Abstract
Background
Long‐standing rheumatoid arthritis produces unique challenges when assessing damage due to joint deformity. The use of extremity magnetic resonance imaging (eMRI) offers the possibility of improved disease assessment because of greater patient tolerability.
Objectives
The aim of this cross‐sectional study was to compare the identification of wrist erosions in a severe rheumatoid arthritis cohort by eMRI with a restricted field of view (eMRI‐RV) to radiography and high field MRI, using the latter as the reference.
Methods
Fifteen patients (87% female, median age 56 years) with active rheumatoid arthritis (median DAS28 7.01 and disease duration 11 years) on leflunomide were enrolled. Radiography of hands, eMRI‐RV (0.2 T MagneVu MV 1000) and high field MRI of unilateral wrist joints were performed.
Results
Of 86 comparable wrist joint areas, high field MRI identified 70 erosions, eMRI‐RV 32 and radiography 4. With high field MRI considered the reference, the sensitivity, specificity and accuracy of eMRI‐RV for erosions were 46%, 94% and 55%, and the corresponding values for x ray were 6%, 100% and 23%, respectively.
Conclusions
In severely damaged rheumatoid arthritis joints, sensitivity of erosion detection was markedly higher for eMRI‐RV than radiography, using high field MRI as the reference. eMRI‐RV was, however, less sensitive than high field MRI.
Magnetic resonance imaging (MRI) has become increasingly recognised as a validated outcome measure for evaluating rheumatoid arthritis.1 In terms of bone damage evaluation, the tomographic nature of MRI provides a significant improvement in sensitivity for erosion detection, as evidenced by recent studies comparing computed tomography, MRI and conventional radiographs.2,3,4 Severe rheumatoid arthritis, however, produces unique challenges when assessing disease damage using current imaging modalities. For example, plain film radiographs of the hands and feet can be difficult to interpret because of joint deformities. Using high field MRI can be problematic if there is difficult patient positioning required: for example, a prone position with an arm extended. The use of extremity MRI (eMRI) therefore offers the possibility of improved disease assessment with greater patient tolerability.5
eMRI machines have been developed primarily for use in the outpatient clinic setting. Such machines have modest space requirements with only the extremity of interest needing to be placed inside the machine, enhancing patient acceptance, reducing cost and increasing availability.6 While these provide valuable alternatives to high field machines, there are some significant trade‐offs. First, as most of the machines use a smaller magnet strength, there is a degree of compromise for image clarity as well as limitations to the field of view (FOV). The exact limitation in terms of FOV depends on the machine manufacturer: for example, in one acquisition, the MagneVu MV1000 can only scan two metacarpophalangeal (MCP) joints or one incomplete carpus whereas the Esaote C scan is capable of imaging 1–5 MCP joints or a wider view of the carpus (for example, including the distal radio‐ulnar joint).
The aim of this cross‐sectional study was to compare the identification of wrist erosions in severe rheumatoid arthritis patients between three imaging modalities: eMRI machine with a restricted field of view (eMRI‐RV), plain film radiography and high field MRI, using the latter as the reference standard.
Methods
Fifteen patients (87% female, median age 56.5 years) with rheumatoid arthritis (as defined by the ACR 1987 revised diagnostic criteria7) on leflunomide were enrolled in the study. Thirteen patients were seropositive for rheumatoid factor and the two seronegative patients were positive for anti‐CCP antibody. The median disease duration was 11 years and median number of disease‐modifying anti‐rheumatic drugs (DMARDs) per patient was 4. Five patients had received previous anti‐tumour necrosis factor α agents. The median DAS28 was 7.01 and median CRP 19.9 mg/l.
The imaging techniques were as follows. Radiography: standard posteroanterior views of both hands with film exposure centred around the third MCP joint (64 kV at 2mA/s). eMRI‐RV: three‐dimensional T1‐weighted images of the dominant wrist were obtained using a MagneVu MV1000 0.2 Tesla machine (MagneVu, Carlsbad, California, USA). The specifications were T1‐weighted spin echo (TR/TE, 100/27 ms; field of view 50×75 mm×15 mm; 2 excitations; 0.625 mm individual slice thickness (Z plane), 1 mm coronal (X and Y in‐plane) resolution. High field MRI: the dominant wrist was imaged using a Philips 1.5T Gyroscan ACS‐NT whole‐body scanner (Philips Medical Systems, Best, the Netherlands) with an 11 cm circular surface coil placed on the dorsum of the subject's wrist. Routine MRI exclusion criteria were applied. Ethical approval was granted by the local ethics committee and all participants gave their informed consent.
