Abstract
Background
Inhaled asbestos fibres can cause inflammation and fibrosis in the lungs called asbestosis. However, there are no non‐invasive means to assess and follow the severity of the inflammation. Exhaled nitric oxide (NO) measured at multiple exhalation flow rates can be used to assess the alveolar NO concentration and bronchial NO flux, which reflect inflammation in the lung parenchyma and airways, respectively. The aim of the present study was to investigate whether exhaled NO or markers in exhaled breath condensate could be used to assess inflammation in asbestosis.
Methods
Exhaled NO and inflammatory markers (leukotriene B4 and 8‐isoprostane) in exhaled breath condensate were measured in 15 non‐smoking patients with asbestosis and in 15 healthy controls. Exhaled NO concentrations were measured at four constant exhalation flow rates (50, 100, 200 and 300 ml/s) and alveolar NO concentration and bronchial NO flux were calculated according to the linear model of pulmonary NO dynamics.
Results
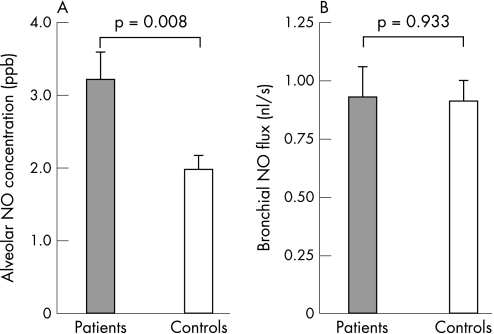
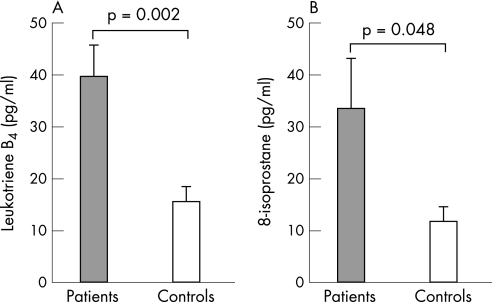
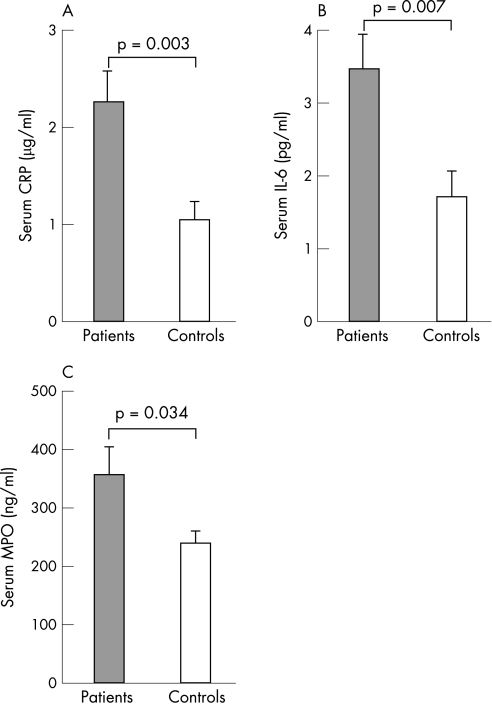
The mean (SE) alveolar NO concentration was significantly higher in patients with asbestosis than in controls (3.2 (0.4) vs 2.0 (0.2) ppb, p = 0.008). There was no difference in bronchial NO flux (0.9 (0.1) vs 0.9 (0.1) nl/s, p = 0.93) or NO concentration measured at ATS standard flow rate of 50 ml/s (20.0 (2.0) vs 19.7 (1.8) ppb, p = 0.89). Patients with asbestosis had increased levels of leukotriene B4 (39.5 (6.0) vs 15.4 (2.9) pg/ml, p = 0.002) and 8‐isoprostane (33.5 (9.6) vs 11.9 (2.8) pg/ml, p = 0.048) in exhaled breath condensate and raised serum levels of C‐reactive protein (2.3 (0.3) vs 1.1 (0.2) μg/ml, p = 0.003), interleukin‐6 (3.5 (0.5) vs 1.7 (0.4) pg/ml, p = 0.007) and myeloperoxidase (356 (48) vs 240 (20) ng/ml, p = 0.034) compared with healthy controls.
Conclusions
Patients with asbestosis have an increased alveolar NO concentration and high levels of leukotriene B4 and 8‐isoprostane in exhaled breath. Measurement of exhaled NO at multiple exhalation flow rates and analysis of inflammatory markers in exhaled breath condensate are promising non‐invasive means for assessing inflammation in patients with asbestosis.
