Abstract
We aimed to identify the attendance rate for all head injuries, and for moderate to severe head injury (MSHI), in an emergency department (ED), and related risk factors for MSHI, including age, sex, area of residence, and socioeconomic status (SES). This was a retrospective descriptive epidemiological study of an ED database of head injury attendances over 6 years, carried out in an ED that serves both urban and mixed rural and urban areas, with a wide socioeconomic range, and a total population of 344 600. The main outcome measure was rates of attendance for head injury. Head injury presentations accounted for 3.4% of all attendances per year. An overall rate of 453 per 100 000 was found for all head injuries, of which 40 per 100 000 were moderate to severe (10.9%). Urban residents had significantly greater risk of presenting with MSHI compared with residents of mixed/rural areas. Males were more at risk than females, and children and adolescents had higher risk of MSHI. A high attendance rate of MSHI was found in the <5 year old age group in urban areas for both sexes. A gradient, with higher attendance in groups with lower SES, was observed for children in urban areas, while the gradient was reversed in mixed/rural areas. Head injuries are a relatively common cause of attendance at ED. There is significant variation in attendance with MSHI with regard to sex, age, socioeconomic factors, and type of area of residence. The planning and delivery of preventative and management services may be improved by such analyses.
Keywords: epidemiology, head injury, brain injury, emergency medicine, public health
Head injury (HI) is a leading cause of disability, and survivors often suffer cognitive, mood, and behavioural disorders.1 The societal cost of disability following HI can be substantial as services need to be provided on a long term, even life long, basis.2 There are, however, few research studies on incidence and risk factors for injury, particularly of the more serious types. Rates of attendance at an emergency department (ED) has been argued to be a reliable guide to community incidence of head injury.3 A study of data gathered in 1974 in Scotland revealed an attendance rate of 1780 per 100 000.3 A UK study across the North West Regional Health Authority of those discharged from hospital following HI identified a rate of 297 per 100 000, based on data collected in 1985.4 Substantial local variation in rates were found (from 88–886 per 100 000) across health districts in the region. More recently, a hospitalised incidence rate of 229 per 100 000 was calculated for England for HI in 2001–2002.5 Again, significant local variation was noted (from 91–419 per 100 000 across health authorities). In the UK, “serious” HI is estimated to have an incidence rate of 52 per 100 000, while an incidence of 12 per 100 000 was reported in Australia for “severe” brain injury.6,7 Risk factors for HI include alcohol intoxication, age, and sex.8,9 Urban areas of residence have been suggested to be a protective factor in Australia but a risk factor in the USA.10,11 Markers of social deprivation and infrastructure issues, such as unemployment and lack of public transport, respectively, have been associated with greater hospital attendance with HI in general.12,13 Definitions and codings of HI have varied in HI epidemiology research, which has made meaningful comparisons of rates and risk factors between studies problematic.14,15 There is, in particular, a lack of analyses of specific risk factors associated with attendance with moderate to severe HI (MSHI), and calls for such analyses.16 We aimed to examine both the general rate of HI of all types, and specific rates and risk factors for MSHI.
In this study, we aimed to identify attendance rates for all HI in an ED in a UK population, and to identify the risk factors associated with attendance for MSHI, including: area of residence (urban versus mixed/rural), age, sex, and socioeconomic status (SES).
MATERIALS AND METHODS
This was a retrospective study based on an existing dataset, created from a dedicated ED database at the Royal Devon and Exeter Hospital. All attendances are logged on the database. Six complete years were selected for analyses (1997–2003). All cases from April 1997 to March 2003 with a diagnostic code relating to HI were selected (n = 11, 700). Codes (18, minor HI; code 19, moderate to severe HI) used were those established by the National Health Service Centre for Clinical Coding and Classification, based on ICD 10.15 Within this system, it is possible to identify HI (any traumatic injuries to the head and brain) and MSHI (when Glasgow Coma Scale scores ⩽12 were recorded).16
Resident based primary care trust (PCT) population estimates were extracted from the general practitioner registration database at the mid point of the study. A combined area estimate population of 344 600 was established. Crude attendance rates (all rates are per 100 000 population) were calculated as an annual average of the 6 years of data by area of residence and environment (urban or mixed/rural). Annual average age specific attendance rates by 5 year age band were used. For MSHI, risk ratios were calculated for each age band to examine the effect of PCT and sex. The effect of socioeconomic deprivation was estimated by allocating each attendance, using postcode, to a ward of residence, stratifying the wards by quartile of deprivation least as assessed by the Index of Multiple Deprivation (2000).17 This index is derived from six domain scores: employment, income, education, skills and training, health deprivation and disability, geographical access to services, and housing. Those in quartile group 1 are most affluent, and those in group 4, most deprived.
RESULTS
HI presentations at the ED accounted for 3.4% of all cases per year. The overall attendance was 453 per 100 000, of which 40 per 100 000 were moderate to severe (10.9%). Attendance rates for all HI and MSHI and by area of residence and sex are shown in table 1.
