Abstract
Background
Hospital admission rates for asthma in Britain rose during the 1980s and fell during the 1990s, but less is known about recent trends in the prevalence of asthma.
Methods
In 1991 and 2002 the same questionnaire was distributed to parents of all school pupils in year 3 (aged 7–8 years) in the London borough of Croydon. Parents of currently wheezy children were then invited for home interview (100% targeted in 1991, 66% in 2002).
Results
The prevalence of wheeze during the previous year increased from 12.9% in 1991 to 17.8% in 2002 (prevalence ratio 1.39 (95% CI 1.23 to 1.56)). Increases were observed in frequent (1.54 (95% CI 1.16 to 2.03)) and infrequent attacks, severe speech limiting episodes (2.25 (95% CI 1.34 to 3.77)), and night waking (1.36 (95% CI 1.07 to 1.72)), and in the reported use of steroids (19.9% v 64.1% of currently wheezy children). Nevertheless, the proportions reporting a visit to the GP at his/her surgery for wheeze in the previous year (prevalence ratio 1.15 (95% CI 0.91 to 1.45)) or an outpatient visit (0.98 (95% CI 0.49 to 1.94)) changed little and an increase in reported casualty attendance (1.66 (95% CI 0.89 to 3.07)) was non‐significant.
Conclusions
There is evidence of an increase in the prevalence of asthma among British primary school children between 1991 and 2002. The absence of a corresponding increase in health service utilisation data may reflect more widespread prophylactic treatment and/or changes in the use and provision of medical services.
Keywords: asthma, prevalence, children, medical services
In Britain in the 1990s downward trends were observed among school children for asthma mortality and hospital admission rates for asthma, while consultation rates in primary care for acute asthma attacks fell, having peaked in 1993.1,2,3 This led to suggestions that asthma morbidity, after increasing throughout the 1970s and 1980s, is now in decline. However, recent serial prevalence studies of parent reported wheeze in primary school children suggest that the prevalence of asthma in this age group is either continuing to rise, albeit at a reduced rate, or has flattened out.4,5,6 We present data from a study of school children aged 7–8 years in Croydon, London that permits comparisons over a 24 year period based on surveys conducted in 1978, 1991, and 2002. Papers contrasting the 1978 and 1991 data have already been published elsewhere so this paper is largely restricted to a comparison between 1991 and 2002.7,8
Methods
Screening survey
In February 1978, 1991, and 2002 the same 1 page questionnaire was distributed through schools to the parents of all children in year 3 (ages 7–8 years) in the London borough of Croydon. The questionnaire asked: “Has your child ever had asthma?” and, if no, “Has he/she ever had attacks of wheezing in the chest?” A positive response to either led to the question: “Has your child had any attacks of asthma or wheezing over the past 12 months?” followed by: “If YES, over the past 12 months: (a) About how many times have these attacks of wheezing or asthma occurred? (Once only, 1–4 times, 5 times or more)”. Questions (b) to (e) on the same branch asked if these attacks caused school absence, if they usually occurred with a cold or bronchitis, and if they had been treated by the GP (family doctor) at his surgery; at hospital in casualty; at hospital in outpatients; and at hospital on the ward. Response rates to the questionnaire were 87% in 1978, 81% in 1991,7 and 73% (3111/4246) in 2002.
Home interview
Following the screening survey in 1991, all children with a report of asthma or wheezing attacks in the previous year were selected for home interview with a parent or guardian. In 2002 a random sample of two thirds of such children were selected. Using the same questions in 2002 as in 1991, information was obtained regarding symptom patterns. These included night waking (“woken up at night with an attack of asthma or wheeziness in the chest”) and severe speech limiting episodes (“severe enough to limit (child's name) to saying no more than 1 or 2 words at a time between breaths”). Information was also collected on hay fever and eczema and on the use of primary and secondary care services in the past year “for asthma or wheeziness in the chest”. The level of detail obtained at the interview stage meant that this (rather than the screening questionnaire) became our primary source of information on medical service use.
Ethics approval for the 2002 survey was obtained from the Croydon local research ethics committee.
