Abstract
Objective
Subthalamic nucleus (STN) stimulation for patients with medically refractory Parkinson disease (PD) is expanding. Reported experience has provided some indication of techniques, efficacy, and morbidity, but few centres have reported more than 50 patients. To expand this knowledge, we reviewed our experience with a large series of consecutive patients.
Methods
From March 1999 to September 2003, 191 subthalamic stimulator devices (19 unilateral) were implanted in 100 patients with PD at New York Presbyterian Hospital/Columbia University Medical Center. Sixteen patients had undergone a prior surgery for PD (pallidotomy, thalamotomy, or fetal transplant). Microelectrode guided implantations were performed using techniques similar to those described previously. Electrode implantation occurred 1–2 weeks before outpatient pulse generator implantation.
Results
Reductions of dyskinesias and off severity/duration were similar to prior published reports. Morbidity included: 7 device infections (3.7%), 1 cerebral infarct, 1 intracerebral haematoma, 1 subdural haematoma, 1 air embolism, 2 wound haematomas requiring drainage (1.0%), 2 skin erosions over implanted hardware (1.0%), 3 periprocedural seizures (1.6%), 6 brain electrode revisions (3.1%), postoperative confusion in 13 patients (6.8%), and 16 battery failures (8.4%). Of the 100 patients, there were no surgical deaths or permanent new neurological deficits. The average hospital stay for all 100 patients was 3.1 days.
Conclusion
Subthalamic stimulator implantation in a large consecutive series of patients with PD produced significant clinical improvement without mortality or major neurological morbidity. Morbidity primarily involved device infections and hardware/wound revisions.
Keywords: deep brain stimulation, subthalamic nucleus, Parkinson disease, morbidity, techniques
In recent years, chronic deep brain stimulation (DBS) largely replaced ablative stereotactic neurosurgical procedures as a resource for patients with medically refractory Parkinson's disease (PD). Subthalamic nucleus (STN) stimulation has become the preferred method of DBS for the majority of patients with PD. Reported experience has provided some indication of techniques, efficacy and morbidity, but few centres have reported more than 50 patients. Many of the reports of DBS for PD have included stimulation at various sites (globus pallidus internus, STN, ventral intermediate nucleus) within a single report.2,6,25,31 Few reports have detailed a large consecutive series of patient receiving STN stimulation only.1,6,26 To expand the knowledge regarding STN stimulation for PD, we reviewed our experience with a large series of consecutive patients.
CLINICAL MATERIALS AND METHODS
Patient selection/demographics
All microelectrode guided implantations were performed by one of two surgeons (RRG: 89 patients; GMM: 11 patients). Patients were selected by the operating surgeon and a neurologist (BF) specialising in the treatment of movement disorders, based on a history of longstanding dopamine responsive parkinsonism with motor fluctuations consisting of periods of severe immobility (“off"), periods with good motor function (“good on”), and levodopa induced dyskinesias despite optimal medication adjustment. Neuropsychological testing was performed as a routine preoperative screening test and recommended for all patients postoperatively. The results of these tests will be the subject of a separate publication, currently in preparation.
From March 1999 to September 2003, 191 subthalamic stimulator devices were implanted in 100 patients with PD (75 men, 25 women) at New York Presbyterian Hospital/ Columbia University Medical Center (NYPH/CUMC). Mean age was 60.1 years (range 31 to 81), and mean PD symptom duration was 12.9 years (range 2 to 30) (table 1). Of the 100 patients, 19 had unilateral electrode implants (four of these patients subsequently returned for a contralateral implant). Of the 81 patients who had bilateral electrode implants, 73 had simultaneous bilateral implantation, while 8 had planned staged procedures. Sixteen patients had undergone a prior surgery for PD (pallidotomy, thalamotomy, or fetal transplant).
Table 1 Demographics of the implanted patients (n = 100).
| Mean (SD) | Range | |||
|---|---|---|---|---|
| Age (years) | 60.08 (10.77) | 31 to 81 | ||
| PD duration (years) | 12.85 (5.43) | 2 to 30 | ||
| *Unilateral/staged BT (min) | 190.59 (65.18) | 95 to 330 | ||
| *Simultaneous BT (min) | 239.37 (60.23) | 125 to 405 | ||
| Admission duration (days) | 3.13 (1.87) | 1 to 15 | ||
| MER passes per side | 1.85 (1.1) | 1 to 7 |
*Based on the first 88 patients. BT, bilateral time; MER, microelectrode recording.