Asbestosis is diffuse interstitial lung fibrosis caused by an inflammatory response to inhaled asbestos fibres.1,2,3,4 It requires moderate or heavy exposure to asbestos and takes at least 15–20 years to develop in most cases. The diagnosis of asbestosis is based on findings of diffuse interstitial fibrosis when a history of sufficient exposure to asbestos exists and other causes of pulmonary fibrosis have been ruled out. The general features of the inflammatory reaction in asbestosis have recently been reviewed.1 However, there are no non‐invasive tools to assess the inflammatory reaction in asbestosis, and efforts to treat the disease have not been successful.1,2,3,4,5
There is a clinical need to develop a direct means of measuring inflammation for follow‐up and diagnostic purposes in inflammatory lung diseases. Exhaled nitric oxide (NO) measurements and inflammatory markers in exhaled breath condensate have recently been introduced as non‐invasive methods for assessing lung inflammation.6,7 NO is a gaseous signalling molecule that regulates various physiological and pathophysiological functions in the lungs and in the whole human body.8,9 It is synthesised in small amounts by constitutive nitric oxide synthases (cNOS) in physiological conditions. In inflammation, the inducible nitric oxide synthase (iNOS) produces higher amounts of NO for prolonged periods.10,11 The NO concentration in exhaled air is known to be increased in diseases such as asthma,12,13,14 chronic obstructive pulmonary disease (COPD)15 and alveolitis.14,16 According to the ERS and ATS recommendations, exhaled NO should be measured at a single exhalation flow rate of 50 ml/s.7 However, measurement of exhaled NO at multiple exhalation flow rates allows assessment of alveolar and bronchial NO output separately.17,18,19,20 The multiple flow rate method is based on a mathematical model which divides the lung into two compartments—the alveolar/peripheral and bronchial/central compartments.17 The multiple exhalation flow rate method has been shown to differentiate successfully between bronchial and alveolar inflammation in asthma, COPD and alveolitis.14,18,19,21,22,23,24,25
Non‐gaseous markers of pulmonary inflammation can be non‐invasively sampled by collecting exhaled breath condensate, and raised levels of inflammatory mediators such as leukotriene B4 (LTB4) and 8‐isoprostane have been found in certain inflammatory lung diseases.26
In the present study we measured exhaled NO at multiple exhalation flow rates and collected exhaled breath condensate in 15 patients with asbestosis and 15 age‐ and sex‐matched healthy controls. The aim of the study was to determine whether patients with asbestosis have altered bronchial or alveolar NO output or increased concentrations of inflammatory markers LTB4 and/or 8‐isoprostane in their exhaled breath condensate.
Methods
Subjects
Exhaled NO levels, markers in exhaled breath condensate, spirometric parameters and pulmonary transfer factor were measured in 15 patients with asbestosis (all men) of mean age 67 years (range 56–74), average exposure to asbestos 20.5 years (range 10–39), in whom exposure had stopped 25.6 years (range 14–39) previously. The patients were recruited from patient records of Tampere University Hospital, and they had been diagnosed (before the year 2002) to have asbestosis by the Tampere University Hospital Pneumoconioses Expert Group (including expertise from pulmonary, radiological and occupational medicine). The diagnosis of asbestosis was based on moderate (10–25 fibre‐years) or heavy (>25 fibre‐years) exposure to asbestos, sufficient latency time, diffuse interstitial lung fibrosis on high resolution computed tomography (HRCT) and exclusion of other causes of diffuse fibrosis according to the Helsinki diagnostic criteria for asbestosis.27 The HRCT images were reviewed by an experienced thoracic radiologist (RJ) and an experienced occupational health physician (PO). The reviewers were blinded to the medical information of the patients, and the images were scored by consensus reading. Lung fibrosis, parietal pleural plaques and diffuse pleural thickening were scored separately as described elsewhere.28,29 The characteristics of the patients are given in tables 1 and 2.
Table 1 Characteristics of patients: lung function.
