Abstract
Background
The natural history of bronchial preinvasive lesions and the risk of developing lung cancer in patients with these lesions are not clear. Previous studies have treated severe dysplasia and carcinoma in situ (CIS) on the assumption that most will progress to invasive carcinoma.
Aims
To define the natural history of preinvasive lesions and assess lung cancer risk in patients with these lesions.
Hypothesis
Most preinvasive lesions will not progress to invasive carcinoma but patients with these lesions will be at high risk.
Methods
A cohort of patients with preinvasive lesions underwent fluorescence bronchoscopy every 4–12 months and computed tomography of the chest annually. The main end point was the development of invasive carcinoma.
Results
22 patients with 53 lesions were followed up for 12–85 months. 11 cancers were diagnosed in 9 patients. Of the 36 high‐grade lesions (severe dysplasia and CIS), 6 progressed to invasive cancers. 5 separate cancers developed at remote sites in patients with high‐grade lesions. All cancers were N0M0 and curative treatment was given to 8 of the 9 patients. The cumulative risk of developing lung cancer in a patient with a high‐grade lesion was 33% and 54% at 1 and 2 years, respectively. Of the 17 low‐grade lesions, none progressed to invasive carcinoma.
Conclusions
Although the risk of malignant progression of individual preinvasive lesions is relatively small, patients with high‐grade lesions are at high risk of lung cancer. Surveillance facilitated early detection and treatment with curative intent in most patients.
Lung cancer continues to carry a poor prognosis.1 Although 5‐year survival prospects are relatively good for early‐stage disease,2 most patients are diagnosed with advanced disease when curative treatment is not feasible.3 This has prompted the development and refinement of several sensitive diagnostic tests that will facilitate detection and treatment at earlier stages.
Fluorescence bronchoscopy has been developed to enhance the detection of preinvasive lesions involving the large airways.4,5 Preinvasive lesions, such as severe dysplasia and carcinoma in situ (CIS), are believed to be precursors of squamous cell carcinoma. However, understanding of their natural history is incomplete because of the previous difficulties of detection using conventional white light bronchoscopy. With the development of fluorescence bronchoscopy, it is now possible to locate these lesions, and this has created a dilemma as to how they should be managed.6
Several studies have recently been undertaken using fluorescence bronchoscopy,7,8,9,10 but all have treated the most severe lesions (severe dysplasia and/or CIS) and this has complicated the interpretation of their natural history. Evidence from postmortem studies conducted by Auerbach et al11 40 years ago, however, suggests that most CIS lesions may not progress to invasive carcinoma. Serial sections obtained from the airways showed CIS in as many as 75% of individuals with heavy smoking histories.11 As CIS is implicated only in the development of squamous cell carcinoma and as only 10% of heavy smokers are likely to develop lung cancer, Auerbach et al11 argued that most lesions were unlikely to progress to clinically relevant lung cancers. However, patients with preinvasive lesions may still be at high risk, as they have been reported to develop cancers at other sites within their lungs.12
We have undertaken a longitudinal study of patients with bronchial dysplasia and CIS, in which we have maintained combined surveillance with fluorescence bronchoscopy and computed tomography of the chest. Treatment was given as soon as a diagnosis of invasive carcinoma was made. The main aims were to define the natural history of preinvasive lesions and assess the risk of developing lung cancer in patients with these lesions. Our hypothesis was that most lesions would not progress to invasive carcinoma but that patients bearing these lesions would be at high risk of lung cancer. Preliminary findings from this study have already been reported.13
Methods
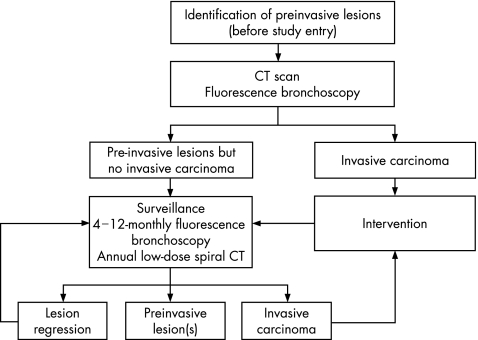
Figure 1 summarises the study protocol that was approved by the University College London Hospitals medical ethics committees.
