Abstract
Background
Fatigue is a major complaint of multiple sclerosis (MS) patients. However, little is known about its pathophysiological mechanisms. Evidence from chronic fatigue syndrome and studies on sickness behaviour suggest that immune and neuroendocrine factors may play a causative role in the development of fatigue.
Methods
We compared whole blood stimulatory capacity for pro‐ (TNFα, IFNγ) and anti‐inflammatory cytokines (IL‐10) as well as hypothalamo‐pituitary‐adrenal (HPA) axis function in 15 MS patients with marked fatigue and 15 patients without fatigue as determined by the Fatigue Severity Scale (FSS).
Results
Proinflammatory cytokines were significantly higher (TNFα: 478.9 v 228.2 pg/ml, p = 0.01; IFNγ: 57.6 v 27.8 pg/ml; p = 0.01) in MS patients with fatigue. Furthermore, TNFα values significantly correlated with daytime sleepiness as measured by the Epworth Sleepiness Scale (r = 0.64, p = 0.001). Controlling for disease activity (as measured by the Cambridge Multiple Sclerosis Basic Score), disease duration, Expanded Disability Status Scale, and depression further increased the correlation of cytokine production and fatigue. HPA axis activity was not related to fatigue but was modestly correlated with cognitive impairment.
Conclusion
Our data suggest that fatigue in MS is at least partially mediated through activation of proinflammatory cytokines. In line with earlier findings, HPA axis dysfunction seems not to be relevant in MS fatigue pathogenesis but appears to be linked to cognitive impairment. Our findings suggest that increased levels of inflammatory cytokines may be involved in MS fatigue. Investigation of cytokine profiles may increase the understanding of fatigue pathogenesis in MS.
Keywords: cytokines, dexamethasone‐CRH test, fatigue, hypothalamo‐pituitary‐adrenal axis, multiple sclerosis
Multiple sclerosis (MS) is an inflammatory and degenerative disease with a presumed autoimmune aetiology.1 Fatigue is common in patients with MS. It is also one of the most disabling symptoms, with up to two thirds of patients describing fatigue as their main complaint (for review see Schwid et al2).
Despite the high clinical relevance, there are few studies on the pathophysiology of MS fatigue and the mechanisms are not yet clear. Based on the finding that many proinflammatory cytokines have been shown to induce fatigue and somnolence when administered exogenously, an immune mediated process for symptoms of fatigue has been postulated.3 In fact, patients suffering from conditions associated with fatigue, such as chronic fatigue syndrome,4 sleep apnea,5 glucocorticoid withdrawal syndrome,4 and depression,6 are known to have altered levels of cytokines in the peripheral circulation, generally skewed towards a T helper type 1 proinflammatory profile.
However, few studies have investigated the inflammatory markers in MS patients with fatigue. Giovannoni et al7 could not find any correlations between fatigue scores and urinary neopterin, CRP, and sICAM‐1 in a sample of 38 MS patients. However, proinflammatory cytokines such as IFNγ and TNFα, which are considered to play a pivotal role in the development of sickness behaviour,6 have not been systematically examined in MS in this context.
While fatigue is not clearly associated with disease subtype, duration, or degree of disability in MS, it is linked to depressive symptomatology.8 Vice versa, fatigue is a crucial feature of major depression. In recent years it has become clear that the hypothalamo‐pituitary adrenal (HPA) axis system is altered in mood disorders, anxiety, and stress associated pathologies.9 An altered HPA axis function has also been described in chronic fatigue syndrome, characterised by blunted responses to pharmacological challenge.10 A centrally disturbed feedback regulation indicating HPA hyperactivity has been demonstrated in approximately 30% of MS patients by means of the dexamethasone‐CRH (Dex‐CRH) test.11,12,13 However, a small subgroup with HPA hypoactivity has also been identified.11 HPA reactivity in MS patients with prominent fatigue has not yet been studied. Based on evidence from studies in chronic fatigue and depression, a neuroendocrine mechanism of fatigue in MS seems possible. It has been shown that inflammatory cytokines induce activation of the HPA axis. Thus, production of inflammatory mediators within the CNS in MS may not only lead to sickness behaviour and fatigue but also to activation of the HPA axis.
The aim of the present study was to compare proinflammatory (IFNγ, TNFα) and anti‐inflammatory (IL‐10) cytokine production as well as HPA axis function in MS patients with and without fatigue. We hypothesised that fatigue would be associated with proinflammatory cytokine production and increased negative feedback of the HPA axis with inadequately low responses to acute stimuli.