| Patient number | FVC (% predicted) | FEV1 (% predicted) | FEV1/FVC (%) | FEF50% (% predicted) | Tlco (% predicted) | Tlco/Va (% predicted) |
|---|---|---|---|---|---|---|
| 1 | 100 | 96 | 77 | 72 | 111 | 108 |
| 2 | 75 | 68 | 73 | 46 | 102 | 116 |
| 3 | 69 | 63 | 75 | 52 | 94 | 122 |
| 4 | 107 | 104 | 77 | 88 | 117 | 111 |
| 5 | 75 | 66 | 70 | 38 | 86 | 109 |
| 6 | 96 | 86 | 75 | 56 | 80 | 93 |
| 7 | 86 | 94 | 89 | 176 | 92 | 113 |
| 8 | 89 | 83 | 75 | 56 | 85 | 101 |
| 9 | 72 | 67 | 75 | 42 | 77 | 102 |
| 10 | 62 | 65 | 87 | 61 | 63 | 116 |
| 11 | 96 | 95 | 81 | 78 | 71 | 82 |
| 12 | 80 | 75 | 77 | 51 | 85 | 112 |
| 13 | 87 | 91 | 83 | 115 | 98 | 114 |
| 14 | 72 | 72 | 80 | 70 | 51 | 80 |
| 15 | 91 | 83 | 76 | 66 | 72 | 77 |
FVC, forced vital capacity; FEV1, forced expiratory volume in 1 s; FEV50%, forced expiratory flow at 50% of expired volume; Tlco, carbon monoxide transfer factor adjusted for haemoglobin; Tlco/Va, specific carbon monoxide transfer factor adjusted for haemoglobin.
Table 2 Characteristics of patients: high resolution computed tomography (HRCT) findings.
| Patient number | Lung fibrosis (grade 0–5) | Parietal pleural plaques (grade 0–5) | Diffuse pleural thickening (grade 0–3) | Lung emphysema |
|---|---|---|---|---|
| 1 | 3 | 4 | 0 | No |
| 2 | 2 | 4 | 0 | No |
| 3 | 2 | 4 | 0 | Bullae |
| 4 | 1 | 3 | 0 | No |
| 5 | 3 | 4 | 0 | No |
| 6 | 3 | 5 | 0 | No |
| 7 | 4 | 3 | 2 | Paraseptal emphysema |
| 8 | 3 | 2 | 0 | No |
| 9 | 3 | 4 | 0 | No |
| 10 | 3 | 3 | 0 | No |
| 11 | 4 | 2 | 0 | No |
| 12 | 3 | 4 | 0 | No |
| 13 | 2 | 5 | 0 | No |
| 14 | 3 | 1 | 2 | Centrilobular and paraseptal emphysema |
| 15 | 2 | 2 | 0 | Centrilobular emphysema, bullae |
The exclusion criteria for the study were current smoking, diagnosed asthma, chronic bronchitis, COPD and other diagnosed pulmonary disease or acute respiratory symptoms. Chronic bronchitis was excluded with a symptoms questionnaire (cough and raising sputum on most days for 3 months during 2 consecutive years).
Fifteen age‐matched healthy male volunteers of mean age 63 years (range 53–73) with normal spirometric values were recruited into the control group. All subjects were non‐smokers (who had quit smoking at least 5 years previously). Subjects had no respiratory symptoms according to the symptoms questionnaire.
The study was approved by the ethics committee of Tampere University Hospital and all subjects gave their written informed consent.
Exhaled NO
Exhaled NO was measured with a Sievers NOA 280 analyser (Sievers Instruments, Boulder, Colorado, USA) at four exhalation flow rates (50, 100, 200 and 300 ml/s). The alveolar NO concentration and bronchial NO flux were calculated according to Tsoukias and George17 as previously described14 by using exhalation flow rates of 100, 200 and 300 ml/s. Exhaled NO output ( = exhaled NO concentration × exhalation flow rate) was plotted against exhalation flow rate and a linear regression was set. Slope and intercept of the regression line are approximates of alveolar NO concentration and bronchial NO flux, respectively.
The desired exhalation flow rates were achieved by letting the patients exhale through a mass flow meter connected to a computer‐controlled adjustable flow restrictor (NOFLA device developed at the University of Tampere). The computer adjusted the flow resistor in real time based on the actual flow rate measured. If the flow rate tended to be higher or lower than the desired flow rate, the flow restriction was increased or decreased in real time to achieve the desired flow rate, regardless of changes in the patient's exhalation effort. A pressure gauge was connected to the system and the subjects were asked to maintain exhalation pressure between 5 and 20 cm H2O during the exhalation.
Exhaled breath condensate
Exhaled breath condensate was collected during 15 min of tidal breathing with Ecoscreen condenser (Ecoscreen, Jaeger, Hoechberg, Germany) while wearing nose clips. The samples were stored at –70°C until assayed. LTB4 and 8‐isoprostane concentrations in the condensates were measured by immuno‐assay with a detection limit of 1.95 pg/ml (Cayman Chemical Company, Ann Arbor, Michigan, USA).