Figure 1 Surveillance protocol for patients with preinvasive lesions involving the bronchial epithelium. Fluorescence bronchoscopies were performed at 4–12‐monthly intervals depending on the grade of the preinvasive lesion: patients with high‐grade lesions (severe dysplasia and carcinoma in situ) underwent bronchoscopy at 4–6‐monthly intervals, whereas those with low‐grade lesions (mild to moderate dysplasia) had bronchoscopies at 6–12‐monthly intervals. CT, computed tomography.
Patient selection
A total of 84 patients received fluorescence bronchoscopy, of whom 22 met the study entry criteria. Table 1 lists the patients, most of whom were referred from other hospitals, and their condition for assessment. All patients with preinvasive lesions underwent spiral computed tomography of the chest with the intention of excluding tumour adjacent to the preinvasive lesion and at remote sites within the lung. Only patients without such evidence of invasive disease entered the study.
Table 1 Patient characteristics (patient demographics, lung cancer risk factors and the circumstances leading to the detection of preinvasive lesions are listed for each patient enrolled in the surveillance study).
| Patient number (code) | Age (years) | Sex | Smoking (pack‐years) | Additional risk factors | Previous malignancy | Reasons for referral |
|---|---|---|---|---|---|---|
| 1 (001) | 75 | M | 90 | COPD | None | Haemoptysis |
| 2 (002) | 73 | F | 40 | None | CIS of breast excised 1 year previously | Haemoptysis |
| 3 (003) | 69 | M | 40 | COPD | None | Persistent cough |
| 4 (004) | 62 | M | 106 | COPD | None | Haemoptysis |
| 5 (005) | 54 | M | 38 | None | None | Persistent cough |
| 6 (006) | 61 | M | 141 | None | None | Pneumonia |
| 7 (007) | 67 | M | 104 | Asbestos exposure, COPD | None | Persistent cough |
| 8 (008) | 62 | M | 96 | COPD | None | Haemoptysis |
| 9 (009) | 66 | M | 88 | COPD | SCLC, chemotherapy or radiotherapy 8 years previously | Persistent cough |
| 10 (010) | 74 | M | 60 | Asbestos exposure, COPD | NSCLC, pneumonectomy 2 years previously | Persistent cough, abnormal sputum cytology |
| 11 (011) | 75 | M | 80 | COPD | NSCLC, lobectomy 2 years previously | Haemoptysis |
| 12 (012) | 61 | M | 60 | None | NSCLC, lobectomy 3 years previously | Haemoptysis |
| 13 (013) | 53 | F | 96 | None | NSCLC, lobectomy 6 months previously | CIS at resection margin |
| 14 (014) | 74 | M | 62 | Asbestos exposure, COPD | NSCLC, lobectomy 6 months previously | CIS at resection margin |
| 15 (015) | 57 | F | 22 | None | NSCLC, lobectomy 6 months previously | SD at the resection margin |
| 16 (016) | 60 | M | 40 | COPD | SCLC, chemotherapy or radiotherapy 6 months previously | Persistent cough |
| 17 (017) | 67 | M | 47 | Asbestos exposure, COPD | NSCLC, lobectomy 6 months previously | CIS at resection margin |
| 18 (018) | 62 | M | 48 | COPD | None | Pneumonia |
| 19 (019) | 70 | M | 120 | COPD | None | Persistent cough |
| 20 (020) | 54 | M | 45 | None | None | Persistent cough |
| 21 (021) | 49 | M | 62 | Asbestos exposure | None | Haemoptysis |
| 22 (022) | 60 | M | 0 | Asbestos exposure | None | Persistent cough, abnormal sputum cytology |
CIS, carcinoma in situ; COPD, chronic obstructive pulmonary disease; F, female; M, male; NSCLC, non‐small‐cell lung cancer; SCLC, small‐cell lung cancer; SD, severe dysplasia.
Patients are numbered from 1 to 22.
The relevance of preinvasive lesions and treatment options were discussed, and informed consent was obtained at study entry. Patients were ineligible for the study if they had any disorder affecting their short‐term prognosis or ability to tolerate bronchoscopy or biopsy.