Methods
Subjects
Patients were recruited from our MS database and divided into two groups according to the Fatigue Severity Scale (FSS).14 Patients with FSS mean scores ⩾5 were allocated to the “Fatigue” group, while those with FSS scores <4 were allocated to the “No fatigue” group. We recruited only patients with definitive MS according to Poser criteria,15 and without steroid therapy within the past 4 weeks. Patients with clinically evident psychiatric disease were excluded. The study was approved by the local ethics committee. All subjects were told about the purpose of the study and written informed consent was obtained prior to entering the study.
Clinical scores and questionnaires
All patients underwent neurological screening to classify disease course according to Lublin et al.16 Expanded Disability Status Scale (EDSS) scores17 were rated by an experienced neurologist in our outpatient clinic. Cognitive impairment was evaluated using the Symbol Digit Modalities Test (SDMT).18 The number of correct answers was compared to that of an age and education adjusted healthy control cohort, and individual scores were then transformed into standard deviations (SD) below or above those normal values. Disease impact was furthermore classified according to the Cambridge Multiple Sclerosis Basic Score (CAMBS)19 for the dimensions disability (graded 0–5: 0, fully independent to 5, totally dependent), relapse (graded 0–5: 0, stable to 5, relapse which requires hospitalisation), progression in the last 12 months (graded 0–5: 0, stable to 5, marked malignant progression), and handicap (graded 0–5: 0, no effect on role in life to 5, incapable of any useful role). Affective symptomatology was assessed with the German version of the Hospital Anxiety and Depression Scale (HADS).20 We further assessed fatigue with the modified Fatigue Impact Scale (MFIS).21 The Epworth Sleepiness Scale (ESS)22 was used to assess daytime sleepiness.
Whole blood cytokine stimulation
Cytokines (IFNγ, TNFα, IL‐10) were determined in a whole blood short term culture. Briefly 400 µl of whole blood was added to 3.2 ml of RPMI (endotoxin content <0.01 EU/ml) supplemented with glutamate and streptomycin/penicillin (100 μg/ml) in sterile 5 ml tubes. We used 10 µg/ml phytohaemagglutinin (PHA) as a stimulant for IFNγ and TNFα, and 25 µg/ml PHA as a stimulant for IL‐10. Control cultures without stimulation were also prepared. Tubes were capped and incubated at 37°C for 24 h. Optimal stimulation conditions had been determined previously using different amounts of PHA (2.5–25 µg/ml) and incubation times (3–24 h). Mean±SD delta changes comparing unstimulated and stimulated cultures were 108±53.2 for IL‐10, 42.3±41.5 for IFNγ, and 330.6±229.1 for TNFα, which were in the ranges of previous studies. The caps were removed and samples centrifuged. Supernatants were collected and frozen at −80°C until ELISA was performed. All tests were performed according to the manufacturer (human IL‐10 ELISA, human TNF‐alpha ELISA Version 2, and human IFN‐gamma ELISA; Bender Med Systems, Vienna, Austria). Probes were analysed in duplicates. The plate was read on the E‐max ELISA processor at 450 nm with 620 nm blank filter. The reported sensitivity of the IL‐10 ELISA was 2 pg/ml with an intra‐ and interassay variation of 5% and 6%. The IFNγ assay had a sensitivity of 1.5 pg/ml and an intra‐ and interassay variation of 4.5% and 5.7%, respectively. The reported sensitivity of the TNFα ELISA was 5.8 pg/ml with an intra‐ and interassay variation of 6.9 and 7.4%, respectively.
Dex‐CRH test
Dex‐CRH tests were performed as described earlier.11 Briefly, patients were pretreated with 1.5 mg oral dexamethasone at 23:00 h the night before the test. An i.v. cannula was inserted at 14:30 h and kept patent. Blood was taken at 14:30, 15:00, 15:30, 16:00, and 16:30 h. At 15:00 h, 100 μg synthetic corticotropin releasing hormone (CRH; Ferring, Kiel, Germany) reconstituted in 1 ml 0.09% saline was injected as an i.v. bolus. The five blood samples were drawn in prechilled tubes, anticoagulated with EDTA, and immediately centrifuged at 4°C. Plasma was frozen and stored at −20°C.