Serum samples
Venous blood was collected into Vacutainer Hemogaard SST tubes (Becton Dickinson, Franklin Lakes, New Jersey, USA) and allowed to clot for 60 min at 22°C. The serum was thereafter separated by centrifugation (1300 g for 10 min). The samples were stored at –70°C until analysed. Serum levels of myeloperoxidase (MPO) were measured by radioimmunoassay (Pharmacia Diagnostics AB, Uppsala, Sweden); the concentration of interleukin‐6 (IL‐6) was determined by enzyme immunoassay (PeliPair ELISA, Sanquin, Amsterdam, the Netherlands); and C‐reactive protein (CRP) was analysed using a particle‐enhanced turbidimetric assay (Cobas Integra 800 Analyser, Roche Diagnostics, Basel, Switzerland).
Analysis of data
The results are presented as mean (SE). All the parameters were normally distributed according to the Kolmogorov‐Smirnov test. Differences between the two groups were analysed by t test. SPSS Version 10.1 (SPSS Inc, Chicago, Illinois, USA) software was used for statistical analysis, with p<0.05 being considered statistically significant.
Results
Alveolar NO concentration and bronchial NO flux
Patients with asbestosis had higher alveolar NO concentrations than healthy controls (3.2 (0.4) vs 2.0 (0.2) ppb, p = 0.008) but bronchial NO flux was similar in both groups (0.9 (0.1) vs 0.9 (0.1) nl/s, p = 0.93; fig 1). Interestingly, there were no differences between patients with asbestosis and healthy controls in exhaled NO concentrations measured at exhalation flow rates of 50 ml/s (the ATS standard flow rate), 100 ml/s or 200 ml/s (table 3), but at the highest exhalation flow rate (300 ml/s) the NO concentration tended to be higher in patients with asbestosis (p = 0.06).
Figure 1 (A) Alveolar NO concentration and (B) bronchial NO flux in patients with asbestosis (n = 15) and in healthy controls (n = 15). Values are given as mean (SE).
Table 3 Mean (SE) exhaled NO concentrations (ppb) at different exhalation flow rates in patients with asbestosis and in healthy controls.
| Exhalation flow rate (ml/s) | Patients (n = 15) | Controls (n = 15) | p Value |
|---|---|---|---|
| 50 | 20.0 (2.0) | 19.7 (1.8) | 0.89 |
| 100 | 12.5 (1.3) | 11.1 (0.9) | 0.38 |
| 200 | 7.9 (0.7) | 6.6 (0.5) | 0.18 |
| 300 | 6.3 (0.5) | 5.0 (0.4) | 0.06 |
Factors increasing alveolar NO concentration
Steady state alveolar NO concentration can be described using the equation Ca = Vno,a/Tlno, where Vno,a (nl/s) is the diffusing rate of NO from tissue to the alveolar space and Tlno (nl/s/ppb) is the transfer factor for NO from the alveolar space to the pulmonary vessels.30 Ca can thus be increased either because of increased NO production in the lung parenchyma causing increased NO diffusion to alveolar air (Vno,a) or because of decreased diffusion of NO from alveolar air to the pulmonary blood vessels caused by decreased alveolar NO transfer factor (Tlno).
We made an effort to estimate whether the increased alveolar NO concentration in the patients with asbestosis is due to increased diffusion of NO to alveolar air (Vno,a) or to decreased transfer factor of NO from alveolar air to the pulmonary blood (Tlno). As Tlno is approximately 4× carbon monoxide transfer factor (Tlco),31 the aforementioned equation can be rearranged to Vno,a = Ca ×4×Tlco, and Vno,a can be calculated based on measurements of alveolar NO concentration and Tlco. We made an assumption that the Tlco in our healthy controls would equal the age‐ and sex‐matched reference value for Tlco,32 and calculated Vno,a in both groups. Vno,a was higher in patients with asbestosis than in healthy control subjects (4.1 (0.6) vs 3.1 (0.3) nl/s), although the difference did not reach statistical significance (p = 0.13).
LTB4 and 8‐isoprostane concentrations in exhaled breath condensate
Patients with asbestosis had increased concentrations of LTB4 (39.5 (6.0) vs 15.4 (2.9) pg/ml, p = 0.002) and 8‐isoprostane (33.5 (9.6) vs 11.9 (2.8) pg/ml, p = 0.048) in exhaled breath condensate than healthy controls (fig 2).
Figure 2 (A) leukotriene B4 and (B) 8‐isoprostane concentrations in exhaled breath condensate in patients with asbestosis (n = 15) and healthy controls (n = 15). Values are given as mean (SE).
Inflammatory markers in serum
Patients with asbestosis had raised serum levels of CRP (2.3 (0.3) vs 1.1 (0.2) μg/ml, p = 0.003), IL‐6 (3.5 (0.5) vs 1.7 (0.4) pg/ml, p = 0.007) and MPO (356 (48) vs 240 (20) ng/ml, p = 0.034) compared with healthy controls (fig 3).