Fluorescence bronchoscopy
The initial fluorescence bronchoscopy was performed under general anaesthesia by passing the bronchoscope (D‐Light autofluorescence bronchoscope; Karl Storz GmbH, Tuttlinger, Germany) inside a rigid bronchoscope. The bronchial tree was first inspected under white light and then under blue light. All areas that appeared abnormal were initially documented and sampled when the bronchoscopy examination was completed. Samples for cytology were obtained using a bronchial brush and saline washings. Bronchial biopsies for histology were then obtained using flexible disposable forceps, a minimum of five specimens were taken from each site to minimise the risk of overlooking foci of invasive disease. Control biopsy specimens were obtained from areas negative for both modalities. Separate forceps were used for each site to eliminate the risk of cross‐contamination. Although rigid bronchoscopy has the potential to miss lesions within the subglottic trachea, this technique enables biopsy specimens to be obtained from multiple sites without additional patient discomfort.
Subsequent bronchoscopies were performed under sedation with intravenous midazolam and topical lignocaine. Bronchial biopsy specimens, brush specimens and washings were obtained from sites that appeared abnormal and from sites of previously documented preinvasive lesions. Additional sites were recorded as distinct lesions when separated by normal mucosa. The same operator (PJG) performed all surveillance bronchoscopies and biopsies to facilitate consistency of sampling throughout the study.
Patients with mild to moderate dysplasia underwent bronchoscopy every 6–12 months as reported previously8,9,10 (fig 1). In patients with CIS and severe dysplasia, bronchoscopic surveillance was performed every 4–6 months on the assumption that these intervals would be sufficient to identify progression to invasive carcinoma without compromising the possibility of curative treatment.
Imaging
Annual low‐dose non‐enhanced spiral computed tomography scan of the thorax was performed to check for the development of incidental cancers within the lung parenchyma. Patients were scanned with a Siemens' Sensation 4 Channel detector multislice scanner (Siemens', Bracknell, UK). The dose was reduced by decreasing the tube current to 50–70 mA. Solitary pulmonary nodules of ⩽1 cm diameter were investigated by repeat computed tomography after an interval of 3–4 months to check for a change in shape or size that might suggest a malignant aetiology. Lesions ⩾1 cm in diameter were imaged by positron emission tomography (PET).
End points
The main end point of the study was the development of invasive carcinoma. Although this was based primarily on histological evidence, clinical suspicion was also accepted. In patients with lesions involving the large airways, histological evidence was obtained. However, clinical diagnoses were made in patients with peripheral lesions who were not fit to undergo tissue biopsies and were based on interval computed tomography scans showing an increase in lung nodule size in association with abnormal uptake on PET. Patients who developed lung cancer were treated promptly after discussion in a multidisciplinary lung cancer clinic and remained under surveillance if their treatment was given with curative intent. Surveillance was discontinued if they developed evidence of recurrent invasive disease.
Histology
Multiple sections from all biopsy specimens were examined by two histopathologists (FP or MF) and verified by a reference pathologist (AGN) who reviewed the same slides. The diagnosis of the reference pathologist was accepted in cases of disagreement. The histological appearances were classified according to the World Health Organization criteria.14 Biopsy specimens from sites of previous lesions that showed no abnormality or a lesser grade of dysplasia on at least two consecutive occasions were considered to indicate regression of the lesion.
Analysis
Preinvasive lesions were subdivided into high‐grade (CIS and severe dysplasia) and low‐grade (mild and moderate dysplasia) lesions. Data were censored when follow‐up ceased or when a patient received treatment that might affect the natural history of that lesion. The probability of a patient developing an invasive carcinoma was estimated with the Kaplan–Meier analysis. Some patients developed >1 invasive carcinoma during surveillance but the analysis was confined to the time the first tumour was detected.