Statistical methods
Population prevalence estimates and 95% confidence intervals (CI) were calculated from data collected at screen using standard statistical theory,9 and from interview data using Poisson regression. Ratios of proportions, 95% CI, and exact p values were calculated using the EPITAB procedure in Stata Release 8.0 (StataCorp, College Station, TX, USA, 2003).
Results
Sampling and response rates
Following a second distribution of questionnaires (not required in 1978 or 1991) the final response rate from 78 out of 83 schools that agreed to participate in 2002 was 73% (3111/4246). Attacks of asthma or wheezing in the previous year were reported by 18.0% of responders to the original and 17.3% of responders to the reminder questionnaire, suggesting minimal response bias. Based on completed questionnaires, the proportion of boys was 48% in 1991 and 49% in 2002.
In 1991 the response rate for the home interview was 80% but in 2002 it was only 55% (table 1). We therefore investigated sampling error and response bias in the 2002 data by comparing answers to all questions on the screening questionnaire between responders to the home interview and all the currently wheezy children identified at screen. In general, there was good agreement between the two. However, the group with home interview data contained fewer girls (41% v 45%), more frequent wheezers (27% v 22%), fewer children born in 1994 (63% v 67%), and more carrying the asthma label (84% v 77%). This suggests a slightly higher response among those with asthma.
Table 1 Response to screening questionnaire and home interview in the 1991 and 2002 studies.
| Detail | 1991 | 2002 |
|---|---|---|
| Population targeted | 3786 | 4246 |
| Forms returned | 3070 | 3111 |
| Response rate | 81% | 73% |
| Wheeze in previous 12 months | 395 | 555 |
| Sought for home interview | 395 | 366† |
| False positives | 7 | 9 |
| Sought for home interview excluding false positives | 388 | 357 |
| Interview obtained | 312 | 198 |
| Response rate | 80% | 55% |
| Exclusions‡ | 10 | 0 |
| After exclusions | 302 | 198 |
Note: Response rates have been calculated after excluding false positives as in the third Croydon study no attempt was made to interview subjects identified as false positives at initial phone contact.
†66% random sample.
‡In 1991 10 stopped wheezing at interview (interviewed as former wheezers).
Population based trends from 1978 to 2002
The prevalence of asthma or wheezing attacks in the previous year based on the screening questionnaire increased from 11.1% in 19787 to 12.9% in 1991 and 17.8% in 2002 (table 2). This represents an increase between 1991 and 2002 of 39% (prevalence ratio 1.39, 95% CI 1.23 to 1.56). This change was not restricted to infrequent or mild symptoms as shown by the increase in frequent wheeze in the previous year from 2.5% in 19787 to 2.6% in 1991 and 4.0% in 2002. Further, using home interview data, we estimated more than a doubling in the prevalence of severe speech limiting episodes between 1991 and 2002, albeit following the near 50% fall reported between 1978 and 1991.8 Also, there was a 36% increase in the prevalence of night waking which was in line with the non‐significant 37% increase reported between 1978 and 1991.8 Defining atopy as a reported history of allergic nose problems and or eczema, the estimated population prevalence of atopic wheeze rose from 8.1% in 1991 to 14.6% in 2002 while the population prevalence of non‐atopic wheeze fell slightly from 4.8% to 3.3% (table 2). The prevalence of current attacks labelled as asthma increased in population terms from 3.4% in 19787 to 7.8% in 1991 and 13.8% in 2002 (table 2), as did the proportion of currently wheezy children labelled as asthmatic (31% in 1978,7 61% in 1991, 77% in 2002). However, there was little change in the population prevalence of attacks causing school absence (8.4% in 1978,7 8.4% in 1991, 9.9% in 2002).