Operative techniques
All patients were admitted the night prior to surgery and had their PD medications withheld on the morning of the surgical procedure. A Cosman‐Roberts‐Wells (Radionics Inc., Burlington, MA, USA) functional stereotactic frame was used for all 100 patients. Volumetric T1 weighted magnetic resonance imaging (MRI) scan in the axial plane was obtained, which included the region of the AC/PC plane with 1.5 or 2 mm slice thickness. The images were then transferred to a stereotactic planning workstation. For the first 26 patients, a StereoPlan platform (Radionics, Raynham, MA, USA) was employed for surgical planning. During frame placement, earbars were used to minimise roll and yaw. Parallel angulation to an imaginary line connecting the external auditory meatus and the orbital floor was used to align the base ring to the anterior–posterior commissure (AC/PC) line. The desired target was calculated relative to the intercommisural midpoint (ICM) (4 mm posterior, 4 mm inferior, and 12 mm lateral), adjusting for any tilt in all three planes. For the subsequent 74 patients, a Stealth FrameLink (Medtronic Inc., Minneapolis, MN, USA) was used. The surgeon defined the AC/PC plane and Stealth software was used to calculate the STN coordinates relative to the ICM as above, adjusting for the AC/PC length.
DBS electrodes were implanted under local anaesthesia with monitored anaesthetic sedation. Patients were positioned supine with the upper back and head elevated 30° and the neck in neutral position, with the head held in place with a Mayfield adaptor for the stereotactic ring. A single dose of intravenous antibiotic (typically cephazolin 2 g) was given prior to incision. The average duration of surgery was approximately 3 hours and 10 minutes for unilateral implants and 4 hours for bilateral implants (table 1). Hair was shaved in the region of all incisions. A burrhole was placed in the region of the coronal suture, approximately 4 cm off the midline, based on a trajectory path obtained on the planning workstation. The trajectory entered the crown of a gyrus, avoiding deep sulci and the lateral ventricle. High impedance tungsten microelectrodes, 24 mm in length with a tip size of 20–25 µm (FHC Microelectrode Positioning Apparatus, Bowdoinham, ME, USA), were advanced through a guide cannula that ended 30 mm above the calculated anatomical target. Impedance at 1000 Hz was measured at 3 mm and 20 mm after the microelectrode left the cannula. Subsequently, the recording microelectrode was advanced to the target by an electronic stepper microdrive to record the electrical signals from single neuronal units. Background activity was filtered at 100–3000 Hz, preamplified and amplified 10 000–50 000 times, digitised, and sent to an oscilloscope and audio system for real time monitoring and to a digital recording device for offline analysis. The MER coordinate positions, Fourier transforms of discharge frequencies, and action potential morphologies of single units, fibre activity, and background changes were quantified and recorded. Typically, bursting cells of the anterior thalamus were encountered, followed by electrically quieter regions corresponding to the fields of Forel and the zona incerta. Proceeding ventrally, an area of increased background noise and irregularly firing neurones (often responsive to movement) were detected, corresponding to the STN. Further ventrally, below the STN, a region of more rapidly and regularly firing neurones, corresponding to the substantia nigra pars reticulata, were detected.
Subsequently, additional parallel microelectrode tracks were made as needed (not in cases where the diameter and depth of the STN matched those expected from the Schaltenbrand and Wahren atlas23) to ensure placement of the DBS electrode contacts well within the STN. MER was used to “map” the superior and inferior STN borders, and in some cases (such as when the initial track did not identify a significant length of STN), also the anterior, lateral, posterior, and/or medial border(s). The mean number of MER passes was 1.9 per electrode implant (range 1 to 7) (table 1). DBS placement (model 3387 or model 3389; Medtronic Inc.) was performed after removing the microelectrode and guide cannula, positioning a longer guide cannula (with its tip 15 mm above the calculated target depth) in the desired trajectory (as determined by previous MER recordings) and advancing the DBS electrode to the desired depth (generally with the distal electrode within 1 mm of the MER defined lower STN boundary). Excessive proximity to the medial lemniscus or internal capsule was evaluated by macrostimulation via the DBS. Macrostimulation (3 V, pulse width 60 μs, 185 Hz, bipolar configuration between the deepest/cathode and most superficial/anode electrodes) at the final implant site did not produce sustained sensory symptoms or dystonic muscle contractions. Macrostimulation of the DBS electrode was also used to confirm therapeutic tremor suppression and improvement in “off” rigidity and bradykinesia. The electrodes were secured with either a titanium plate or a NavigusT anchoring device (Image Guided Neurologics, Melbourne, FL, USA). For more recent operations, a silastic collar (cut from the protective boot supplied with the DBS electrode) was placed on the DBS electrode wire at the titanium plate contact point, to minimise the risk of insulation erosion or wire damage. MR imaging (same technique as preoperatively) was carried out to confirm the desired electrode location within 48 hours of the DBS electrode implant. Implantation of the lead extension wire and pulse generator (neurostimulator) was carried out 1–2 weeks later under general anaesthesia.
