Abstract
Introduction
Endothelin receptor antagonism has become an important component in the treatment of pulmonary arterial hypertension (PAH) associated with connective tissue disease (CTD). The purpose of this study was to analyse the safety and effectiveness of sitaxsentan, a selective antagonist of the ETA receptor, in a cohort of patients with PAH and CTD. Short‐term clinical and haemodynamic effects and longer‐term follow‐up data are presented.
Methods
A post hoc subgroup analysis was performed on 42 patients who had PAH associated with CTD, out of a group of 178 patients enrolled in a 12‐week, double‐blind, randomised clinical trial of sitaxsentan versus placebo. Data from 33 patients assigned to sitaxsentan 100 mg or 300 mg daily were pooled and compared with nine placebo‐treated patients. There were 41 patients entered into the blinded extension study, in which all patients received either 100 mg or 300 mg sitaxsentan once daily.
Results
Patients treated with sitaxsentan had a mean (SD) increase in 6 minute walk distance of 20 (5) m from baseline to week 12 (p = 0.037), whereas the placebo group had a decrease of 38 (84) m, resulting in a placebo‐subtracted treatment effect of 58 m (p = 0.027). Parallel improvements in quality of life and haemodynamics were also observed. No patient discontinued their drug during the 12‐week trial. In the blinded extension study (median treatment duration 26 weeks), more patients were in functional class I–II than in III–IV (p<0.001) at the end of the study compared with the start of active therapy. Elevation of hepatic transaminase levels occurred in two patients.
Conclusions
Sitaxsentan appears to be efficacious in patients with PAH associated with CTD.
Keywords: endothelin, exercise capacity, hemodynamics, pulmonary hypertension, scleroderma
Pulmonary arterial hypertension (PAH) is an increasingly recognised complication of connective tissue diseases (CTD). The prevalence of echocardiographic evidence of pulmonary hypertension has been estimated to be as high as 27% among patients with systemic sclerosis (SSc, scleroderma)1 and 12% in patients with systemic lupus erythematosus (SLE).2 Approximately 10–15% of patients with SSc have PAH. In the absence of effective treatment, rapid progression occurs, resulting in right heart failure; survival beyond 5 years is rare.3,4 Currently available therapies for PAH have had variable short‐term efficacy in the CTD population,5,6,7,8,9 with long‐term outcomes less than ideal.6,10,11 Despite aggressive treatment, 3‐year survival rate in SSc‐related PAH is ∼50%.12,13 Thus, there is an urgent need for more effective treatment regimens.
The endothelial injury characteristic of the pulmonary vasculopathy of the CTD is associated with increased levels in both plasma and tissues of the vasoconstrictor peptide, endothelin.14 Endothelin receptor antagonism has emerged as an important component of PAH therapy.15 Two distinct endothelin (ET) receptor isoforms have been identified; type A (ETA) and type B (ETB). The ETA receptor is located primarily on vascular smooth muscle cells and cardiac myocytes. Activation of ETA and ETB receptors on pulmonary vascular smooth muscle cells facilitates vasoconstriction and stimulates vascular smooth muscle cell proliferation. ETB receptors are located primarily on endothelial cells and facilitate vasodilation via release of vasodilators such as nitric oxide and prostacyclin.16 ETB receptors are also thought to be involved in the clearance of ET‐1, particularly in the vascular beds of the lung and kidney. Treatment with bosentan, an ETA/ETB receptor antagonist, has led to improvements in clinical outcomes in PAH patients overall,17,18 although the efficacy appears less robust in CTD‐related PAH.6,9,10
Selective ETA antagonism is hypothesised to offer an advantage over ETA/ETB receptor blockade, by allowing endothelial cell ETB receptor release of the vasodilators nitric oxide (NO) and prostacyclin, and clearance of ET‐1, while suppressing the vasoconstrictor and proliferative actions of the ETA receptor.19 Sitaxsentan, a selective ETA antagonist, improved 6‐minute walk distance (6MWD), New York Heart Association (NYHA) functional class and haemodynamics in patients enrolled in the Sitaxsentan To Relieve Impaired Exercise (STRIDE‐1) trial, a 12‐week, multicentre, double‐blind, randomised, placebo‐controlled trial for PAH.20 We report the effects of sitaxsentan among the subset of patients with PAH related to CTD enrolled in this trial.