Table 2 Estimated population prevalences† (per 100 children) of morbidity and service use, and estimated prevalence ratios (2002:1991).
| Estimated population prevalence (per 100) | |||
|---|---|---|---|
| 1991 | 2002 | 2002:1991 prevalence ratio (95% CI) | |
| Screening survey data (morbidity) | |||
| Attacks of asthma or wheezing in last year | 12.9 | 17.8 | 1.39 (1.23 to 1.56)*** |
| Frequent attacks in last year‡ | 2.6 | 4.0 | 1.54 (1.16 to 2.03)** |
| Attacks causing school absence in last year | 8.4 | 9.9 | 1.18 (1.01 to 1.39)* |
| Asthma diagnosis with attacks in last year | 7.8 | 13.8 | 1.76 (1.51 to 2.04)*** |
| Previous attacks but not in the last year | 8.0 | 13.5 | 1.69 (1.45 to 1.96)*** |
| Home interview data (morbidity) | |||
| Severe speech limiting attacks in last year | 1.20 | 2.70 | 2.25 (1.34 to 3.77)** |
| Waking at night in last year with wheeze | 7.56 | 10.25 | 1.36 (1.07 to 1.72)* |
| Atopic wheezing in the last year§ | 8.10 | 14.58 | 1.80 (1.46 to 2.22)*** |
| Non‐atopic wheezing in the last year§ | 4.77 | 3.26 | 0.68 (0.47 to 1.00)* |
| Wheezing triggered only by colds | 1.28 | 1.62 | 1.27 (0.71 to 2.28) |
| Home interview data (medical service use) | |||
| Visited GP at surgery in last year for wheeze | 8.89 | 10.23 | 1.15 (0.91 to 1.45) |
| Outpatient attendance in last year for wheeze | 1.11 | 1.09 | 0.98 (0.49 to 1.94) |
| Casualty attendance in last year for wheeze | 0.98 | 1.62 | 1.66 (0.89 to 3.07) |
| Hospital admission in last year for wheeze | 0.47 | 0.27 | 0.58 (0.16 to 2.07) |
*p<0.05, **p<0.01, ***p<0.001.
†Population: 7–8 year old children attending schools in the London borough of Croydon.
‡Frequent = five or more attacks.
§Attacks of asthma and or wheezing in the last year at screen with (atopic) or without (non‐atopic) a reported history of eczema and/or allergic nose problems.
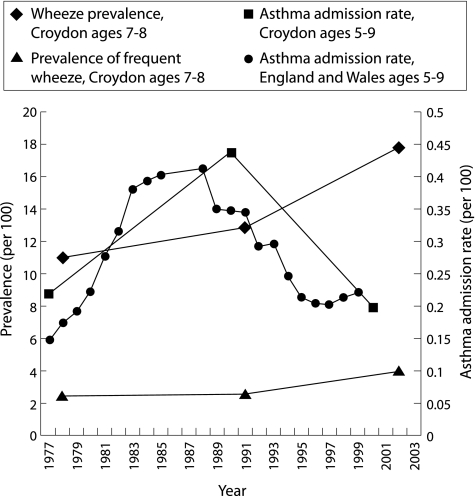
The prevalence of former wheeze (that is, previous attacks but not in the past year) also increased between surveys from 8.0% in 1991 to 13.5% in 2002. However, based on routine data, admission rates for childhood asthma nationally suggested a major increase through 1977 and into the 1980s followed by a sharp decline in the 1990s (fig 1, right hand axis). Among 5–9 year old children in Croydon the estimated number of emergency asthma admissions rose from 57 (22 per 10 000) in 1977 to 83 (44 per 10 000) in 1990,7 falling to 48 (20 per 10 000) in 2000 (Hospital Episode System (HES) data supplied by Lung and Asthma Information Agency (www.laia.ac.uk)).
Figure 1 Trends in wheeze prevalence and hospital admission rates for asthma. Source: Hospital In‐Patient Enquiry (HIPE) data, Welsh Health Common Services Authority data, and Hospital Episode System (HES) data supplied by the Lung and Asthma Information Agency (ww.laia.ac.uk) and Strachan and Anderson.7
Home interview: medical services
A larger proportion of Croydon children in 2002 than in 1991 had a report of casualty attendance for wheeziness in the past year (table 2), while the proportion reporting a visit to the GP at his/her surgery for wheezing was only slightly higher in 2002. However, both observed increases failed to reach statistical significance at the 5% level. There was no evidence of a change in the prevalence of wheeziness treated in outpatients, and the estimated fall in the prevalence of hospital asthma admission—though in line with trends in routinely collected data for Croydon—was also non‐significant.
