OVERVIEW
The goal of our study was to determine if there were an association between prepregnancy BMI, hypertensive disorders of pregnancy, and subsequent maternal mortality.
Background and Objective
Hypertensive disorders of pregnancy (HDP) complicate 6-8% of all pregnancies and are the second leading cause of maternal mortality. [The following line was not a sentence, which is why I corrected it] Although early reports argued that there were no adverse maternal health consequences after delivery of a pregnancy complicated by hypertensive disease, more recent studies have shown elevated mortality and morbidity, particularly from cardiovascular causes.
Hypertensive disorders of pregnancy have been associated with various metabolic abnormalities that are known risk factors for cardiovascular disease. Without information on prepregnancy metabolic status, however, it is difficult to tell whether the subsequent development of cardiovascular disease in women who have had a hypertensive pregnancy is a result of pathologic events that occurred during the pregnancy or of preexisting risk factors.
Elevated prepregnancy body mass index (BMI) has been linked to various pregnancy complications, including preeclampsia. Elevated BMI has also been linked to increased morbidity and mortality from cardiovascular disease. However, the relationship between BMI and hypertensive disorders of pregnancy and mortality has not been well characterized. We examined the association between prepregnancy BMI, hypertensive disorders of pregnancy, and subsequent maternal mortality.
Materials and Methods
We analyzed data on a subset of Jewish women in Jerusalem who had given birth in 1975-1976 and were interviewed about their prepregnancy weight and height. Hypertensive disorders of pregnancy were defined as gestational hypertension or preeclampsia. Long-term follow-up was conducted by linking the personal identification numbers of the subjects to national registries.
The final analysis was restricted to women who had survived to 1978 and for whom data on prepregnancy BMI was recorded (n=13,722). BMI <18.5 kg/m2 was considered underweight; 18.5-24.9, normal weight; 25-29.9, overweight; and ≥30, obese. Hypertensive disorders of pregnancy (HDP) were defined as a history of preeclampsia or gestational hypertension in the index pregnancy and/or past pregnancies.
Survivors were censored on Jan. 1, 2005. We constructed 2 models: one for women who survived <15 years and one for women who survived ≥15 years.
Results
As expected, the incidence of HDP increased with increasing BMI. The crude rates of HDP were 3.3% and 5.3% for underweight and normal weight, respectively, vs 14.8% and 26.9% for women who were overweight and obese, respectively. After adjustment for age, the odds ratios (ORs) were 0.67 (95% CI, 0.48-0.92) for underweight women, 1 for women of normal weight (reference category), 2.82 (2.40-3.31) for overweight women, and 5.51 (4.15-7.31) for obese women.
Compared with women who were of normal weight before pregnancy, those who were overweight showed a 42% increase in subsequent mortality; those who were obese showed a 143% increase. The age-adjusted hazard ratios (HRs) in the 4 groups were 1.05 (95% CI, 0.73-1.53), 1 (reference group), 1.42 (1.10-1.83), and 2.43 (1.61-3.68), respectively.
We created 2 models for survival after HDP: one for the first 15 years of follow-up and one for follow-up after 15 years. In the first 15 years after delivery, no significant difference in survival was noted between patients who had HDP and those who had normotensive pregnancies (age-adjusted HR, 1.05 [95% CI, 0.49-2.27); age- and BMI-adjusted HR, 1.14 [0.42-2.49]). After 15 years of follow-up, a significant decrease in survival was observed among women who had HDP vs women who did not have HDP. The age-adjusted HR for mortality after HDP, adjusted for maternal age, was 1.94 (1.42-2.67). This result remained significant, although slightly attenuated, after the addition of prepregnancy BMI to the model (HR, 1.65 [1.19, 2.79]).