The high field and eMRI‐RV images were subsequently scored by an experienced reader (PGC) for the presence/absence of bone erosions at each bony site. The OMERACT definition of an MRI erosion was used which describes a sharply marginated bone lesion, with correct juxta‐articular localisation and typical signal characteristics, with a cortical break and which is visible in two adjacent planes.8 Bony sites excluded from the data presented in table 1 included the base of metacarpals 1 and 5, trapezium and pisiform as these are infrequently visualised. The radiographs were also scored in a dichotomised fashion, with presence/absence of erosions noted at all wrist bone sites including the metacarpal bases.
Table 1 Bone erosions in metacarpophalangeal joint and wrist bones: comparison between high field MRI, low field MRI and radiography.
| Examined bone* | Examined bones†, n | High field MRI | Low field MRI | x ray | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Erosions, n | Erosions, n | Sensitivity | Specificity | Accuracy | ICC‡ | Erosions, n | Sensitivity | Specificity | Accuracy | ||
| Base of MC2 | 7 | 7 | 1 | 0.14 | N/A | 0.14 | −0.058§ | 0 | 0.00 | N/A | 0.00 |
| Base of MC3 | 10 | 5 | 1 | 0.20 | 1.00 | 0.60 | 0.110 | 0 | 0.00 | 1.00 | 0.50 |
| Base of MC4 | 9 | 4 | 1 | 0.25 | 1.00 | 0.67 | 0.182 | 0 | 0.00 | 1.00 | 0.56 |
| Trapezoid | 6 | 5 | 1 | 0.20 | 1.00 | 0.33 | 0.854 | 0 | 0.00 | 1.00 | 0.17 |
| Capitate | 7 | 7 | 2 | 0.29 | N/A | 0.29 | 0.492 | 0 | 0.00 | N/A | 0.00 |
| Hamate | 10 | 8 | 4 | 0.50 | 1.00 | 0.60 | −0.009§ | 1 | 0.13 | 1.00 | 0.30 |
| Scaphoid | 7 | 6 | 4 | 0.67 | 1.00 | 0.71 | 0.714 | 0 | 0.00 | 1.00 | 0.14 |
| Lunate | 7 | 7 | 4 | 0.57 | N/A | 0.57 | 0.611 | 0 | 0.00 | N/A | 0.00 |
| Triquetrum | 10 | 10 | 5 | 0.50 | N/A | 0.50 | 0.884 | 0 | 0.00 | N/A | 0.00 |
| Distal radius | 7 | 6 | 5 | 0.83 | 0.00 | 0.71 | 0.407 | 1 | 0.17 | 1.00 | 0.29 |
| Distal ulna | 6 | 5 | 4 | 0.80 | 1.00 | 0.83 | 0.420 | 2 | 0.40 | 1.00 | 0.50 |
| Total | 86 | 70 | 32 | 0.46 | 0.94 | 0.55 | 0.689 | 4 | 0.06 | 1.00 | 0.23 |
ICC, intraclass correlation coefficient; MC, metacarpal; NA, not applicable.
*Bony sites excluded from scoring included the base of metacarpals 1 and 5, trapezium and pisiform as these are infrequently visualised.
†Where complete data for all three imaging modalities available for comparison.
‡p<0.001.
§Intraclass correlation coefficient negative due to slight inverse relation between high and low field scores for these sites (indicating poor agreement).
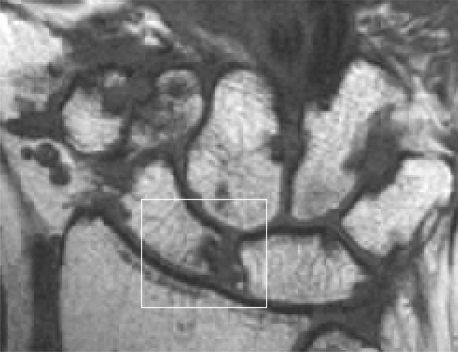
Figure 1 High field MRI: a scaphoid erosion (box).