Medical services data collected as part of the self‐completed screening questionnaire were not presented in tables as they were thought to be prone to over‐reporting with the inclusion of events more than 12 months ago. This was evidenced in both the 1991 and 2002 studies by particularly high prevalence estimates at odds with information collected at home interview, as well as routine data on hospital asthma admission rates. However, the home interview data may also be prone to bias, given the low response rate of 55% in 2002, and affords lower statistical power. We therefore compared prevalence ratios and 95% confidence intervals based firstly on the home interview data and secondly on the screening data. The results were (1.15 (95% CI 0.91 to 1.45) v 1.21 (95% CI 1.06 to 1.39)) for GP visit at surgery, (1.66 (95% CI 0.89 to 3.07) v 1.86 (95% CI 1.32 to 2.61)) for casualty attendance, (0.98 (95% CI 0.49 to 1.94) v 0.89 (95% CI 0.55 to 1.43)) for treatment at outpatients, and (0.58 (95% CI 0.16 to 2.07) v (0.80 (95% CI 0.52 to 1.22)) for hospital admission. Despite the time lag between screen and interview which may account for some differences, the prevalence ratios presented above were not that dissimilar. Furthermore, based on screening data, the prevalence ratio for casualty attendance reached statistical significance.
Home interview: medications
There was a threefold increase in the percentage reporting use of antihistamines in the past year as a treatment for wheeziness (3.0% in 1991 v 9.6% in 2002), a reduction of more than half in the percentage reporting antibiotics (22.2% v 10.6%), but little change in the reported use of expectorants (9.6% v 10.1%, table 3). The percentage reporting use of asthma drugs for wheeziness in the past year (75.8% v 82.8%) also changed little (p = 0.07). This reflected the small and non‐significant increase (p = 0.06) in the reported use of β2 agonists (72.4% v 80.3%), in stark contrast to the increasing trend observed in Croydon children between 1978 and 1991.1,10 However, in line with previous trends,1,10 there was a threefold increase in the reported use of steroids (19.9% v 64.1%). This was mainly due to an increase in inhaled steroids (17.9% v 64.1%) with a more modest increase observed in oral steroids (4.0% v 8.6%). The apparent change in steroid prescription was mirrored though not fully accounted for by a fall in the reported use of cromoglycates over the same period (7.9% v 0.5%), suggesting a large increase in the proportion using preventer drugs.
Table 3 Precipitating factors and treatment as reported at the home interview.
| Percentage of wheezy children | |||
|---|---|---|---|
| 1991 | 2002 | 2002:1991 ratio of proportions (95% CI) | |
| Wheeze brought on by: | |||
| Exercise | 51.7 | 58.4 | 1.13 (0.96 to 1.33) |
| Colds | 92.7 | 92.4 | 1.00 (0.95 to 1.05) |
| Excitement | 42.1 | 37.9 | 0.90 (0.72 to 1.12) |
| Animals | 28.8 | 28.0 | 0.97 (0.73 to 1.31) |
| Foods | 15.5 | 20.8 | 1.34 (0.92 to 1.97) |
| Plants | 31.0 | 39.3 | 1.27 (0.99 to 1.62) |
| Dust | 17.7 | 30.7 | 1.74 (1.23 to 2.45)** |
| Smoke | 36.3 | 41.0 | 1.13 (0.89 to 1.44) |
| Weather | 57.2 | 65.5 | 1.14 (0.99 to 1.32) |
| Pollution | 18.5 | 45.7 | 2.48 (1.84 to 3.34)*** |
| Treatment for wheeze in the last year | |||
| Oral steroids | 4.0 | 8.6 | 2.16 (1.06 to 4.43)* |
| Inhaled steroids | 17.9 | 64.1 | 3.59 (2.76 to 4.67)*** |
| Any steroids | 19.9 | 64.1 | 3.23 (2.52 to 4.14)*** |
| β agonists | 72.4 | 80.3 | 1.11 (1.01 to 1.22) |
| Cromoglycate | 7.9 | 0.5 | 0.06 (0.01 to 0.47)*** |
| Any asthma drugs† | 75.8 | 82.8 | 1.09 (1.00 to 1.20) |
| Antihistamines | 3.0 | 9.6 | 3.2 (1.49 to 6.97)** |
| Antibiotics | 22.2 | 10.6 | 0.48 (0.30 to 0.75)*** |
| Expectorants | 9.6 | 10.1 | 1.05 (0.61 to 1.80) |
In 2002 there were no reports of children having taken methylxanthenes or sympathomimetic with antihistamine preparations in the past 12 months. Anticholinergics were reported as being taken in the past 12 months for less than 1% of wheezy children in both studies (0.3% in 1991 and 0.5% in 2002).