During the series, two significant modifications of technique were made with the goal of reducing risk. Beginning with patient 40, a trough was drilled into the skull above the mastoid to lower the profile of the connector and reduce the risk of scalp erosion. Beginning with patient 80, the connector end of an extension wire was placed over the proximal end of the DBS electrode to allow it to be passed to a subgaleal location in the mastoid region at the time of the first operation. This allowed the extension wire and pulse generator implantation to be performed without reopening the incision at the DBS implant site.
Postoperative care
Several stimulator programming sessions were carried out for the first few months following implantation, and patients were subsequently followed up as necessary by the NYPH/CUMC for Movement Disorders Surgery team, including the implanting neurosurgeon, a neurologist (BF), and nurse (LMW).
RESULTS
Clinical outcome
A subset of 28 patients was rigorously evaluated for the effectiveness of STN stimulation 1 year postoperatively, the results of which have been reported in detail previously.8 In that subset, STN stimulation was associated with a 29.5% reduction in motor scores. Hoehn and Yahr scores and Schwab and England ADL scores in the “on” state and in the “off” state were not significantly changed, and the mean Mini Mental Status Examination score did not change. Patients showed a statistically significant weight gain during the year following surgery, increasing from a mean of 75.6 kg to 78.4 kg. The duration of daily wearing off episodes was reduced by 69%, dyskinesia severity was reduced by 60%, and medication requirements (in levodopa equivalents) declined by 30%. A retrospective chart review of the remaining patients in this series indicated at least as much improvement of wearing off episodes and dyskinesia severity.
Postoperative course
There were no surgical deaths or new permanent neurological deficits among the 100 patients, and 74 patients experienced no morbidity. Perioperative and device related morbidity (191 implants) included: 7 device infections (3.7%; 5% of patients), 6 brain electrode revisions (3.1%), 1 cerebral infarct, 1 intracerebral haematoma, 1 subdural haematoma, 1 air embolism, 2 wound haematomas requiring drainage (1.0%), 2 skin erosions over implanted hardware (1.0%), 3 periprocedural seizures (1.6%), and postoperative confusion in 13 patients (6.8%), a total of 37 complications (table 2). Six patients experienced multiple complications. To date, there have been 16 battery failures (8.4%). The overall complication rate was 37% of patients and 19% of implants. The infections were diagnosed at various times after implantation (mean 4 months; range 1 to 11).
Table 2 Complications associated with DBS STN implantation in 100 patients (no patient experienced permanent sequelae).
| Complication | No. of events | Patients (%) | Electrodes (%) | |||
|---|---|---|---|---|---|---|
| Postoperative confusion | 13 | 13 | 6.8 | |||
| Device infections | 7 | 5 | 3.7 | |||
| Brain electrode revisions | 6 | 5 | 3.1 | |||
| Periprocedural seizures | 3 | 3 | 1.6 | |||
| Wound haematomas requiring drainage | 2 | 2 | 1.0 | |||
| Skin erosions | 2 | 2 | 1.0 | |||
| Subdural haematomas | 1 | 1 | 0.5 | |||
| Intracerebral haematomas | 1 | 1 | 0.5 | |||
| Cerebral infarct | 1 | 1 | 0.5 | |||
| Air embolism | 1 | 1 | 0.5 |
*191 leads.
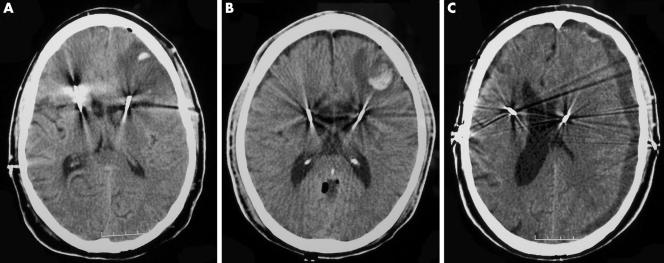
The cerebral infarct occurred in a 52 year old man with coagulopathy induced by factor XI antibody. This condition was diagnosed after right STN implantation, when the patient developed a large subcutaneous haematoma at the pulse generator sight. He was discharged 1 day after left STN electrode implant, but readmitted the following day because of an episode of decreased mental status. CT scan demonstrated a frontal lobe infarct in the region of the newly placed electrode (fig 1A). Within 1 day of hospitalisation, he had returned to his neurological baseline.