Figure 3 Serum concentrations of (A) C‐reactive protein (CRP), (B) interleukin‐6 (IL‐6) and (C) myeloperoxidase (MPO) in patients with asbestosis (n = 15) and in healthy controls (n = 15). Values are given as mean (SE).
Discussion
In this study we have measured lung inflammation in patients with asbestosis using two recently described non‐invasive methods—exhaled NO measurement with multiple exhalation flow rates and exhaled breath condensate. The alveolar concentration of NO was higher in patients with asbestosis than in healthy controls, while there were no differences in bronchial NO flux. The concentrations of LTB4 and 8‐isoprostane in exhaled breath condensate were also higher in patients with asbestosis than in healthy controls.
Increased exhaled NO serves as a marker of lung inflammation in diseases such as asthma and alveolitis.12,13,14,16 The multiple exhalation flow rate method is an extension of the standard single flow method for measuring exhaled NO. It can be used to assess the bronchial or proximal (large airway) and peripheral (small airway and alveolar) contribution to NO output separately and, accordingly, the bronchial and peripheral components of lung inflammation.18 In our previous studies we have shown that this method can be used to differentiate between bronchial and alveolar inflammation in patients with asthma and alveolitis, and in those patients the values returned towards normal levels during anti‐inflammatory treatment.14,21,33 In other studies, raised alveolar concentrations of NO have been found in COPD (2.1–2.4‐fold increase),24,25 liver cirrhosis (1.8‐fold increase)23 and in patients with lung fibrosis associated with scleroderma (2.6‐fold increase).34 Increased bronchial NO flux has been found in patients with asthma or asthma‐like symptoms.14,19,21,22,24,33,35,36,37
The inflammatory process in the lungs induced by inhaled asbestos is characterised by alveolitis, inflammation in the surrounding interstitium, and inflammation and fibrosis in the respiratory bronchioles that extend into adjacent alveolar tissue. Bronchoalveolar lavage (BAL) in patients with asbestosis has demonstrated an alveolitis associated with increases in macrophages and neutrophils.4,38 Studies using BAL, CT scanning, and gallium‐67 scanning have shown that inflammatory events occur early before the onset of symptoms and diagnosis of asbestosis.4,38 With the knowledge that asbestosis is an inflammatory disease of the lung parenchyma,1 we hypothesised that alveolar NO might be increased in those patients. The present results showed an increased alveolar NO concentration and normal bronchial NO flux in patients with asbestosis. However, the alveolar NO concentrations in asbestosis (1.6‐fold increase) were lower than those in alveolitis (3.7‐fold increase) in our previous studies.14,21 Interestingly, when NO concentrations in exhaled air were measured at a single exhalation flow rate according to the ATS standards (50 ml/s),7 there was no difference between patients with asbestosis and healthy controls. Only at the highest exhalation flow rate used (300 ml/s) did NO concentrations in exhaled breath tend to be higher in patients with asbestosis than in healthy controls (p = 0.06). These results, and our previous results in patients with alveolitis, show that the multiple flow rate method is more sensitive for detecting the alveolar/peripheral component of lung inflammation than the conventional single exhalation flow rate method which, in many cases, ignores the peripheral component of inflammation, especially when a low exhalation flow rate (50 ml/s) is used.
The alveolar NO concentration is determined by NO production in the lung tissue and by alveolar transfer factor of NO. The increased alveolar NO concentration found in patients with asbestosis could therefore be caused by decreased pulmonary transfer factor and/or increased NO production in alveolar tissue. The decreased pulmonary gas diffusing capacity is typical for asbestosis,5 and it probably increases the alveolar NO concentration in these patients, but the level of iNOS expression in lung tissue has not been investigated in patients with asbestosis. However, enhanced iNOS expression has been shown in the alveolar epithelium of patients with other fibrosing lung diseases,39 and exposure to asbestos induces iNOS expression in human pneumocytes in vitro40 and in mice and rat lung in vivo.41,42 It is therefore likely that alveolar NO production is increased in patients with asbestosis and contributes to the increased alveolar NO concentration. Our estimate of alveolar NO production rate in asbestosis was higher than in healthy subjects, but the difference did not reach statistical significance in the present relatively small group of patients. However, we were not able to measure Tlno in patients but it was estimated based on Tlco,31 and Tlno in healthy subjects was estimated based on normal values in the population. Further studies are needed to confirm the contributions of increased pulmonary NO production rate and reduced Tlno to the enhanced alveolar NO concentration found in patients with asbestosis.