*p<0.05, **p<0.01, ***p<0.001.
†Includes steroids, β agonists, xanthenes, cromglycate, anticholinergics, sympathomimetic prepartions (with xanthines or antihistamines), and other anti‐asthma medications.
Home interview: characteristics of wheezers
Those with home interview data in the 1991 study were similar to those in the 2002 study in terms of the percentage with no older siblings (42% v 43%) and mean (SD) age at interview (8.4 (0.37) v 8.5 (0.38) years), although in 1991 a slightly higher proportion had a mother born in the UK (77% v 68%) or a father in a non‐manual social class (60% v 55%) and median (interquartile range) lag time in months between the commencement of the screening survey and the completion of a home interview was slightly lower (5 (3–8) v 7 (3–8)).
A shift in opinion between 1991 and 2002 as to the factors which precipitate attacks of wheezing was evidenced by more than a doubling in the proportion reporting air pollution as a trigger for their child's wheezing and a 74% (95% CI 23% to 145%) increase in the proportion reporting dust (table 3). A modest increase in the estimated population prevalence of wheeze triggered only by colds was non‐significant (table 2). There was little change in the proportion reporting exercise, animals, or tobacco smoke as triggers—that is, triggers that had become more commonly reported between 1978 and 1991.8 Pollution as a trigger was not recorded separately in the 1978 study.
Discussion
Is asthma still increasing?
Between 1991 and 2002 differences were observed in Croydon in the parent reported prevalence of both infrequent and frequent attacks of asthma/wheezing and of speech limiting episodes. However, since response rates in 2002 were lower than in 1991, the possibility that any increase has been overestimated cannot be totally ruled out. These findings may suggest that the prevalence of wheezing illness has continued to rise into the 21st century. Alternatively, they are consistent with a rise in prevalence occurring in the early to mid 1990s, stabilising or even falling to some extent thereafter. With respect to the modest increase observed in the prevalence of night waking, it is possible that this was due at least in part to the slight over‐representation of asthmatic subjects and frequent wheezers in the 2002 home interview data. However, when we attempted to adjust for such over‐representation, the prevalence ratio for speech limiting episodes was little changed (2.14 v 2.25).