Hormone assays
An immunoluminometric two step assay (Nichols Advantage, San Juan Capistrano, CA) was used for the determination of adrenocorticotropic hormone (ACTH) in plasma. Two monoclonal antibodies, one luminescent labelled and the other immobilised on the inner surface of the tube, recognise different binding sites on corticotropin to form a sandwich‐type complex bound to the tube. The luminescence signal is directly proportional to the corticotropin concentration. The detection limit was 1 pg/ml. The intra‐ and interassay coefficients of variation were 2.7% and 6.4%, respectively. Cortisol was measured by a dual antibody chemiluminescence assay using the Elecsys System 2010 (Roche, Grenzach‐Whylen, Germany) kit. The detection limit was 3.6 ng/ml. Intra‐ and interassay coefficients of variation were 1.3% and 1.5%, respectively.
Statistical analysis
Baseline cortisol and ACTH as well as the area under the curve (AUC) over time by trapezoidal estimation were used from the Dex‐CRH test. Because cytokine and endocrine parameters were not normally distributed, we used log transformed values in all analyses.
Group differences (fatigue and no fatigue according to FSS cut offs) in demographic as well as disease describing factors, cytokines, and endocrine parameters were analysed using parametric t tests for independent samples. The χ2 test was used for nominal variables.
For further differentiation of the association of MS fatigue and neuroendocrine and cytokine parameters, we analysed Pearson correlation coefficients with an MS specific measure of fatigue (MFIS) and a score of daytime sleepiness (ESS).
In order to control for potential confounding factors such as disease severity and affective symptomatology, we also computed partial correlations statistically removing the effect of disability (EDSS, CAMBS), interferon medication (interferon v other or no treatment), and disease duration as well as depressive symptoms (HADS). The possible effect of the disease course was investigated by computing correlations for patients with relapsing remitting MS and patients with chronic disease (secondary progressive MS and primary progressive MS) separately.
Results are given as means±SD. All analyses were conducted with statistical software (SPSS 11.0; SPSS, Chicago, IL). A p value less than 0.05 was considered significant. A p value less than 0.10 was accepted in order to detect trends.
Results
Demographic data
Thirty patients were included in the study (table 1). Patients in the two groups differed strongly according to their score on the FSS. Patients with fatigue also had significantly higher mean values in the fatigue scale (MFIS) and in the daytime sleepiness scale (ESS). In addition to the fatigue scores, there were other significant differences between the two groups. The fatigue group showed significantly higher levels on the EDSS, and higher scores on the CAMBS subscales disability, progression, and handicap. The fatigue group further showed more depressive symptoms on the HADS. Four patients had scores above the cut off for overt depression (that is, a score of 12 or higher on the HADS depression subscale). Nineteen patients were receiving immunomodulatory treatment.
Table 1 Demographic data of the study sample.
| Fatigue | No fatigue | p | |
|---|---|---|---|
| n | 15 | 15 | |
| Age | 46.6±11.69 | 42.87±10.17 | 0.36 |
| Gender, M/F | 6/9 | 6/9 | >0.99* |
| Years with MS | 13.80±9.68 | 8.60±5.57 | 0.09 |
| EDSS | 4.36±1.49 | 2.30±1.84 | 0.002 |
| FSS | 6.08±0.68 | 1.51±0.69 | <0.001 |
| MFIS | 58.07±10.55 | 7.53±8.08 | <0.001 |
| ESS | 10.53±4.71 | 3.27±2.37 | <0.001 |
| HADS | 7.93±3.30 | 3.13±3.50 | 0.001 |
| CAMBS | |||
| Disability | 2.93±0.25 | 1.93±0.79 | <0.001 |
| Relapse | 1.33±0.48 | 1.60±0.63 | 0.21 |
| Progression | 2.40±0.91 | 1.53±0.63 | 0.01 |
| Handicap | 3.60±0.82 | 2.00±1.06 | <0.001 |
| SDMT | −0.40±1.72 | 0.13±1.30 | 0.35 |
| Disease course | 6 RR, 8 SP, 1 PP | 11 RR, 2 SP, 2 PP | 0.07* |
| Treatment | 6 immune modulators, 4 immuno‐ suppressants | 9 immune modulators | 0.51* |
Data are given as means±SD; p values according to t test or χ2 test*.
CAMBS, Cambridge Multiple Sclerosis Basic Score; EDSS, Expanded Disability Status Scale; ESS, Epworth Sleepiness Scale; FSS, Fatigue Severity Scale; MFIS, modified Fatigue Impact Scale; HADS, Hospital Anxiety and Depression Scale; SDMT, Symbol Digit Modalities Scale.