During the processing of the present paper, Sandrini et al43 reported increased exhaled NO concentration in patients with asbestos‐related respiratory diseases by a single exhalation flow rate method using a high exhalation flow rate (200 ml/s). This is in line with our study showing increased alveolar NO concentration in patients with asbestosis as increased alveolar NO concentration would increase exhaled NO concentrations at higher rather than at lower exhalation flow rates. However, the peripheral origin of increased exhaled NO concentrations in patients with asbestosis cannot be reliably verified in the study by Sandrini et al43 as they used only a single exhalation flow rate in NO measurements.
To our knowledge, there are no previous studies on inflammatory markers in exhaled breath condensate from patients with asbestosis. We have shown that concentrations of LTB4 and 8‐isoprostane are increased in breath condensate from patients with asbestosis. This is in agreement with earlier studies showing that LTB4 levels are raised in the BAL fluid from asbestos workers.44 LTB4 is produced by activated neutrophils and is a potent inducer of granulocyte activation. Increased levels of LTB4 in breath condensate have earlier been found in, for example, patients with COPD and asthma.26,45,46,47 8‐isoprostane is a marker of oxidative stress, and raised levels have previously been found in exhaled breath condensate in, for example, patients with asthma, COPD and acute lung injury.26,47,48,49,50
Inflammation in the lungs in patients with asbestosis has been evaluated by gallium‐67 staging38,51 or by measuring inflammatory markers in BAL fluid or in blood.52 The present criteria for a diagnosis of asbestosis exclude gallium scanning, and it is suggested that additional indicators of active inflammation may become useful in future.4,5 The present results show that measurement of exhaled NO using the multiple exhalation flow rate method and analysis of inflammatory markers in the exhaled breath condensate offer a promising non‐invasive means of measuring lung inflammation in patients with asbestosis. Further studies are needed to elucidate whether the progression of the disease or responsiveness to anti‐inflammatory treatment can be evaluated or predicted by these methods.
Acknowledgements
The authors thank Ms Sari Leinonen, Ms Marja‐Leena Lampen, Ms Kirsti Nilsson and Ms Riitta Hietala for skilful technical assistance and Ms Heli Määttä for secretarial help.
Abbreviations
BAL - bronchoalveolar lavage
COPD - chronic obstructive pulmonary disease
CRP - C‐reactive protein
FVC - forced vital capacity
FEV1 - forced expiratory volume in 1 s
FEV50% - forced expiratory flow at 50% of expired volume
HRCT - high resolution computed tomography
IL - interleukin
iNOS - inducible nitric oxide synthase
LTB4 - leukotriene B4
MPO - myeloperoxidase
NO - nitric oxide
Tlco - carbon monoxide transfer factor adjusted for haemoglobin
Tlco/Va - specific carbon monoxide transfer factor adjusted for haemoglobin
Tlno - nitric oxide transfer factor
Vno - a, diffusing rate of nitric oxide from tissue to the alveolar space
Footnotes
This study was supported by grants from the Academy of Finland, Tampere Tuberculosis Foundation, the Medical Research Fund of Tampere University Hospital and from the Finnish Work Environment Fund.
Competing interests: None declared.
References
- 1.Manning C B, Vallyathan V, Mossman B T. Diseases caused by asbestos: mechanisms of injury and disease development. Int Immunopharmacol 20022191–200. [DOI] [PubMed] [Google Scholar]
- 2.Ross M H, Murray J. Occupational respiratory disease in mining. Occup Med 200454304–310. [DOI] [PubMed] [Google Scholar]
- 3.Bolton C, Richards A, Ebden P. Asbestos‐related disease. Hosp Med 200263148–151. [DOI] [PubMed] [Google Scholar]
- 4.American Thoracic Society Diagnosis and initial management of nonmalignant diseases related to asbestos. Am J Respir Crit Care Med 2004170691–715. [DOI] [PubMed] [Google Scholar]
- 5.Ross R M. The clinical diagnosis of asbestosis in this century requires more than a chest radiograph. Chest 20031241120–1128. [DOI] [PubMed] [Google Scholar]
- 6.Kharitonov S A, Barnes P J. Exhaled markers of pulmonary disease. Am J Respir Crit Care Med 20011631693–1722. [DOI] [PubMed] [Google Scholar]