Figure 1 Axial CT images demonstrating the three haemorrhagic related morbidities in our 100 patient series. (A) Low intensity left frontal lobe lesion consistent with venous infarction (this patient had a history of anti‐factor XI antibodies); (B) lesion consistent with small frontal lobe haemorrhage; (C) hypointense left subdural collection consistent with subacute haematoma with significant midline shift. Each patient recovered without permanent neurological sequelae.
The intracerebral haematoma occurred in a 54 year old man who was discharged home 1 day after an uneventful bilateral STN implantation. The following day, he had a seizure and was readmitted. Head CT scan showed a small left frontal lobe haemorrhage (fig 1B), and subsequent scans showed no change. He was placed on phenytoin (Dilantin), had no further seizures, and was discharged in his baseline neurological condition 2 days after his seizure.
The subdural haematoma occurred in a 70 year old man who had uneventful bilateral STN implantation and developed confusion and lethargy 1 month after implantation. CT scan revealed a left subdural haematoma (fig 1C), and on examination, he was also found to have an infection at the left pulse generator site. He had burrhole evacuation of the sterile haematoma and removal of the pulse generator and the extension wire, with antibiotic treatment for his infection. Six months later, he had recurrent infection at the residual extension wire and underwent surgery for removal of the residual extension wire, retention of the brain electrode in situ, and antibiotic treatment. Four months later, he had implantation of a new extension wire and pulse generator with uneventful recovery.
Of the seven device infections, three were associated with removal of the entire hardware system (including the brain electrode). Four infections were eradicated with removal of the pulse generator and extension wire only (without removal of the brain electrode). Of the six brain electrode revisions, three were performed because of suboptimal clinical benefit and one revision was performed during the pulse generator implantation surgery because postoperative MRI indicated that the electrode tip had deviated anteriorally and laterally from the intended target. The remaining two revisions, in a single patient who had been getting frequent vigorous scalp massage treatments, were performed because of insulation breaks at the anchoring site. Reimplantation was performed with image guidance only. The brain and target region was seen to be firm and a path was created in the brain using a rigid (Radionics thermister) electrode before passing the DBS electrode. Two hardware revisions were required because of scalp erosion at the connector site (patients 20 and 34). All revisions provided significant clinical benefit.
The average hospital stay for the inpatient electrode implantation for all 100 patients was 3.1 days (table 1), including hospital admission on the day prior to DBS implantation (to facilitate having the patients remain off of their anti‐parkinsonian medication on the implant day). The vast majority of admissions was 3 days or fewer, with only four requiring a hospital stay of >6 days (fig 2). In each of these cases, the extended length of stay was directly attributable to postoperative confusion. Analysis of the 13 patients with postoperative confusion revealed no statistically significant differences in age (58.5 v 60.1 years; SD 10.8) or duration of PD (11.8 v 12.9 years; SD 5.6) compared with the overall mean. Of the 13 patients, 11 experienced confusion following bilateral electrode implantation. However, analysis of these patients revealed no statistically significant difference in length of operation (252.27 v 236.42 minutes; SD 62.13) compared with bilaterally implanted patients who did not experience confusion.
Figure 2 Two dimensional histogram depicting the distribution of hospital stay (days) for the 100 patients (113 admissions).
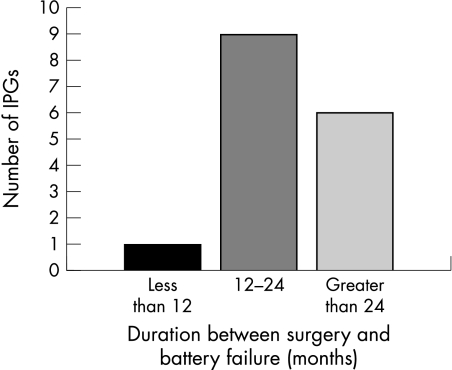
For the 16 battery failures (rundown), the average duration from surgery to failure was 24.6 months, with the majority of failures occurring 12–24 months postoperatively (fig 3). Battery replacements were accomplished without any complications. The remaining devices that have not yet required replacement (up to September 2004) have been in place for an average of 22.6 months (range 12 to 57).
Figure 3 Two dimensional histogram depicting the distribution of duration (months) from implantation to battery failure in the 11 patients (16 batteries) who experienced battery failure.