In the fatigue group, there was a statistical trend towards longer disease duration (p = 0.09). Disease courses also differed: in the fatigue group, six patients had relapsing remitting MS (RRMS), eight secondary progressive MS (SPMS), and one primary progressive MS (PPMS), whereas in the no fatigue group, 11 patients had RRMS, two SPMS, and two PPMS (χ2 = 5.40, p = 0.07). Five patients in the fatigue group were treated with interferons compared to six patients in the group without fatigue (χ2 = 0.144, p = 0.71).
Cytokine findings
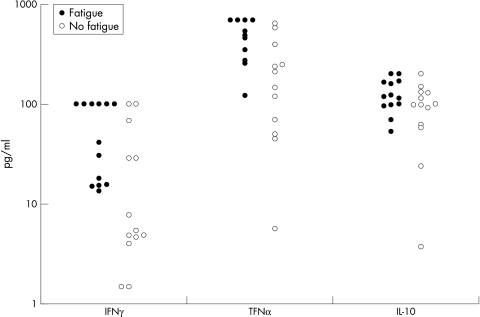
MS patients with fatigue based on the FSS grouping had significantly higher mean IFNγ and TNFα production capacity than patients without fatigue (IFNγ: 57.6±41.6 v 27.8±37.1 pg/ml, p = 0.01; TNFα: 478.9±209.7 v 228.2±208.1 pg/ml, p = 0.01). IL‐10 production showed no significant difference between the two groups (128.2±47.0 v 97.0±52.3 pg/ml, p = 0.10) (fig 1).
Figure 1 Pro‐inflammatory (IFNγ, TNFα) and anti‐inflammatory (IL‐10) cytokines in MS patients with and without fatigue. Each measurement is represented by a dot. See Results section for mean values and statistical differences.
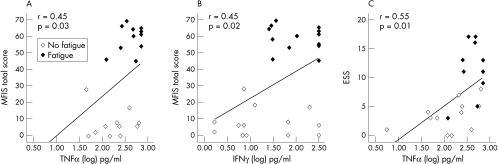
MFIS scores correlated significantly with IFNγ and TNFα but not with IL‐10 production (IFNγ: r = 0.45, p = 0.02; TNFα: r = 0.45, p = 0.03; IL‐10: r = 0.26, p = 0.20; see fig 2A,B).
Figure 2 (A, B) Correlation of MFIS (total score) with (A) TNFα (n = 23) and (B) IFNγ (n = 26). (C) Correlation of ESS with TNFα (n = 23).
The total score and the cognitive and physical subscales of the MFIS correlated equally with the IFNγ and TNFα findings (data not shown). TNFα was the only cytokine correlating significantly with daytime sleepiness as measured by the ESS (TNFα: r = 0.55, p = 0.01, see fig 2C; IFNγ: r = 0.33, p = 0.09; IL‐10: r = 0.24, p = 0.24).
It is important to note that the correlations observed between fatigue and cytokine levels were not due to group differences in disease severity, duration, or depressive symptoms. When statistically controlling for EDSS, disease duration (years), disease severity (CAMBS‐Handicap, CAMBS‐Disability) and progression (CAMBS‐Progression), depressive symptoms (HADS), and interferon treatment, the partial correlation coefficients actually increased (IFNγ: r = 0.68, p = 0.001; TNFα: r = 0.54, p = 0.03). When correlations were computed for RRMS and chronic MS (SPMS and PPMS) separately, the coefficients actually increased (RRMS: IFNγ: r = 0.57, p = 0.03; TNFα: r = 0.54, p = 0.06; SPMS and PPMS: IFNγ: r = 0.47, p = 0.15; TNFα: r = 0.53, p = 0.12).