Methods
The methods of STRIDE‐1 have been previously described.20 In brief, this trial enrolled patients aged 16–75 years who had symptomatic PAH despite conventional therapy if they met the following criteria: (1) symptomatic PAH that was idiopathic, related to CTD or related to congenital systemic pulmonary shunts; (2) peak oxygen uptake of 25–75% of predicted value; and (3) mean pulmonary artery pressure (MPAP) ⩾25 mmHg, mean pulmonary capillary wedge pressure (PCWPm) ⩽15 mmHg and pulmonary vascular resistance (PVR) ⩾240 dynes/sec/cm5. Exclusion criteria included portal hypertension, HIV infection, chronic liver disease or hepatic transaminase levels >1.5 times the upper limit of normal (ULN), chronic renal insufficiency and significant parenchymal lung disease. The latter was defined as a total lung capacity (TLC) of <60% of predicted value (or TLC 60–70% of predicted value with more than mild interstitial changes using high‐resolution CT of the chest) or a forced expiratory volume in 1 s of <50% of predicted value. Prior or concomitant therapy with another endothelin receptor antagonist, a prostacyclin analogue or a phosphodiesterase inhibitor was not permitted. The protocol and informed‐consent documents were approved after local institutional review at each of the 18 participating centres (17 in the US and 1 in Canada). All patients provided written informed consent (and assent if applicable) prior to enrolment.
Connective tissue disease subgroup
In STRIDE‐1, 178 patients were randomised in a 1:1:1 ratio to receive either placebo (n = 60) or sitaxsentan at an oral dose of either 100 mg (n = 55) or 300 mg (n = 63) once daily for 12 weeks. Of these patients, 42 (24%) had CTD classified as scleroderma (limited or diffuse), SLE, mixed connective tissue disease (MCTD) or overlap syndrome: 9 were on placebo, 16 on sitaxsentan 100 mg and 17 on sitaxsentan 300 mg. The primary outcome measure was the change in peak oxygen uptake on cycle ergometry. This endpoint was not met for the entire PAH cohort20 and was not analysed separately in this CTD subset. The secondary endpoints of change in 6MWD, NYHA functional class, quality of life (as measured by the Medical Outcomes Study short form (SF)‐36 questionnaire)21 and haemodynamics from baseline to week 12 were included in this analysis.
Open‐label extension phase
Subjects completing the 12‐week, double‐blind, randomised, placebo‐controlled trial were eligible to participate in the blinded extension phase (STRIDE‐1X), in which all subjects received active sitaxsentan. All patients randomised to 100 mg or 300 mg sitaxsentan in STRIDE‐1 continued with their assigned dosage. Eight of the nine placebo patients in STRIDE‐1 were equally randomised to either sitaxsentan 100 mg or 300 mg. All patients remained blinded to their doses. In total, 20 patients with CTD received sitaxsentan 100 mg and 21 received 300 mg. Change in functional class and safety and tolerability measures were assessed from the first day of active therapy to the study endpoint. STRIDE‐1X was terminated prematurely because of the occurrence of two cases of acute hepatoxicity, which were subsequently identified, after the database was locked, as restricted to the 300 mg group; neither subject had CTD. The 41 patients with CTD had a mean and median exposure to sitaxsentan of 26 weeks (range 13 days to 56 weeks).
Statistical analyses
Continuous data are presented as mean (SD) and categorical data as n (%). All 42 patients received the treatment to which they were randomly assigned. Because treatment effects of sitaxsentan 100 mg and 300 mg (versus placebo) on 6MWD, NYHA functional class and haemodynamic endpoints were similar in the entire STRIDE‐1 cohort and the CTD subset, the two sitaxsentan dosage groups were pooled in this post hoc subgroup analysis. Changes in 6MWD and other continuous variables (SF‐36 and haemodynamics) from baseline to week 12 were compared between treatment groups using analysis of covariance models adjusted for baseline value (covariate). Changes in NYHA functional class were compared between treatment groups using the Cochran–Mantel–Haenszel method adjusted for baseline value. All statistical tests were two‐sided and significance set at p<0.05; p values were not adjusted for multiple comparisons. Upon completion of the STRIDE‐1X study, for analysis of change in NYHA functional class, data was imputed using the last observation carried forward method for patients who discontinued prematurely. Patients who died during the study were given the worst functional class at end of study (class IV). Functional class at end of study was compared with baseline using the McNemar test. Statistical analyses were conducted using the SAS 8.2 statistical package (SAS Institute, Cary, North Carolina, USA).