Results
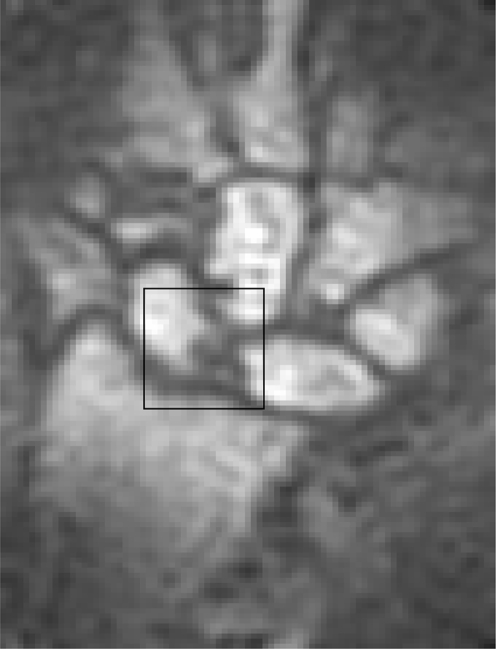
See table 1 and figs 1–3. Of 86 comparable joint areas (where the bony site was visualised by all three imaging techniques), high field MRI identified 70 erosions, eMRI‐RV 32 and radiography 4. With high field MRI considered as the reference method, the sensitivity, specificity and accuracy of eMRI‐RV for erosions were 46%, 94% and 55%, and the corresponding values for x ray were 6%, 100% and 23%, respectively. The sensitivity of eMRI‐RV was maximal at the distal radius (83%) and ulna (80%). The intraclass correlation coefficient between eMRI‐RV and high field MRI scores was 0.689 (p<0.001). Where the same number of bony sites were visualised, high field MRI identified erosions in 81% of examined bone sites compared with 37% by eMRI‐RV and 5% by radiography.
Figure 2 Low field MRI: a scaphoid erosion (box).
Of note, not all bony sites in the wrist are consistently visualised with the eMRI‐RV because of concomitant factors such as a large sized hand which exceeds its restricted FOV. When looking at sites that were regularly not imaged with eMRI‐RV (MC1 and 5, trapezium and pisiform), there were erosions seen at all these sites. When comparing erosion detection by modality (and not by bony site), high field MRI identified erosions in 81% of bony sites, eMRI‐RV in 21% and radiography in 9%.
Figure 3 Radiography: a scaphoid erosion (box).
Discussion
In this severe, long disease duration rheumatoid arthritis cohort, using high field MRI as the reference standard, sensitivity of erosion detection at the wrist was markedly higher for eMRI‐RV than radiography. eMRI‐RV, however, was less sensitive for erosion identification than high field MRI when comparing the eMRI‐RV FOV and was considerably less sensitive when compared to the conventional high field FOV. This is the first validation study comparing the MV1000 with high field MRI, although similar results for specificity of erosion detection have been demonstrated with another eMRI machine, the C scan.9 However, the sensitivity of erosion detection for the MV1000 was less than that reported for the C scan. This was probably due to poorer image quality with the MV1000 (rather than reduced FOV) as only bones visualised by both high field and eMRI‐RV were compared in the statistical analysis of this study. This highlights again the different capabilities between eMRI machines.
Previous work comparing eMRI‐RV with radiography by Crues et al10 with respect to erosion detection in wrist and MCP joints has shown the eMRI‐RV identified more bone erosions than radiography but without formal comparison to a reference standard such as high field MRI. Crues et al reported that eMRI‐RV identified erosions in 78% of bone sites assessed compared with 39% by radiography, but no formal sensitivity, specificity and accuracy data were presented for comparison between the two modalities.
The clinical ramifications of these data are worth considering. Even with its restricted FOV, eMRI offers increased sensitivity for erosion detection compared to radiography but without the issues that surround high field MRI such as access, affordability and patient tolerance. The importance of patient tolerance is paramount in a severe rheumatoid arthritis patient group where joint damage makes compliance with high field MRI imaging procedures problematic. Avoiding ionising radiation exposure in the form of x rays is also preferable in this group which otherwise will have cumulative exposure. However more research on the clinical utility and cost effectiveness of eMRI versus radiology is essential. High field MRI may be more appropriately used in clinical trials or proof‐of‐concept studies where defining patient phenotype is paramount, as opposed to clinical practice where the lesser degree of sensitivity of eMRI may be adequate.