Results
Patients, lung cancer risk factors and clinical presentations
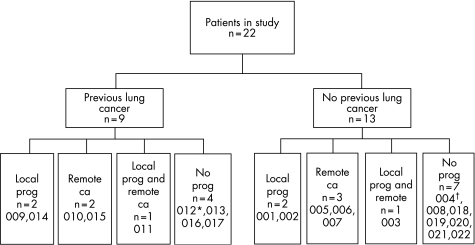
Twenty two patients (mean age 64 years; 19 men) entered the study and were followed up for 12–85 months (median 23 months). All but one gave significant smoking histories. Table 1 summarises the demographics, clinical presentations and circumstances leading to the discovery of preinvasive lesions in patients. Six patients had low‐grade lesions only, whereas the remaining 16 had both high‐grade and low‐grade lesions. Nine patients had been successfully treated for a previous lung cancer, whereas 13 had no such history; there were no marked differences between these groups, except that patients with only low‐grade lesions at study entry were most often in the “no previous lung cancer” category (fig 2).
Figure 2 Distribution of histological outcomes. Of the 22 patients, 9 had previous lung cancer and 13 had no previous cancer. Each group is divided into (1) patients who showed local progression from a preinvasive lesion to carcinoma (local prog), (2) patients who developed a carcinoma at a site remote from the detectable preinvasive disease (remote ca), (3) patients with both local progression (local prog) and a remote carcinoma (remote ca) and (4) patients with no progression of their preinvasive disease. The numbers of each are shown in the lowest tier of boxes together with the patients' code numbers. Tables 1 and 2 give these cross‐references with the study numbers. Those in italics are patients with low‐grade lesions at study entry. As this study was closed, patient 012 (designated*) developed local progression to carcinoma; patient 004 (designated†) developed carcinoma at a remote site.
In all, 36 high‐grade lesions (7 of severe dysplasia and 29 of CIS) were identified in 16 patients: 23 were detected with fluorescence bronchoscopy at study entry, whereas 11 new lesions developed during surveillance in sites that had previously been judged to be normal. Another two high‐grade lesions were detected in two patients at conventional bronchoscopy before study entry, and subsequently verified by independent histological review of their biopsy specimens, but regressed by the time of the initial fluorescence bronchoscopy.
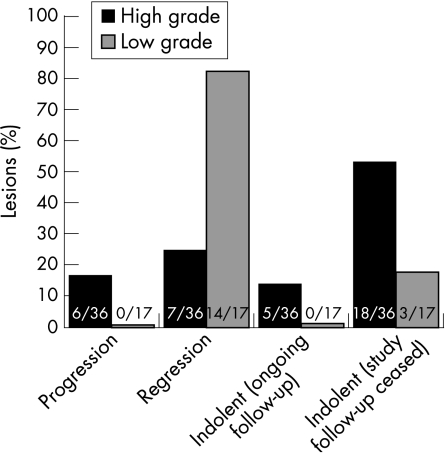
Of the 36 high‐grade lesions, six progressed to invasive squamous cell carcinoma at intervals ranging from 4 to 17 months, whereas seven lesions, including two lesions detected before study entry, appeared to regress to normal or to a lesser grade of dysplasia (fig 3). The remaining 23 lesions persisted with unchanged histology for 6–50 months, although follow‐up ceased in 18 lesions when patients received treatments that might have affected their behaviour (table 3).
Figure 3 Outcomes of surveillance in 36 high‐grade (black bars) and 17 low‐grade (grey bars) preinvasive lesions. A large number of lesions persisted with unchanged histology during surveillance, although follow‐up ceased in some of these patients when treatments were given to adjacent carcinomas that may have influenced their behaviour.
Table 3 Circumstances leading to the censorship of high‐grade preinvasive lesions during surveillance.
| Patient identity code | Reasons for censorship | Preinvasive lesions affected (n) | Duration of surveillance (months) |
|---|---|---|---|
| 007 | Upper lobectomy for synchronous carcinoma in the same lobe | 1 | 19 |
| 005 | Radical external radiotherapy to synchronous carcinoma in the same lung | 2 | 8 |
| 003 | PDT to synchronous carcinoma in the same lung | 3 | 6 |
| 003 | Chemotherapy for recurrent cancer in the contralateral lung | 1 | 10 |
| 002 | Lower lobectomy for synchronous carcinoma in the same lung, with sleeve resection and reimplantation of the upper lobe after removing proximal preinvasive lesions | 4 | 19 |
| 001 | PDT to the adjacent synchronous carcinoma | 1 | 4 |
| 014 | Surgery to correct postoperative bronchial stricture with removal of lesion | 1 | 11 |
| 010 | Radical external radiotherapy to synchronous carcinoma in the same lung | 4 | 22 |
| 011 | Radical endobronchial radiotherapy to synchronous carcinoma in the same lung | 1 | 20 |
PDT, photodynamic therapy.