Table 1 Attendance rates for all HI and MSHI by area of residence and sex, per 100 000.
| All HI | MSHI | |||
|---|---|---|---|---|
| Urban | ||||
| Male | 1037.3 | 78.3 | ||
| Female | 626.9 | 38.8 | ||
| All | 826.9 | 55.6 | ||
| Mixed/rural | ||||
| Male | 273.6 | 39.5 | ||
| Female | 178.0 | 20.4 | ||
| All | 223.8 | 29.6 | ||
| Total | ||||
| Male | 567.0 | 52.5 | ||
| Female | 347.1 | 27.4 | ||
| All | 453.1 | 39.5 |
HI, head injury; MSHI, moderate to severe head injury.
Risk factors
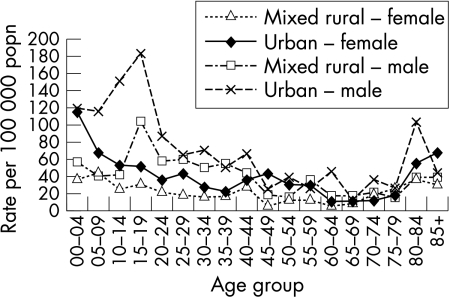
For the MSHI group, rates were highest for the 15–19 age group for males (fig 1). From 24 years of age onwards, there is a gradual decline up to the age of 79 years, and then an increase. It is worth noting that urban male and female patients <5 years old are strongly represented.
Figure 1 Attendance rates for moderate tosevere head injury per 100 000 population for each 5 year age band by sex and area of residence.
Risk ratio analyses revealed a consistent trend for higher rates in urban areas, particularly marked for children aged between 0 and 14 years. From the ages of 5–14 years, an increased risk for males emerged. This trend is most marked between 15 and 29 years (risk ratio (RR) 2.7, p = 0.0000), and remained persistent up to the age of 64 years (RR 1.7, p = 0.0007). For children, highest attendance was observed for those <5 years of age in urban areas (121 per 100 000 compared with 49 per 100 000 in mixed/rural areas), and of these, groups with lower SES had highest attendance (quartiles 3 and 4, with 189 per 100 000 and 129 per 100 000 respectively, compared with 88 per 100 000 and 76 per 100 000 for quartiles 1 and 2). Within the mixed/rural groups, for those <5 years of age, an inverse relationship between attendance and SES was found (rates of 87, 51, 38 and 25 per 100 000 from quartiles 1 to 4).
DISCUSSION
The overall HI incidence per 100 000 (453) falls within the range identified in this study in northwest England (88–886) as do those of the urban (826) and mixed/rural (223) areas.4,5 Our mean attendance is higher than the average rates found in recent UK studies, but significantly lower than a study based on 1974 data.3,4,5 This may reflect differential rates, or may be due to differences in the timescales of studies, or of accuracy of coding and recording of head injuries.18 Our rate for MSHI (40 per 100 000) falls below but near that of estimates for the UK, but with a significant variation between urban area of residence (56 per 100 000) compared with mixed/rural area of residence (30 per 100 000). The discrepancy with the Australian rate may be explained by their focus on “severe” injuries.7 The finding of 10.9% of all cases falling into the MSHI category is consistent with that reported in other studies.19
Males are more at risk than females. Adolescent and adult males may be more at risk due to participating in particular occupational and leisure activities. Children and adolescents have been considered risk groups for injury.20,21 Our findings support this view, but we also found a very high rate of MSHI in the age group <5 years old for both males and females in urban areas.
We found a greater risk of presenting with head injuries for urban compared with mixed/rural areas of residence. These findings are consistent with rates from the USA, where mortality rates and injury severity were found to be higher in inner city communities.11,22 This differential pattern may be attributable, in part, to such factors as greater density of population, traffic flow, and, potentially, crime rates.
Social deprivation is a risk factor for child injury mortality.23,24 Our findings suggest children <5 years of age from lower socioeconomic groups in urban areas are particularly vulnerable. This could be due to a range of factors noted above, and to less access to safety information and/or services and products.25 We discovered a inverse relationship between SES and attendance in children in mixed/rural areas for those <5 years of age. People of higher SES in more rural areas may have greater travel distances, use less public transport, and/or those of lower SES may have barriers to accessing healthcare.5 Further research on whether “hidden needs” exists is crucial.
Prospective research into specific causes of injury are indicated, as are analyses of the contribution of SES whilst controlling for area of residence and distance. This was an ecological study and as such is subject to confounding. We attempted to minimise this by using age specific rates rather than an age standardisation, given the U shaped relationship with age. Diagnostic codes may not reliably identify all head or brain injuries; moreover, we may expect the minority of those with mild HI to have sustained long term neurological sequelae to their injuries.14,18 Thus, the rates we found may well be a conservative estimate of the number of cases of long term neurological disability.
