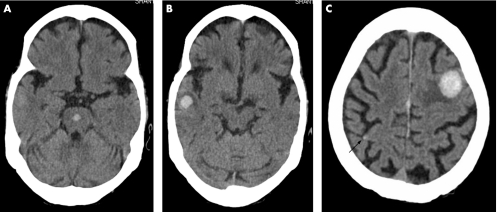
During an outbreak of dengue viral infection in India, a 68‐year‐old woman presented with fever and myalgia for 4 days and altered sensorium for 1 day. At presentation, she was comatose with a Glasgow Coma score of 6. Physical examination showed high fever (39°C), mild conjunctival injection and hepatosplenomegaly. The pulse rate and blood pressure were within normal limits. The tourniquet test was positive. Laboratory investigations showed mild leucocytosis, thrombocytopenia (65 000 per mm3) and increased haematocrit (48.7%). Prothrombin time and partial thromboplastin time were raised. There was associated hypoproteinaemia (3.2 g/dl) and increased serum aspartate aminotransferase (985 U/l). The test for dengue‐specific IgM antibody was positive. The cerebrospinal fluid also showed dengue‐specific IgM antibody; protein, cell and glucose levels in cerebrospinal fluid were normal. Non‐contrast computed tomography of the brain (fig 1) showed multiple well‐defined haematomas within the cerebral parenchyma and pons with surrounding oedema. Unfortunately, the patient did not survive the infection, and died on the third day after admission.
Figure 1 Non‐contrast computed tomography of the brain shows multiple focal parenchymal haemorrhages in the pons (A), right temporal lobe (B), left high frontal lobe (C) and right parietal lobe (arrow in C). Surrounding oedema is seen around the right temporal and left frontal lesions.
Dengue fever is an acute febrile viral illness presenting with headache, bone or joint pains, myalgias and rash. Dengue haemorrhagic fever (DHF) is characterised by four major clinical manifestations: high fever, haemorrhagic phenomena, often hepatomegaly, and, in severe cases, signs of circulatory failure. A few patients may develop hypovolaemic shock because of plasma leakage. This is called dengue shock syndrome.1
Dengue associated encephalopathy is an atypical manifestation. It accounted for only 0.5% of 5400 patients admitted with DHF in a study by Cam et al.2 In most cases, it is thought to be caused by prolonged DHF with fluid extravasation, cerebral oedema, hyponatraemia, liver failure, renal failure or a possible direct neurotropic effect of dengue virus. The neurological symptoms are only rarely caused by bleeding. In the study by Cam et al,2 only 1 out of 27 patients with dengue‐associated encephalopathy had intracranial haemorrhage.
Apart from coagulopathy, the other aetiologies of intracranial haematomas include trauma, hypertension, amyloid angiopathy, neoplasm, vascular malformation and infarction.
Although a rare manifestation of DHF, encephalopathy should, however, be investigated in endemic areas and during epidemics of dengue, as early diagnosis is essential for its management.
References
- 1.de Souza L J, Martins A L, Paravidini P C.et al Hemorrhagic encephalopathy in dengue shock syndrome: a case report. Braz J Infect Dis 20059257–261. [DOI] [PubMed] [Google Scholar]
- 2.Cam B V, Fonsmark L, Hue N B.et al Prospective case‐control study of encephalopathy in children with dengue hemorrhagic fever. Am J Trop Med Hyg 200165848–851. [DOI] [PubMed] [Google Scholar]