Surveillance was discontinued in 18 high‐grade preinvasive lesions when patients received treatment that might influence the outcome of the lesion. The duration of follow‐up and the reasons for censorship are given for each patient.
Seventeen low‐grade lesions were detected in nine patients (fig 3). Three patients had synchronous high‐grade lesions and the remaining six patients had only low‐grade lesions. Twelve low‐grade lesions were detected at study entry and five developed during surveillance at sites that had previously appeared normal. None progressed to invasive carcinoma, whereas 14 spontaneously regressed to normal. The remaining three lesions (all in the same patient) remained indolent, although follow‐up ceased after 12 months as a result of deteriorating lung function.
Incidental lung cancers detected during surveillance
Five patients (all with high‐grade lesions) developed incidental lung cancers at remote sites and were detected by computed tomography (fig 2, table 2). Three patients underwent surgery and were found to have squamous cell carcinomas. The remaining two patients developed mass lesions that were judged to be primary lung cancers on the basis of their appearance on computed tomography and PET, but a biopsy specimen could not be examined or removed surgically, and so a histological diagnosis was not obtained. None of the six patients with only low‐grade lesions developed incidental cancers during surveillance.
Table 2 Treatment and patient outcomes. Details of 11 lung cancers diagnosed in nine patients during the surveillance study.
| Patient code | Time to diagnosis (months) | Tumour site | Histology | How diagnosed | Stage | Treatment | Outcome after treatment |
|---|---|---|---|---|---|---|---|
| 001 | 3 | Trachea | sq cell ca | FB: progressed from known CIS | (C) T4N0M0 | PDT | Eradicated: no evidence of recurrence |
| 11 | RUL | sq cell ca | FB: progressed from new CIS | (C) T1N0M0 | Radical RT | Progressive disease | |
| 002 | 15 | LLL | sq cell ca | Clinical suspicion: progressed from known CIS | (S) T1N0M0 | Surgery | Alive: no evidence of recurrent disease after 5 years |
| 003 | 5 | RML | sq cell ca | FB: progressed from known CIS | (C) T1N0M0 | Radical RT (PDT unsuccessful) | Progressive disease |
| 005 | 8 | RUL | Not known | CT surveillance followed by | (C) T1N0M0 | Radical RT | Alive: no evidence of recurrence after 3 years |
| PET:CT scan | |||||||
| 006 | 19 | LLL | sq cell ca | CT surveillance, followed by | (S) T1N0M0 | Surgery | Alive: no evidence of recurrence after 1 year |
| PET scan | |||||||
| 007 | 6 | RUL | sq cell ca | CT surveillance, followed by | (S) T1N0M0 | Surgery | Progressive disease |
| PET scan | Alive after 1 year | ||||||
| 009 | 4 | LUL | sq cell ca | FB: progressed from known CIS | (C) T1N0M0 | PDT: refused surgery and ineligible for radical RT | Progressive disease |
| 010 | 17 | LLL | Not known | CT surveillance | (C) T1N0M0 | Symptomatic: unfit for surgery/RT due to previous pneumonectomy | Progressive disease |
| 011 | 14 | LL lobectomy stump | sq cell ca | FB: progressed from known CIS | (C) T1N0M0 | Radical brachytherapy | Eradicated: no recurrence after 1 year |
| 14 | RLL | sq cell ca | CT surveillance, followed by | (S) T1N0M0 | Surgery | No evidence of recurrence after 1 year | |
| PET:CT scan |
(C), clinical staging and (S), surgical staging; CIS, carcinoma in situ; CT, computed tomography; FB, fluorescence bronchoscopy; LLL, left lower lobe; LUL, left upper lobe; PDT, photodynamic therapy; PET, positron emission tomography; RLL, right lower lobe; RML, right middle lobe; RT, radiotherapy; RUL, right upper lobe; sq cell ca, squamous cell carcinoma; TNM, tumour‐node‐metastasis.