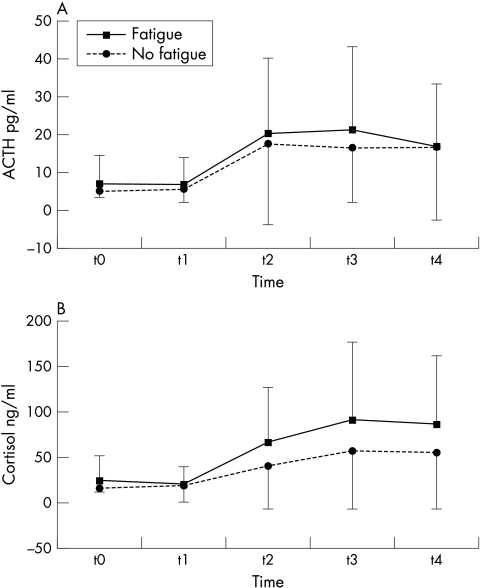
Endocrine findings
In the whole group, only three patients showed non‐suppression in the Dex‐CRH tests according to the cortisol cut off of 40 pg/ml.23 Patients with fatigue and without fatigue showed similar response patterns of baseline ACTH or cortisol as well as AUC ACTH or cortisol in the Dex‐CRH test (fig 3). After controlling for disability, disease duration, depression, disease course, and interferon medication, only the correlation between cortisol baseline and fatigue as measured by the FSS showed a trend (r = 0.38, p = 0.08).
Figure 3 Time course of ACTH and cortisol plasma concentration in the Dex‐CRH test in MS patients with (n = 15) and without (n = 15) fatigue (mean values with SD).
Neither baseline ACTH or cortisol nor AUC ACTH or cortisol correlated significantly with cytokine levels (all coefficients below r = 0.29 after controlling for the confounding factors mentioned above). Further analysis of Dex‐CRH tests in our sample disclosed six patients with low cortisol (<10 pg/ml) after dexamethasone pretreatment and nearly no stimulatory effect of ACTH. While these patients had greater cognitive impairment, they did not have higher fatigue scores, disease activity, or disability in general.
Effects of depression and cognitive impairment
HADS scores did not correlate with any of the measured cytokines (TNFα: r = 0.08, p = 0.70; IFNγ: r = 0.08, p = 0.67; IL‐10: r = −0.001, p = 0.99) or endocrine parameters (ACTH baseline: r = −0.10, p = 0.59; AUC: r = −0.01, p = 0.95; cortisol baseline: r = −0.07, p = 71; AUC: r = 0.03, p = 0.84).
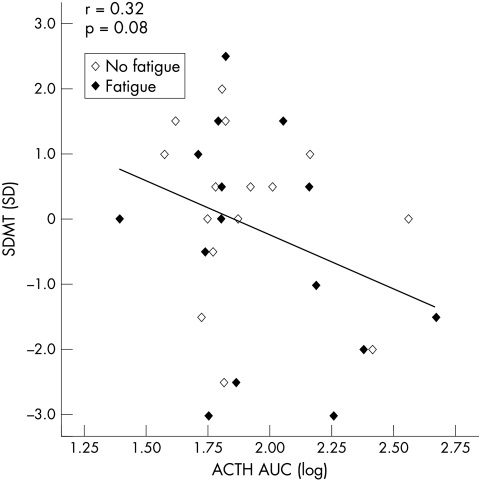
However, cognitive impairment was significantly correlated with suppression of ACTH after dexamethasone pretreatment (ACTH baseline: r = −0.43, p = 0.02) but not with cortisol at baseline (r = −0.20, p = 0.30). Furthermore, cognitive impairment showed a modest correlation with hyperresponsiveness of ACTH AUC in the Dex‐CRH test (r = −0.32, p = 0.08; see fig 4), while cortisol AUC was not correlated (r = −0.09, p = 0.63). Again, correlation coefficients increased after controlling for confounding factors (ACTH baseline: r = −0.53, p = 0.01; cortisol baseline: r = −0.37, p = 0.08; ACTH AUC: r = −0.43, p = 0.04; cortisol AUC: r = −0.22, p = 0.32).
Figure 4 Scatter plot of ACTH AUC (log) corresponding to SDMT (with SD). ACTH AUC values were log transformed and are given in arbitrary units (trapezoidal estimation).
Discussion
This study investigated cytokine and endocrine characteristics in MS patients with marked fatigue according to the FSS compared to patients with low FSS scores. IFNγ and TNFα production capacity in response to PHA was significantly enhanced in MS patients with fatigue. IL‐10 production seemed less affected. TNFα moderately correlated with disease activity as well as with fatigue. TNFα also correlated with daytime sleepiness as measured by the ESS. We thus hypothesise that TNFα is a key mediator of MS fatigue. Furthermore, daytime sleepiness might be a clinical indicator for a cytokine mediated fatigue syndrome.