DISCUSSION
Ablative treatments for PD, including thalamotomy, pallidotomy, and subthalamotomy have been reported to produce significant clinical benefits.4,7,27 However, even unilateral thalamotomy and pallidotomy have been associated with permanent neurological morbidity and (in the case of pallidotomy) significant mortality.5,24 A recent review of unilateral pallidotomy reported an overall mortality rate of 1.2% and a permanent morbidity rate of 13.8%.5 In this same review, bilateral pallidotomy was reported to have a permanent neurological morbidity rate of >30%.5 In a recent small series, bilateral subthalamotomy had a morbidity (hemiballism resolving 4 weeks postoperatively) rate of 25%, with unilateral subthalamotomy having both mortality and permanent neurological morbidity rates of 25%.27
Non‐destructive chronic DBS therapy has been reported to provide similar (or better) clinical benefits and a lower risk of permanent neurological morbidity.9,29 The clinical benefits of DBS therapy are in general dependent on continuous stimulation, implying that it produces no significant permanent tissue injury or dysfunction. In contrast to lesioning procedures, DBS therapy is complicated by device related complications such as infections and hardware failures. In general, these complications are treatable by device removal or revision and do not produce permanent morbidity.10,13,19
For this study, we reviewed 19 published studies reporting a total of 913 patients with PD who had STN implants (table 3).1,2,3,6,11,12,14,15,16,17,18,20,21,22,25,26,28,30,32 The mortality rate was 0.3% (three deaths). Eighteen of these reports described the occurrence of postoperative confusion (the incidence was 14.7%). The incidence of reported infections/lead erosions was 3.1% (36 events/1157 electrodes). All of our infections were diagnosed within 11 months of surgery. Symptomatic intracerebral haemorrhage was reported in 0.9% of lead implants (17/1796), at least five of which (0.3%) were reported to be associated with permanent neurological deficits. The complications in this series (summarised in table 2) compare favourably with these previous reports (table 3). It is worthwhile noting that this included all patients implanted at our centre to September 2003. Procedure related seizures occurred in 3% of the patients in our series. Six of the published studies have included reference to procedure related seizures, with incidence ranging from 2.9 to 8.6% (table 3). Only two previous reports1,6 have reported the incidence and variety of complications in a consecutive series of at least 100 patients, restricted to DBS STN implantation for PD. Only one of these series (253 electrode implantations in 127 patients, see table 3)1 was a single centre series similar to ours.
Table 3 Literature review of complications of DBS STN implantation*.
| Authors and year | No. of patients (electrodes) | Minimum no. of months of follow up | Mortality (% of patients) and cause | ICH (% of leads) | Infection or erosion (% of leads) | Other serious complication (% of patients) | Confusion (% of patients) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kumar et al., 1998 | 22 (44) | 12 | 0 (0) | 1 (2.3) | NR | 1 lead migration (4.5) | 7 (31.8) | |||||||
| Limousin et al., 1998 | 24 (48) | 12 | 0 (0) | 1 (2.1); persistent aphasia/severe paralysis | 1 (2.1) | NR | 8 (33.3) | |||||||
| Benabid et al., 2000 | 127 (253) | NR | 1 (0.8); PE | 5 (2.0); 2 symptomatic, 3 asymptomatic | “Less than 5%” | 4 transient hemiballism (3.1) | 7 (5.5) | |||||||
| Houeto et al., 2000 | 23 (46) | 6 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 3 (13.0) | |||||||
| Rodriguez‐Oroz et al., 2000 | 15 (30) | 12 | 0 (0) | 2 (6.7); permanent motor deficits | NR | 1 wound haematoma requiring drainage (6.7) | 1 (6.7) | |||||||
| Beric et al., 2001 | 61 (122) | NR | 0 (0) | NR | NR | NR | 4 (6.6) | |||||||
| Broggi et al., 2001 | 17 (34) | 6 | 0 (0) | 1 (2.9); silent | NR | NR | 3 (17.6) | |||||||
| DBS for PD Group, 2001 | 102 (198) | 6 | 0 (0) | 3 (1.5) | 4 (2.5) | 3 seizures (2.9), 1 PE (0.9), 1 brachial plexus injury (0.9), 1 nonhaemorhagic paralysis (0.9), 3 lead migrations (2.9), 1 lead break (0.9) | 1 (1.0) | |||||||
| Lopiano et al., 2001 | 20 (40) | NR | 0 (0) | NR | 1 (2.5) | NR | 2 (10.0) | |||||||
| Ostergaard et al., 2002 | 26 (52) | 12 | 0 (0) | NR | 1 (1.9) | 1 seizure (3.8) | 3 (11.5) | |||||||
| Simuni et al., 2002 | 13 (26) | 12 | 1 (7.7); PE | 1 (3.8); transient | 2 (7.7) | 1 seizure (7.7), 1 subdural haematoma (7.7%) | 1 (7.7) | |||||||