Staging is according to the international staging system.2
Clinical outcomes in patients with invasive lung cancers
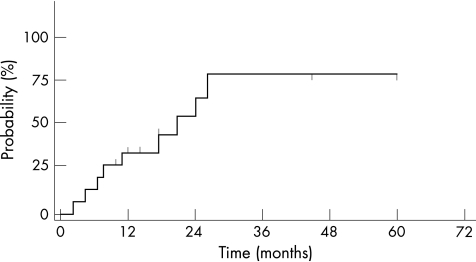
Eleven lung cancers were detected in nine patients, all of whom were known to have high‐grade lesions (table 2). Although the risk of developing a lung cancer was negligible in patients with only low‐grade lesions, it was estimated to be 33% at 1 year and 54% at 2 years in patients with high‐grade lesions (fig 4).
Figure 4 Kaplan–Meier plot indicating the estimated probability of invasive lung cancer developing at any site in the lungs of patients with high‐grade lesions.
All tumours were N0M0 at the time of diagnosis, and all were stage 1a with the exception of a patient with a primary tracheal tumour, which was stage 111b (patient 001 in table 2). It was possible to offer potentially curative treatment to all patients, with the exception of one who had previously undergone a pneumonectomy and who developed a second primary cancer in the periphery of the remaining lung (patient 010 in table 2). This patient received supportive care but has since died. Of the remaining 10 lung cancers in eight patients, four have recurred in four patients of whom three are dead. There is no evidence of recurrent disease in the remaining four patients after 14–60 months.
Discussion
Our study supports the hypothesis that most of the high‐grade preinvasive lesions do not progress to invasive carcinoma, but patients bearing these lesions are at extremely high risk of developing lung cancer (fig 4). Our findings also show the potential of surveillance with fluorescence bronchoscopy and computed tomography of the chest to detect lung cancers in such high‐risk patients at early stages when treatment with curative intent is feasible.
Previous studies on preinvasive lesions have treated severe dysplasia and CIS because of concerns that a large proportion would progress to invasive carcinoma.7,8,9,10,15 In our study, treatment was withheld until there was histological or radiological evidence of progression to invasive carcinoma in order to evaluate their malignant potential as precisely as possible. Although the outcome of high‐grade lesions was variable, only a minority progressed to invasive carcinoma in the first 2 years (fig 3). A similar proportion of high‐grade lesions regressed to normal, whereas the remainder persisted with unchanged histology for long periods of time (fig 3). In addition, new lesions appeared during the course of surveillance, and it has not been possible to predict which lesion is destined to progress to invasive carcinoma from the initial histology.
These findings differ from those of Venmans et al and Breuer et al7,10 who reported that all CIS lesions progressed to squamous cell carcinoma. However, comparison between studies may be complicated by the classification of preinvasive lesions. We have found that sequential biopsy specimens from the same site may be scored as severe dysplasia or CIS (unpublished observations). In addition to intraobservational and interobservational variation, there may also be morphological heterogeneity within lesions. Further, we found no difference in the outcomes of lesions classified as severe dysplasia or CIS at initial presentation.16 We therefore find it appropriate to group these two grades together.
In our study, no low‐grade lesions progressed to carcinoma (fig 3) or to a higher grade (results not shown) unlike those observed in the study by Breuer et al10 who described a 9% (6/64) progression rate for mild–moderate dysplasia followed up for a median of 21 months. The reasons for these discrepancies are unknown but could be elucidated in a large multicentre study with a longer follow‐up.