Results
Patients
The baseline characteristics of the PAH‐CTD subgroup are shown in table 1. The placebo and patients with PAH and CTD treated with sitaxsentan were similar, with the exception of a non‐significantly increased 6MWD in the placebo‐treated group (p = 0.063) vs the active sitaxsentan‐treated group.
Table 1 Baseline characteristics of PAH‐CTD subgroup study population.
| Characteristic | Treatment group | |||||
|---|---|---|---|---|---|---|
| STRIDE‐1 | Extension† | |||||
| Placebo (n = 9) | SITAX 100/300 mg pooled data (n = 33) | SITAX 100/300 mg pooled data (n = 41) | ||||
| Age (years), mean (SD) (range) | 43 (18) (18 to 69) | 51 (11) (26 to 70) | 50 (13) (18 to 70) | |||
| Gender | ||||||
| Female, n. (%) | 8 (89) | 31 (94) | 38 (93) | |||
| Race/ethnicity, n (%) | ||||||
| White | 4 (44) | 19 (58) | 23 (56) | |||
| Hispanic | 3 (33) | 4 (12) | 6 (15) | |||
| African | 0 | 6 (18) | 6 (15) | |||
| Asian | 1 (11) | 3 (9) | 4 (10) | |||
| Other | 1 (11) | 1 (3) | 2 (5) | |||
| Type of CTD,* n (%) with | ||||||
| Scleroderma | 2 (22) | 17 (51) | 19 (46) | |||
| SLE | 5 (56) | 11 (33) | 15 (37) | |||
| MCTD or overlap syndrome | 2 (22) | 5 (15) | 7 (17) | |||
| NYHA functional class, n (%) in | ||||||
| Class II | 3 (33) | 10 (30) | 12 (29) | |||
| Class III | 6 (67) | 23 (70) | 29 (71) | |||
| Prior or concomitant treatment, n (%) | ||||||
| Warfarin | 7 (78) | 23 (70) | 30 (71) | |||
| Diuretics | 4 (44) | 23 (70) | 27 (64) | |||
| Calcium channel blockers | 5 (56) | 25 (76) | 30 (71) | |||
| Digoxin | 2 (22) | 6 (18) | 8 (19) | |||
| Supplemental oxygen | 2 (22) | 7 (21) | 9 (21) | |||
| Exercise and haemodynamic parameters | ||||||
| 6MWD, m | 414 (59) | 340 (108) | 355 (105) | |||
| VO2max, % of predicted | 44 (15) | 43 (11) | 43 (11) | |||
| Mean pulmonary arterial pressure, mmHg | 44 (8) | 46 (11) | 46 (11) | |||
| Right atrial pressure, mmHg | 7 (6) | 8 (5) | 8.3 (4) | |||
| Cardiac index, l/min/m2 | 2.4 (0.8) | 2.6 (0.8) | 2.5 (0.8) | |||
| Pulmonary vascular resistance, dynes/sec/cm−5 | 722 (255) | 735 (365) | 773 (74) | |||
6MWD, 6‐minute walk distance; MCTD, connective tissue disease; NYHA, New York Heart Association; SLE, systemic lupus erythematosus; VO2max, peak oxygen consumption during cardiopulmonary exercise testing.
*By individual investigator judgment.
†All patients on active sitaxsentan treatment (100/300 mg).
Efficacy of sitaxsentan
Six‐minute walk distance and pulmonary haemodynamics
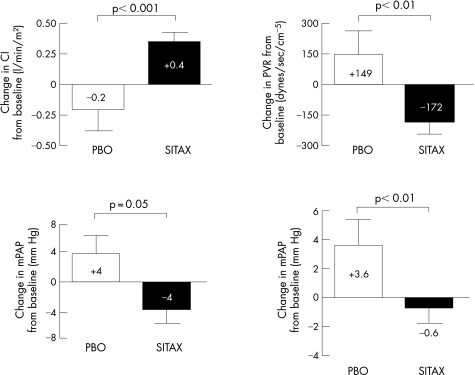
All patients with CTD completed the 12‐week randomised STRIDE‐1 study. The placebo group (n = 9) had a mean (SD) decrease in 6MWD of 38 (84) m from baseline to week 12. In contrast, patients treated with sitaxsentan (n = 33) had an increase from baseline of 20 (52) m (p = 0.037) with a placebo‐subtracted treatment effect of 58 m (p = 0.027). In addition, sitaxsentan therapy was associated with significant improvements compared with placebo in mean right atrial pressure (mRAP), cardiac index (CI) and pulmonary vascular resistance (PVR) (fig 1).
