The case of a patient who presented with a necrotic myelopathy and bilateral optic neuritis in association with a thymoma and circulating anti‐CV2/CRMP5 antibodies is reported. This case shows that in some rare instances, a clinical presentation suggestive of a neuromyelitis optica can be of paraneoplastic origin.
A 45‐year‐old woman with a history of Hashimoto thyroiditis presented with a 4‐month history of asthenia and a weight loss of 10 kg. A computed tomography of the chest showed an anterior mediastinal mass suspicious for a thymoma. The mediastinal mass was completely removed by surgery. Histological examination showed a B2‐type thymoma with pleural, pericardial and left phrenic local extension. There was no evidence of mediastinal adenopathy or metastasis on computed tomography of the abdomen and pelvis. Treatment with radiation therapy was planned, but 1 month later the patient developed difficulties in walking for over 2 weeks, paraesthesia of the four limbs and bladder dysfunction.
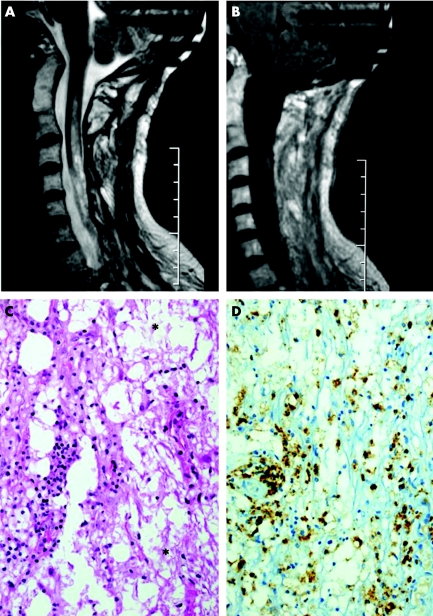
Neurological examination showed a left spastic motor paresis, brisk reflexes and a left Babinski response; proprioceptive sensation was predominantly affected on the left limbs, whereas pain and thermal sensation were affected on the right limbs, suggesting a left cervical Brown–Sequard syndrome. Visual acuity was initially normal. There was no sign of polyneuropathy, and electromyography was normal. The patient did not have fever, and had no signs of systemic disease and no sicca syndrome on general examination. Magnetic resonance imaging (MRI) of the spine showed an enlargement of the cervical cord consecutive to an extensive cervicodorsal (C1 to D7) intramedullary lesion with focal heterogenous gadolinium enhancement (fig 1A,B). MRI of the brain was normal. The cerebrospinal fluid (CSF) had only an increased protein concentration of 82 g/dl; there was no intrathecal synthesis of IgG, and isoelectric focusing was negative. Polymerase chain reaction of herpes simplex virus (HSV)1 and HSV2 was negative in the CSF on two occasions. The following microbiological tests were also negative; enterovirus, varicella zoster virus, cytomegalovirus, Epstein‐Barr virus, Lyme disease, syphilis, HIV and Mycoplasma pneumoniae. Anti‐double‐stranded DNA antibodies and anti‐Sjogren's syndrome A and B antibodies were negative.
Figure 1 T2‐weighted sequence of the spinal cord magnetic resonance imaging showing an extensive cervical intramedullary hypersignal (A). T1 sequence after gadolinium infusion showing focal heterogenous gadolinium enhancement (B). (C) Haematoxylin, ploxine and saffron staining of the biopsy showing reactive gliosis, oedema, necrosis (*) and microglial infiltration. (D) CD68 immunostaining showing microglial infiltration (brown colouration).
As an intramedullary metastasis of the thymoma was suspected, a biopsy of the lesion was performed at level C7. On histological examination, the lesions were found to be localised in both white and and grey matter. These lesions consisted of a reactive gliosis, with foci of oedema and necrosis with numerous macrophages and some perivascular lymphocytes (fig 1C,D). Bodian luxol coloration showed demyelinisation. There were no features of vasculitis, nor of viral inclusion or tumour infiltration. This was consistent with a necrotic myelopathy. Serum screening for neuromyelitis optica (NMO) IgG antibodies was negative.1 Serum screening for onconeural antibodies was negative for anti‐Hu, anti‐Ri, anti‐Yo, and anti‐amphyphysin antibodies, but was strongly positive for anti‐CV2/CRMP5 antibodies. Immediately after the biopsy, the patient became quadripleglic; this deterioration was probably related to the biopsy. She developed an intestinal subocclusion complicated with aspiration pneumonia. She was treated with high‐dose methylprednisolone, but her condition did not improve and she developed a respiratory insufficiency that necessitated artificial ventilation in an intensive care unit. Ten plasma exchanges were also ineffective. At 4 months after the onset of myelopathy, the patient presented a bilateral painless visual loss. Funduscopic examination was normal, and evoked visual potentials showed a bilateral optic neuropathy. The patient finally died of septicaemia 5 months after the onset of myelopathy. No necropsy was performed.