Our study has two important limitations. Firstly, it has been assumed that preinvasive lesions in patients with previous histories of lung cancer behave similarly to those in patients with no such histories. Although there is no apparent difference between these two groups (fig 2), a larger study with a longer follow‐up is needed to establish whether this assumption is correct. Secondly, it is assumed that biopsy specimens taken from preinvasive lesions do not influence the outcome of that lesion. However, it has been suggested that bronchial biopsies may completely remove some lesions.7 Although this possibility cannot be discounted, this is unlikely as most lesions appeared considerably larger than the area sampled by biopsy. This could be considered in a future study by using non‐invasive techniques, such as endobronchial ultrasound and optical coherence tomography. It is likely, however, that treatment given to invasive carcinomas will have affected the behaviour of preinvasive lesions adjacent to these carcinomas. Follow‐up data from these lesions were therefore censored at the time of treatment (table 3). Although a large proportion of data were discarded, our assessments of the behaviour of preinvasive lesions are consistent with the conclusions made by Auerbach et al.11
Despite this relatively low rate of malignant progression of individual lesions (fig 3), we found that patients with high‐grade lesions are at extremely high risk of developing invasive carcinoma (fig 4). This high risk is because of the multifocal distribution of lesions and the development of incidental cancers at remote sites within the lung. These findings are consistent with the “field cancerisation” concept, in which the entire bronchial epithelium is exposed to the carcinogenic effects of tobacco smoke and is therefore at risk of progressing to invasive carcinoma.17
The observation of multifocal disease and the large proportion of patients developing incidental cancers at remote sites within their lungs raises important questions as to how high‐grade lesions and patients should be managed clinically. Treatment options presently include surgery and a variety of endobronchial treatments. Surgery undoubtedly provides the most effective method of eradicating lesions, but is associated with considerable morbidity and mortality, which is difficult to justify for a condition that may not necessarily progress to malignancy. Further, there is a risk that it may render the patient unfit for curative treatment if an invasive carcinoma subsequently develops within the remaining lung.
Endobronchial treatments have the advantage of conserving lung tissue and are used more widely. However, their efficacy is difficult to evaluate, given the unpredictable nature of high‐grade lesions and the observation that patients with these lesions are just as likely to develop incidental cancers at remote sites within their lungs. Ultimately, systemic treatments aimed at preventing the progression to invasive carcinoma may be more appropriate for such a field‐change disease.
Maintaining combined surveillance with computed tomography and bronchoscopy ensures that definitive treatment has been directed to the most appropriate site within the patient's airway and that incidental lung cancers have been diagnosed and treated early. Nevertheless, four of the eight patients developed metastatic disease despite receiving treatment with curative intent. Three cancers progressed from known preinvasive lesions (table 2), and it could be argued that preemptive treatment would have prevented this. However, three studies have reported high rates of tumour progression, ranging from 17% to 67%, despite endobronchial treatment,7,9,15 and underline the importance of conducting randomised controlled clinical trials to evaluate different treatment strategies.
The evidence of variable outcomes in preinvasive lesions also highlights the need to identify reliable markers of tumour progression. We have established an archive of blood, sputum and bronchoscopic specimens so that it is now possible to conduct molecular biological studies on histologically identical lesions with different clinical outcomes.18 In addition to identifying markers of disease progression, this study also provides new insights into the biology of the invasion process.
Although our main aim was to study the natural history of preinvasive lesions, the finding of such a high risk of lung cancer in patients with severe dysplasia and CIS suggests that the lesions have potential as disease biomarkers. The clinical value of fluorescence bronchoscopy may therefore lie in its ability to identify patients at especially high risk of developing lung cancer by detecting these lesions. Although bronchoscopy is too invasive and time consuming to be developed as a screening tool, evidence suggests that patients with preinvasive lesions may be identified non‐invasively with sputum cytometry.19 Screening with sputum cytometry, combined with surveillance, may therefore facilitate the diagnosis of lung cancers at earlier stages when curative treatment is feasible in high‐risk groups.
Acknowledgements
We acknowledge the helpful comments of Professor S Spiro and Dr Allan Hackshaw during the preparation of this manuscript.
Abbreviations
CIS - carcinoma in situ
PET - positron emission tomography
Footnotes
Funding: The work was supported by the University College London Hospitals Charitable Foundation. Karl Storz GmbH, Germany, supported the project with the unconditional loan and maintenance of the fluorescence bronchoscope. AKB was supported by a grant from the Ellermann Foundation. PHR was supported by MRC Programme grant number G9703123. FP was supported by Cancer Research UK.