The Table illustrates, for women who survived for at least 15 years, the excess mortality risk after HDP for women in each BMI category vs women in that category who did not have HDP. This model allows us to examine in detail the role of BMI in attenuating the association between HDP and mortality. Hypertensive disorders of pregnancy were not associated with a significant increase in mortality for women who were underweight or of normal weight before pregnancy. For overweight women, however, HDP conferred almost a 2-fold increase in mortality risk vs overweight women who did not have HDP. For obese women, the increased risk was even larger (HR, 2.90 [1.28-6.58]).
Comment
This study demonstrates that elevated BMI is associated with increased risk for HDP and that HDP are associated with increased maternal mortality for those who survive for more than 15 years. The HR for mortality after HDP remained significant, although attenuated, after the addition of BMI to the model, suggesting that BMI contributes to, but does not fully explain, the excess mortality. Elevated prepregnancy BMI was associated with increased maternal mortality after HDP.
Sattar and Greer suggested that the physiologic changes of pregnancy could serve as a “stress test” of the maternal metabolic pathways and vascular function. The basic principle is that preexisting subclinical risk factors (such as subtle metabolic derangements or endothelial dysfunction) appear as clinical disease during the metabolic and vascular stress of pregnancy. After the cessation of the pregnancy stress, the clinical manifestations of the disease disappear, only to reappear later in life with the increased stress of aging and other pathologic events. Although previous reviews have addressed this concept, few studies have measured the prepregnancy risk factors required to test the hypothesis adequately. Instead, most of the studies examining risk factors for HDP and later-life disease measured these factors during pregnancy, thereby making it impossible to determine whether they are risk factors for pregnancy complications or simply evidence of a more widespread underlying systemic disorder.
To avoid this problem, the current study used a risk factor that predated the pregnancy: prepregnancy BMI. Elevated BMI has been linked to various physiologic changes that could underlie the association between HDP and subsequent maternal mortality. In this cohort, increased prepregnancy BMI was associated with an increased risk for later-life mortality after HDP.
This finding suggests that prepregnancy risk factors can affect the relationship between pregnancy complications and later-life disease. Although these observations do not exclude a role for pathologic events in pregnancy and subsequent cardiovascular disease, they argue strongly in favor of the importance of prepregnancy risk factors as a major determinant of both the development of HDP and long-term maternal mortality. These findings also suggest that women with HDP should be followed after pregnancy and that appropriate interventions be instituted to increase their long-term survival.
CLINICAL IMPLICATIONS
Elevated prepregnancy BMI is associated with increased risk for hypertensive disorders of pregnancy (HDP).
HDP are associated with increased long-term maternal mortality, which is significantly greater in women who are overweight or obese before pregnancy than in those who are underweight or of normal weight, suggesting that prepregnancy risk factors can affect the relationship between pregnancy complications and later-life disease.
Women with HDP should be followed after pregnancy and appropriate interventions should be instituted to increase their long-term survival.
Figure 1.
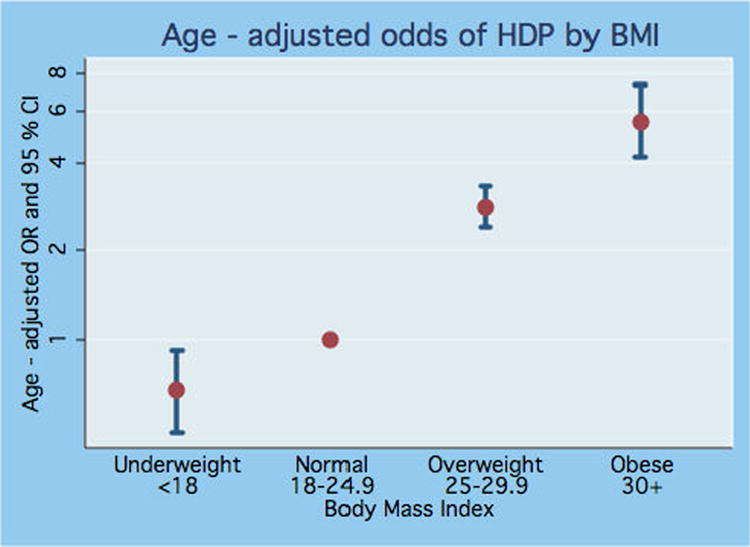
Figure 2.