Synovitis was not assessed in this study because the validity of evaluating synovitis using the MV1000 has not yet been reported and would require a comparison with high field MRI. In order to assess synovitis it would have been necessary to use intravenous gadolinium which is the gold standard for assessing synovitis. This adds time and some expense to the eMRI evaluation and because the major advantage of eMRI is for routine clinical practice, it would seem unlikely that gadolinium will be commonly used.
In conclusion, eMRI had a much greater sensitivity and accuracy than plain film radiography for erosion detection, with reduced sensitivity compared to high field MRI. The magnitude of the erosion detection difference has implications for both routine clinical management and clinical trials.
Acknowledgements
The authors wish to thank Phil Grice (MagneVu) for his technical advice and Centocor, Inc (especially Rebecca Bolce and Greg Keenan) for an unrestricted research grant which partially supported this work.
Abbreviations
eMRI - extremity magnetic resonance imaging
eMRI‐RV - eMRI with restricted view
FOV - field of view
MCP - metacarpophalangeal
Footnotes
Competing interests: None.
References
- 1.Conaghan P G, McQueen F M, Peterfy C G, Lassere M N, Ejbjerg B, Bird P.et al The evidence for magnetic resonance imaging as an outcome measure in proof‐of‐concept rheumatoid arthritis studies. J Rheumatol 2005322465–2469. [PubMed] [Google Scholar]
- 2.Ostergaard M, Hansen M, Stoltenberg M, Jensen K E, Szkudlarek M, Pedersen‐Zbinden B.et al New radiographic bone erosions in the wrists of patients with rheumatoid arthritis are detectable with magnetic resonance imaging a median of two years earlier. Arthritis Rheum 2003482128–2131. [DOI] [PubMed] [Google Scholar]
- 3.Perry D, Stewart N, Benton N, Robinson E, Yeoman S, Crabbe J.et al Detection of erosions in the rheumatoid hand; a comparative study of multidetector computerized tomography versus magnetic resonance scanning. J Rheumatol 200532256–267. [PubMed] [Google Scholar]
- 4.Dohn U M, Ejbjerg B J, Court‐Payen M, Hasselquist M, Narvestad E, Szkudlarek M.et al Are bone erosions detected by magnetic resonance imaging and ultrasonography true erosions? A comparison with computed tomography in rheumatoid arthritis metacarpophalangeal joints. Arthritis Res Ther 20068R110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Savnik A, Malmskov H, Thomsen H S, Bretlau T, Graff L B, Nielsen H.et al MRI of the arthritic small joints: comparison of extremity MRI (0.2 T) vs high‐field MRI (1.5 T). Eur Radiol 2001111030–1038. [DOI] [PubMed] [Google Scholar]
- 6.Cohen S. Extremity magnetic resonance imaging in rheumatoid arthritis: report of the American College of Rheumatology Extremity Magnetic Resonance Imaging Task Force. Arthritis Rheum 2006541034–1047. [DOI] [PubMed] [Google Scholar]
- 7.Arnett F, Edworthy S, Bloch D, McShane D, Fries J, Cooper N.et al The American Rheumatism Association 1987 Revised Criteria for the Classification of Rheumatoid Arthritis. Arthritis Rheum 198831315–324. [DOI] [PubMed] [Google Scholar]
- 8.Ostergaard M, Edmonds J, McQueen F, Peterfy C, Lassere M, Ejbjerg B.et al An introduction to the EULAR‐OMERACT rheumatoid arthritis MRI reference image atlas. Ann Rheum Dis. 2005;64(Suppl 1)i3–i7. [DOI] [PMC free article] [PubMed]
- 9.Ejbjerg B, Narvestad E, Jacobsen S, Thomsen H S, Ostergaard M. Optimised, low cost, low field dedicated extremity MRI is highly specific and sensitive for synovitis and bone erosions in rheumatoid arthritis wrist and finger joints: a comparison with conventional high‐field MRI and radiography. Ann Rheum Dis 2005641280–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crues J, Shellock F, Dardashti S, James T, Troum O. Identification of wrist and metacarpophalangeal joint erosions using a portable magnetic resonance imaging system compared to conventional radiographs. J Rheumatol 200431676–685. [PubMed] [Google Scholar]