Figure 1 Mean (SE) changes in pulmonary haemodynamics from baseline to week 12 in patients with PAH related to CTD receiving sitaxsentan (SITAX) 100 mg or 300 mg orally once daily (pooled data) compared with placebo (PBO). mRAP, mean right atrial pressure; mPAP, mean pulmonary artery pressure; CI, cardiac index; PVR, pulmonary vascular resistance.
NYHA functional class
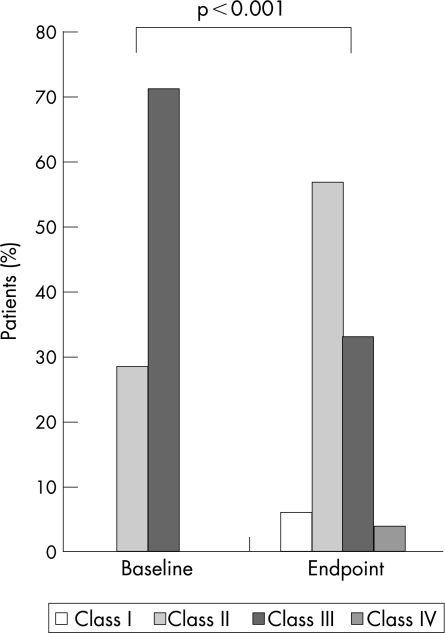
In the 12‐week STRIDE‐1 study, 8 (24%) patients with CTD improved by one NYHA functional class with sitaxsentan compared with one (11%) control given placebo (p = 0.14). One patient treated with placebo, but none of the patients treated with sitaxsentan, had deterioration in functional class. In the extension study, 16 (39%) of 41 patients had an improvement of at least 1 NYHA functional class by the end of the study compared with the start of active sitaxsentan therapy, whereas only 2 patients had a deterioration in NYHA functional class, both of whom died. Before the start of active sitaxsentan therapy, 12 (29%) patients were NYHA functional class I–II and 29 (71%) were class III–IV. By the end of the extension study, 26 (63%) were class I–II and 15 (37%) were class III–IV (p<0.001 vs start of active therapy) (fig 2).
Figure 2 Change in NYHA functional class from start of active therapy to end of study (median follow‐up 26 weeks) in patients with PAH related to CTD receiving sitaxsentan 100 mg or 300 mg orally once daily (last observation carried forward at end of study).
Quality of life
Significant improvements in the domains of physical functioning and role physical of the SF‐36 were observed in the patients treated with sitaxsentan compared with those treated with placebo during the 12‐week randomised STRIDE‐1 trial (table 2). No significant differences were noted in the other domains.
Table 2 Health‐related quality of life as assessed by the Short Form‐36 in patients with PAH and CTD in STRIDE‐1.
| SF‐36 domains | Placebo | Sitaxsentan | p Value* | ||
|---|---|---|---|---|---|
| Baseline (n = 9) | Change after 12 weeks | Baseline (n = 33) | Change after 12 weeks | ||
| Physical functioning | 30.3 (11.3) | −2.2 (9.3) | 29.4 (9.6) | +3.5 (7.5) | 0.042 |
| Role: physical | 34.3 (11.5) | ‐6.8 (12.0) | 31.5 (8.4) | +4.6 (10.3) | 0.01 |
| Role: emotional | 35.1 (12.3) | +4.3 (13.8) | 41.5 (12.1) | +0.4 (10.9) | 0.61 |
| Social functioning | 40.5 (11.9) | −1.2 (13.3) | 41.6 (11.6) | +2.3 (10.8) | 0.3 |
| Bodily pain | 46.2 (10.3) | +3.5 (6.6) | 44.2 (9.4) | +3.2 (8.0) | 0.67 |
| Mental health | 38.4 (11.5) | +4.4 (7.9) | 47.3 (12.7) | +2.2 (9.1) | 0.64 |
| Vitality | 41.7 (9.9) | −2.1 (7.5) | 40.8 (11.3) | +4.9 (10.5) | 0.057 |
| General health perception | 35.6 (8.7) | −1.2 (5.4) | 32.7 (8.7) | +2.8 (7.5) | 0.21 |
*Δ Sitaxsentan versus placebo at 12 weeks.