Competing interests: None.
References
- 1.Toms J R. ed. CancerStats Monograph 2004. London: Cancer Research UK, 2004
- 2.Mountain C F. Revisions in the international system for staging lung cancer. Chest 19971111710–1717. [DOI] [PubMed] [Google Scholar]
- 3.Bulzebruck H, Bopp R, Drings P.et al New aspects in the staging of lung cancer: prospective validation of the international union against cancer TNM classification. Cancer 1992701102–1110. [DOI] [PubMed] [Google Scholar]
- 4.Lam S, Kennedy T, Unger M.et al Localization of bronchial intraepithelial neoplastic lesions by fluorescence bronchoscopy. Chest 1998113696–770. [DOI] [PubMed] [Google Scholar]
- 5.Kennedy T C, Lam S, Hirsch F. Review of recent advances in fluorescent bronchoscopy in early localisation of central airway lung cancer. Oncologist 20016257–262. [DOI] [PubMed] [Google Scholar]
- 6.Banerjee A K, Rabbitts P H, George P J. Are all high‐grade preinvasive lesions premalignant, and should they all be treated? Am J Respir Crit Care Med 20021651452–1453. [DOI] [PubMed] [Google Scholar]
- 7.Venmans B J, van Boxem T J, Smit E F.et al Outcome of bronchial carcinoma in situ. Chest 20001171572–1576. [DOI] [PubMed] [Google Scholar]
- 8.Bota S, Auliac J B, Paris C.et al Follow‐up of bronchial precancerous lesions and carcinoma in situ using fluorescence endoscopy. Am J Respir Crit Care Med 20011641688–1693. [DOI] [PubMed] [Google Scholar]
- 9.Moro‐Sibilot D, Fievet F, Jeanmart M.et al Clinical prognostic indicators of high‐grade pre‐invasive bronchial lesions. Eur Respir J 20042424–29. [DOI] [PubMed] [Google Scholar]
- 10.Breuer R H, Pasic A, Smit E F.et al The natural course of pre neoplastic lesions in bronchial epithelium. Clin Cancer Res 200511537–543. [PubMed] [Google Scholar]
- 11.Auerbach O, Stout A P, Hammond E C.et al Changes in bronchial epithelium in relation to cigarette smoking and in relation to lung cancer. N Engl J Med 1961265255–267. [DOI] [PubMed] [Google Scholar]
- 12.Pairolero P C, Williams D E, Bergstralh E J.et al Postsurgical stage I bronchogenic carcinoma: morbid implications of recurrent disease Ann Thorac Surg 198438331–338. [DOI] [PubMed] [Google Scholar]
- 13.Banerjee A K, Rabbitts P H, George J. Pre‐invasive bronchial lesions: surveillance or intervention. Chest 2004125S95–S96. [DOI] [PubMed] [Google Scholar]
- 14.Travis W D, Colby T V, Corrin B.et alWorld Health Organization international histological classification of tumours. Histological typing of lung and pleural tumours. 3rd edn. London: Springer, 1999
- 15.Deygas N, Froudarakis M, Ozenne G.et al Cryotherapy in early superficial bronchogenic carcinoma. Chest 200112026–31. [DOI] [PubMed] [Google Scholar]
- 16.McCaughan F, Banerjee A K, Nichoson A G.et al Does the grade of pre‐invasive bronchial lesion predict outcome? Proc Am Thorac Soc 20052A118 [Google Scholar]
- 17.Vauthey J N, Walsh G L, Vlastos G.et al Importance of field cancerisation in clinical oncology. Lancet Oncol 2000115–16. [DOI] [PubMed] [Google Scholar]
- 18.Foster N A, Banerjee A K, Xian J.et al Somatic genetic changes accompanying lung tumour development. Genes Chromosomes Cancer 20054465–75. [DOI] [PubMed] [Google Scholar]
- 19.Xing S, Khanavkar B, Nakhosteen J A.et al Predictive value of image cytometry for diagnosis of lung cancer in heavy smokers. Eur Respir J 200525956–963. [DOI] [PubMed] [Google Scholar]