Discussion
Histological evaluation in our patient showed a necrotic myelopathy. It seems unlikely that occlusive vascular disease was implicated because the illness progressed over several weeks. Pathologically, there was no vascular occlusion, and the distribution of the lesions did not correspond to the territory of supply of any of the cord's vessels. There were neither clinical nor biological arguments for an infectious, postinfectious or vasculitic myelitis. In particular, HSV2, which has been reported in association with acute necrotic myelopathy in patients with cancer, was negative in the CSF (polymerase chain reaction). The patient did not receive radiotherapy, thus excluding a radiation myelopathy.
At 4 months after the onset of myelopathy, the patient presented a bilateral optic neuritis suggesting Devic's syndrome. As in our patient, the myelopathy in Devic's syndrome is usually necrotic. However, the subacute clinical onset, the context of a recently diagnosed malignant thymoma and the presence of anti‐CV2/CRMP5 antibodies distinguish our case from that of patients with “classic” Devic's syndrome. These features rather suggest that in our patient this Devic's syndrome‐like phenotype was paraneoplastic.2 Furthermore, even if it does not exclude Devic's syndrome, we did not detect anti‐NMO antibodies.1 The clinical presentation and histological examination of the myelopathy could have been consistent with a paraneoplastic necrotising myelopathy, but a bilateral optic neuritis has never been described in this clinical entity.3 A case of Devic's syndrome occurring after surgical resection of a thymoma was recently described by Antoine et al4. However, this patient was different because he had myasthenia gravis, developed necrotising myositis in addition to neuromyelitis optica, and had antibodies reacting with the central nervous system and thymic epithelial cells in the serum, but no anti‐CV2/CRMP5 antibodies. In fact, the most likely hypothesis in our case is that the Devic's syndrome‐like phenotype was related to the presence of anti‐CV2/CRMP5 antibodies. Cross et al5 recently reported three patients who had a myelopathy with optic neuritis, anti‐CV2/CRMP5 antibodies and a cancer. Associated cancer was a thyroid papillary carcinoma, a small cell lung cancer and a renal cell cancer. Similar to our case, two patients had an extensive myelopathy and in one of them there was a gadolinium enhancement of the entire thoracic cord suggesting necrotic myelopathy. An autopsy was performed in a third patient (patient 15) with a less extensive myelopathy (spinal MRI abnormalities were limited to a patchy midthoracic T2 hypersignal). Spinal cord pathology showed microglial infiltration, important T cell infiltration but no necrosis. In contrast, the histological evaluation in our patient showed an important microglial infiltration with foci of oedema and necrosis. It shows that in patients with a Devic's syndrome‐like phenotype and anti‐CV2/CRMP5 antibodies, the myelopathy can be necrotic as in Devic's syndrome. Together with Cross et al's5 article, our report also suggests that the presence of anti‐CV2/CRMP5 antibodies should be carefully studied in cases of myelopathy of unknown origin.
Acknowledgements
We thank V Rogemond and G Cavillon for their technical assistance.
Footnotes
Competing interests: None.
References
- 1.Lennon V A, Wingerchuk D M, Kryzer T J.et al A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet 20043642106–2112. [DOI] [PubMed] [Google Scholar]
- 2.Graus F, Delattre J Y, Antoine J C.et al Recommended diagnostic criteria for paraneoplastic neurological syndromes. J Neurol Neurosurg Psychiatry 2004751135–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ojeda V J. Necrotizing myelopathy associated with malignancy. A clinicopathologic study of two cases and literature review. Cancer 1984531115–1123. [DOI] [PubMed] [Google Scholar]
- 4.Antoine J C, Camdessanché J P, Absi L.et al Devic disease and thymoma with anti‐central nervous system and antithymus antibodies. Neurology 200462978–980. [DOI] [PubMed] [Google Scholar]
- 5.Cross S A, Salomao D R, Parisi J E.et al Paraneoplastic auto‐immune optic neuritis with retinitis defined by CRMP‐5‐IgG. Ann Neurol 20035438–50. [DOI] [PubMed] [Google Scholar]