Our results appear to be representative of a wider population since the changes in asthma admission rates for Croydon between 1978 and 2002 were consistent with national trends (fig 1). Trends in prevalence in British school children may therefore be age specific. This could explain why increases were observed in young children in Croydon but not in teenagers in the Health Survey for England6 or in the UK arm of the International Study of Asthma and Allergies in Childhood (ISAAC UK).11 In ISAAC UK, a national study of 12–14 year olds, the 12 month period prevalence of self‐reported wheeze for south east England fell from 31% in 1995 to 26% in 200211 while data from the Health Survey for England indicated the prevalence of wheeze in the past 12 months among 13–15 year old children was 19% in 1995–7 and 17% in 2001–2.6
Two recent British serial prevalence studies that more closely resembled our study in terms of age and period were the study of children aged 8–9 years in Sheffield by Kwong et al4 and a study of children aged 9–12 years in Aberdeen by Devenny et al.5 The Sheffield study reported an increase in the 12 month period prevalence of wheeze between 1991 and 1999 from 17.0% to 19.4%. However, the increase was small and confined to occasional symptoms. The authors took this to indicate that either any real increase was being tempered by the appropriate treatment of severe asthma or that minor wheezing symptoms were simply more readily recognised and reported.4 The latter seems unlikely to explain the findings in Croydon where reports of frequent wheeze, speech limiting episodes, and night waking appeared to rise alongside infrequent wheeze, and where such a large proportion of currently wheezy children had taken steroids in the past year. The Aberdeen study also reported an increase, this time in the prevalence of wheeze over the previous 3 years which rose from 20% in 1989 through 25% in 1994 to 28% in 1999.5
The results of these three local studies widely dispersed throughout the UK suggest that, at least in primary school children, there is evidence of an increase in prevalence during the 1990s. The Aberdeen data also suggest that the rate of increase may have slowed in the latter part of the decade.5 This suggestion is supported by data from the Health Survey for England which reported that the prevalence of wheeze in the past 12 months for 7–9 year olds was 15% in 1995–7 and 16% in 2001–2.6
In common with the abovementioned studies4,5,6,11 and with a recent (1990–8) serial prevalence study of pre‐school children in Leicestershire,12 we found evidence of an increase in the prevalence of an asthma diagnosis. However, in Croydon as in Sheffield this appeared to be due not only to an increase in disease prevalence, but also to a continued rise in the use of the asthma label among currently wheezy children (that is, diagnostic transfer).
Treatment
Large increases in the prescription of inhaled steroids have been suggested by several authors as a possible reason for the fall in hospital admissions observed in the 1990s.1,13,14 In our study we found evidence of increases in the prescription of both inhaled and oral steroids, although the largest absolute rise appeared to be in the former. The increase in inhaled steroids appeared to far exceed any decrease in the use of cromoglycate, suggesting a large overall rise in the reported use of preventer therapy (in contrast to a slight rise between 1978 and 1991).1,10 However, there was little evidence to suggest that this trend had had any impact on the overall proportion of children with untreated wheezing.
Atopic wheezing
The threefold increase in the reported use of antihistamines may suggest an increase in the inappropriate use of these treatments for asthma or indicate an increase in the prevalence of co‐morbidity with hay fever. This latter is in line with the apparent increase in the prevalence of atopic wheeze, a smaller non‐signifcant increase in the prevalence of wheeze triggered only by colds and a fall in the prevalence of non‐atopic wheeze. These observed trends could be due to an overall change in the prevalence of atopy in the general population4,5 and/or a real increase in the prevalence of wheezing confined to children with a history of other atopic disease.
Although our study collected information on parent reported triggers for wheeze, this provided few clues as to the reason for any such restricted increase. The significantly higher proportion reporting exercise, contact with animals, and tobacco smoke as triggers in 1991 compared with 1978,8 and the higher proportion reporting pollution and dust as triggers in 2002 compared with 1991, seem best explained by changing patterns of public perception—patterns which, in the case of pollution, are not always consistent with scientific opinion.15
Use of medical services
On the whole our data on utilisation of medical services did not tend to follow trends in reported prevalence. There was only a small non‐significant increase in the proportion visiting the GP at his/her surgery with wheezing in the past year and no evidence of an increase in outpatient attendance. According to Sunderland and Fleming2,3 and based on data from the Weekly Returns Service (WRS), our two studies straddle a period during which GP consultation rates for acute asthma episodes in children reached a peak in 1993 returning to levels seen in the late 1980s by the year 2000.2,3 It is also a period during which paediatric medical hospital episode rates for England rose16 but hospital admission rates for asthma in children fell both locally and nationally (fig 1). However, medical service utilisation data may not only be influenced by the underlying prevalence of disease. Trends may also depend on changes in the provision of medical services—for example, the introduction of nurse run asthma clinics and the updating of British Thoracic Society (BTS) guidelines on asthma management2,17—and on how patients access medical care and, in the case of the WRS data, changes in the frequency of acute attacks.
The proportion of children in Croydon reportedly attending casualty for wheeziness was, however, higher in 2002 than in 1991, raising the possibility that some children may now be taken to casualty for an acute attack whereas in the past they would have been taken to the GP. The recent emergence of out‐of‐hours doctors' surgeries situated next to accident and emergency departments (such as CROYDOC) may also have had an impact on how patients access medical care and may have introduced some misclassification into our 2002 figures. In the few instances where such visits were specified, they were excluded from the home interview data on casualty attendance but a similar adjustment could not be made to the data collected at screen.
