have been used for the injection procedure. In the our experience, however, the error caused by the divergent beam would have been minimal and would have been unlikely to have made significant differences to the recorded imaged ICL.
Use of fluoroscopy when performing spinal injections would negate any errors when choosing the correct spinal level for injection but if not practical in the clinical situation, then use of bedside ultrasound has been shown to improve the reliability of choosing the correct level (Furness et al. 2002).
Conclusion
This study shows that the ICL identifies different spinal levels depending on whether it is formed by palpation of the iliac crests or through spinal imaging. Through palpation, the L3 spinous process and L3–4 interspinous spaces are most frequently identified, whereas, with imaging, it is the L4 spinous process and the L4–5 interspinous spaces which are most frequently identified. These two methods of forming the ICL should therefore be considered as separate instruments used in identifying the correct spinal level. In the clinical situation, it may be more appropriate to consider that palpation of the ICL is a guide for identifying the L3 or L3–4 spinal levels rather than the L4 or L4–5 levels, particularly in females and patients with higher BMI. The PSIS line identifies the S2 spinous process most frequently followed by the S1 spinous process and is therefore an unreliable guide for the correct spinal level.
References
- Atkinson RS, Rushman GB, Lee A, editors. Synopsis of Anaesthesia. 10. Bristol: Wright Publishing; 1987. [Google Scholar]
- Bartali B, Benvenuti E, Corsi AM, Bandinelli S, Russo CR, Di Iorio A, Lauretani F, Ferrucci L. Changes in anthropometric measures in men and women across the life-span: findings from the InCHIANTI study. Soz Praventivmed. 2002;47:336–348. doi: 10.1007/pl00012644. [DOI] [PubMed] [Google Scholar]
- Borley NR, editor. Concise Colour Guide to Clinical Surface Anatomy. London: Manson Publishing Ltd; 1997. [Google Scholar]
- Broadbent CR, Maxwell WB, Ferrie R, Wilson DJ, Gawne-Cain M, Russell R. Ability of anaesthetists to identify a marked lumbar interspace. Anaesthesia. 2000;55:1122–1126. doi: 10.1046/j.1365-2044.2000.01547-4.x. [DOI] [PubMed] [Google Scholar]
- Cunningham DJ, Ramenes CJ, editors. Cunningham's Manual of Practical Anatomy. 14. Oxford: Oxford University Press; 1979. [Google Scholar]
- Ellis H, Feldman S, editors. Anatomy for Anaesthetists. 6. Oxford: Blackwell; 1993. [Google Scholar]
- Ford LT, Goodman FG. X-ray studies of the lumbosacral spine. South Med J. 1966;59:1123–1128. doi: 10.1097/00007611-196610000-00001. [DOI] [PubMed] [Google Scholar]
- Frederickson BE, Baker D, McHolick WJ, Yuan HA, Lubicky JP. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am. 1984;66:699–707. [PubMed] [Google Scholar]
- Furness G, Reilly MP, Kuchi S. An evaluation of ultrasound imaging for identification of lumbar intervertebral level. Anaesthesia. 2002;57:277–280. doi: 10.1046/j.1365-2044.2002.2403_4.x. [DOI] [PubMed] [Google Scholar]
- Gallagher D, Visser M, Sepulveda D, Pierson RN, Harris T, Heymsfield SB. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol. 1996;143:228–239. doi: 10.1093/oxfordjournals.aje.a008733. [DOI] [PubMed] [Google Scholar]
- Ievins FA. Accuracy of placement of extradural needles in the L3–4 interspace: comparison of two methods of identifying L4. Br J Anaesth. 1991;66:381–382. doi: 10.1093/bja/66.3.381. [DOI] [PubMed] [Google Scholar]
- Jung CW, Bahk JH, Lee JH, Lim YJ. The tenth rib line as a new landmark of the lumbar vertebral level during spinal block. Anaesthesia. 2004;59:359–363. doi: 10.1111/j.1365-2044.2004.03657.x. [DOI] [PubMed] [Google Scholar]
- Kim JT, Bahk JH, Sung J. Influence of age and sex on the position of the conus medullaris and Tuffier's line in adults. Anesthesiology. 2003a;99:1359–1363. doi: 10.1097/00000542-200312000-00018. [DOI] [PubMed] [Google Scholar]
- Kim JT, Jung CW, Lee JR, Min SW, Bahk JH. Influence of lumbar flexion on the position of the intercrestal line. Reg Anesth Pain Med. 2003b;28:509–511. doi: 10.1016/j.rapm.2003.08.027. [DOI] [PubMed] [Google Scholar]
- Kubota Y, Toyoda Y, Kubota H. Jacoby's line rather than Tuffier's line as a guide to lumbar puncture. Anesth Analg. 1992;74:939. doi: 10.1213/00000539-199206000-00043. [DOI] [PubMed] [Google Scholar]
- O'Driscoll CM, Irwin A, Saifuddin A. Variations in the morphology of the lumbosacral junction on sagittal MRI: correlation with plain radiography. Skeletal Radiol. 1996;25:225–230. doi: 10.1007/s002560050069. [DOI] [PubMed] [Google Scholar]
- Ombregt L, Bischop P, ter Veer HJ, van der Vede T. A System of Orthopaedic Medicine. London: WA Saunders Co Ltd; 1998. [Google Scholar]
- Render CA. The reproducibility of the iliac crest as a marker of lumbar spine level. Anaesthesia. 1996;51:1070–1071. doi: 10.1111/j.1365-2044.1996.tb15009.x. [DOI] [PubMed] [Google Scholar]
- Tuffier T. Anesthesie medullaire chirurgicale par injection sous-arachnoidienne lombaire de cocaine; technique et results. Sem Med. 1900;20:167–169. [Google Scholar]
- Van Gessel EF, Forster A, Gamulin Z. Continuous spinal anesthesia: where do spinal catheters go? Anesth Analg. 1993;76:1004–1007. doi: 10.1213/00000539-199305000-00015. [DOI] [PubMed] [Google Scholar]
- Williams PL, Warwick R, editors. Gray's Anatomy. 36. Edinburgh: Churchill Livingstone; 1980. [Google Scholar]