- 7.American Thoracic Society ATS/ERS recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide, 2005. Am J Respir Crit Care Med 2005171912–930. [DOI] [PubMed] [Google Scholar]
- 8.Vallance P, Leiper J. Blocking NO synthesis: how, where and why? Nature Reviews, Drug Discovery 20021939–950. [DOI] [PubMed] [Google Scholar]
- 9.Ricciardolo F L. Multiple roles of nitric oxide in the airways. Thorax 200358175–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alderton W K, Cooper C E, Knowles R G. Nitric oxide synthases: structure, function and inhibition. Biochem J 2001357593–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Korhonen R, Lahti A, Kankaanranta H.et al Nitric oxide production and signaling in inflammation. Curr Drug Targets‐Inflamm Allergy 20054471–479. [DOI] [PubMed] [Google Scholar]
- 12.Alving K, Weitzberg E, Lundberg J M. Increased amount of nitric oxide in exhaled air of asthmatics. Eur Respir J 199361368–1370. [PubMed] [Google Scholar]
- 13.Kharitonov S A, Yates D, Robbins R A.et al Increased nitric oxide in exhaled air of asthmatic patients. Lancet 1994343133–135. [DOI] [PubMed] [Google Scholar]
- 14.Lehtimäki L, Kankaanranta H, Saarelainen S.et al Extended exhaled NO measurement differentiates between alveolar and bronchial inflammation. Am J Respir Crit Care Med 20011631557–1561. [DOI] [PubMed] [Google Scholar]
- 15.Maziak W, Loukides S, Culpitt S.et al Exhaled nitric oxide in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998157998–1002. [DOI] [PubMed] [Google Scholar]
- 16.Paredi P, Kharitonov S A, Loukides S.et al Exhaled nitric oxide is increased in active fibrosing alveolitis. Chest 19991151352–1356. [DOI] [PubMed] [Google Scholar]
- 17.Tsoukias N M, George S C. A two‐compartment model of pulmonary nitric oxide exchange dynamics. J Appl Physiol 199885653–666. [DOI] [PubMed] [Google Scholar]
- 18.George S C, Högman M, Permutt S.et al Modeling pulmonary nitric oxide exchange. J Appl Physiol 200496831–839. [DOI] [PubMed] [Google Scholar]
- 19.Silkoff P E, Sylvester J T, Zamel N.et al Airway nitric oxide diffusion in asthma: role in pulmonary function and bronchial responsiveness. Am J Respir Crit Care Med 20001611218–1228. [DOI] [PubMed] [Google Scholar]
- 20.Lehtimäki L. Measurement of exhaled nitric oxide. Acta Univ Tamperensis 2003925
- 21.Lehtimäki L, Turjanmaa V, Kankaanranta H.et al Increased bronchial nitric oxide production in patients with asthma measured with a novel method of different exhalation flow rates. Ann Med 200032417–423. [DOI] [PubMed] [Google Scholar]
- 22.Shin H W, Rose‐Gottron C M, Cooper D M.et al Airway diffusing capacity of nitric oxide and steroid therapy in asthma. J Appl Physiol 20049665–75. [DOI] [PubMed] [Google Scholar]
- 23.Delclaux C, Mahut B, Zerah‐Lancner F.et al Increased nitric oxide output from alveolar origin during liver cirrhosis versus bronchial source during asthma. Am J Respir Crit Care Med 2002165332–337. [DOI] [PubMed] [Google Scholar]
- 24.Högman M, Holmkvist T, Wegener T.et al Extended NO analysis applied to patients with COPD, allergic asthma and allergic rhinitis. Respir Med 20029624–30. [DOI] [PubMed] [Google Scholar]
- 25.Brindicci C, Ito K, Resta O.et al Exhaled nitric oxide from lung periphery is increased in COPD. Eur Respir J 20052652–59. [DOI] [PubMed] [Google Scholar]
- 26.Horvath I, Hunt J, Barnes P J.et al Exhaled breath condensate: methodological recommendations and unresolved questions. Eur Respir J 200526523–548. [DOI] [PubMed] [Google Scholar]
- 27.Anon Asbestos, asbestosis, and cancer: the Helsinki criteria for diagnosis and attribution. Scand J Work Environ Health 199723311–316. [PubMed] [Google Scholar]
- 28.Oksa P, Suoranta H, Koskinen H.et al High‐resolution computed tomography in the early detection of asbestosis. Int Arch Occup Environ Health 199465299–304. [DOI] [PubMed] [Google Scholar]
- 29.Huuskonen O, Kivisaari L, Zitting A.et al High‐resolution computed tomography classification of lung fibrosis for patients with asbestos‐related disease. Scand J Work Environ Health 200127106–112. [DOI] [PubMed] [Google Scholar]
- 30.Hyde R W, Geigel E J, Olszowka A J.et al Determination of production of nitric oxide by lower airways of humans‐theory. J Appl Physiol 1997821290–1296. [DOI] [PubMed] [Google Scholar]