Data are mean (SD).
Comparison with the idiopathic pulmonary arterial hypertension subset
The efficacy of sitaxsentan in the CTD population was comparable with that observed in the 94 patients with idiopathic PAH (pooled sitaxsentan 100 mg and 300 mg groups, n = 57; placebo, n = 37). No significant differences between the PAH plus CTD cohort treated with sitaxsentan and the IPAH cohort treated with sitaxsentan were observed in any of the efficacy parameters from baseline to week 12. The placebo‐subtracted treatment effect in 6MWD from baseline to week 12 in STRIDE‐1 for the IPAH cohort was +34 m (sitaxsentan group +24 (68) m vs placebo group –10 (65) m; p = 0.02). Treatment effects in haemodynamic parameters for the IPAH cohort were also of similar magnitude to the CTD group, with mean placebo‐subtracted treatment changes in mPAP of −5 mmHg (p = 0.01 vs IPAH placebo group), CI of +0.49 l/min/m2 (p<0.001) and PVR of −311 dyne/sec/cm5 (p<0.001). Functional class improved in 32% of IPAH patients treated with sitaxsentan compared with 16% of the placebo group. Deterioration in NYHA class occurred in 2% of IPAH patients treated with sitaxsentan versus 8% of the placebo group. Quality of life testing in the IPAH subset revealed an improvement in the physical functioning domain (change from baseline to 12 weeks +3.77 (7.6) vs −0.1 (7.7) for the IPAH sitaxsentan and placebo groups, respectively; p<0.01).
Safety
Sitaxsentan appeared to be well tolerated; no patient with PAH and CTD discontinued treatment during the 12‐week STRIDE‐1 trial. Adverse events occurring more frequently in the sitaxsentan group than in the placebo group included peripheral oedema, nasopharyngitis, headache and nasal congestion. There were no increases in hepatic transaminases >3×ULN in the 12‐week STRIDE‐1. Two cases (5%) occurred during the extension phase. One patient in the 100 mg group had hepatic transaminase rises of 3–5×ULN, which normalised after temporarily halting the drug; recommencement of sitaxsentan did not result in reoccurrence of elevated hepatic transaminase levels. The second patient in the 300 mg group had hepatic transaminase rises >5×ULN, which normalised after discontinuation of sitaxsentan; rechallenge was not performed.
Discontinuations
Five subjects discontinued sitaxsentan during the extension phase before the study was stopped. One stopped because of liver function abnormalities (in the 300 mg arm). One patient had worsening PAH after beginning new chronic PAH therapy and another discontinued because of an adverse event reported as worsening dyspnoea, nausea and blurred vision. In both cases, NYHA functional class was class III at baseline and at end of study. Two deaths occurred: one due to acute myocardial infarction and the second associated with infection and acute hypoxaemic respiratory failure. Both subjects had been assigned to the 100 mg sitaxsentan group in STRIDE‐1 and both died 19 weeks from STRIDE‐1 baseline. In neither case was the death considered by the clinical investigator to be related to sitaxsentan.
Discussion
In this post hoc subgroup analysis of patients with PAH associated with CTD who were enrolled in the 12‐week STRIDE‐1 multicentre, double‐blind, randomised placebo‐controlled trial, sitaxsentan therapy improved exercise capacity (as assessed by 6MWD test), haemodynamics and physical health domains of a quality of life instrument compared with patients treated with placebo treated. These treatment effects were of similar magnitude to those occurring in the subset of IPAH patients. Improvements in NYHA functional class were observed during a median follow‐up period of 26 weeks. Given the well‐recognised prognostic impact of functional class, 6MWD and haemodynamics in response to PAH therapy,22,23 selective ETA antagonism with sitaxsentan may represent an important treatment option in the management of PAH associated with CTD.