In conclusion, our study provides evidence of an increase in the prevalence of asthma among British primary school children between 1991 and 2002, although the possibility that the rate of increase slowed or reached some sort of plateau at the end of the decade cannot be excluded. There are indications that this increase was restricted to allergic asthma. The absence of a corresponding increase in health services utilisation data may reflect more widespread prophylactic treatment and/or changes in the use and provision of medical services.
Acknowledgements
The authors thank Melanie Chesnokov, Rahat Rafiq and Maria Kirwan for organising the distribution and collection of screening questionnaires, for conducting home interviews and for their assistance with data entry; Emma Pole, Vivienne Monk and Jenny Teeling for administrative help; the staff and children of the Croydon schools in 2002, 1991 and 1978 without whose help and support these serial prevalence studies would not have been completed; and Ramyani Gupta from the Lung and Asthma Information Agency for providing routine data on hospital admission rates and data on wheeze prevalence from the Heath Survey for England.
Footnotes
Funding: The 2002 follow up study was unfunded. The 1991 study was funded by the National Asthma Campaign.
Competing interest: BKB owns shares in GlaxoSmithKline.
References
- 1.Anderson H R, Gupta R. Trends in asthma. In: Partridge MR, Miles A, eds. The effective management of asthma. London: Aesculapius Medical Press, 20023–17.
- 2.Fleming D M, Sunderland R, Cross K W.et al Declining incidence of episodes of asthma: a study of trends in new episodes presenting to general practitioners in the period 1989–98. Thorax 200055657–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sunderland R S, Fleming D M. Continuing decline in acute asthma episodes in the community. Arch Dis Child 200489282–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kwong G N M, Proctor A, Billings C.et al Increasing prevalence of asthma diagnosis and symptoms in children is confined to mild symptoms. Thorax 200156312–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Devenny A, Wassall H, Ninan T.et al Respiratory symptoms and atopy in children in Aberdeen: questionnaire studies of a defined school population repeated over 35 years. BMJ 2004329489–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sproston K, Primatesta P. eds. Health survey for England 2002. Summary of key findings; Volume 1: The health of children and young people. London: The Stationery Office, 2003
- 7.Strachan D P, Anderson H R. Trends in hospital admission rates for asthma in children. BMJ 1992304819–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson H R, Butland B K, Strachan D P. Trends in prevalence and severity of childhood asthma. BMJ 19943081600–1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Armitage P, Berry G.Statistical methods in medical research. 2nd ed. Oxford: Blackwell Scientific Publications, 1990
- 10.Anderson H R, Butland B K, Paine K M.et al Trends in the medical care of asthma in childhood; Croydon 1978 and 1991. Thorax 199348451 [Google Scholar]
- 11.Anderson H R, Ruggles R, Strachan D P.et al Trends in prevalence of symptoms of asthma, hayfever and eczema in 12–14 year olds in the British Isles, 1995–2002: a questionnaire survey. BMJ 20043281052–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kuehni C E, Davis A, Brooke A M.et al Are all wheezing disorders in very young (preschool) children increasing in prevalence? Lancet 20013571821–1825. [DOI] [PubMed] [Google Scholar]
- 13.Suissa S, Ernst P, Kezouh A. Regular use of inhaled corticosteroids and long term prevention of hospitalisation for asthma. Thorax 200257880–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burney P. The changing prevalence of asthma? Thorax 200257(Suppl 2)ii36–ii39. [PMC free article] [PubMed] [Google Scholar]
- 15.Strachan D P. The role of environmental factors in asthma. Br Med Bull 200056865–882. [DOI] [PubMed] [Google Scholar]
- 16.MacFaul R, Werneke U. Recent trends in hospital use by children in England. Arch Dis Child 200185203–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.British Thoracic Society British Paediatric Association, Research Unit of the Royal College of Physicians of London, et al. Guidelines on the management of asthma. Thorax 199348(Suppl)S1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]