While there were significant differences regarding disease severity between fatigued and non‐fatigued patients, it is unlikely that the differences are responsible for the observed effects in cytokine levels. There were more patients with secondary progressive disease in the fatigue group. As a result, average disease duration was significantly longer and mean EDSS was higher. Later disease stages are generally considered to have less inflammatory activity, particularly in the secondary progressive phase.1 It would, therefore, be counterintuitive to expect higher levels of proinflammatory cytokines in a group of patients with later‐stage disease. In line with this argument, statistically adjusting for measures of disease severity (EDSS, duration of disease, CAMBS‐Handicap, CAMBS‐Disability) actually further increased the direct correlations of IFNγ and TNFα production capacity and fatigue scores. Thus, it appears unlikely that our findings are confounded by disease severity.
Our findings suggest a key role for TNFα in MS fatigue. Anti‐TNFα treatment strategies have recently been shown to suppress fatigue very effectively in sleep apnea syndrome,24 stressing the relevance of TNFα in fatigue pathogenesis. Our findings are supported by a recent study by Flachenecker et al,25 which reported fatigue scores were correlated with TNFα mRNA production in 27 MS patients with FSS scores ⩾4. IFNγ or IL‐10 levels, however, were not related to fatigue in their study. Cytokine production capacity upon whole blood stimulation represents more of a functional test than a measurement of actual transcribed cytokines, which might render our method more sensitive. These methodological differences might explain the divergent findings concerning IFNγ.
In a previous study on neuropsychological fatigue in MS,26 we found baseline cytokine production levels were not altered in 23 MS patients compared to 25 healthy controls. After a 40 min cognitive stressor, MS patients showed lower IFNγ production capacities, while IL‐10 responses were unaltered. This finding was in accordance with our previous experimental stress studies demonstrating attenuated cytokine responses in MS upon acute experimental physical or psychological stress.27,28 In the abovementioned study, MS patients with fatigue were compared to healthy controls, thus precluding any conclusion on fatigue mechanisms. Furthermore, fatigue scores were lower than in the present study.
Since MS fatigue was associated with enhanced proinflammatory cytokine production capacity in the present study, anti‐inflammatory treatment may represent an alternative treatment option to administering agents which promote wakefulness, such as modafinil, for therapy in MS fatigue. This concept requires further investigation.
Fatigue was not significantly correlated with any parameter of the Dex‐CRH test. Thus, HPA axis dysregulation does not appear to be a general mediator of MS fatigue. This finding confirms previous studies which found no correlation of fatigue scores with Dex‐CRH test results.12,13,29 However, all these reports, including the study presented here, had small sample sizes, thus limiting generalisability.
In a recent study by Gottschalk et al,30 increased HPA activity was reported in MS patients with fatigue. While Gottschalk et al analysed data from a similar number of patients and used an almost identical cut off value for fatigue, their sample exclusively consisted of RRMS patients, most of whom were untreated and had a shorter disease duration as well as lower overall disability. In contrast, our sample contained a significant portion of chronic progressive patients, and more than 50% of our subjects had received immunomodulatory or immunosuppressive treatment. This has likely increased the interindividual variation in HPA measures and in turn decreased our statistical power for this part of the analyses. It is also conceivable that fatigue in RRMS is associated with different factors than fatigue in the more progressive phase of the disease. This may in part explain the stronger association of fatigue and HPA axis function in the study by Gottschalk et al30 compared to our data. Clearly, larger studies of homogeneous patient groups are necessary to clarify the contribution of inflammation, neurodegeneration, neuropsychiatric symptoms, and HPA activity to fatigue in MS.
In the present study, we were able to replicate our previous finding of an association of cognitive dysfunction with hyperreactivity in the Dex‐CRH test.12 Further studies comparing cognitively impaired and unimpaired MS patients using the Dex‐CRH test and MRI are under the way to clarify the mechanisms of this association. As depression scores were low in our sample with only four patients above the clinical cut off score of 12, no conclusion concerning the relation between the HPA axis and depressive symptomatology in MS can be drawn from this study.
So far, attempts to establish objective markers of MS fatigue have been unsuccessful. Recruitment of patients to study fatigue has to rely on patient self report, which mixes symptoms and compensation strategies. By definition, there is considerable overlap of fatigue and depressive symptoms and self report measures may be heavily affected by recall bias.2 The FSS is one of the most commonly used screening scales for fatigue and has been shown to have acceptable reliability and validity in MS.31 However, it is a short screening tool that is biased towards assessing physical fatigue.31
We conclude that higher proinflammatory cytokine production capacity may in part be responsible for symptoms of fatigue in MS patients. Our data suggest that TNFα in particular may be important for daytime sleepiness. Fatigue significantly interferes with activities of daily living and is described by patients as one of the most disabling symptoms.2 In addition to tests of central motor excitability, inhibition pathways, and sympathetic function, cytokine production capacity could be useful to classify patients. Potentially, the investigation of cytokine profiles may increase understanding of fatigue pathogenesis in MS and ultimately help to develop better symptomatic treatment.