The gains in physical health‐related quality of life demonstrated in the sitaxsentan‐treated patients with CTD are also worth noting. This group of patients has been shown to have significantly lower physical health‐related quality of life compared with IPAH.24
Sitaxsentan treatment was generally well tolerated, with a 5% incidence of hepatic transaminase elevation and a low discontinuation rate. However, conclusions regarding safety cannot be made on the basis of this small retrospective subset analysis. A subsequent 18‐week trial has confirmed a low incidence of transaminase elevation with the 100 mg/day dose25 and preliminary data from a 1‐year extension of this study support the long‐term safety of this dosage in patients with PAH and CTD.26
Despite the beneficial effects noted in short‐term (12–16 weeks) randomised, double‐blind, placebo‐controlled clinical trials, long‐term outcomes with any therapy for PAH associated with CTD have been disappointing, with less efficacy and reduced survival compared with IPAH patients.10,11,27,28 Although the medium‐term improvement in functional class reported here with sitaxsentan is encouraging, more patients with longer follow‐up are needed to adequately gauge the long‐term efficacy of sitaxsentan in PAH‐CTD.
These data are comparable with a similar analysis of the ETA/ETB receptor antagonist, bosentan, in PAH associated with CTD.6 After 12–16 weeks, there was a trend towards an improvement in 6MWD in 44 patients treated with bosentan (+19.5 m, 95% confidence interval (CI) −3.2 to 42.2]) whereas 22 subjects receiving placebo had no change (−2.6 m, 95% CI −54.0 to 48.7). The placebo‐subtracted treatment effect of 22.1 m was not significant. Of 40 patients who remained on bosentan monotherapy in an open‐label long‐term extension phase, 10 experienced an improvement in NYHA functional class, and 6MWD increased by +14.7 m (95% CI –11 to 40). Nevertheless, survival in the entire cohort of 64 patients receiving bosentan for a mean (SD) duration of 1.8 (0.8) years (86% at 1 year; 74% at 2 years) was notably better than historical controls. This was consistent with the experience from the Royal Free Hospital Registry, which found that patients treated with bosentan had a 1‐year and 2‐year survival rate of 81% and 71%, respectively.29
The present findings with sitaxsentan and those available for bosentan suggest that ET receptor antagonism, either selective ETA or non‐selective ETA/ETB, appears to have durable effects on overall patient status and survival. These data are in stark contrast with several studies of continuous intravenous epoprostenol, in which a survival benefit has been lacking.11,12,28 The sustained disease‐modifying effects of ET receptor antagonism may be underestimated by short‐term effects on exercise capacity.
Limitations
There were several limitations to this study. This was a post hoc analysis of the subset of PAH patients with CTD from the STRIDE‐1/1X trials. The primary outcome measure of this trial, maximum oxygen consumption, was not met. This parameter has not been validated in therapeutic trials and may be less responsive than the 6MWD. The latter has been the primary endpoint for all other clinical trials in PAH.20 Our sample size was limited and data from the two dosage groups of sitaxsentan were pooled. Additional studies are needed to further explore the efficacy of sitaxsentan in this challenging subset of PAH patients. The type of CTD was not homogenous; it included both the scleroderma spectrum of disease5 and SLE. The natural history of PAH associated with SLE is not well characterised, but a large proportion of these cases often has concomitant features of systemic sclerosis.30 The 6MWD data were not collected during the extension phase, thus it is not known if the medium‐term benefit in NYHA class is accompanied by sustained improvements in exercise capacity. Furthermore, changes in functional class during the extension phase must be interpreted with caution, as all subjects were on the active drug.
Conclusion
In summary, treatment with the oral ETA‐selective antagonist, sitaxsentan, given once daily, improved exercise capacity (assessed by the 6MWD test), functional class, physical health‐related quality of life and haemodynamics in patients with PAH associated with CTD, and had a low incidence of acute hepatotoxicity. Sitaxsentan may prove useful in the long‐term management of these patients. Further studies are warranted.