ACKNOWLEDGEMENTS
We thank L Ellett (research psychologist) for her contribution to initial data management, J Ridgers (ED information manager) for the preparation of data, and our colleagues in the Royal Devon and Exeter clinical audit department for their cooperation and assistance with the first phase of analyses.
Abbreviations
ED - emergency department
HI - head injury
MSHI - moderate to severe head injury
PCT - primary care trust
RR - risk ratio
SES - socioeconomic status
Footnotes
Competing interests: P J Yates and W H Williams have been reimbursed by government and professional scientific bodies for attending scientific symposiums. Other research into head injuries in their departments have been supported by the Economic and Social Research Council.
This study was approved by the local research ethics committee and Caldicott Guardian of the Royal Devon & Exeter Hospital Trust.
References
- 1.Fleminger S, Ponsford J. Long term outcome after traumatic brain injury. More attention needs to be paid to neuropsychiatric functioning. BMJ 20053311419–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turner‐Stokes L. The national service framework for long term conditions: a novel approach for a “new style” NSF. J Neurol Neurosurg Psychiatry 200576901–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jennett B, MacMillan R. Epidemiology of head injury. BMJ 1981282101–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tennant A. The epidemiology of head injury. In: Chamberlain MA, Neumann V, Tennant A, eds. Traumatic brain injury rehabilitation: services, treatments and outcomes. London: Chapman Hall, 1996
- 5.Tennant A. Admission to hospital following head injury in England: Incidence and socio‐economic associations. BMC Public Health 2005521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wenden F J, Crawford S, Wade D T. Assault, post‐traumatic amnesia and other variables related to outcome following head injury. Clin Rehabil 19961253–63. [DOI] [PubMed] [Google Scholar]
- 7.Tate T. Incidence of hospital‐treated traumatic brain injury in an Australian community. Aust N Z J Public Health 199822419–423. [DOI] [PubMed] [Google Scholar]
- 8.Kreutzer J S, Witol A D, Marwitz J H. Alcohol and drug use among young persons with traumatic brain injury. J Learn Disabil 199629643–651. [DOI] [PubMed] [Google Scholar]
- 9.Thurman D J, Guerrero J L. Trends in hospitalisation associated with traumatic brain injury. J Am Med Assoc 1999282954–957. [DOI] [PubMed] [Google Scholar]
- 10.Stella J, Spivulis P, Cooke C. Head injury‐related road crash mortality in rural Western Australia. Aust N Z Jnl Surg 200171665–668. [DOI] [PubMed] [Google Scholar]
- 11.Whitman S, Coonley‐Hoganson R, Desai B T. Comparative head trauma experiences in two socio‐economically different Chicago‐area communities: a population study. Am J Epidemiol 1984119570–580. [DOI] [PubMed] [Google Scholar]
- 12.Dunn L, Henry J, Beard D. Social Deprivation and adult head injury: A national study. J Neurol Neurosurg Psychiatry 2003741060–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.J J, Hauser W A. The epidemiology of traumatic brain injury: A review. Epilepsia 200344(suppl)2–10. [DOI] [PubMed] [Google Scholar]
- 14.Jennett B. Epidemiology of head injury. Arch Dis Child 199878403–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.NHS Centre for Coding and Classification 1996 Health Service Guidelines – NHS Executive, (96)23. www.connectingforhealth.nhs.uk/clinicalcoding . Accessed 11 January 2006
- 16.Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet 1974281–84. [DOI] [PubMed] [Google Scholar]
- 17.Department for Environment, Transport and the Regions Index of multiple deprivation 2000: regeneration research summary, number 31. London: The Stationery Office, 2000
- 18.Deb S. ICD‐10 codes detect only a proportion of all head injury admissions. Brain Inj 199913369–373. [DOI] [PubMed] [Google Scholar]
- 19.Kay A, Teasdale G. Head injury in the United Kingdom. World J Surgery 2003251210–1220. [DOI] [PubMed] [Google Scholar]
- 20.Greenwald B D, Burnett D M, Miller M A. Congenital and acquired brain injury; epidemiology and pathophysiology. Arch Phys Med Rehab 200384S3–S7. [PubMed] [Google Scholar]
- 21.Guerrero J L, Thurman D J, Sniezek J E. Emergency department visits associated with traumatic brain injury: United States, 1995–1996. Brain Inj 200014181–186. [PubMed] [Google Scholar]
- 22.Wagner A K, Dasser H C, Hammond F M.et al Intentional traumatic brain injury: epidemiology, risk factors, and associations with injury severity and mortality. J Trauma 200049404–410. [DOI] [PubMed] [Google Scholar]
- 23.Roberts I, Power C. Does the decline in child injury mortality vary by social class? A comparison of class specific mortality in1981 and 1991. BMJ 1996313784–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lyons R A, Jones S J, Deacon T.et al Socioeconomic variation in children and older people: A population based study. Inj Prev 2003933–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lalloo R, Sheiham A. Risk factors for childhood major and minor head and other injuries in a nationally representative sample. Injury 200334261–266. [DOI] [PubMed] [Google Scholar]