- 31.Borland C D, Higenbottam T W. A simultaneous single breath measurement of pulmonary diffusing capacity with nitric oxide and carbon monoxide. Eur Respir J 1989256–63. [PubMed] [Google Scholar]
- 32.Viljanen A A, Viljanen B C, Halttunen P K.et al Pulmonary diffusing capacity and volumes in healthy adults measured with the single breath technique. Scand J Clin Lab Invest 198215921–34. [PubMed] [Google Scholar]
- 33.Lehtimäki L, Kankaanranta H, Saarelainen S.et al Inhaled fluticasone decreases bronchial but not alveolar nitric oxide output in asthma. Eur Respir J 200118635–639. [DOI] [PubMed] [Google Scholar]
- 34.Girgis R E, Gugnani M K, Abrams J.et al Partitioning of alveolar and conducting airway nitric oxide in scleroderma lung disease. Am J Respir Crit Care Med 20021651587–1591. [DOI] [PubMed] [Google Scholar]
- 35.Lehtimäki L, Kankaanranta H, Saarelainen S.et al Increased alveolar nitric oxide concentration in asthmatic patients with nocturnal symptoms. Eur Respir J 200220841–845. [DOI] [PubMed] [Google Scholar]
- 36.Lehtimäki L, Kankaanranta H, Saarelainen S.et al Peripheral inflammation in patients with asthmatic symptoms but normal lung function. J Asthma 200542605–609. [DOI] [PubMed] [Google Scholar]
- 37.Mahut B, Delclaux C, Tillie‐Leblond I.et al Both inflammation and remodeling influence nitric oxide output in children with refractory asthma. J Allergy Clin Immunol 2004113252–256. [DOI] [PubMed] [Google Scholar]
- 38.Begin R, Cantin A, Berthiaume Y.et al Clinical features to stage alveolitis in asbestos workers. Am J Ind Med 19858521–536. [DOI] [PubMed] [Google Scholar]
- 39.Saleh D, Barnes P J, Giaid A. Increased production of the potent oxidant peroxynitrite in the lungs of patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 19971551763–1769. [DOI] [PubMed] [Google Scholar]
- 40.Park S H, Aust A E. Regulation of nitric oxide synthase induction by iron and glutathione in asbestos‐treated human lung epithelial cells. Arch Biochem Biophys 199836047–52. [DOI] [PubMed] [Google Scholar]
- 41.Dorger M, Allmeling A M, Kiefmann R.et al Dual role of inducible nitric oxide synthase in acute asbestos‐induced lung injury. Free Radic Biol Med 200233491–501. [DOI] [PubMed] [Google Scholar]
- 42.Dorger M, Allmeling A M, Kiefmann R.et al Early inflammatory response to asbestos exposure in rat and hamster lungs: role of inducible nitric oxide synthase. Toxicol Appl Pharm 200218193–105. [DOI] [PubMed] [Google Scholar]
- 43.Sandrini A, Johnson A R, Thomas P S.et al Fractional exhaled nitric oxide concentration is increased in asbestosis and pleural plaques. Respirology 200611325–329. [DOI] [PubMed] [Google Scholar]
- 44.Garcia J G, Griffith D E, Cohen A B.et al Alveolar macrophages from patients with asbestos exposure release increased levels of leukotriene B4. Am Rev Respir Dis 19891391494–1501. [DOI] [PubMed] [Google Scholar]
- 45.Montuschi P, Kharitonov S A, Ciabattoni G.et al Exhaled leukotrienes and prostaglandins in COPD. Thorax 200358585–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cap P, Chladek J, Pehal F.et al Gas chromatography/mass spectrometry analysis of exhaled leukotrienes in asthmatic patients. Thorax 200459465–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Biernacki W A, Kharitonov S A, Barnes P J. Increased leukotriene B4 and 8‐isoprostane in exhaled breath condensate of patients with exacerbations of COPD. Thorax 200358294–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baraldi E, Ghiro L, Piovan V.et al Increased exhaled 8‐isoprostane in childhood asthma. Chest 200312425–31. [DOI] [PubMed] [Google Scholar]
- 49.Montuschi P, Kharitonov S A, Ciabattoni G.et al Exhaled 8‐isoprostane as a new non‐invasive biomarker of oxidative stress in cystic fibrosis. Thorax 200055205–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Carpenter C T, Price P V, Christman B W. Exhaled breath condensate isoprostanes are elevated in patients with acute lung injury or ARDS. Chest 19981141653–1659. [DOI] [PubMed] [Google Scholar]
- 51.Begin R, Cantin A, Drapeau G.et al Pulmonary uptake of gallium‐67 in asbestos‐exposed humans and sheep. Am Rev Respir Dis 1983127623–630. [DOI] [PubMed] [Google Scholar]
- 52.Oksa P, Huuskonen M S, Jarvisalo J.et al Follow‐up of asbestosis patients and predictors for radiographic progression. Int Arch Occup Environ Health 199871465–471. [DOI] [PubMed] [Google Scholar]