Abbreviations
6MWD - 6‐minute walk distance
CI - Cardiac Index
CTD - connective tissue disease
ET - endothelin
ETA - endothelin receptor isoform type A
ETB - endothelin receptor isoform type B
IPAH - idiopathic pulmonary arterial hypertension
MCTD - mixed connective tissue disease
mPAP - mean pulmonary artery pressure
mRAP - mean right atrial pressure
NO - nitric oxide
NYHA - New York Heart Association
PAH - pulmonary arterial hypertension
PCWPm - mean pulmonary capillary wedge pressure
PVR - pulmonary vascular resistance
SF‐36 - Short Form 36
SLE - systemic lupus erythematosus
SSc - systemic sclerosis
STRIDE‐1 - Sitaxsentan to Relieve Impaired Exercise trial
STRIDE‐1X - Sitaxsentan to Relieve Impaired Exercise extension trial
ULN - upper limit of the normal range
Footnotes
Financial disclosure: Supported by Encysive Pharmaceuticals (Houston, Texas, USA).
References
- 1.Wigley F M, Lima J A, Mayes M, McLain D, Chapin J L, Ward‐Able C. The prevalence of undiagnosed pulmonary arterial hypertension in subjects with connective tissue disease at the secondary health care level of community‐based rheumatologists (the UNCOVER study). Arthritis Rheum 2005522125–2132. [DOI] [PubMed] [Google Scholar]
- 2.Johnson S R, Gladman D D, Urowitz M B, Ibanez D, Granton J T. Pulmonary hypertension in systemic lupus. Lupus 200413506–509. [DOI] [PubMed] [Google Scholar]
- 3.Koh E T, Lee P, Gladman D D, Abu‐Shakra M. Pulmonary hypertension in systemic sclerosis: an analysis of 17 patients. Br J Rheumatol 199635989–993. [DOI] [PubMed] [Google Scholar]
- 4.Stupi A M, Steen V D, Owens G R, Barnes E L, Rodnan G P, Medsger T A., Jr Pulmonary hypertension in the CREST syndrome variant of systemic sclerosis. Arthritis Rheum 198629515–524. [DOI] [PubMed] [Google Scholar]
- 5.Badesch D B, Tapson V F, McGoon M D, Brundage B H, Rubin L J, Wigley F M.et al Continuous intravenous epoprostenol for pulmonary hypertension due to the scleroderma spectrum of disease. A randomized, controlled trial. Ann Intern Med 2000132425–434. [DOI] [PubMed] [Google Scholar]
- 6.Denton C P, Humbert M, Rubin L, Black C M. Bosentan treatment for pulmonary arterial hypertension related to connective tissue disease: a subgroup analysis of the pivotal clinical trials and their open‐label extensions. Ann Rheum Dis 2006651336–1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Galie N, Ghofrani H A, Torbicki A, Barst R J, Rubin L J, Badesch D.et al Sildenafil citrate therapy for pulmonary arterial hypertension. N Engl J Med 20053532148–2157. [DOI] [PubMed] [Google Scholar]
- 8.Oudiz R J, Schilz R J, Barst R J, Galie N, Rich S, Rubin L J.et al Treprostinil, a prostacyclin analogue, in pulmonary arterial hypertension associated with connective tissue disease. Chest 2004126420–427. [DOI] [PubMed] [Google Scholar]
- 9.Rubin L J, Badesch D B, Barst R J, Galie N, Black C M, Keogh A.et al Bosentan therapy for pulmonary arterial hypertension. N Engl J Med 2002346896–903. [DOI] [PubMed] [Google Scholar]
- 10.Girgis R E, Mathai S C, Krishnan J A, Wigley F M, Hassoun P M. Long‐term outcome of bosentan treatment in idiopathic pulmonary arterial hypertension and pulmonary arterial hypertension associated with the scleroderma spectrum of diseases. J Heart Lung Transplant 2005241626–1631. [DOI] [PubMed] [Google Scholar]
- 11.Kawut S M, Taichman D B, Archer‐Chicko C L, Palevsky H I, Kimmel S E. Hemodynamics and survival in patients with pulmonary arterial hypertension related to systemic sclerosis. Chest 2003123344–350. [DOI] [PubMed] [Google Scholar]
- 12.Fagan K A, Badesch D B. Pulmonary hypertension associated with connective tissue disease. Prog Cardiovasc Dis 200245225–234. [DOI] [PubMed] [Google Scholar]