Acknowledgements
We thank W Tessmer for excellent help in performing the cytokine studies and R Jung, Department of Clinical Chemistry for analysis of cortisol and ACTH.
Abbreviations
ACTH - adrenocorticotropic hormone
AUC - area under the curve
CAMBS - Cambridge Multiple Sclerosis Basic Score
CRH - corticotropin releasing hormone
Dex‐CRH test - dexamethasone‐CRH test
EDSS - Expanded Disability Status Scale
ESS - Epworth Sleepiness Scale
FSS - Fatigue Severity Scale
HADS - Hospital Anxiety and Depression Scale
HPA axis - hypothalamo‐pituitary‐adrenal axis
MFIS - modified Fatigue Impact Scale
MS - multiple sclerosis
PHA - phytohaemagglutinin
PPMS - primary progressive MS
RRMS - relapsing remitting MS
SD - standard deviation
SDMT - Symbol Digit Modalities Test
SPMS - secondary progressive MS
Footnotes
This study was supported by the Gemeinnützige Hertie‐Stiftung (grant nos: 1.319.120‐01‐01 and 1.01.1/03/013). Stefan M Gold is in part supported by a grant from the Deutsche Forschungsgemeinschaft (DFG; grant no: GO 1357/1‐1)
Competing interests: none declared
References
- 1.Lucchinetti C, Brueck W, Parisi J.et al Heterogeneity of multiple sclerosis lesions: implications for the pathogenesis of demyelination. Ann Neurol 200047707–717. [DOI] [PubMed] [Google Scholar]
- 2.Schwid S R, Covington M, Segal B M.et al Fatigue in multiple sclerosis: current understanding and future directions. J Rehabil Res Dev 200239211–224. [PubMed] [Google Scholar]
- 3.Konsman J P, Parnet P, Dantzer R. Cytokine‐induced sickness behaviour: mechanisms and implications. Trends Neurosci 200225154–159. [DOI] [PubMed] [Google Scholar]
- 4.Papanicolau D A, Amsterdam J D, Levine S.et al Neuroendocrine aspects of chronic fatigue syndrome. Neuroimmunomodulation 20041165–74. [DOI] [PubMed] [Google Scholar]
- 5.Vgontzas A N, Papanicolaou D A, Bixler E O.et al Sleep apnea and daytime sleepiness and fatigue: relation to visceral obesity, insulin resistance, and hypercytokinemia. J Endocrinol Metab 2000851151–1158. [DOI] [PubMed] [Google Scholar]
- 6.Lee B N, Dantzer R, Langley K E.et al A cytokine‐based neuroimmunologic mechanism of cancer related symptoms. Neuroimmunomodulation 200411279–292. [DOI] [PubMed] [Google Scholar]
- 7.Giovannoni G, Thompson A J, Miller D H.et al Fatigue is not associated with raised inflammatory markers in multiple sclerosis. Neurology 2001581134. [DOI] [PubMed] [Google Scholar]
- 8.Kroencke D C, Lynch S G, Denney D R. Fatigue in multiple sclerosis: relationship to depression, disability, and disease pattern. Mult Scler 20006(2)131–136. [DOI] [PubMed] [Google Scholar]
- 9.Gold P W, Gabry K E, Yasuda M R.et al Divergent endocrine abnormalities in melancholic and atypical depression: clinical and pathophysiologic implications. Endocrinol Metab Clin North Am 200231(1)37–62. [DOI] [PubMed] [Google Scholar]
- 10.Cleare A J. The HPA axis and the genesis of chronic fatigue syndrome. Trends Endocrinol Metab 20031555–59. [DOI] [PubMed] [Google Scholar]
- 11.Grasser A, Möller A, Backmund A.et al Heterogeneity of hypothalamic‐pituitary‐adrenal system response to a combined dexamethasone‐CRH test in multiple sclerosis. Exp Clin Endocrinol 199610431–37. [DOI] [PubMed] [Google Scholar]
- 12.Heesen C, Gold S M, Raji A.et al Cognitive impairment correlates with hypothalamo‐pituitary‐adrenal axis dysregulation in multiple sclerosis. Psychoneuroendocrinology 200227505–517. [DOI] [PubMed] [Google Scholar]
