An exacerbation of chronic obstructive pulmonary disease (COPD) has a serious impact on disease progression and is associated with high medical costs, but the cause of about one‐third of exacerbations cannot be identified.1 Adequate protective reflexes in the airways play an important role in the prevention of aspiration of bacteria‐containing oropharyngeal or gastric secretions. Impairment of these reflexes, such as the swallowing reflex, therefore represents a potential risk factor for exacerbations of COPD. We have conducted a cross‐sectional survey to evaluate the prevalence of impairment of the swallowing reflex in patients with COPD and to determine whether this is a risk factor for COPD exacerbations.
Fifty clinically stable patients with COPD were enrolled from the outpatient clinic of Ishinomaki Red Cross Hospital, Ishinomaki, Japan. Patients who were current smokers and those with oral corticosteroid use, oral and pharyngeal cancer, previous head and neck surgery, neuromuscular disease and oesophageal disease were excluded. Twenty‐five patients (22 men and 3 women) had at least one exacerbation during the previous year, while the other 25 patients (21 men and 4 women) were stable. In the exacerbation group the patients had 2.4 (range 1–10) exacerbations per year, and 20 patients (80%) required hospital admission. There was no significant difference between the stable group and the exacerbation group in age (mean (SE) 75.0 (1.3) years vs 77.2 (1.0) years), forced expiratory volume in 1 s (FEV1) (mean (SE) 1.11 (0.11) l vs 1.07 (0.09) l), percentage predicted value of FEV1 (mean (SE) 47.1 (3.7)% vs 50.1 (3.7)%) and the rate of home oxygen therapy (4% vs 20%). All patients were eating an entirely oral diet without complaining of dysphagia prior to enrolment.
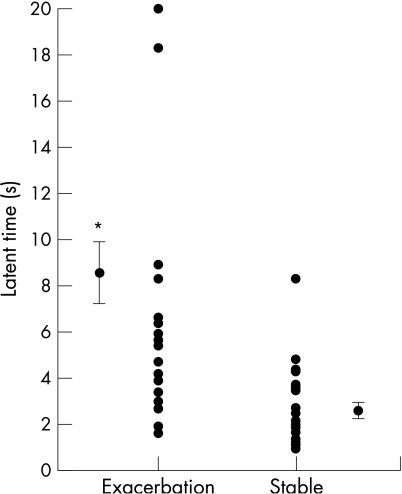
We evaluated the swallowing reflex on the basis of the latency of response to the onset of the swallowing action timed from the injection of 1 ml distilled water into the pharynx through a nasal catheter.2 The mean (SE) latent time of the swallowing reflex was significantly longer in the exacerbation group than in the stable group (8.6 (1.3) s vs 2.6 (0.3) s, p<0.001; fig 1). We classified a response as normal or impaired according to whether the swallowing reflex was induced within 3 s of the injection. In the exacerbation group 22 of 25 patients (88%) exhibited an impaired response compared with 8 of 25 patients (32%) in the stable group (p<0.001). Impairment of the swallowing reflex was significantly associated with an exacerbation of COPD (relative risk 2.8, 95% confidence interval 1.5 to 5.0).
Figure 1 Comparison of latent time of the swallowing reflex in patients with exacerbations of chronic obstructive pulmonary disease and those with stable disease.
These results indicate that there is a high incidence of impairment of the swallowing reflex in patients with COPD and this is a risk factor for an exacerbation of COPD. To date, there are few published reports available on swallowing dysfunction in patients with COPD.3,4,5 The impact of impairment of the swallowing reflex in COPD exacerbations has not been clarified. The findings of our study highlight a novel risk factor for exacerbations of COPD and raise the possibility that precautions against aspiration could be useful to prevent these exacerbations.
Acknowledgements
The authors thank Dr Naoya Fujino for data collection.
Footnotes
Funding: None
Competing interests: None.
References
- 1.Donaldson G C, Wedzicha J A. COPD exacerbations. 1: Epidemiology. Thorax 200661164–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ebihara T, Sekizawa K, Nakazawa H.et al Capsaicin and swallowing reflex. Lancet 1993341432. [DOI] [PubMed] [Google Scholar]
- 3.Stein M, Williams A J, Grossman F.et al Cricopharyngeal dysfunction in chronic obstructive pulmonary disease. Chest 199097347–352. [DOI] [PubMed] [Google Scholar]
- 4.Good‐Fratturelli M D, Curlee R F, Holle J L. Prevalence and nature of dysphagia in VA patients with COPD referred for videofluoroscopic swallow examination. J Commun Disord 20003393–110. [DOI] [PubMed] [Google Scholar]
- 5.Mokhlesi B, Logemann J A, Rademaker A W.et al Oropharyngeal deglutition in stable COPD. Chest 2002121361–369. [DOI] [PubMed] [Google Scholar]