- 13.Mukerjee D, St George D, Coleiro B, Knight C, Denton C P, Davar J.et al Prevalence and outcome in systemic sclerosis associated pulmonary arterial hypertension: application of a registry approach. Ann Rheum Dis 2003621088–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hachulla E, Coghlan J G. A new era in the management of pulmonary arterial hypertension related to scleroderma: endothelin receptor antagonism. Ann Rheum Dis 2004631009–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Channick R N, Sitbon O, Barst R J, Manes A, Rubin L J. Endothelin receptor antagonists in pulmonary arterial hypertension. J Am Coll Cardiol 200443(Suppl S)62S–7S. [DOI] [PubMed] [Google Scholar]
- 16.Benigni A, Remuzzi G. Endothelin antagonists. Lancet 1999353133–138. [DOI] [PubMed] [Google Scholar]
- 17.McLaughlin V V, Sitbon O, Badesch D B, Barst R J, Black C, Galie N.et al Survival with first‐line bosentan in patients with primary pulmonary hypertension. Eur Respir J 200525244–249. [DOI] [PubMed] [Google Scholar]
- 18.Provencher S, Sitbon O, Humbert M, Cabrol S, Jais X, Simonneau G. Long‐term outcome with first‐line bosentan therapy in idiopathic pulmonary arterial hypertension. Eur Heart J 200627589–595. [DOI] [PubMed] [Google Scholar]
- 19.Galie N, Manes A, Branzi A. The endothelin system in pulmonary arterial hypertension. Cardiovasc Res 200461227–237. [DOI] [PubMed] [Google Scholar]
- 20.Barst R J, Langleben D, Frost A, Horn E M, Oudiz R, Shapiro S.et al Sitaxsentan therapy for pulmonary arterial hypertension. Am J Respir Crit Care Med 2004169441–447. [DOI] [PubMed] [Google Scholar]
- 21.Ware J E, Jr, Sherbourne C D. The MOS 36‐item short‐form health survey (SF‐36). I. Conceptual framework and item selection. Med Care 199230473–483. [PubMed] [Google Scholar]
- 22.McLaughlin V V, Shillington A, Rich S. Survival in primary pulmonary hypertension: the impact of epoprostenol therapy. Circulation 20021061477–1482. [DOI] [PubMed] [Google Scholar]
- 23.Sitbon O, Humbert M, Nunes H, Parent F, Garcia G, Herve P.et al Long‐term intravenous epoprostenol infusion in primary pulmonary hypertension: prognostic factors and survival. J Am Coll Cardiol 200240780–788. [DOI] [PubMed] [Google Scholar]
- 24.Taichman D B, Shin J, Hud L, Archer‐Chicko C, Kaplan S, Sager J S.et al Health‐related quality of life in patients with pulmonary arterial hypertension. Respir Res 2005692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barst R J, Langleben D, Badesch D, Frost A, Lawrence E C, Shapiro S.et al Treatment of pulmonary arterial hypertension with the selective endothelin‐A receptor antagonist sitaxsentan. J Am Coll Cardiol 2006472049–2056. [DOI] [PubMed] [Google Scholar]
- 26.Benza R, Frost A, Girgis R, Langleben D, Lawrence E C, Naeije R. Chronic treatment of pulmonary arterial hypertension with sitaxsentan and bosentan. Am J Respir Crit Care Med 20063A729 [Google Scholar]
- 27.Fisher M R, Mathai S C, Champion H C, Girgis R E, Housten‐Harris T, Hummers L.et al Clinical differences between idiopathic and scleroderma‐related pulmonary hypertension. Arthritis Rheum 2006543043–3050. [DOI] [PubMed] [Google Scholar]
- 28.Kuhn K P, Byrne D W, Arbogast P G, Doyle T P, Loyd J E, Robbins I M. Outcome in 91 consecutive patients with pulmonary arterial hypertension receiving epoprostenol. Am J Respir Crit Care Med 2003167580–586. [DOI] [PubMed] [Google Scholar]
- 29.Williams M H, Das C, Handler C E, Akram M R, Davar J, Denton C P.et al Systemic sclerosis associated pulmonary hypertension: improved survival in the current era. Heart 200692926–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tanaka E, Harigai M, Tanaka M, Kawaguchi Y, Hara M, Kamatani N. Pulmonary hypertension in systemic lupus erythematosus: evaluation of clinical characteristics and response to immunosuppressive treatment. J Rheumatol 200229282–287. [PubMed] [Google Scholar]