| Starr et al., 2002 | 44 (76) | NR | 0 (0) | 2 (2.6) | 2 (2.6) | 2 seizures (4.5), 1 lead break (2.3) | 9 (20.5) | |||||||
| Tavella et al., 2002 | 47 (94) | 3 | 0 (0) | NR | 1 (1.1) | NR | 7 (14.9) | |||||||
| Vesper et al., 2002 | 38 (76) | 12 | 0 (0) | NR | 2 (2.6) | NR | 10 (26.3) | |||||||
| Herzog et al., 2003 | 48 (96) | 6 | 0 (0) | 1 (1.0); transient | NR | 1 dislocation of impulse generator (2.1), 1 subdural haematoma (2.1) | 7 (14.6) | |||||||
| Krack et al., 2003 | 49 (98) | 3 (5 years in 42) | 1 (2.0); ICH | 10 (10.2); 2 permanent, 8 asymptomatic | 5 (5.0) | 2 seizures (4.1), 2 contusions (4.1), 1 ballism (2.0), 1 depressive suicide (2.0), 1 heart failure (2.0) | 12 (24.5) | |||||||
| Landi et al., 2003 | 72 (144) | 6 | 0 (0) | 1 (0.7); transient | 4 (2.8) | 1 PE (1.4) | 8 (11.1) | |||||||
| Pahwa et al., 2003 | 35 (70 | 12 | 0 (0) | 0 (0) | 5 (7.1) | 1 fracture (2.9), 3 seizures (8.6), | 5 (14.3) | |||||||
| Tamma et al., 2003 | 30 (60) | 12 | 0 (0) | NR | NR | 3 contusions (10.0) | 9 (30.0) | |||||||
| Present study | 100 (191) | 6 | 0 (0) | 1 (0.5); transient | 9 (4.7) | 3 seizures (3.0), 2 wound haematomas requiring drainage (2.0), 1 subdural haematoma (1.0), 1 extension wire replacement (1.0) | 13 (13.0) |
*NR, Not reported; ICH, intracerebral haemorrhage; PE, pulmonary embolism. Mortality rate 3/913 (0.3%); symptomatic ICH 17/1796(0.9%). Total incidence of confusion (patients) 120/913 (13.1%) (without DBS 119/811 (14.7%)) (range 5.5 to 33.3%). Total incidence of reported infection/erosion (leads) 36/1157 (3.1%) (range 0 to 7.7%)
The other series that have been reported1,2,3,6,11,12,14,15,16,17,18,20,21,22,25,26,28,30,32 do not address the issue of battery failures in a way that would allow us to compare our experience (STN patients with at least 1 year of follow up) with theirs. Our experience is that the battery life is quite variable, as predicted by the manufacturer (Medtronic). Of the 191 implanted batteries for which we have at least 1 year's follow up, 16 (8.4%) have already reached battery failure. Three of these failures occurred in one patient who had wire breakage due to vigorous scalp massages (referred to above). In retrospect, it was realised that his battery drainage had occurred because the electrode insulation had broken down and led to current leakage, which caused rapid battery drainage. This occurrence should be taken into account when examining our battery failure rate. The remaining 13 battery failures we have seen seem to be at the appropriate time based on the parameters that were programmed (including the current). It will be interesting to learn from our future experience (and that of others) what will be the range and average battery life.
It may be worth noting that this series included a significant number of implants with each of two types of electrodes. The 3389 electrodes span the length of 7.5 mm, while the 3387 electrode span is 10.5 mm. The deepest contact was placed at the same depth for both electrode types, thus the highest contact would be 3 mm higher (anatomically) with the 3387 electrode. This might be expected to produce a systematic difference in stimulation responses between the two electrode types (both for intraoperative and subsequent stimulation), but none has been seen. Bipolar stimulation effects generally appear to be dominated by the cathode, which was typically the deepest contact intraoperatively. This may explain the lack of difference between the two electrode types. For both electrode types, one of the central electrodes is typically found to provide the best clinical response.
One important technical issue has been the anchoring of the DBS electrode to the skull. For many of the patients in this series, we used titanium plates rather than the Navigus plastic anchoring device, both because of the lower profile (improved cosmesis) and the ease of allowing fine adjustment of the electrode depth before final anchoring. The two wire insulation breakages that were noted in this series occurred at the point of anchoring by the titanium plate. It is possible that such a breakage would not have occurred with the plastic anchoring device or with our modification using a silastic collar at the anchoring place contact point. It is noteworthy that these two breakages (occurring in the same patient) were associated with the unusual circumstance of a patient receiving frequent vigorous scalp massages.