- 13.Fassbender K, Schmidt R, Mossner R.et al Mood disorders and dysfunction of the hypothalamic‐pituitary‐adrenal axis in multiple sclerosis: association with cerebral inflammation. Arch Neurol 19985566–72. [DOI] [PubMed] [Google Scholar]
- 14.Krupp L B, LaRocca N G, Muir‐Nash J.et al The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol 1989461121–1123. [DOI] [PubMed] [Google Scholar]
- 15.Poser C M. New diagnostic criteria for multiple sclerosis: guidelines for research protocols. Ann Neurol 198313227–231. [DOI] [PubMed] [Google Scholar]
- 16.Lublin F D, Reingold SC for the National Multiple Sclerosis Society (USA) Advisory Committee on Clinical Trials of New Agents in Multiple Sclerosis Defining the clinical course of multiple sclerosis: results of an international survey. Neurology 199646907–911. [DOI] [PubMed] [Google Scholar]
- 17.Kurtzke J M. Rating neurological impairment in multiple sclerosis: an expanded disability status scale. Neurology 1983331444–1452. [DOI] [PubMed] [Google Scholar]
- 18.Smith A. The Symbol Digit Modalities Test. Learn Disord 1968383–91. [Google Scholar]
- 19.Mumford C, Compston A. Problems with rating scales for multiple sclerosis: a novel approach – the CAMBS score. J Neurol 1993240209–215. [DOI] [PubMed] [Google Scholar]
- 20.Zigmond A S, Snaith R P. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 198367361–370. [DOI] [PubMed] [Google Scholar]
- 21.Multiple Sclerosis Council for Clinical Practice Guidelines Fatigue and multiple sclerosis: evidence‐based management strategies for fatigue in multiple sclerosis. Washington, DC: Paralyzed Veterans of America, October, 1998
- 22.Hoddes E, Zarcone V, Smythe H.et al Quantification of sleepiness: a new approach. Psychophysiology 197310431–436. [DOI] [PubMed] [Google Scholar]
- 23.Von Bardeleben U, Holsboer F. Cortisol response to a continued dexamethasone human corticotrophin‐releasing hormone challenge in patients with depression. J Neuroendocrinol 19891485–488. [DOI] [PubMed] [Google Scholar]
- 24.Vgontzas A N, Zoumakis E, Lin H M.et al Marked decrease in sleepiness in patients with sleep apnea by etanercept, a tumor necrosis factor‐α antagonist. J Endocrinol Metab 2004894409–4413. [DOI] [PubMed] [Google Scholar]
- 25.Flachenecker P, Bihler I, Weber F.et al Cytokine mRNA expression in patients with multiple sclerosis and fatigue. Mult Scler 200410165–169. [DOI] [PubMed] [Google Scholar]
- 26.Heesen C, Koehler G, Gross R.et al Altered cytokine responses to cognitive stress in multiple sclerosis patients with fatigue. Mult Scler 20051151–57. [DOI] [PubMed] [Google Scholar]
- 27.Heesen C, Schulz H, Schmidt M.et al Endocrine and cytokine responses to acute psychological stress in multiple sclerosis. Brain Behav Immun 200216282–287. [DOI] [PubMed] [Google Scholar]
- 28.Heesen C, Gold S M, Hartmann S.et al Endocrine and cytokine response to standardized physical stress in patients with multiple sclerosis and healthy controls. Brain Behav Immun 200317473–481. [DOI] [PubMed] [Google Scholar]
- 29.Then Bergh F, Kümpfel T, Trenkwalder C.et al Dysregulation of the hypothalamo‐pituitary‐adrenal axis is related to the clinical course of MS. Neurology 199953772–777. [DOI] [PubMed] [Google Scholar]
- 30.Gottschalk M, Kümpfel T, Flachenecker P.et al Fatigue and regulation of the hypothalamo‐pituitary‐adrenal axis in multiple sclerosis. Arch Neurol 200562277–280. [DOI] [PubMed] [Google Scholar]
- 31.Tellez N, Rio J, Tintore M.et al Does the Modified Fatigue Impact Scale offer a more comprehensive assessment of fatigue in MS? Mult Scler 200511198–202. [DOI] [PubMed] [Google Scholar]