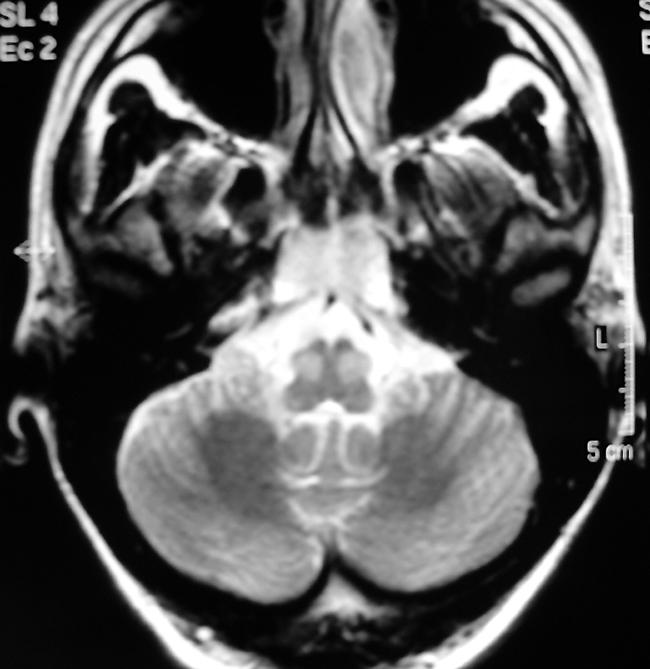
A 39 years old woman was admitted to neurological department after acute onset of right haemiparesis, vertigo, and oculomotor paresis. Magnetic resonance (MR) disclosed multiple ischaemic lesions in the brainstem involving pons and mesencephalon, and altered signal in the basilar artery corresponding to partial trombosis. The patient developed coma, was admitted to the ICU, and treated with anticoagulant drugs. Her clinical condition gradually improved: after 1 month she was alert, dysartric, there was bilateral dysmetria of the arms without paresis and a bilateral orizzontal gaze paresis with dissociated nystagmus (one and half syndrome), and no palatal myoclonus was present. A second MR was performed: no findings of basilar occlusion were present, ischaemic damage was evident in the pons and in the median region of the midbrain. An altered bilateral and symmetric signal in the inferior olivar nucleus was also evident (increased signal on T2 and proton density images) (see figure).
Hypertrophic olivary degeneration is a rare finding secondary to focal lesions of the brain stem involving a functional system—the Guillain–Mollaret triangle—composed of the contralateral dentate nucleus, the ipsilateral red nucleus, the ipsilateral central tegmental tract, and the ipsilateral inferior olivary nucleus.
In the CNS the degeneration of an anatomical structure is usually characterised by neuronal loss replaced by proliferation of glial elements. Unique to the inferior olivary nucleus is transneuronal degeneration resulting in hypertrophy of the targeted region. Pathologically, cell body enlargement, vacuolation of the cytoplasm, astrocytic hyperplasia and proliferation, demyelination, and fibrillary gliosis have been described. The palatal myoclonus and other involuntary movements are the hallmark symptom of this disease and have been described since 1886.
Most commonly a lesion involving central tegmental tract causes unilateral olivary degeneration. We consider our patient having bilateral hypertrophic degeneration from a unique ischaemic lesion located in the midbrain and corresponding to region of Werneking decussation (decussation of the superior cerebellar peduncle or brachium conjunctivum). Central tegmental tract, arising from the parvocellular part of red nucleus, cannot be damaged by a unique lesion located in mesencephalic tegmentum. The same lesion involving bilateral cerebello‐rubro fibers explains bilateral cerebellar ataxia of the arms.
The differential diagnosis of signal hyperintensity on T2 weighted images within the pontomedullary region includes tumours, demyelinating lesions, infarction, and inflammatory processes. The lack of contrast enhancement, however, is against many tumourous entities or an infectious origin. Therefore, a T2 hyperintense non‐contrast enhancing lesion that is accompanied by enlargement of the olivary nucleus, particularly if bilateral and simmetric, as in this patient, can be explained only by hypertrophic olivary degeneration; typically MR hyperintensity was evident after one month, the signal hyperintensity was absent in the first neuroradiological examination. In the next few months the patient could complain palatal myoclonus that is not evident now and has been described until one year after initial damage.
References
- 1.Krings T, Foltys H, Meister I G.et al Hypertrophic olivary degeneration following pontine haemorrhage: hypertensive crisis or cavernous haemangioma bleeding? J Neurol Neurosurg Psychiatry 200374797–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salamon‐Murayama N, Russell E J, Rabin B M. Diagnosis please. Case 17: hypertrophic olivary degeneration secondary to pontine haemorrhage, Radiology 199921381417. [DOI] [PubMed] [Google Scholar]
- 3.Goyal M, Versnick E, Tuite P.et al Hypertrophic olivary degeneration: metaanalysis of the temporal evolution of MR findings. Am J Neuroradiol 2000211073–1077. [PMC free article] [PubMed] [Google Scholar]