Another important technical note is that the two modifications made during the series each appeared to contribute to reducing morbidity. The first modification (lowering the profile of the connector) resulted in no subsequent scalp erosions (61 patients) compared with two beforehand (39 patients). The second modification (enabling the extension wire and pulse generator implantation to be performed without reopening the DBS implant incision site) resulted in only one subsequent device infection (21 patients) compared with six beforehand (79 patients). In addition to reducing morbidity, each modification significantly increased patient comfort. The rate of other morbidities did not appear to change throughout the course of this series.
CONCLUSION
In this second largest reported consecutive single centre series, subthalamic stimulator implantation of patients with PD was carried out without major neurological morbidity or mortality. Morbidity primarily involved device infections and hardware/wound revisions. The results from this study reinforce previous reports that subthalamic stimulation produces significant benefits in patients with advanced PD, particularly improving motor fluctuations, with a low incidence of severe neurological morbidity and mortality.
ACKNOWLEDGEMENTS
We would like to thank M Marshall and E Mejia for invaluable secretarial assistance.
Abbreviations
AC - anterior commissure
DBS - deep brain stimulation
ICM - intercommisural midpoint
MER - microelectrode recording
MRI - magnetic resonance imaging
NYPH/CUMC - New York Presbyterian Hospital/Columbia University Medical Center
PC - posterior commissure
PD - Parkinson's disease
STN - subthalamic nucleus
Footnotes
Competing interests: none of the authors received any financial support in conjunction with the generation of this submission.
References
- 1.Benabid A L, Krack P P, Benazzouz A.et al Deep brain stimulation of the subthalamic nucleus for Parkinson disease: methodologic aspects and clinical criteria. Neurology 200055(suppl 6)S40–S44. [PubMed] [Google Scholar]
- 2.Beric A, Kelly P J, Rezai A.et al Complications of deep brain stimulation surgery. Stereotact Funct Neurosurg 20017773–78. [DOI] [PubMed] [Google Scholar]
- 3.Broggi G, Franzini A, Ferroli P.et al Effect of bilateral subthalamic electrical stimulation in Parkinson disease. Surg Neurol 20015689–96. [DOI] [PubMed] [Google Scholar]
- 4.Burchiel K J. Thalamotomy for movement disorders. Neurosurg Clin N Am 1995655–71. [PubMed] [Google Scholar]
- 5.de Bie R M, de Haan R J, Schuurman P R.et al Morbidity and mortality following pallidotomy in Parkinson disease: a systematic review. Neurology 2002581008–1012. [DOI] [PubMed] [Google Scholar]
- 6.Deep‐Brain Stimulation for Parkinson Disease Study Group Deep‐brain stimulation of the subthalamic nucleus or the pars interna of the globus pallidus in Parkinson disease. N Engl J Med 2001345956–963. [DOI] [PubMed] [Google Scholar]
- 7.Fine J, Duff J, Chen R.et al Long‐term follow‐up of unilateral pallidotomy in advanced Parkinson disease. N Engl J Med 20003421708–1714. [DOI] [PubMed] [Google Scholar]
- 8.Ford B, Winfield L, Pullman S L.et al Subthalamic nucleus stimulation in advanced Parkinson disease: blinded assessments at one year follow up. J Neurol Neurosurg Psychiatry 2004751255–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gregory R. Surgery for movement disorders. J Neurol Neurosurg Psychiatry 200272(suppl 1)I32–I35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hamel W, Schrader B, Weinert D.et al Technical complication in deep brain stimulation. Zentralbl Neurochir 200263124–127. [DOI] [PubMed] [Google Scholar]
- 11.Herzog J, Volkmann J, Krack P.et al Two‐year follow‐up of subthalamic deep brain stimulation in Parkinson disease. Mov Disord 2003181332–1337. [DOI] [PubMed] [Google Scholar]
- 12.Houeto J L, Damier P, Bejjani P B.et al Subthalamic stimulation in Parkinson disease: a multidisciplinary approach. Arch Neurol 200057461–465. [DOI] [PubMed] [Google Scholar]