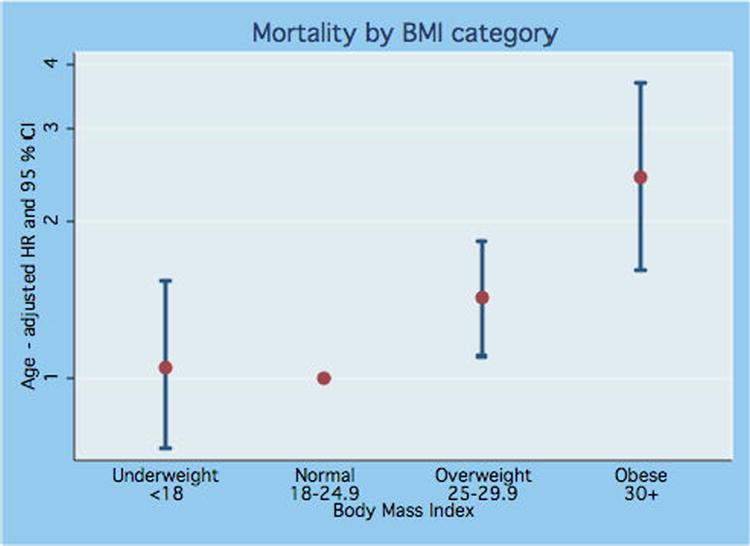
Table I.
Characteristics of the Cohort
| Characteristic | Ever had HDP
(n=926) |
Never had HDP
(n=12796) |
Total cohort
(n=13,722) |
|||
|---|---|---|---|---|---|---|
| Age (years) | Mean | SD | Mean | SD | Mean | SD |
| 29.3 | 5.9 | 27.3 | 5.2 | 27.4 | 5.2 | |
| BMI Category | N | % | N | % | N | % |
| Underweight (<18.5 kg/m2) | 41 | 4.4 | 1185 | 9.3 | 10501 | 76.5 |
| Normal weight (18.5-24.9) | 555 | 59.9 | 9946 | 77.7 | 1712 | 12.5 |
| Overweight (25-29.9) | 254 | 27.4 | 1458 | 11.4 | 283 | 2.1 |
| Obese (>30) | 76 | 8.2 | 207 | 1.6 | 1226 | 8.9 |
| Survival | ||||||
| Surviving <15 years | 7 | 0.8 | 105 | 0.8 | 112 | 0.8 |
| Surviving ≥ 15 years | 919 | 99.2 | 12691 | 99.2 | 13610 | 99.2 |
| Alive in 2005 | 873 | 94.3 | 12426 | 97.1 | 13299 | 96.9 |
| Dead before 2005 | 53 | 5.7 | 370 | 2.9 | 423 | 3.1 |
Table II.
Mortality after HDP for those who survived ≥15 years by BMI category
| Underweight | Normal | Overweight | Obese | |
|---|---|---|---|---|
| No | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| HDP | ||||
| HDP* | 1.31 | 1.26 | 1.86 | 2.90 |
| 95% CI | 0.18, 9.76 | 0.74, 2.14 | 1.07, 3.20 | 1.28, 6.58 |
Age-adjusted
Acknowledgments
Ms Samuels-Kalow received a summer research grant from NIH–NHLBI through the Office of Student Research, Yale University School of Medicine. Dr Funai was supported by the National Center for Research Resources, RR15536-05. Ms Harlap was supported by NARSAD and by the National Cancer Institute (2R01CA-080197).
Footnotes
Presented at the 53rd Annual Scientific Meeting of the Society for Gynecologic Investigation, Toronto, ON, Canada, March 22-25, 2006.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.