- 13.Joint C, Nandi D, Parkin S.et al Hardware‐related problems of deep brain stimulation. Mov Disord 200217(suppl 3)S175–S180. [DOI] [PubMed] [Google Scholar]
- 14.Krack P, Batir A, Van Blercom N.et al Five‐year follow‐up of bilateral stimulation of the subthalamic nucleus in advanced Parkinson disease. N Engl J Med 20033491925–1934. [DOI] [PubMed] [Google Scholar]
- 15.Kumar R, Lozano A M, Kim Y J.et al Double‐blind evaluation of subthalamic nucleus deep brain stimulation in advanced Parkinson disease. Neurology 199851850–855. [DOI] [PubMed] [Google Scholar]
- 16.Landi A, Parolin M, Piolti R.et al Deep brain stimulation for the treatment of Parkinson disease: the experience of the Neurosurgical Department in Monza. Neurol Sci 200324(suppl 1)S43–S44. [DOI] [PubMed] [Google Scholar]
- 17.Limousin P, Krack P, Pollak P.et al Electrical stimulation of the subthalamic nucleus in advanced Parkinson disease. N Engl J Med 19983391105–1111. [DOI] [PubMed] [Google Scholar]
- 18.Lopiano L, Rizzone M, Perozzo P.et al Deep brain stimulation of the subthalamic nucleus: selection of patients and clinical results. Neurol Sci 20012267–68. [DOI] [PubMed] [Google Scholar]
- 19.Oh M Y, Abosch A, Kim S H.et al Long‐term hardware‐related complications of deep brain stimulation. Neurosurgery 2002501268–1276. [DOI] [PubMed] [Google Scholar]
- 20.Ostergaard K, Sunde N, Dupont E. Effects of bilateral stimulation of the subthalamic nucleus in patients with severe Parkinson disease and motor fluctuations. Mov Disord 200217693–700. [DOI] [PubMed] [Google Scholar]
- 21.Pahwa R, Wilkinson S B, Overman J.et al Bilateral subthalamic stimulation in patients with Parkinson disease: long‐term follow up. J Neurosurg 20039971–77. [DOI] [PubMed] [Google Scholar]
- 22.Rodriguez‐Oroz M C, Gorospe A, Guridi J.et al Bilateral deep brain stimulation of the subthalamic nucleus in Parkinson disease. Neurology 200055(suppl 6)S45–S51. [PubMed] [Google Scholar]
- 23.Schaltenbrand G, Bailey P.Introduction to stereotaxis with an atlas of the human brain. Stuttgart: Thieme, 1959
- 24.Schuurman P R, Bosch D A, Bossuyt P M.et al A comparison of continuous thalamic stimulation and thalamotomy for suppression of severe tremor. N Engl J Med 2000342461–468. [DOI] [PubMed] [Google Scholar]
- 25.Simuni T, Jaggi J L, Mulholland H.et al Bilateral stimulation of the subthalamic nucleus in patients with Parkinson disease: a study of efficacy and safety. J Neurosurg 200296666–672. [DOI] [PubMed] [Google Scholar]
- 26.Starr P A, Christine C W, Theodosopoulos P V.et al Implantation of deep brain stimulators into the subthalamic nucleus: technical approach and magnetic resonance imaging‐verified lead locations. J Neurosurg 200297370–387. [DOI] [PubMed] [Google Scholar]
- 27.Su P C, Tseng H M, Liu H M.et al Subthalamotomy for advanced Parkinson disease. J Neurosurg 200297598–606. [DOI] [PubMed] [Google Scholar]
- 28.Tamma F, Rampini P, Egidi M.et al Deep brain stimulation for Parkinson disease: the experience of the Policlinico‐San Paolo Group in Milan. Neurol Sci 200 24(suppl 1)S41–S42. [DOI] [PubMed] [Google Scholar]
- 29.Tasker R R. Deep brain stimulation is preferable to thalamotomy for tremor suppression. Surg Neurol 199849145–154. [DOI] [PubMed] [Google Scholar]
- 30.Tavella A, Bergamasco B, Bosticco E.et al Deep brain stimulation of the subthalamic nucleus in Parkinson disease: long‐term follow‐up. Neurol Sci 200223(suppl 2)S111–S112. [DOI] [PubMed] [Google Scholar]
- 31.Umemura A, Jaggi J L, Hurtig H I.et al Deep brain stimulation for movement disorders: morbidity and mortality in 109 patients. J Neurosurg 200398779–784. [DOI] [PubMed] [Google Scholar]
- 32.Vesper J, Klostermann F, Stockhammer F.et al Results of chronic subthalamic nucleus stimulation for Parkinson disease: a 1‐year follow‐up study. Surg Neurol 200257306–313. [DOI] [PubMed] [Google Scholar]